The Effect of Acrylic Surface Preparation on Bonding Denture Teeth to Cellulose Fiber-Reinforced Denture Base Acrylic †
Abstract
1. Introduction
- Procedures enabling the creation of new chains and/or increasing the over-etching of the tooth’s structure (e.g., through using isobutyl methacrylate [9], dichloromethane [10], MMA [9,11], etc.), ready-made mixes sold as “glues” [9,12,13,14,15]), or rubbing the tooth structure with a selected chemical reagent;
- A combination of the two above methods (which is even suggested by manufacturers [15]).
- The patient is missing two or more teeth;
- The force exerted on the tooth acts along the axis of the tooth (such forces are present in the case of premolars and molars);
- The surface of contact between the artificial tooth and the dental base is quite large (again, such surfaces are present in the case of premolars and molars);
- The teeth can be more deeply embedded into the dental plate (possibly in complete acrylic dentures).
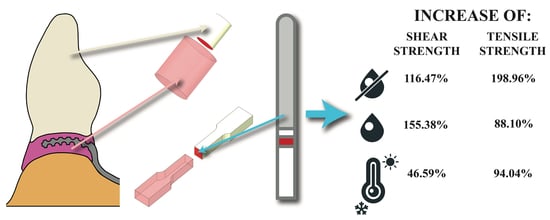
2. Materials and Methods
- No impact (group D);
3. Results
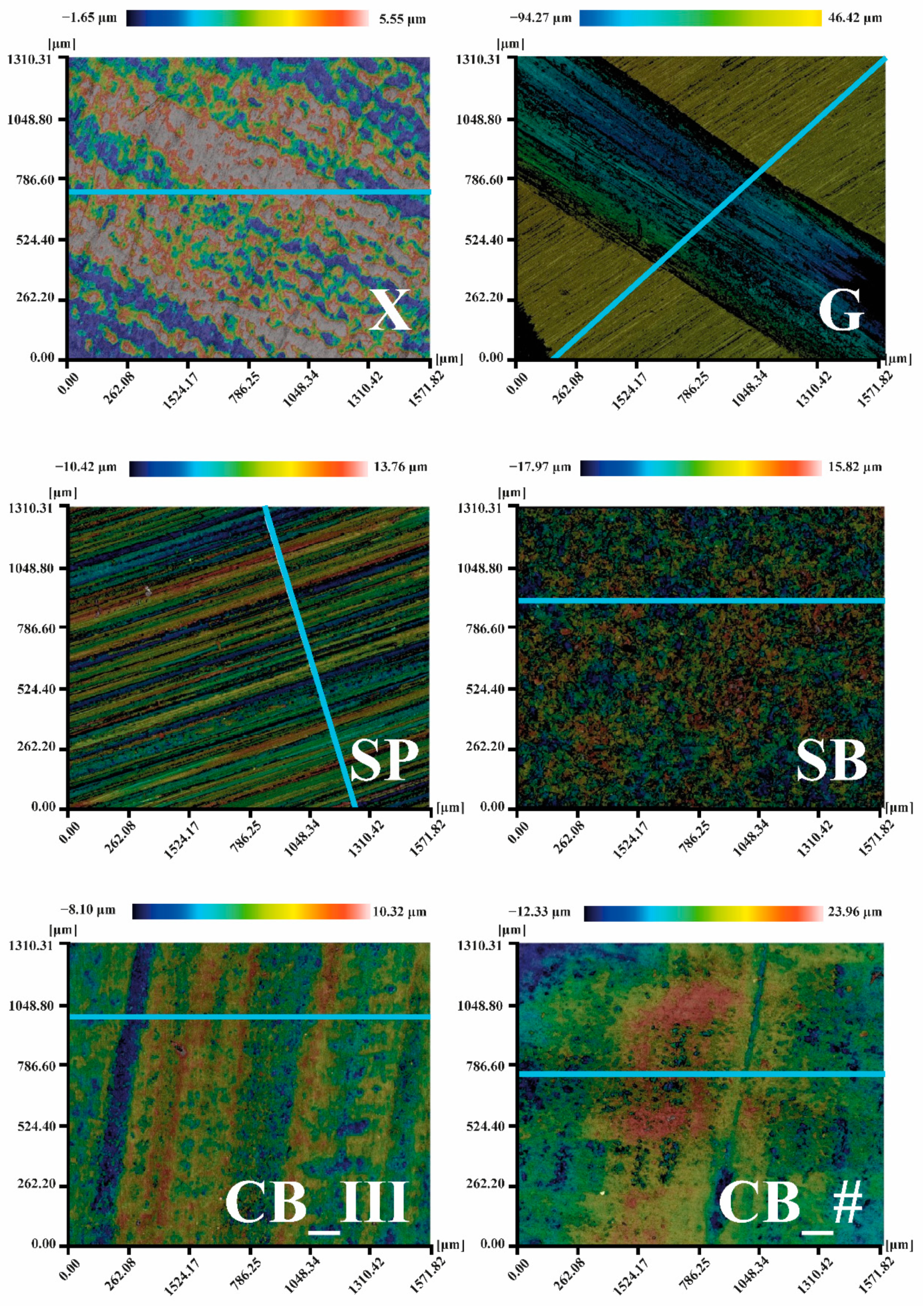
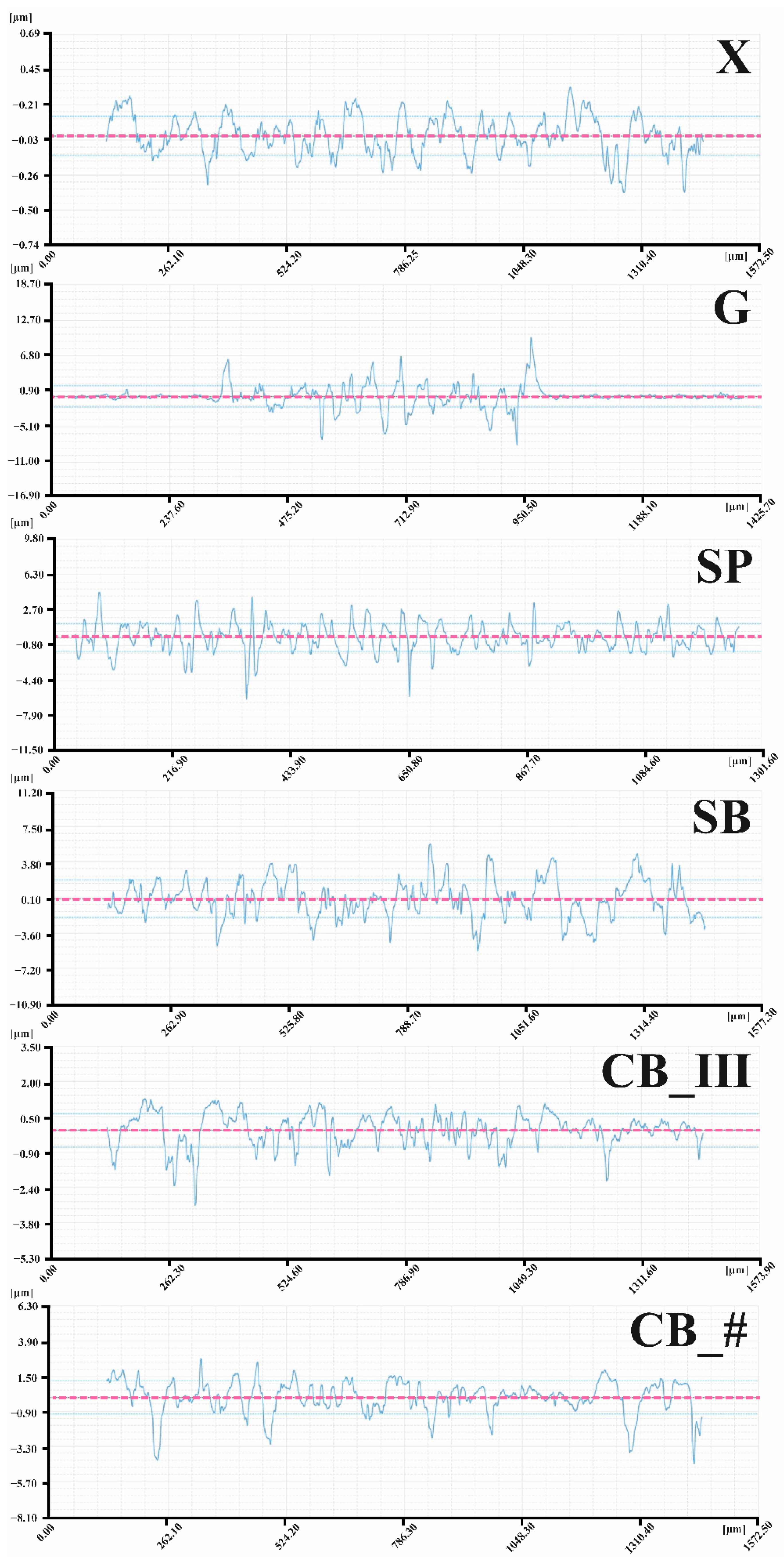
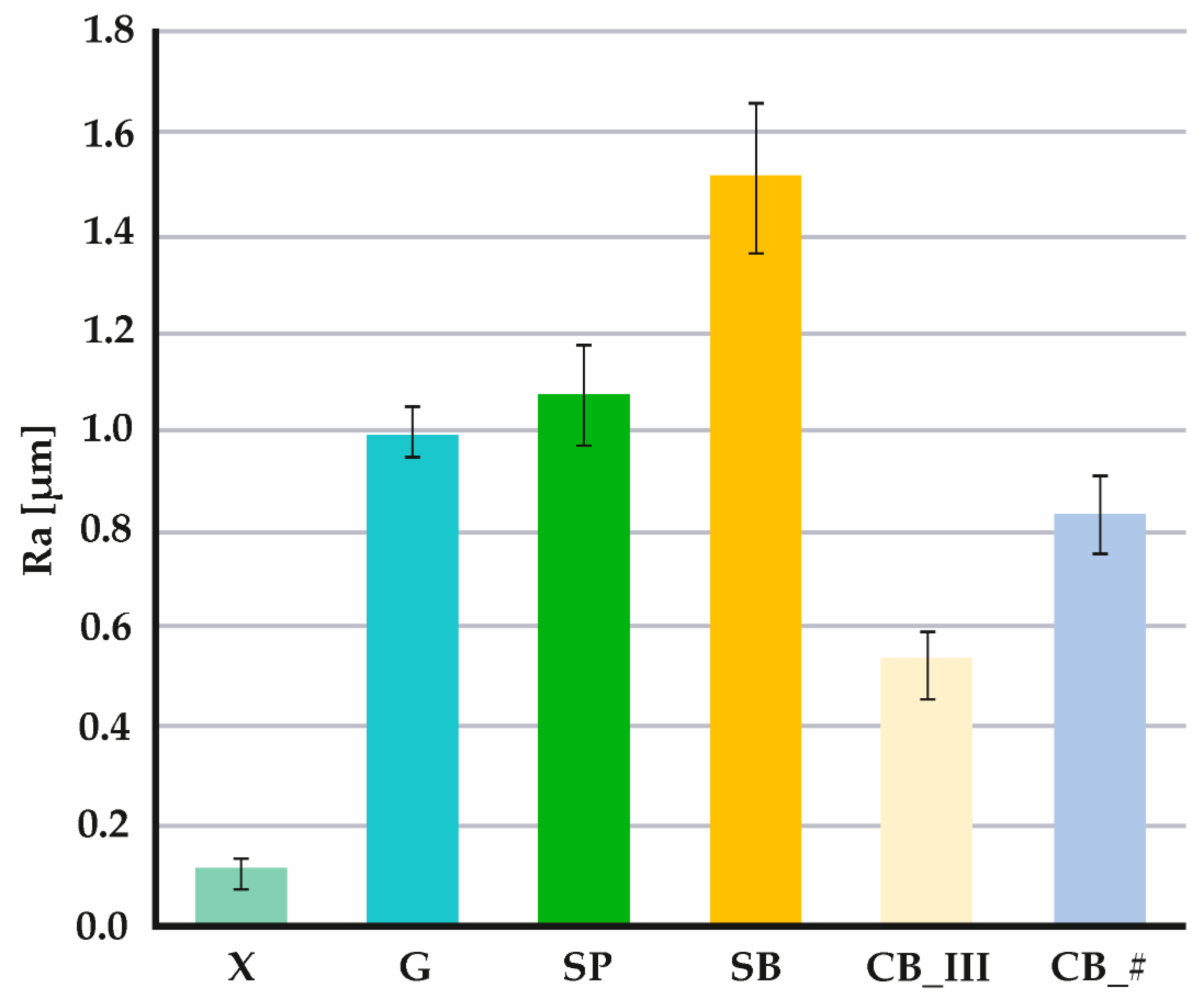
3.1. 3D Microscope Observations by Profilometer
- X—Sa 0.26 μm, Sq 0.33 μm;
- G—Sa 42.84 μm, Sq 45.39 μm;
- SP—Sa 2.17 μm, Sq 2.72 μm;
- SB—Sa 2.86 μm, Sq 3.60 μm;
- CB_III—Sa 0.79 μm, Sq 1.04 μm;
- CB_#—Sa 1.54 μm, Sq 1.99 μm.
