Comparative Evaluation of Color Stability and Fracture Resistance of CAD/CAM and Chairside Provisional Restorations: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Objectives
2.2. Model Fabrication and Digital Workflow
2.2.1. Intraoral Scanning and Model Preparation
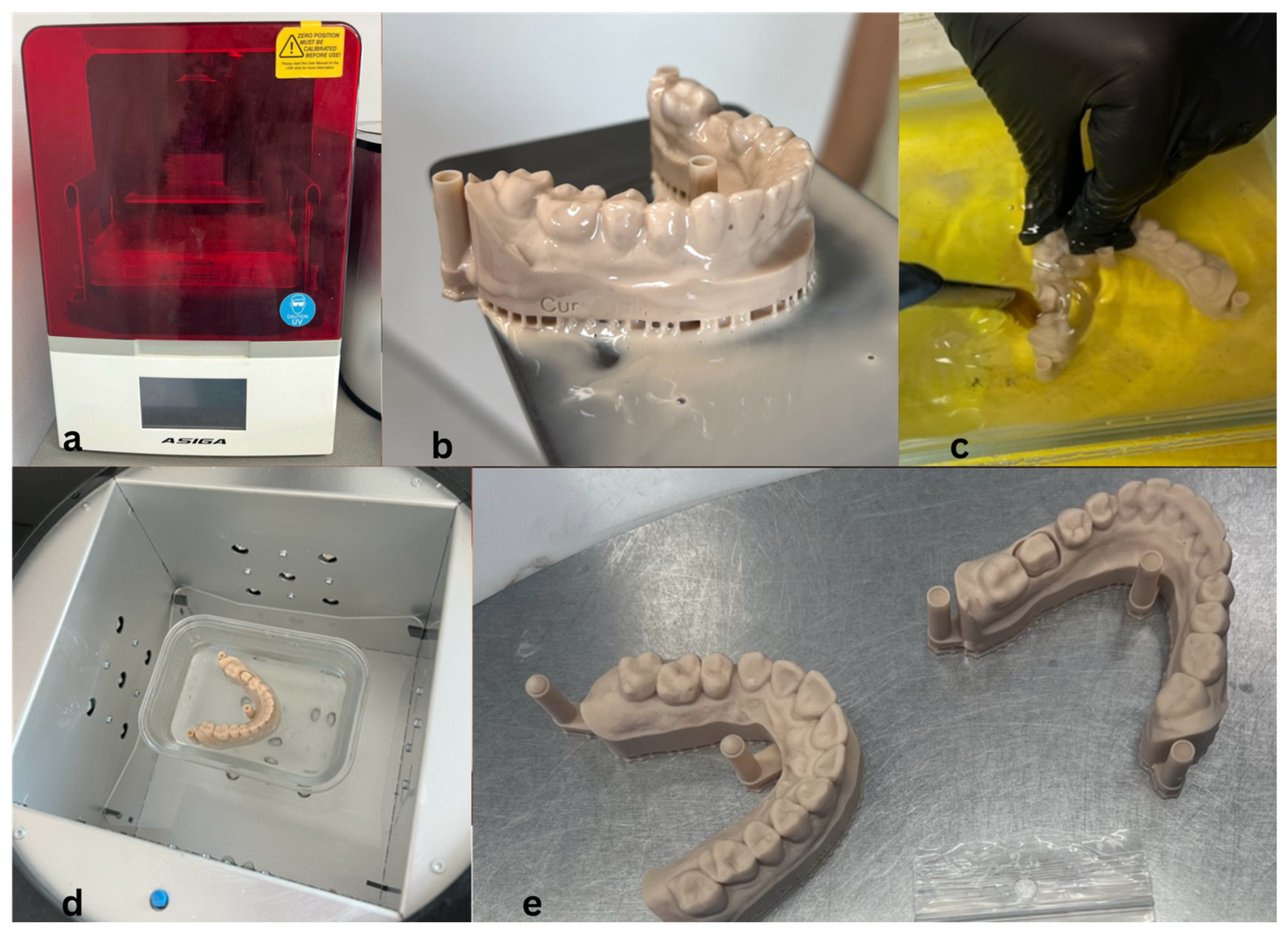
2.2.2. Three-Dimensional Printing of Working Models
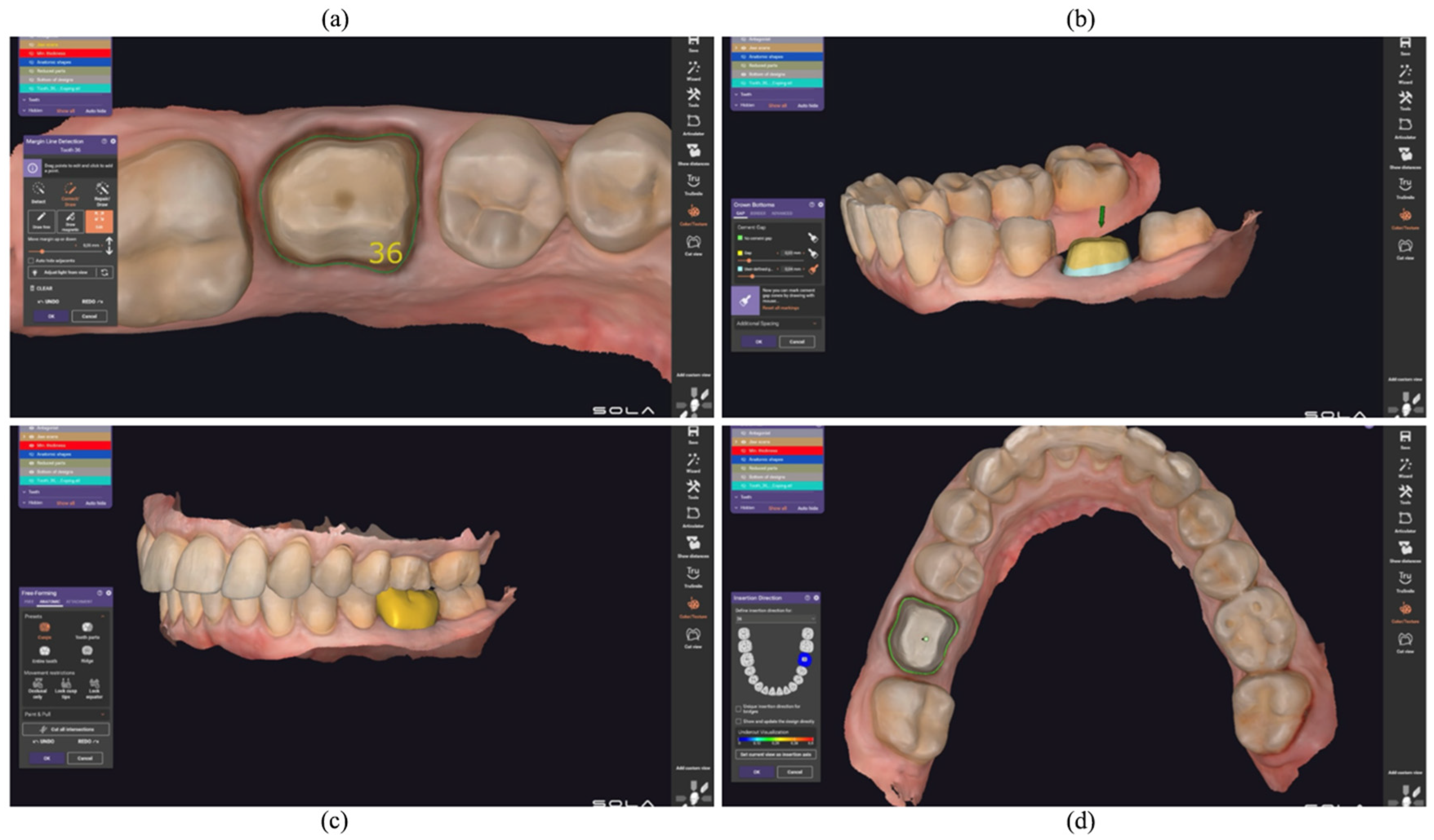
2.3. CAD Design and CAM Manufacturing
2.3.1. Virtual Design and Articulation
2.3.2. Milling Procedure
2.4. Fabrication of Provisional Crowns Using the Conventional Direct Chairside Technique
2.5. Experimental Evaluation
2.5.1. Color Stability Assessment
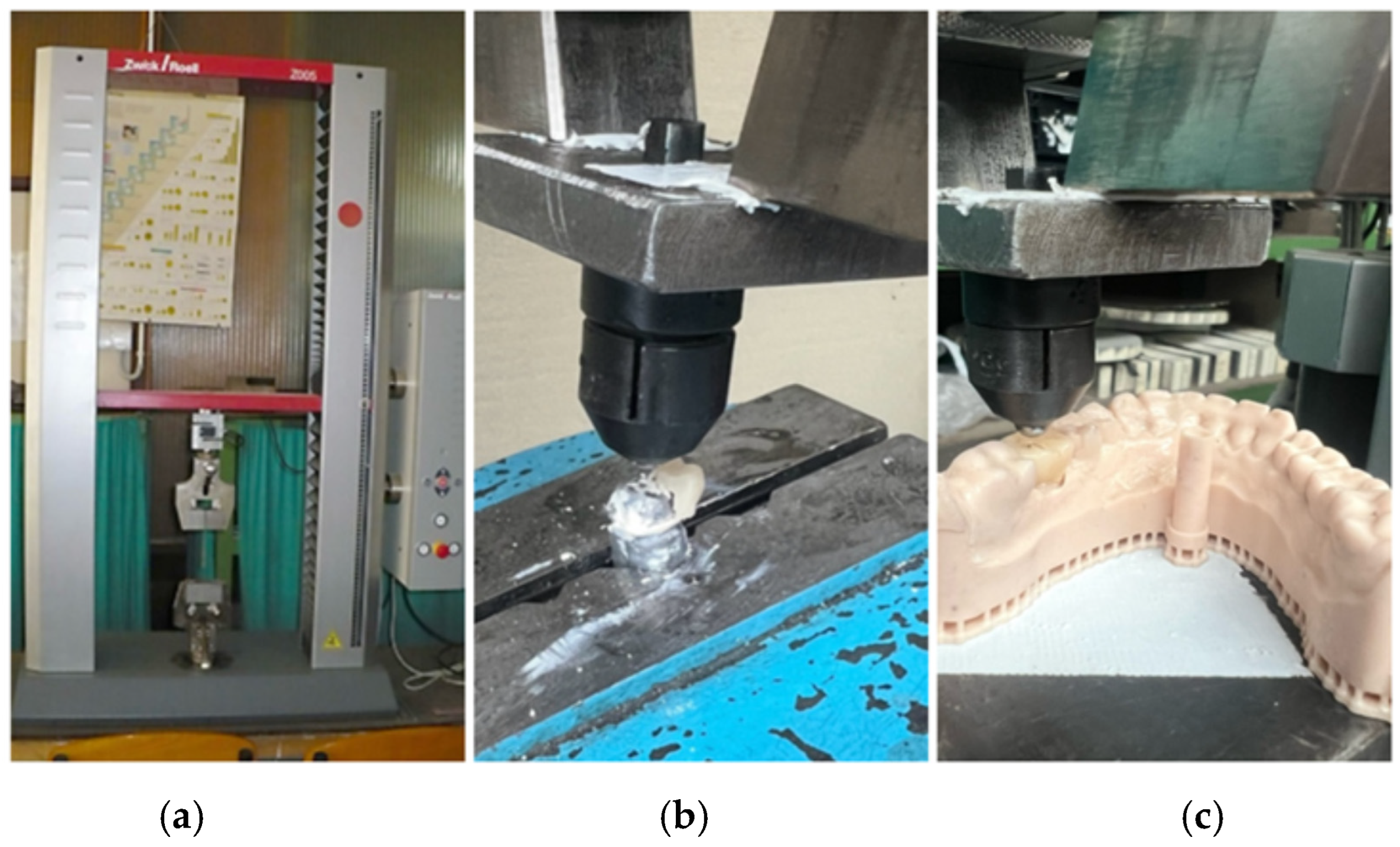
2.5.2. Fracture Resistance Testing
2.6. Statistical Analysis
3. Results
3.1. Color Stability
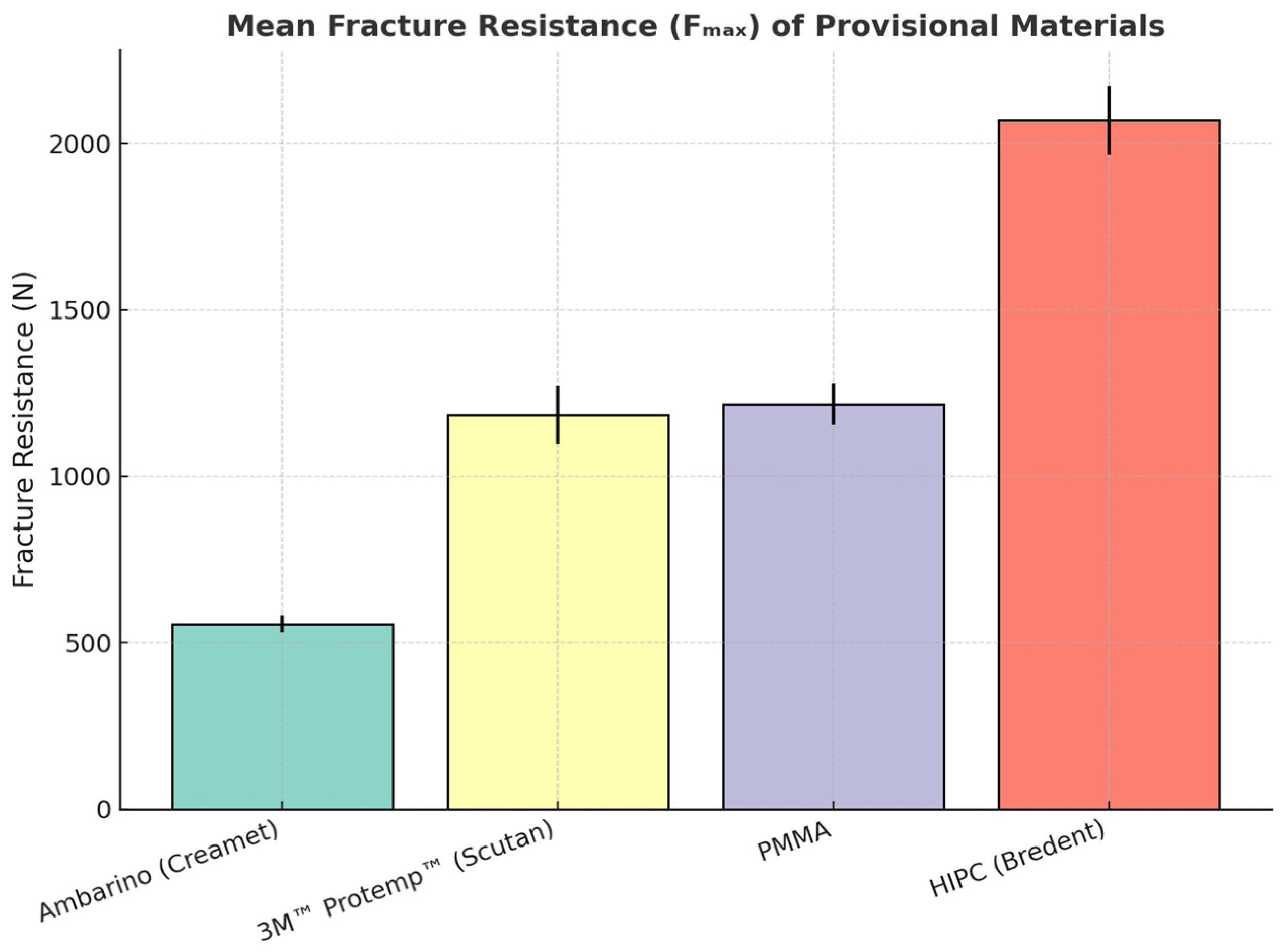
3.2. Fracture Resistance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goodacre, C.J.; Spolnik, K.J. The prosthodontic management of endodontically treated teeth: A literature review. Part I. Success and failure data, treatment concepts. J. Prosthodont. 1994, 3, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 5th ed.; Elsevier: St. Louis, MO, USA, 2016; pp. 185–210. [Google Scholar]
- Misch, C.E.; Perez, H.A.; Sato, Y. Contemporary Implant Dentistry, 4th ed.; Mosby: St. Louis, MO, USA, 2015; pp. 120–145. [Google Scholar]
- Shillingburg, H.T.; Hobo, S.; Whitsett, L.; Jacobi, R.; Brackett, S. Fundamentals of Fixed Prosthodontics, 4th ed.; Quintessence Publishing: Chicago, IL, USA, 2012; pp. 300–320. [Google Scholar]
