Fracture and Fatigue of Dental Implants Fixtures and Abutments with a Novel Internal Connection Design: An In Vitro Pilot Study Comparing Three Different Dental Implant Systems
Abstract
1. Introduction
2. Materials and Methods
2.1. Types of Specimens and Preparation
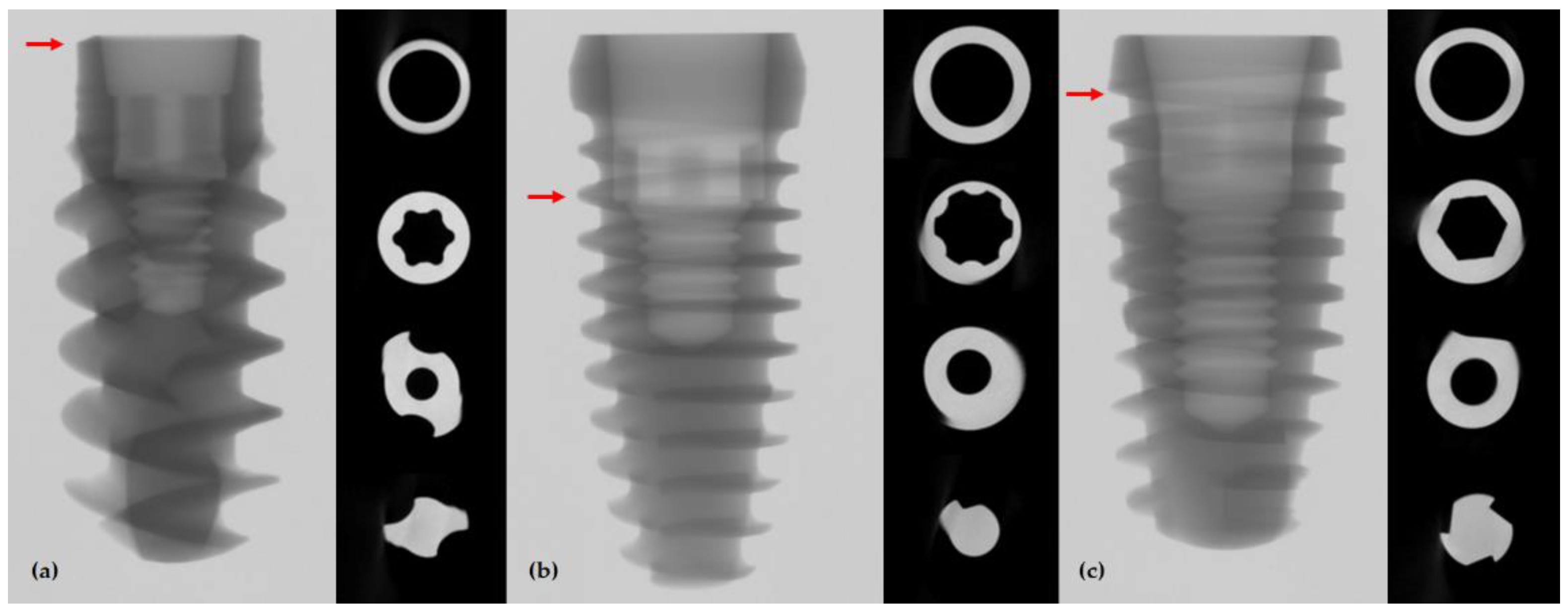
2.2. Acquisition of Micro-Computed Tomography (μ-CT) Image
2.3. Static Compression to Fracture Test and Dynamic Cyclic Fatigue Test
2.4. Statistical Analysis
3. Results
3.1. μ-CT Image Analysis
3.2. Result of Static Compression to Fracture Test
3.3. Result of Dynamic Cyclic Fatigue Test
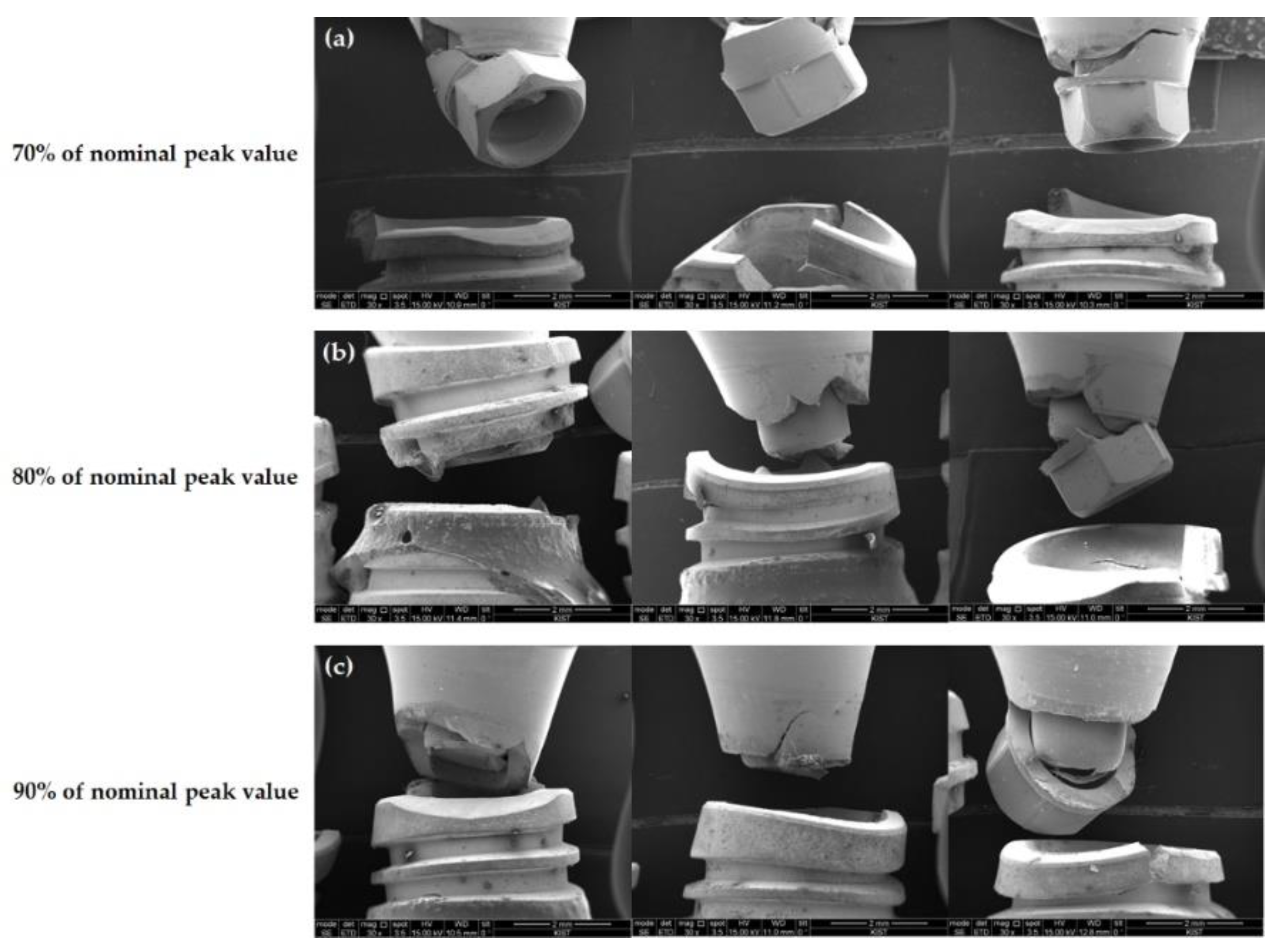
3.4. Failure Modes on Microscopic Observation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buser, D.; Janner, S.F.; Wittneben, J.G.; Bragger, U.; Ramseier, C.A.; Salvi, G.E. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: A retrospective study in 303 partially edentulous patients. Clin. Implant. Dent. Relat. Res. 2012, 14, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Grondahl, K.; Jemt, T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin. Implant. Dent. Relat. Res. 2006, 8, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Ravald, N.; Dahlgren, S.; Teiwik, A.; Grondahl, K. Long-term evaluation of Astra Tech and Branemark implants in patients treated with full-arch bridges. Results after 12–15 years. Clin. Oral Implant. Res. 2013, 24, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23 (Suppl. 6), 22–38. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Pjetursson, B.E.; Glauser, R.; Zembic, A.; Zwahlen, M.; Lang, N.P. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin. Oral Implant. Res. 2008, 19, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, R.; Behnia, H.; Taherian, S.; Hesami, N. What Are the Incidence and Factors Associated With Implant Fracture? J. Oral Maxillofac. Surg. 2017, 75, 1866–1872. [Google Scholar] [CrossRef] [PubMed]