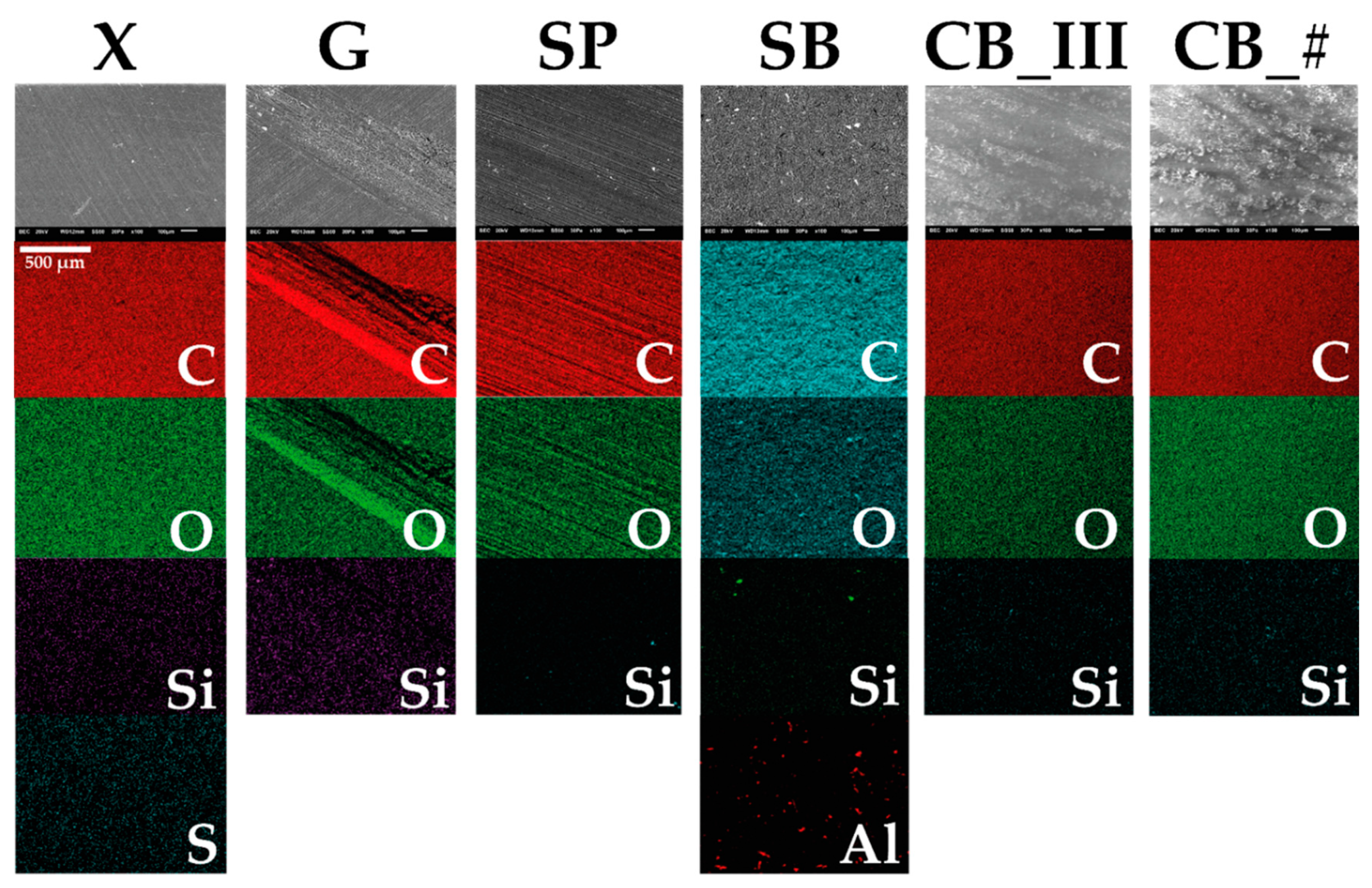
3.2. EDS
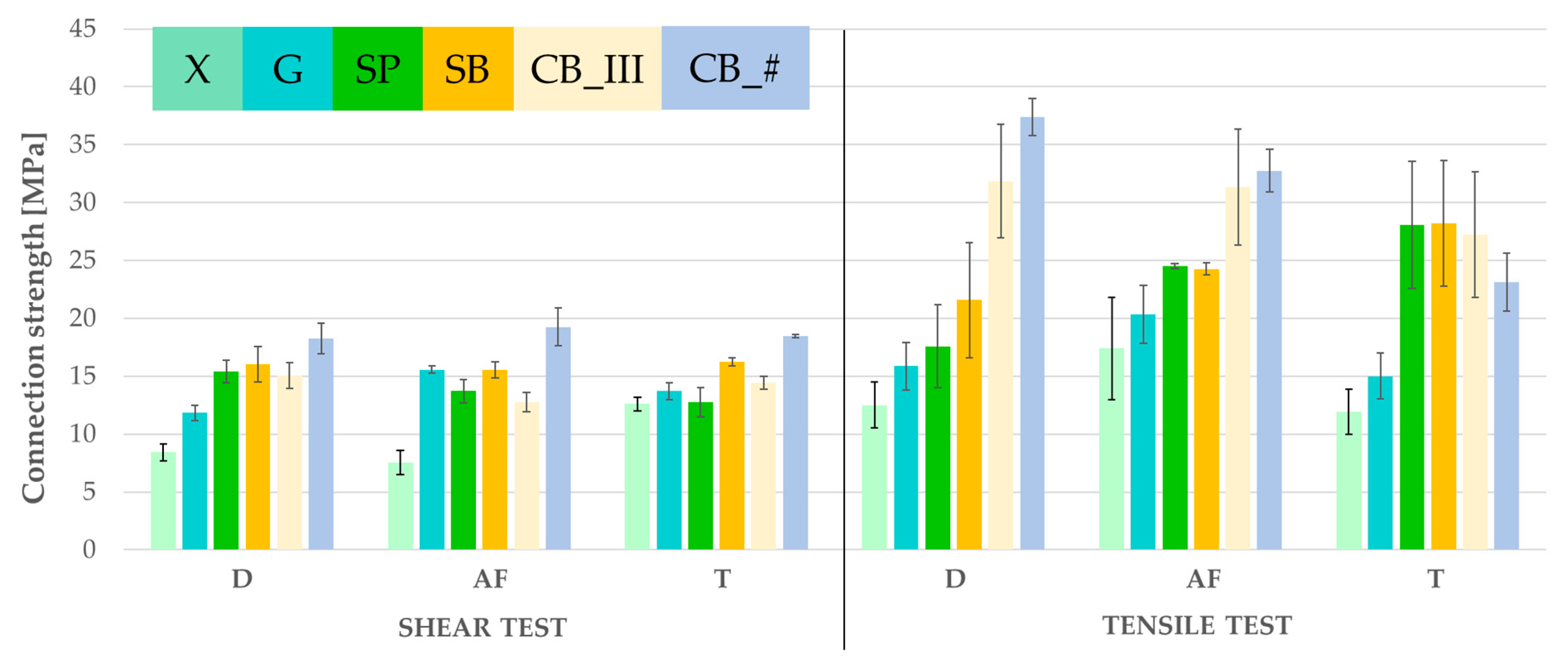
3.3. Strength Tests
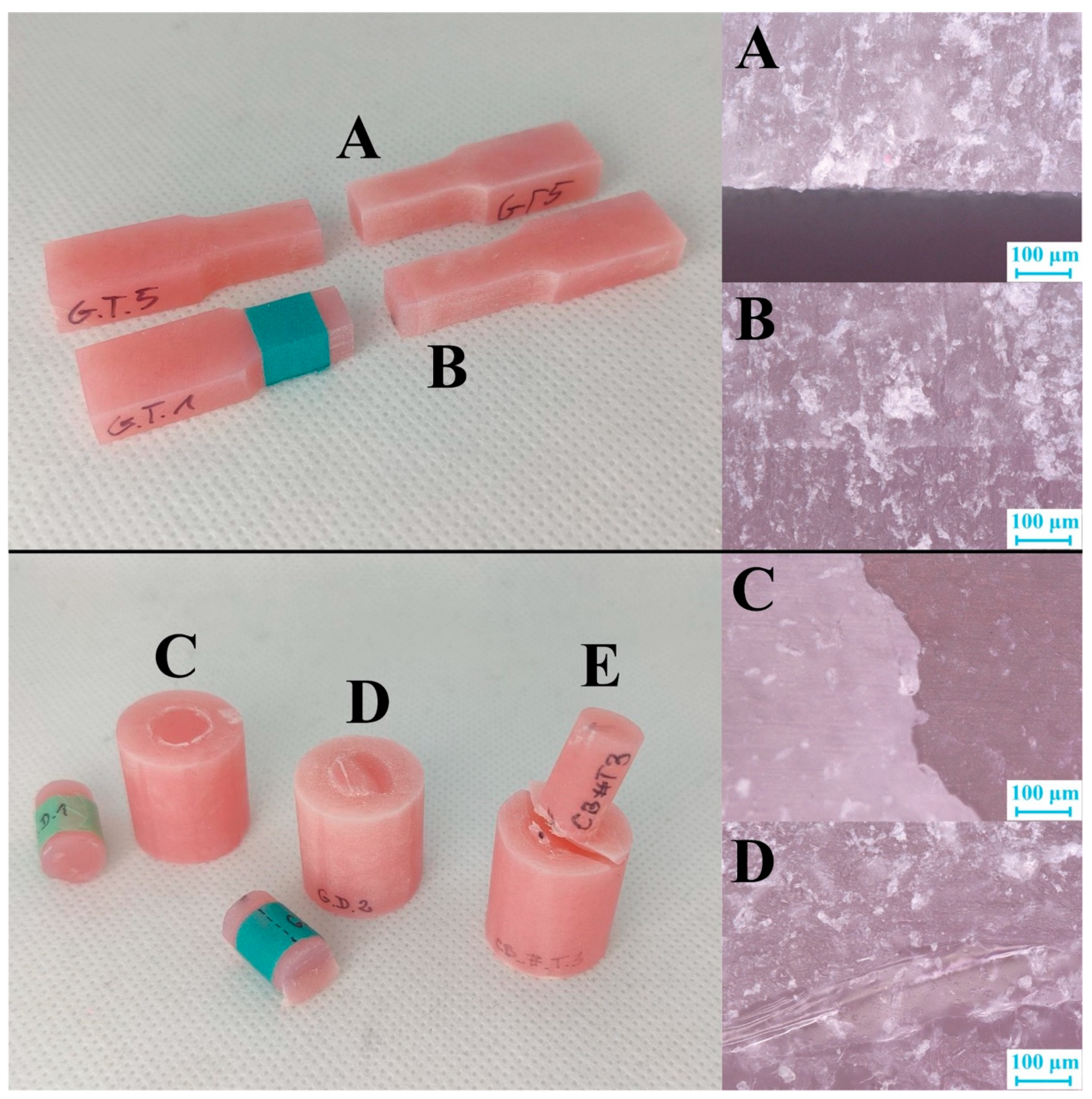
3.4. Observation of Fissures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Surface Preparation | Environment | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
| 1 | X | D | 1.00 | 0.64 | 0.95 | 0.01 | 0.20 | 0.04 | 0.71 | 0.60 | 0.01 | 0.01 | 0.00 | 0.03 | 0.20 | 0.03 | 0.00 | 0.00 | 0.00 | |
| 2 | X | AF | 1.00 | 0.26 | 0.66 | 0.00 | 0.05 | 0.01 | 0.31 | 0.23 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.01 | 0.00 | 0.00 | 0.00 | |
| 3 | X | T | 0.64 | 0.26 | 1.00 | 0.87 | 1.00 | 1.00 | 1.00 | 1.00 | 0.94 | 0.91 | 0.79 | 0.99 | 1.00 | 0.99 | 0.17 | 0.01 | 0.05 | |
| 4 | G | D | 0.95 | 0.66 | 1.00 | 0.49 | 1.00 | 0.88 | 1.00 | 1.00 | 0.63 | 0.55 | 0.38 | 0.81 | 1.00 | 0.85 | 0.04 | 0.00 | 0.01 | |
| 5 | G | AF | 0.01 | 0.00 | 0.87 | 0.49 | 1.00 | 1.00 | 0.83 | 0.90 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.73 | 0.97 | |
| 6 | G | T | 0.20 | 0.05 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 1.00 | 0.60 | 0.07 | 0.28 | |
| 7 | SP | D | 0.04 | 0.01 | 1.00 | 0.88 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.94 | 0.32 | 0.71 | |
| 8 | SP | AF | 0.71 | 0.31 | 1.00 | 1.00 | 0.83 | 1.00 | 0.99 | 1.00 | 0.91 | 0.87 | 0.74 | 0.98 | 1.00 | 0.99 | 0.14 | 0.01 | 0.04 | |
| 9 | SP | T | 0.60 | 0.23 | 1.00 | 1.00 | 0.90 | 1.00 | 1.00 | 1.00 | 0.96 | 0.93 | 0.83 | 0.99 | 1.00 | 1.00 | 0.20 | 0.01 | 0.06 | |
| 10 | SB | D | 0.01 | 0.00 | 0.94 | 0.63 | 1.00 | 1.00 | 1.00 | 0.91 | 0.96 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.60 | 0.93 | |
| 11 | SB | AF | 0.01 | 0.00 | 0.91 | 0.55 | 1.00 | 1.00 | 1.00 | 0.87 | 0.93 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.68 | 0.96 | |
