Dental Implant Rehabilitation of Posterior Maxillary Edentulism via Sinus Augmentation Using the Lateral Window Technique: A Retrospective Analysis of 289 Implants Followed Up for 15 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patient Selection Criteria
2.3. Premedication
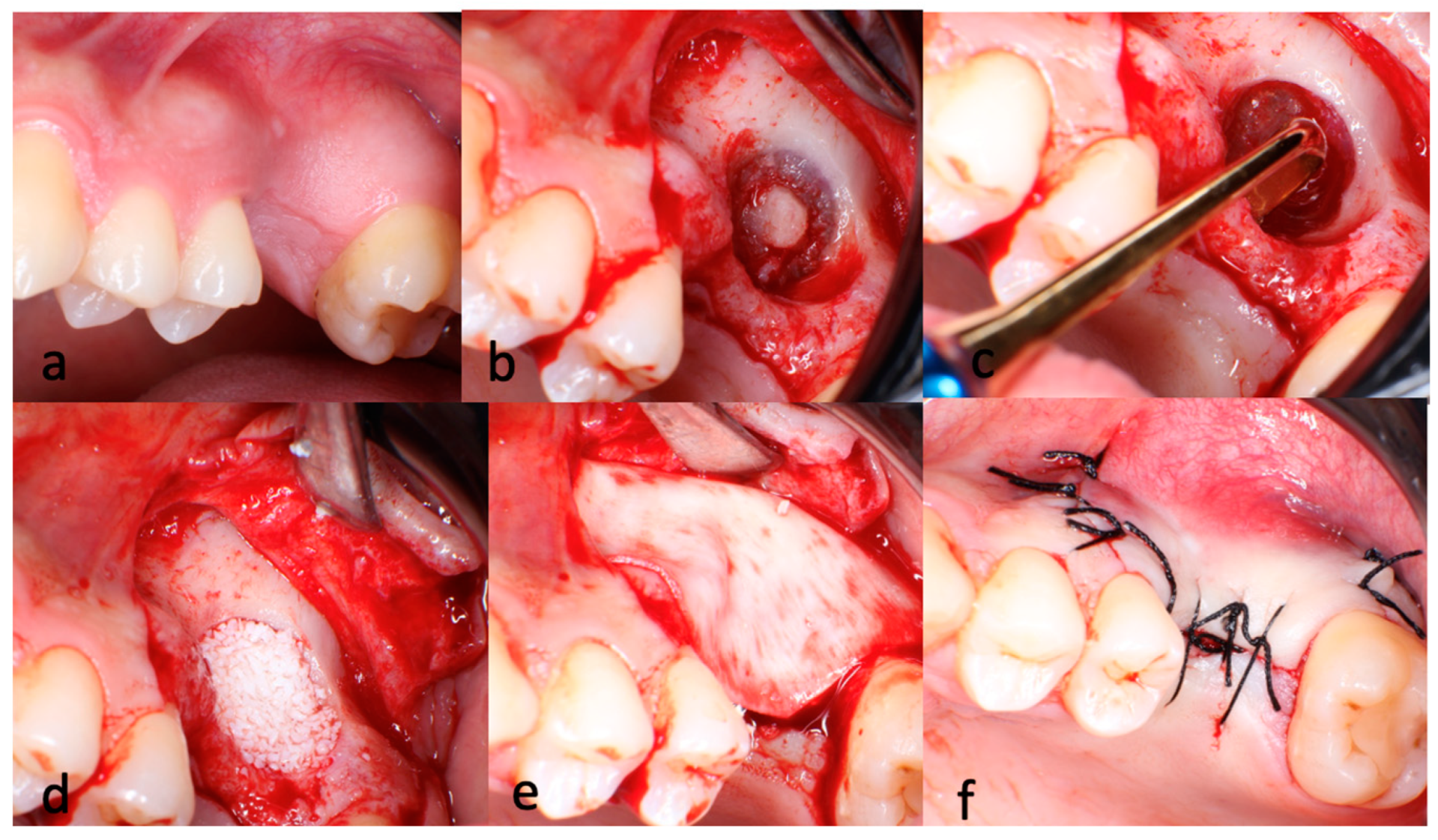
2.4. Surgical and Restorative Steps
2.5. Analysis of the Study Data
2.6. Statistical Analysis
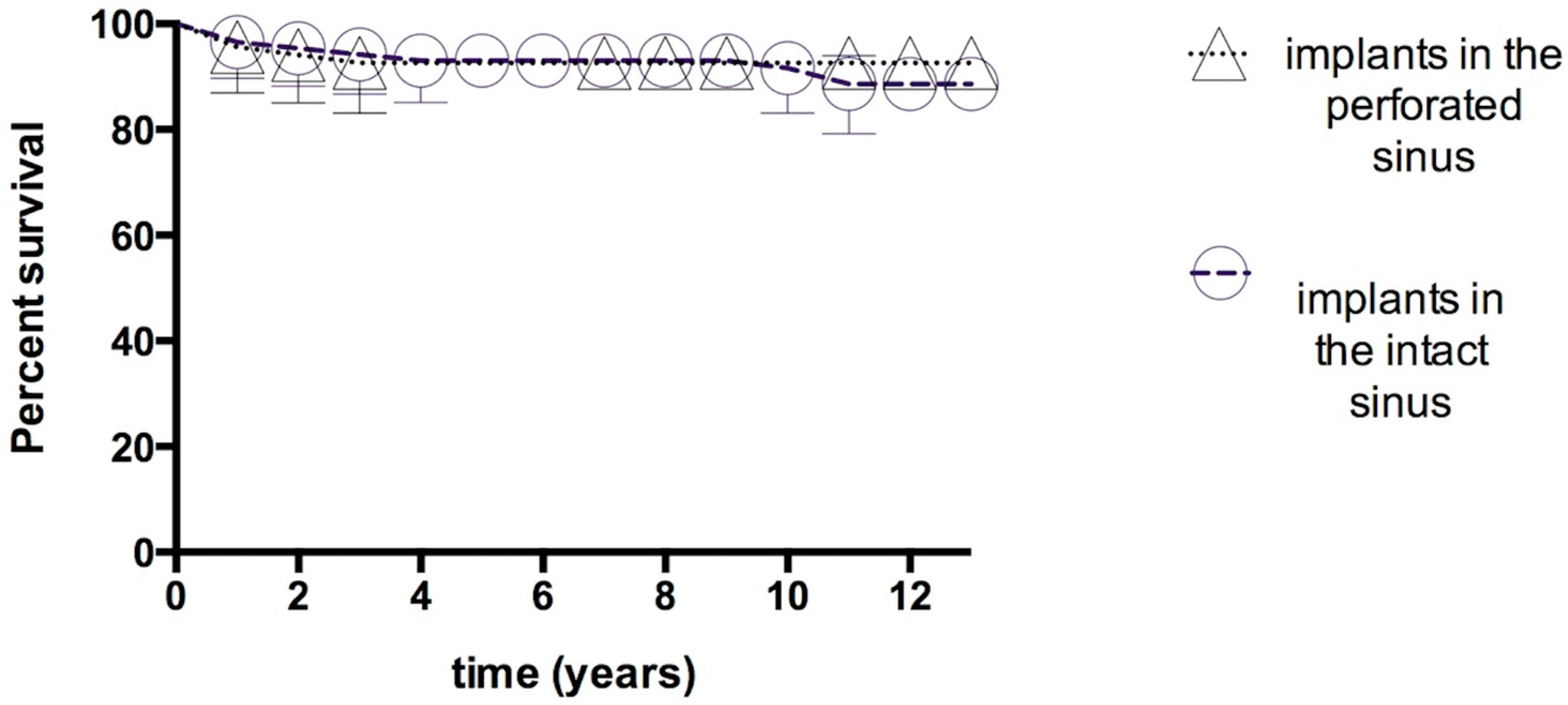
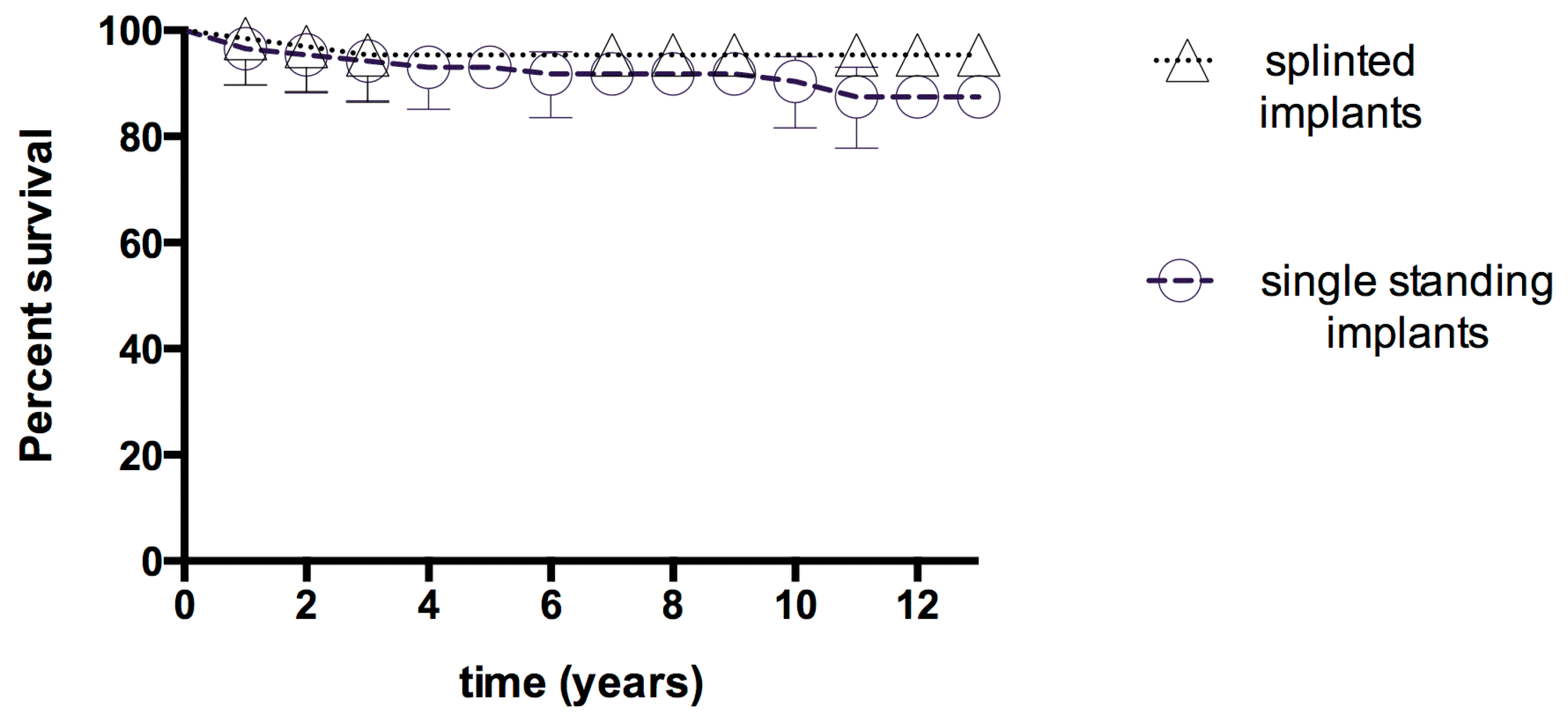
3. Results
3.1. Early-Term Complications and Failures
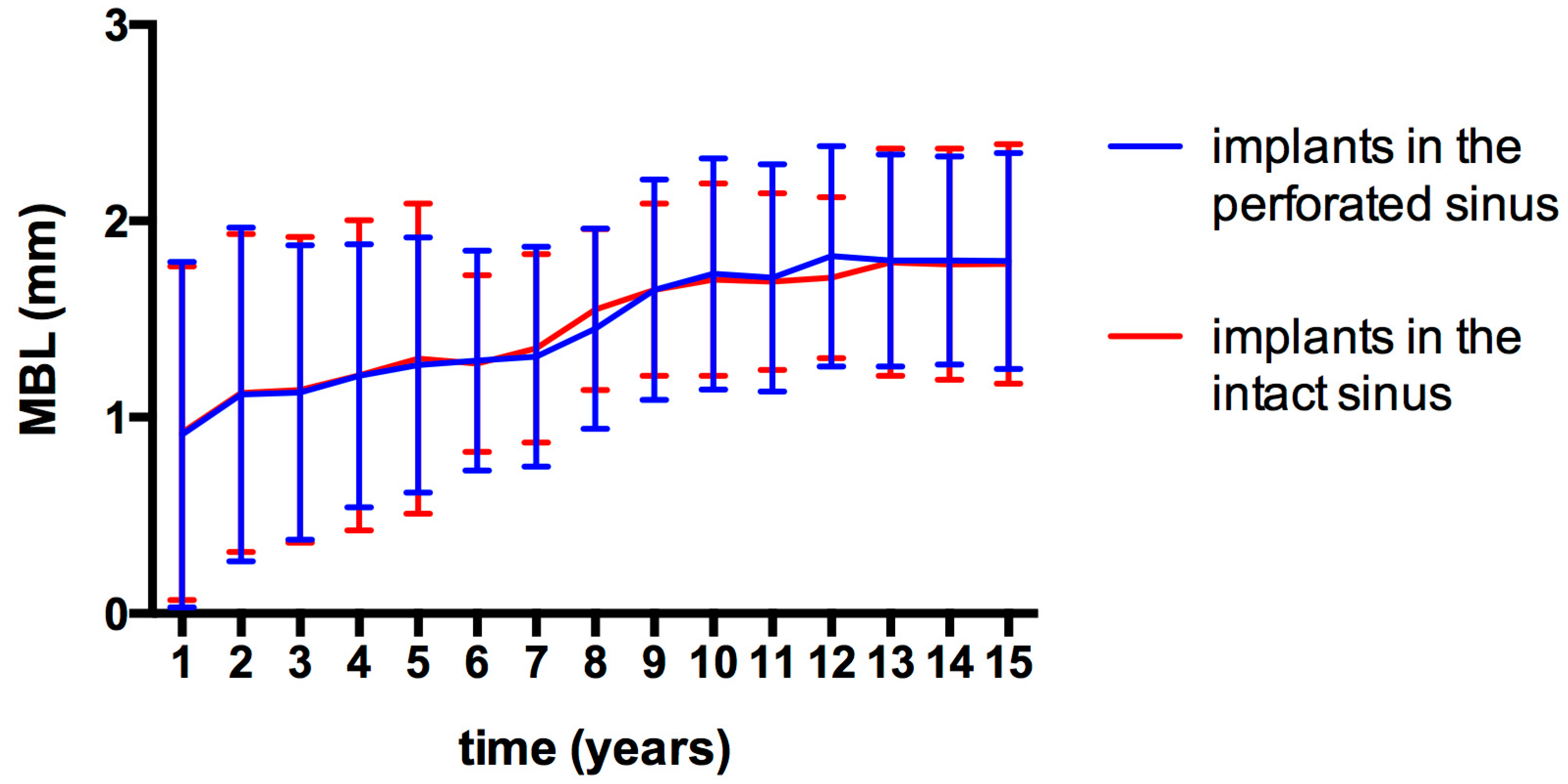
3.2. Marginal Bone Loss (MBL)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yu, Z.; Ma, Y.; Li, C.; Bi, W. Research Progress of Maxillary Sinus Cyst and Maxillary Posterior Dental Region Implantation. Int. J. Biol. Sci. 2023, 3, 44–46. [Google Scholar] [CrossRef]
- Tatum, H. Maxillary and Sinus Implant Reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; James, R.A. Grafting of the Maxillary Sinus Floor with Autogenous Marrow and Bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar] [PubMed]
- Van Den Bergh, J.P.A.; Ten Bruggenkate, C.M.; Disch, F.J.M.; Tuinzing, D.B. Anatomical Aspects of Sinus Floor Elevations. Clin. Oral Implants Res. 2000, 11, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Sala, Y.M.; Lu, H.; Chrcanovic, B.R. Clinical Outcomes of Maxillary Sinus Floor Perforation by Dental Implants and Sinus Membrane Perforation during Sinus Augmentation: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1253. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A New Concept in Maxillary Implant Surgery: The Osteotome Technique. Compendium 1994, 15, 152. [Google Scholar]
- Zitzmann, N.U.; Schärer, P. Sinus Elevation Procedures in the Resorbed Posterior Maxilla: Comparison of the Crestal and Lateral Approaches. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Vernamonte, S.; Mauro, V.; Vernamonte, S.; Messina, A.M. An Unusual Complication of Osteotome Sinus Floor Elevation: Benign Paroxysmal Positional Vertigo. Int. J. Oral Maxillofac. Surg. 2011, 40, 216–218. [Google Scholar] [CrossRef]