- Donovan, T.E.; Cho, S.-H. Provisional Restorations in Fundamentals of Operative Dentistry: A Contemporary Approach; Young, D.A., Hicks, M.J., Eds.; Fusayama’s Methodology Revisited; Quintessence Publishing: Berlin, Germany, 2014; pp. 345–355. [Google Scholar]
- Magne, P.; Belser, U.C. Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach; Quintessence Publishing: Chicago, IL, USA, 2017; pp. 210–230. [Google Scholar]
- Chee, W.W. Provisional restorations in soft tissue management around dental implants. Periodontology 2000 2001, 27, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Germano, F.; Arcuri, L.; Bigelli, E.; Arcuri, C.; Barlattani, A. CEREC CAD/CAM Chairside System. Oral Implantol. 2015, 7, 57–70. [Google Scholar] [PubMed] [PubMed Central]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Represa, V.; Abalos-Labruzzi, C.; Herrera-Martinez, M.; Guerrero-Pérez, M.O. Nanomaterials in Dentistry: State of the Art and Future Challenges. Nanomaterials 2020, 10, 1770. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fasbinder, D.J. Digital dentistry: Innovation for restorative treatment. Compend. Contin. Educ. Dent. 2010, 31, 2–11. [Google Scholar] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Fehér, A.; Filser, F.; Lüthy, H.; Gauckler, L.J.; Schärer, P.; Franz Hämmerle, C.H. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence Int. 2006, 37, 685–693. [Google Scholar] [PubMed]
- Anselm Wiskott, H.W.; Perriard, J.; Scherrer, S.S.; Dieth, S.; Belser, U.C. In vivo wear of three types of veneering materials using implant-supported restorations: A method evaluation. Eur. J. Oral Sci. 2002, 110, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Strasding, M.; Valente, N.A.; Zwahlen, M.; Liu, S.; Pjetursson, B.E. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin. Oral Implant. Res. 2018, 29 (Suppl. 16), 184–198. [Google Scholar] [CrossRef]