| 12 | SB | T | 0.00 | 0.00 | 0.79 | 0.38 | 1.00 | 0.99 | 1.00 | 0.74 | 0.83 | 1.00 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 0.83 | 0.99 | |
| 13 | CB_III | D | 0.03 | 0.00 | 0.99 | 0.81 | 1.00 | 1.00 | 1.00 | 0.98 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.97 | 0.41 | 0.80 | |
| 14 | CB_III | AF | 0.20 | 0.05 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 0.60 | 0.07 | 0.28 | |
| 15 | CB_III | T | 0.03 | 0.01 | 0.99 | 0.85 | 1.00 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.96 | 0.36 | 0.76 | |
| 16 | CB_# | D | 0.00 | 0.00 | 0.17 | 0.04 | 1.00 | 0.60 | 0.94 | 0.14 | 0.20 | 1.00 | 1.00 | 1.00 | 0.97 | 0.60 | 0.96 | 1.00 | 1.00 | |
| 17 | CB_# | AF | 0.00 | 0.00 | 0.01 | 0.00 | 0.73 | 0.07 | 0.32 | 0.01 | 0.01 | 0.60 | 0.68 | 0.83 | 0.41 | 0.07 | 0.36 | 1.00 | 1.00 | |
| 18 | CB_# | T | 0.00 | 0.00 | 0.05 | 0.01 | 0.97 | 0.28 | 0.71 | 0.04 | 0.06 | 0.93 | 0.96 | 0.99 | 0.80 | 0.28 | 0.76 | 1.00 | 1.00 |
| Surface Preparation | Environment | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
| 1 | X | D | 1.00 | 1.00 | 1.00 | 0.95 | 1.00 | 1.00 | 0.62 | 0.37 | 0.95 | 0.80 | 0.16 | 0.01 | 0.10 | 0.36 | 0.00 | 0.04 | 0.63 | |
| 2 | X | AF | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.98 | 1.00 | 1.00 | 0.86 | 0.28 | 0.75 | 0.98 | 0.03 | 0.49 | 1.00 | |
| 3 | X | T | 1.00 | 1.00 | 1.00 | 0.92 | 1.00 | 1.00 | 0.57 | 0.32 | 0.93 | 0.75 | 0.13 | 0.01 | 0.08 | 0.31 | 0.00 | 0.03 | 0.57 | |
| 4 | G | D | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.95 | 0.79 | 1.00 | 0.99 | 0.51 | 0.08 | 0.38 | 0.79 | 0.00 | 0.18 | 0.95 | |
| 5 | G | AF | 0.95 | 1.00 | 0.92 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.99 | 0.67 | 0.98 | 1.00 | 0.13 | 0.87 | 1.00 | |
| 6 | G | T | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.97 | 1.00 | 1.00 | 0.84 | 0.25 | 0.72 | 0.97 | 0.02 | 0.45 | 1.00 | |