- Mazor, Z.; Kfir, E.; Lorean, A.; Mijiritsky, E.; Horowitz, R.A. Flapless Approach to Maxillary Sinus Augmentation Using Minimally Invasive Antral Membrane Balloon Elevation. Implant Dent. 2011, 20, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Poblete-Michel, M.M.J.-M. Clinical Success in Bone Surgery Using Ultrasonic Devices; Quintessence Books; Quintessence Publishing Company, Inc.: Batavia, IL, USA, 2009. [Google Scholar]
- Kim, J.M.; Sohn, D.S.; Heo, J.U.; Park, J.S.; Jung, H.S.; Moon, J.W.; Lee, J.H.; Park, I.S. Minimally Invasive Sinus Augmentation Using Ultrasonic Piezoelectric Vibration and Hydraulic Pressure: A Multicenter Retrospective Study. Implant Dent. 2012, 21, 536–542. [Google Scholar] [CrossRef]
- Puterman, I.; Weinstein, B.; Walton, P.; Fien, M. The Modified Osseodensification Visco-Elastic (MOVE) Sinus Protocol: A Case Series to Illustrate the Combination of Osseodensification with Viscoelastic Bone Replacement Material. Clin. Adv. Periodontics 2022, 12, 180–185. [Google Scholar] [CrossRef]
- Fischer, J.L.; Riley, C.A.; Kacker, A. Sinonasal Complications Following the Sinus Lift Procedure. Ochsner J. 2023, 23, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Tanaka, T.; Ibaragi, S.; Okui, T.; Hamaguchi, J.; Min, S.; Tubbs, R.S. Revisiting Major Anatomical Risk Factors of Maxillary Sinus Lift and Soft Tissue Graft Harvesting for Dental Implant Surgeons. Surg. Radiol. Anat. 2020, 42, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Jamali, S.; Nasrabadi, N.; Payahoo, S.; Darvish, M.; Ahmadizadeh, H.; Khosravi, S. Management of the Maxillary Sinus Complications after Dental Implantation: A Systematic Review and Meta-Analysis. Braz. Dent. Sci. 2020, 23, 1–10. [Google Scholar] [CrossRef]