- Lee, H.-J.; Jeon, J.; Moon, H.S.; Oh, K.C. Digital Workflow to Fabricate Complete Dentures for Edentulous Patients Using a Reversing and Superimposing Technique. Appl. Sci. 2021, 11, 5786. [Google Scholar] [CrossRef]
- Hategan, S.I.; Belea, A.L.; Tanase, A.D.; Gavrilovici, A.M.; Petrescu, E.L.; Marsavina, L.; Sinescu, C.; Negrutiu, M.L.; Manole, M.C. The Evaluation of the Prosthetic Preparations Finish Lines for Provisional Crowns with the Impact on Periodontal Health. Rom. J. Oral Rehabil. 2024, 16, 453–459. [Google Scholar] [CrossRef]
- Balkenhol, M.; Knapp, M.; Ferger, P.; Heun, U.; Wöstmann, B. Correlation between polymerization shrinkage and marginal fit of temporary crowns. Dent. Mater. 2008, 24, 1575–1584. [Google Scholar] [CrossRef] [PubMed]
- Doray, P.G.; Eldiwany, M.S.; Powers, J.M. Effect of resin surface sealers on improvement of stain resistance for a composite provisional material. J. Esthet. Restor. Dent. 2003, 15, 244–249; discussion 249–250. [Google Scholar] [CrossRef] [PubMed]
- Chitpattanakul, P.; Prawatvatchara, W.; Limpuangthip, N.; Katheng, A.; Uasuwan, P.; Boonpitak, K. Effect of various solvents on the repairability of aged CAD/CAM provisional restorative materials with flowable resin composite: An in vitro study. BMC Oral Health 2025, 25, 368. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Atria, P.J.; Lagos, I.; Sampaio, C.S. In vitro evaluation of surface roughness, color stability, and color masking of provisional restoration materials for veneers and crowns. Int. J. Comput. Dent. 2020, 23, 343–350. [Google Scholar] [PubMed]