| 7 | SP | D | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 0.89 | 0.31 | 0.79 | 0.99 | 0.03 | 0.53 | 1.00 | |
| 8 | SP | AF | 0.62 | 1.00 | 0.57 | 0.95 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.96 | 1.00 | 1.00 | 0.44 | 1.00 | 1.00 | |
| 9 | SP | T | 0.37 | 0.98 | 0.32 | 0.79 | 1.00 | 0.97 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.71 | 1.00 | 1.00 | |
| 10 | SB | D | 0.95 | 1.00 | 0.93 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.99 | 0.65 | 0.97 | 1.00 | 0.12 | 0.85 | 1.00 | |
| 11 | SB | AF | 0.80 | 1.00 | 0.75 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.88 | 1.00 | 1.00 | 0.28 | 0.97 | 1.00 | |
| 12 | SB | T | 0.16 | 0.86 | 0.13 | 0.51 | 0.99 | 0.84 | 0.89 | 1.00 | 1.00 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 0.92 | 1.00 | 1.00 | |
| 13 | CB_III | D | 0.01 | 0.28 | 0.01 | 0.08 | 0.67 | 0.25 | 0.31 | 0.96 | 1.00 | 0.65 | 0.88 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.96 | |
| 14 | CB_III | AF | 0.10 | 0.75 | 0.08 | 0.38 | 0.98 | 0.72 | 0.79 | 1.00 | 1.00 | 0.97 | 1.00 | 1.00 | 1.00 | 1.00 | 0.97 | 1.00 | 1.00 | |
| 15 | CB_III | T | 0.36 | 0.98 | 0.31 | 0.79 | 1.00 | 0.97 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.71 | 1.00 | 1.00 | |
| 16 | CB_# | D | 0.00 | 0.03 | 0.00 | 0.00 | 0.13 | 0.02 | 0.03 | 0.44 | 0.71 | 0.12 | 0.28 | 0.92 | 1.00 | 0.97 | 0.71 | 1.00 | 0.44 | |
| 17 | CB_# | AF | 0.04 | 0.49 | 0.03 | 0.18 | 0.87 | 0.45 | 0.53 | 1.00 | 1.00 | 0.85 | 0.97 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 18 | CB_# | T | 0.63 | 1.00 | 0.57 | 0.95 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.96 | 1.00 | 1.00 | 0.44 | 1.00 |
References
- Powers, M.J.; Wataha, C.J. Dental Materials: Properties and Manipulation, 10th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Raszewski, Z. A New View at Acrylic Materials; Elamed: Łódź, Poland, 2009. [Google Scholar]