- Kirmeier, R.; Payer, M.; Wehrschuetz, M.; Jakse, N.; Platzer, S.; Lorenzoni, M. Evaluation of Three-Dimensional Changes after Sinus Floor Augmentation with Different Grafting Materials. Clin. Oral Imlants Res. 2008, 19, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Menini, M.; Canullo, L.; Khijmatgar, S.; Modenese, L.; Gallifante, G.; Del Fabbro, M. Radiographic and Histomorphometric Evaluation of Biomaterials Used for Lateral Sinus Augmentation: A Systematic Review on the Effect of Residual Bone Height and Vertical Graft Size on New Bone Formation and Graft Shrinkage. J. Clin. Med. 2021, 10, 4996. [Google Scholar] [CrossRef] [PubMed]
- Fouad, W.; Osman, A.; Atef, M.; Hakam, M. Guided Maxillary Sinus Floor Elevation Using Deproteinized Bovine Bone versus Graftless Schneiderian Membrane Elevation with Simultaneous Implant Placement: Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2018, 20, 420–433. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2195. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alfaro, F.; Torradeflot, M.M.; Marti, C. Prevalence and Management of Schneiderian Membrane Perforations during Sinus-Lift Procedures. Clin. Oral Implants Res. 2008, 19, 91–98. [Google Scholar] [CrossRef]
- ten Bruggenkate, C.M.; van den Bergh, J.P.A. Maxillary Sinus Floor Elevation: A Valuable Pre-prosthetic Procedure. Periodontol. 2000 1998, 17, 176–182. [Google Scholar] [CrossRef]
- Randolph, R. Resnik. Misch’s Contemporary Implant Dentistry, 4th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Karabuda, C.; Arısan, V.; Hakan, Ö. Effects of Sinus Membrane Perforations on the Success of Dental Implants Placed in the Augmented Sinus. J. Periodontol. 2006, 77, 1991–1997. [Google Scholar] [CrossRef] [PubMed]
- Prentice, R.L.; Kalbfleisch, J.D. Hazard Rate Models with Covariates. Biometrics 1979, 35, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, D.A. Sample-Size Formula for the Proportional-Hazards Regression Model. Biometrics 1983, 39, 499–503. [Google Scholar] [CrossRef]