- Balik, A.; Karatas, M.O.; Keskin, H. Effects of different abutment connection designs on the stress distribution around five different implants: A 3-dimensional finite element analysis. J. Oral Implantol. 2012, 38, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.H.; Yoon, H.I.; Kim, T.H.; Park, E.J. Improvement in Fatigue Behavior of Dental Implant Fixtures by Changing Internal Connection Design: An In Vitro Pilot Study. Materials 2019, 12, 3264. [Google Scholar] [CrossRef] [PubMed]
- ISO 14801:2016 (en); Dentistry—Implants—Dynamic Loading Test for Endosseous Dental Implants. ISO: Geneve, Switzerland, 2016.
- Duan, Y.; Griggs, J.A. Effect of loading frequency on cyclic fatigue lifetime of a standard-diameter implant with an internal abutment connection. Dent. Mater. 2018, 34, 1711–1716. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, C.H.; Mahan, P.E.; Mauderli, A.; Lundeen, H.C.; Walsh, E.K. Limits of human bite strength. J. Prosthet. Dent. 1986, 56, 226–229. [Google Scholar] [CrossRef]
- Helkimo, E.; Carlsson, G.; Helkimo, M. Bite forces used during chewing of food. J. Dent. Res. 1959, 29, 133–136. [Google Scholar]
- Richter, E.J. In vivo vertical forces on implants. Int. J. Oral Maxillofac. Implant. 1995, 10, 99–108. [Google Scholar]
- Waltimo, A.; Kononen, M. A novel bite force recorder and maximal isometric bite force values for healthy young adults. Scand. J. Dent. Res. 1993, 101, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.M.; Tsai, C.M.; Chang, C.C.; Lin, C.T.; Lee, S.Y. Evaluation of loading conditions on fatigue-failed implants by fracture surface analysis. Int. J. Oral Maxillofac. Implant. 2005, 20, 854–859. [Google Scholar]