- Dejak, B. Compendium of Making Prosthetic Restorations; Med Tour Press International: Otwock, Poland, 2014. [Google Scholar]
- Taczała, J.; Sawicki, J. Bond between single artificial teeth and the base plate in removable denture metal framework. J. Achiev. Mater. Manuf. Eng. 2018, 1, 11–21. [Google Scholar] [CrossRef]
- Carr, A.; David, B. McCracken’s Removable Partial Prosthodontics, 13th ed.; Mosby: Maryland Heights, MO, USA, 2015. [Google Scholar]
- Taczała, J. Influence of the inhibitor on the properties of dental acrylic resin. In The Book of Articles National Scientific Conference “Knowledge—Key to Success, 4th ed.; Promovendi Foundation Publishing: Łódź, Poland, 2020; pp. 120–128. [Google Scholar]
- Raszewski, Z. Mechanical properties of hot curing acrylic resins after reinforced with different kinds of fibers. Int. J. Biomed. Mater. Res. 2013, 1, 9–13. [Google Scholar] [CrossRef]
- Majewski, S.W.; Pryliński, M. Materials and Technologies of Contemporary Dental Prosthetics: A Textbook for Dentistry Students, Doctors and Dental Technicians; Czelej: Lublin, Polonia, 2013. [Google Scholar]
- Akin, H.; Kirmali, O.; Tugut, F.; Coskun, M.E. Effects of different surface treatments on the bond strength of acrylic denture teeth to polymethylmethacrylate denture base material. Photomed. Laser Surg. 2014, 32, 512–516. [Google Scholar] [CrossRef]
- Jain, G.; Palekar, U.; Awinashe, V.; Mishra, S.K.; Kawadkar, A.; Rahangdale, T. The effect of different chemical surface treatments of denture teeth on shear bond strength: A comparative study. J. Clin. Diagn. Res. 2014, 8, 15–19. [Google Scholar] [CrossRef]