- Cricchio, G.; Sennerby, L.; Lundgren, S. Sinus Bone Formation and Implant Survival after Sinus Membrane Elevation and Implant Placement: A 1-to 6-year Follow-up Study. Clin. Oral Implants Res. 2011, 22, 1200–1212. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Bretón Brinkmann, J.; Madrigal Martínez-Pereda, C.; Farfán Navio, G.; Díaz-Olivares, L.A.; Leco-Berrocal, I.; Barona-Dorado, C.; López-Quiles, J. Influence of Schneiderian Membrane Perforation during Maxillary Sinus Floor Augmentation with Lateral Approach on Dental Implant Survival Rates: A Retrospective Study in a University Setting. Clin. Oral Investig. 2024, 28, 625. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Olivares, L.A.; Cortés-Bretón Brinkmann, J.; Martínez-Rodríguez, N.; Martínez-González, J.M.; López-Quiles, J.; Leco-Berrocal, I.; Meniz-García, C. Management of Schneiderian Membrane Perforations during Maxillary Sinus Floor Augmentation with Lateral Approach in Relation to Subsequent Implant Survival Rates: A Systematic Review and Meta-Analysis. Int. J. Implant Dent. 2021, 7, 91. [Google Scholar] [CrossRef] [PubMed]
- Schiavo-Di Flaviano, V.; Egido-Moreno, S.; González-Navarro, B.; Velasco-Ortega, E.; López-López, J.; Monsalve-Guil, L. Influence of Schneiderian Membrane Perforation on Implant Survival Rate: Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 3751. [Google Scholar] [CrossRef] [PubMed]
- Starch-Jensen, T.; Aludden, H.; Hallman, M.; Dahlin, C.; Christensen, A.E.; Mordenfeld, A. A Systematic Review and Meta-Analysis of Long-Term Studies (Five or More Years) Assessing Maxillary Sinus Floor Augmentation. Int. J. Oral Maxillofac. Surg. 2018, 47, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Al-Dajani, M. Incidence, Risk Factors, and Complications of Schneiderian Membrane Perforation in Sinus Lift Surgery: A Meta-Analysis. Implant Dent. 2016, 25, 409–415. [Google Scholar] [CrossRef]