- Sham, A.S.; Chu, F.C.; Chai, J.; Chow, T.W. Color stability of provisional prosthodontic materials. J. Prosthet. Dent. 2004, 91, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Conrad, H.J.; Seong, W.-J.; Pesun, I.J. Current ceramic materials and systems with clinical ecommendations: A systematic review. J. Prosthet. Dent. 2007, 98, 389–404. [Google Scholar] [CrossRef]
- Anusavice, K.J. Phillips’ Science of Dental Materials, 12th ed.; Saunders: St. Louis, MO, USA, 2013; pp. 270–300. [Google Scholar]
- Yildiz, E.; Sirin Karaarslan, E.; Simsek, M.; Ozsevik, A.S.; Usumez, A. Color stability and surface roughness of polished anterior restorative materials. Dent. Mater. J. 2015, 34, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Powers, J.M.; Sakaguchi, R.L. Craig’s Restorative Dental Materials, 14th ed.; Elsevier: St. Louis, MO, USA, 2013; pp. 160–190. [Google Scholar]
- Heintze, S.D.; Forjanic, M.; Ohmiti, K.; Rousson, V. Surface deterioration of dental materials after simulated toothbrushing in relation to brushing time and load. Dent. Mater. 2010, 26, 306–319. [Google Scholar] [CrossRef] [PubMed]
- Bollen, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Burrow, M.F.; Tyas, M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J. Dent. 2005, 33, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Bedir, F.; Karadas, M. Evaluation of Color Stability and Translucency of Different Composite Resins Exposed to Alcohol. Niger. J. Clin. Pract. 