- Bernhard, N.; Berner, S.; De Wild, M.; Wieland, M. The binary TiZr alloy—A newly developed Ti alloy for use in dental implants. Forum Implant. 2020, 22, 30–39. [Google Scholar]
- Watanabe, S.; Nakano, T.; Ono, S.; Yamanishi, Y.; Matsuoka, T.; Ishigaki, S. Fracture Resistance of Zirconia Abutments with or without a Titanium Base: An In Vitro Study for Tapered Conical Connection Implants. Materials 2022, 15, 364. [Google Scholar] [CrossRef] [PubMed]




| Components | Test Group 1 (n = 15) | Test Group 2 (n = 15) | Control Group (n = 15) |
|---|---|---|---|
| Fixture | TORX++ implant 1 | IU implant 2 | BLX implant 3 |
| (4.7 mm × 11 mm) | (4.5 mm × 10 mm) | (4.5 mm × 10 mm) | |
| Abutment | Torx+ design | Internal hex design | Torx design |
| Abutment height: 7 mm | Abutment height: 7 mm | Abutment height: 5.5 mm | |
| Gingival height: 2 mm | Gingival height: 6 mm | Gingival height: 3.5 mm |
| Load at Break (N) | ||||
|---|---|---|---|---|
| Products | First Specimen | Second Specimen | Third Specimen | Mean ± SD |
| BLX | 611.22 | 593.66 | 530.48 | 578.45 ± 42.46 |
| TORX++ | 828.68 | 727.00 | 824.11 | 793.26 ± 57.43 |
| IU | 938.71 | 790.43 | 857.74 | 862.30 ± 74.25 |
| BLX Implant | |||
| Loading Level (%) | Sinusoidal Loading (N) | Number of Cycles Performed | Mean |
| 90 | 520 | 29,278; 78,008; 90,399 | 65,895 |
| 80 | 462 | 217,424; 501,002; 5,000,000 | 1,906,142 |
| 70 | 405 * | 5,000,000; 5,000,000; 5,000,000 | 5,000,000 |
| 60 | 347 | 5,000,000; 5,000,000; 5,000,000 | 5,000,000 |
| 50 | 289 | 5,000,000; 5,000,000; 5,000,000 | 5,000,000 |
| TORX++ Implant | |||
| Loading Level (%) | Sinusoidal Loading (N) | Number of Cycles Performed | Mean |
| 90 | 714 | 8745; 22,108; 6544 | 12,466 |
| 80 | 634 | 28,593; 42,415; 16,995 | 29,334 |
| 70 | 555 | 39,319; 25,529; 23,329 | 29,392 |
| 60 | 476 | 403,005; 227,229; 312,357 | 314,197 |