- Danesh-Sani, S.A.; Loomer, P.M.; Wallace, S.S. A Comprehensive Clinical Review of Maxillary Sinus Floor Elevation: Anatomy, Techniques, Biomaterials and Complications. Br. J. Oral Maxillofac. Surg. 2016, 54, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.S.; Lee, J.W.; Chong, J.H.; Han, J.J.; Jung, S.; Kook, M.S.; Park, H.J.; Ryu, S.Y.; Oh, H.K. Evaluation of Clinical Outcomes of Implants Placed into the Maxillary Sinus with a Perforated Sinus Membrane: A Retrospective Study. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 50. [Google Scholar] [CrossRef] [PubMed]
- Viña-Almunia, J.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. Influence of Perforation of the Sinus Membrane on the Survival Rate of Implants Placed after Direct Sinus Lift. Literature Update. Med. Oral Patol. Oral Cir. Bucal. 2009, 14, 133–136. [Google Scholar]
- Raza, M.; Albeshri, S.; Wallace, S.S. Repairing Maxillary Sinus Membrane Perforations, Iatrogenic or Intentional: Two Case Reports. Clin. Adv. Periodontics 2022, 12, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Pignataro, L.; Mantovani, M.; Torretta, S.; Felisati, G.; Sambataro, G. ENT Assessment in the Integrated Management of Candidate for (Maxillary) Sinus Lift. Acta Otorhinolaryngol. Ital. 2008, 28, 110–119. [Google Scholar]
- Fugazzotto, P.A.; Vlassis, J. A Simplified Classification and Repair System for Sinus Membrane Perforations. J. Periodontol. 2003, 74, 1534–1541. [Google Scholar] [CrossRef]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian Membrane Perforation and Sinus Lift Graft Outcome: A Retrospective Evaluation of 359 Augmented Sinus. J. Oral Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, B.E.; Westhoff, D.; Behrens, E.; Wiltfang, J.; Becker, S.T. Impact of Surgical Management in Cases of Intraoperative Membrane Perforation during a Sinus Lift Procedure: A Follow-up on Bone Graft Stability and Implant Success. Int. J. Implant Dent. 2018, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Kao, S.Y.; Lui, M.T.; Cheng, D.H.; Chen, T.W. Lateral Trap-Door Window Approach with Maxillary Sinus Membrane Lifting for Dental Implant Placement in Atrophied Edentulous Alveolar Ridge. J. Chin. Med. Assoc. 2015, 78, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, Y.; Yu, Z.; Tang, L.; Zhang, J.; Yang, G.; Huang, T. Radiographic Outcomes of Lateral Sinus Floor Elevation at Sites without Perforations and Sites with Perforations Managed with a Resorbable Membrane: A Retrospective Study. J. Clin. Periodontol. 2024, 51, 1134–1146. [Google Scholar] [CrossRef]