2024, 27, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Cappare, P.; Sannino, G.; Minoli, M.; Montemezzi, P.; Ferrini, F. Conventional versus Digital Impressions for Full Arch Screw-Retained Maxillary Rehabilitations: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2019, 16, 829. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Hassouneh, L.; Jum’ah, A.; Ferrari, M.; Wood, D.J. A Micro-computed Tomography Analysis of Marginal and Internal Fit of Endocrowns Fabricated from Three CAD/CAM Materials. Oper. Dent. 2023, 48, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Saravi, B.; Vollmer, A.; Hartmann, M.; Lang, G.; Kohal, R.-J.; Boeker, M.; Patzelt, S.B.M. Clinical Performance of CAD/CAM All-Ceramic Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. Materials 2021, 14, 2672. [Google Scholar] [CrossRef]
- Duarte, S., Jr.; Phark, J.-H. Advances in Dental Restorations: A Comprehensive Review of Machinable and 3D-Printed Ceramic-Reinforced Composites. J. Esthet. Restor. Dent. 2025, 37, 257–276. [Google Scholar] [CrossRef]
- Hajaj, T.; Lile, I.E.; Veja, I.; Titihazan, F.; Rominu, M.; Negruțiu, M.L.; Sinescu, C.; Novac, A.C.; Talpoș-Niculescu, S.; Zaharia, C. Influence of Pontic Length on the Structural Integrity of Zirconia Fixed Partial Dentures (FPDs). J. Funct. Biomater. 2025, 16, 116. [Google Scholar] [CrossRef]
- Hajaj, T.; Marian, D.; Zaharia, C.; Niculescu, S.T.; Negru, R.M.; Titihazan, F.; Rominu, M.; Sinescu, C.; Novac, A.C.; Dobrota, G.; et al. Fracture Resistance of CAD/CAM-Fabricated Zirconia and Lithium Disilicate Crowns with Different Margin Designs: Implications for Digital Dentistry. J. Funct. Biomater. 2025, 16, 205. [Google Scholar] [CrossRef]