| 50 | 397 * | 5,000,000; 5,000,000; 5,000,000 | 5,000,000 |
| IU Implant | |||
| Loading Level (%) | Sinusoidal Loading (N) | Number of Cycles Performed | Mean |
| 90 | 776 | 219,622; 100,262; 8652 | 109,512 |
| 80 | 690 | 52,514; 34,935; 660,358 | 249,269 |
| 70 | 603 | 2,508,358; 114,156; 587,202 | 1,069,905 |
| 60 | 517 | 1,252,553; 5,000,000; 5,000,000 | 3,750,851 |
| 50 | 431 * | 5,000,000; 5,000,000; 5,000,000 | 5,000,000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
On, S.-W.; Yi, S.-M.; Park, I.-Y.; Byun, S.-H.; Yang, B.-E. Fracture and Fatigue of Dental Implants Fixtures and Abutments with a Novel Internal Connection Design: An In Vitro Pilot Study Comparing Three Different Dental Implant Systems. J. Funct. Biomater. 2022, 13, 239. https://doi.org/10.3390/jfb13040239
On S-W, Yi S-M, Park I-Y, Byun S-H, Yang B-E. Fracture and Fatigue of Dental Implants Fixtures and Abutments with a Novel Internal Connection Design: An In Vitro Pilot Study Comparing Three Different Dental Implant Systems. Journal of Functional Biomaterials. 2022; 13(4):239. https://doi.org/10.3390/jfb13040239
Chicago/Turabian StyleOn, Sung-Woon, Sang-Min Yi, In-Young Park, Soo-Hwan Byun, and Byoung-Eun Yang. 2022. "Fracture and Fatigue of Dental Implants Fixtures and Abutments with a Novel Internal Connection Design: An In Vitro Pilot Study Comparing Three Different Dental Implant Systems" Journal of Functional Biomaterials 13, no. 4: 239. https://doi.org/10.3390/jfb13040239
APA StyleOn, S.-W., Yi, S.-M., Park, I.-Y., Byun, S.-H., & Yang, B.-E. (2022). Fracture and Fatigue of Dental Implants Fixtures and Abutments with a Novel Internal Connection Design: An In Vitro Pilot Study Comparing Three Different Dental Implant Systems. Journal of Functional Biomaterials, 13(4), 239. https://doi.org/10.3390/jfb13040239