- Carmagnola, D.; Pispero, A.; Pellegrini, G.; Sutera, S.; Henin, D.; Lodi, G.; Achilli, A.; Dellavia, C. Maxillary Sinus Lift Augmentation: A Randomized Clinical Trial with Histological Data Comparing Deproteinized Bovine Bone Grafting vs Graftless Procedure with a 5–12-year Follow-up. Clin. Implant Dent. Relat. Res. 2024, 26, 972–985. [Google Scholar] [CrossRef] [PubMed]
- Jamcoski, V.H.; Faot, F.; Marcello-Machado, R.M.; Melo, A.C.M.; Fontão, F.N.G.K. 15-Year Retrospective Study on the Success Rate of Maxillary Sinus Augmentation and Implants: Influence of Bone Substitute Type, Presurgical Bone Height, and Membrane Perforation during Sinus Lift. Biomed Res. Int. 2023, 2023, 9144661. [Google Scholar] [CrossRef] [PubMed]
- Alsharekh, M.S.; Almutairi, A.A.; Jahlan, A.S.; Alhazani, A.S.; Almohaimeed, S.M.; Aljnoubi, L.A.; AlGhamdi, G.A.; AlBenyan, T.T.; Alduhyaman, S.F.; Alnaffaie, N.M.; et al. Evolving Techniques and Trends in Maxillary Sinus Lift Procedures in Implant Dentistry: A Review of Contemporary Advances. Cureus 2024, 16, 71424. [Google Scholar] [CrossRef] [PubMed]
- Manso MC, V.G. Instalação Imediata de Implantes Rosqueados Em Seios Maxilares Extremamente Pneumatizados. Rev. Bras. Implant. 2001, 7, 8–12. [Google Scholar]
- Zhou, Y.; Shi, Y.; Si, M.; Wu, M.; Xie, Z. The Comparative Evaluation of Transcrestal and Lateral Sinus Floor Elevation in Sites with Residual Bone Height ≤6 Mm: A Two-Year Prospective Randomized Study. Clin. Oral Implants Res. 2021, 32, 180–191. [Google Scholar] [CrossRef]
- Reiser, G.M.; Rabinovitz, Z.; Bruni, J.; Damoulis, P.; Griffin, T.J. Evaluation of Maxillary Sinus Membrane Response Following Elevation with the Crestal Osteotome Technique in Human Cadavers. Int. J. Oral Maxillofac. Implants 2001, 16, 833–840. [Google Scholar]