- Hajaj, T.; Lile, I.E.; Negru, R.M.; Niculescu, S.T.; Stuparu, S.; Rominu, M.; Sinescu, C.; Albu, P.; Titihazan, F.; Veja, I. Adhesive Performance of Zirconia and Lithium Disilicate Maryland Cantilever Restorations on Prepared and Non-Prepared Abutment Teeth: An In Vitro Comparative Study. Biomimetics 2025, 10, 413. [Google Scholar] [CrossRef] [PubMed]
- Lile, I.E.; Hajaj, T.; Constantin, G.D.; Niculescu, S.T.; Marian, D.; Stana, O.; Zaharia, C.; Veja, I. Association Between Occlusal Interferences, Temporomandibular Joint Dysfunction, and Bruxism in Romanian Adults. J. Clin. Med. 2025, 14, 5612. [Google Scholar] [CrossRef]
- Niculescu, S.T.; Veja, I.; Constantin, G.-D.; Lile, I.E.; Armeniakos, C.; Munteanu, I.R.; Hajaj, T. Comparative In Vitro Evaluation of Marginal Sealing in Class I Composite Restorations Using Fifth- and Seventh-Generation Adhesives. J. Funct. Biomater. 2025, 16, 301. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Al-Harbi, F.A.; Rahoma, A.; Al-Zordk, W.A. Color Stability and Surface Roughness of 3D-Printed, CAD/CAM-Milled, and Conventional Denture Resins: An In Vitro Comparative Study. J. Prosthodont. 2021, 30, 695–702. [Google Scholar] [CrossRef]
- Hassan, R.H.; Elsheikh, A.; Alhajj, M.N.; Abotaleb, M.M.; Ali, A.I.; Badran, O. Mechanical Properties and Fracture Resistance of CAD/CAM Provisional Materials: An In Vitro Study. J. Prosthet. Dent. 2022, 128, 874–881. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Effects of Printing Orientation and Post-Curing on the Flexural Strength of 3D-Printed Resin Materials for Provisional Restorations. J. Prosthodont. 2020, 29, 164–170. [Google Scholar] [CrossRef]