- Saglanmak, A.; Cinar, I.C.; Zboun, M.; Arisan, V.; Mijiritsky, E. Maxillary Sinus Floor Elevation and Simultaneous Implant Installation via Osseodensification Drills: A Retrospective Analysis of Bone Gain in 72 Patients Followed for 6 Months. J. Clin. Med. 2024, 13, 2225. [Google Scholar] [CrossRef]
- Mazor, Z.; Gaspar, J.; Silva, R.; Pohl, S.; Gandhi, Y.; Huwais, S.; Bergamo, E.T.P.; Bonfante, E.A.; Neiva, R. Maxillary Sinus Membrane Perforation Rate Utilizing Osseodensification-mediated Transcrestal Sinus Floor Elevation: A Multicenter Clinical Study. Clin. Implant Dent. Relat. Res. 2024, 26, 1172–1180. [Google Scholar] [CrossRef] [PubMed]
- Ellegaard, B.; Baelum, V.; Petersen, J.K. Non-Grafted Sinus Implants in Periodontally Compromised Patients: A Time-to-Event Analysis. Clin. Oral Implants Res. 2006, 17, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Park, W.B.; Kang, K.L.; Han, J.Y. Factors Influencing Long-Term Survival Rates of Implants Placed Simultaneously with Lateral Maxillary Sinus Floor Augmentation: A 6- to 20-Year Retrospective Study. Clin. Oral Implants Res. 2019, 30, 97–988. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Moreno, P.; León-Cano, A.; Ortega-Oller, I.; Monje, A.; O’valle, F.; Catena, A. Marginal Bone Loss as Success Criterion in Implant Dentistry: Beyond 2 Mm. Clin. Oral Implants Res. 2015, 26, 28–34. [Google Scholar] [CrossRef]
- Carr, A.B.; Arwani, N.; Lohse, C.M.; Gonzalez, R.L.V.; Muller, O.M.; Salinas, T.J. Early Implant Failure Associated with Patient Factors, Surgical Manipulations, and Systemic Conditions. J. Prosthodont. 2019, 28, 623–633. [Google Scholar] [CrossRef] [PubMed]
| Interval (Years) | Implants at the Start of Interval | Drop-Outs | Drop-Outs (Died) | Implants Under Risk | Failures During Interval | Survival Rate (%) | Cumulative Survival Rate (%) |
|---|---|---|---|---|---|---|---|
| 0–1 | 289 | 0 | 0 | 289 | 7 | 97.58 | 97.58 |
| 1–2 | 282 | 1 | 1 | 280 | 6 | 97.85 | 95.44 |
| 2–3 | 274 | 2 | 0 | 272 | 2 | 99.26 | 94.71 |
| 3–4 | 270 | 1 | 1 | 268 | 1 | 99.62 | 94.24 |
| 4–5 | 267 | 3 | 3 | 261 | 0 | 100 | 94.24 |
| 5–6 | 261 | 3 | 9 | 249 | 0 | 100 | 94.24 |
| 6–7 | 249 | 3 | 3 | 243 | 0 | 100 | 94.24 |
| 7–8 | 243 | 4 | 6 | 233 | 0 | 100 | 94.24 |
| 8–9 | 233 | 2 | 0 | 231 | 0 | 100 | 94.24 |
| 9–10 | 231 | 2 | 0 | 229 | 1 | 99.56 | 93.81 |
| 10–11 | 228 | 3 | 0 | 225 | 2 | 99.11 | 92.93 |
| 11–12 | 223 | 4 | 0 | 219 | 0 | 100 | 92.93 |
| 12–13 | 219 | 11 | 0 | 208 | 0 | 100 | 92.93 |
| 13–14 | 208 | 9 | 0 | 199 | 0 | 100 | 92.93 |
| 14–15 | 199 | 12 | 0 | 187 | 0 | 100 | 92.93 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sağlanmak, A.; Arısan, V.; Karabuda, C.; Özyuvacı, H. Dental Implant Rehabilitation of Posterior Maxillary Edentulism via Sinus Augmentation Using the Lateral Window Technique: A Retrospective Analysis of 289 Implants Followed Up for 15 Years. J. Funct. Biomater. 2025, 16, 65. https://doi.org/10.3390/jfb16020065
Sağlanmak A, Arısan V, Karabuda C, Özyuvacı H. Dental Implant Rehabilitation of Posterior Maxillary Edentulism via Sinus Augmentation Using the Lateral Window Technique: A Retrospective Analysis of 289 Implants Followed Up for 15 Years. Journal of Functional Biomaterials. 2025; 16(2):65. https://doi.org/10.3390/jfb16020065
Chicago/Turabian StyleSağlanmak, Alper, Volkan Arısan, Cüneyt Karabuda, and Hakan Özyuvacı. 2025. "Dental Implant Rehabilitation of Posterior Maxillary Edentulism via Sinus Augmentation Using the Lateral Window Technique: A Retrospective Analysis of 289 Implants Followed Up for 15 Years" Journal of Functional Biomaterials 16, no. 2: 65. https://doi.org/10.3390/jfb16020065
APA StyleSağlanmak, A., Arısan, V., Karabuda, C., & Özyuvacı, H. (2025). Dental Implant Rehabilitation of Posterior Maxillary Edentulism via Sinus Augmentation Using the Lateral Window Technique: A Retrospective Analysis of 289 Implants Followed Up for 15 Years. Journal of Functional Biomaterials, 16(2), 65. https://doi.org/10.3390/jfb16020065