- Gad, M.M.; Al-Harbi, F.A.; Abualsaud, R.; Rahoma, A.; Al-Zordk, W.A. Fracture Resistance and Microhardness of CAD/CAM and Conventional Interim Restorations Fabricated from Different Materials. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef]
- Saini, R.S.; Gurumurthy, V.; Quadri, S.A.; Bavabeedu, S.S.; Abdelaziz, K.M.; Okshah, A.; Alshadidi, A.A.F.; Yessayan, L.; Mosaddad, S.A.; Heboyan, A. The flexural strength of 3D-printed provisional restorations fabricated with different resins: A systematic review and meta-analysis. BMC Oral Health 2024, 24, 66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ayuso-Montero, R.; Salmerón-Valdés, E.N.; Cerutti-Kopplin, D.; Roig, M.; Jané-Salas, E. Color Stability of Provisional Restorative Materials Exposed to Different Beverages: An In Vitro Study. J. Esthet. Restor. Dent. 2020, 32, 371–378. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.-F. Evaluation of Mechanical and Optical Properties of Current High-Performance CAD/CAM Polymers for Long-Term Provisional Restorations. J. Esthet. Restor. Dent. 2021, 33, 303–313. [Google Scholar] [CrossRef]
| Material | n | Shade Before | Shade After | ΔE (Mean ± SD) |
|---|---|---|---|---|
| HIPC (Bredent) | 10 | A2 | A3 | 2.8 ± 0.3 |
| Ambarino (Creamet) | 10 | B3 | B3 | 1.1 ± 0.2 |
| 3M™ Protemp™ (Scutan) | 10 | A3 | A4 | 4.9 ± 0.4 |
| PMMA | 10 | Bleach 1 | Bleach 1 | 2.0 ± 0.3 |
| Material | Mean (N) | SD (N) | Tukey Group |
|---|---|---|---|
| Ambarino (Creamet) | 555.41 | 25.40 | d |
| 3M™ Protemp™ (Scutan) | 1183.40 | 86.40 | c |
| PMMA | 1215.78 | 61.36 | c |
| HIPC (Bredent) | 2068.92 | 103.99 | a |
| Comparison | Mean Difference (N) | Significance |
|---|---|---|
| HIPC vs. PMMA | 853.1 | *** |
| HIPC vs. Protemp™ | 885.5 | *** |
| HIPC vs. Ambarino | 1513.5 | *** |
| PMMA vs. Protemp™ | 32.4 | ns |
| PMMA vs. Ambarino | 660.4 | *** |
| Protemp™ vs. Ambarino | 628.0 | *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Titihazan, F.; Veja, I.; Zaharia, C.; Hajaj, T.; Sinescu, C.; Constantin, G.D.; Rominu, M. Comparative Evaluation of Color Stability and Fracture Resistance of CAD/CAM and Chairside Provisional Restorations: An In Vitro Study. J. Funct. Biomater. 2025, 16, 426. https://doi.org/10.3390/jfb16110426
Titihazan F, Veja I, Zaharia C, Hajaj T, Sinescu C, Constantin GD, Rominu M. Comparative Evaluation of Color Stability and Fracture Resistance of CAD/CAM and Chairside Provisional Restorations: An In Vitro Study. Journal of Functional Biomaterials. 2025; 16(11):426. https://doi.org/10.3390/jfb16110426
Chicago/Turabian StyleTitihazan, Florina, Ioana Veja, Cristian Zaharia, Tareq Hajaj, Cosmin Sinescu, George Dumitru Constantin, and Mihai Rominu. 2025. "Comparative Evaluation of Color Stability and Fracture Resistance of CAD/CAM and Chairside Provisional Restorations: An In Vitro Study" Journal of Functional Biomaterials 16, no. 11: 426. https://doi.org/10.3390/jfb16110426
APA StyleTitihazan, F., Veja, I., Zaharia, C., Hajaj, T., Sinescu, C., Constantin, G. D., & Rominu, M. (2025). Comparative Evaluation of Color Stability and Fracture Resistance of CAD/CAM and Chairside Provisional Restorations: An In Vitro Study. Journal of Functional Biomaterials, 16(11), 426. https://doi.org/10.3390/jfb16110426