- Muñoz, M.; Reales, E.; Prates, L.; Volpato, C. Bond strength assessment between acrylic teeth and acrylic resin repairs: Effect of different surface treatments. Odovtos-Int. J. Dent. Sci. 2016, 18, 109–124. [Google Scholar] [CrossRef][Green Version]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond strength of denture teeth to heat-cured, CAD/CAM and 3D printed denture acrylics. J. Prosthodont. 2019, 29, 415–421. [Google Scholar] [CrossRef]
- Akin, H.; Tugut, F.; Guney, U.; Akar, T. Shear bond strength of denture teeth to two chemically different denture base resins after various surface treatments. J. Prosthodont. 2014, 23, 152–156. [Google Scholar] [CrossRef]
- Jayakrishnakumar, S.; Ramakrishnan, H.; Divagar, C.; Mahadevan, V.; Azhagarasan, N. Comparative evaluation of the effect of surface treatments on theshearbond strength between acrylic denture teeth and denture base resin—Three dimensional study. IOSR J. Dent. Med. Sci. 2019, 18, 29–45. [Google Scholar] [CrossRef][Green Version]
- Schütz Dental GmbH, FuturAcryl 2000, RosbacH. Available online: https://www.schuetz-dental.de/media/pdf/60/3a/0f/Product_Catalog_English.pdf (accessed on 9 September 2022).
- Taczała, J. Influence of the groove on stress distribution and deformations in the case of a single incisor in removable partial denture metal framework. In The Book of Articles National Scientific Conference “Zrozumieć Naukę”, 2nd ed.; Promovendi Foundation Publishing: Łódź, Poland, 2018; pp. 238–248. [Google Scholar]
- Taczała, J.; Krupanek, K.; Sawicki, J. Numerical analysis of the influence of surface modification on the bond strength between a single incisal tooth with a removable partial denture metal framework. AIP Conf. Proc. 2019, 2078, 020057. [Google Scholar] [CrossRef]
- Phukela, S.S.; Chintalapudi, S.K.; Sachdeva, H.; Dhall, R.S.; Sharma, N.; Prabhu, A. Comparative evaluation of different mechanical modifications of denture teeth on bond strength between high-impact acrylic resin and denture teeth: An in vitro study. J. Int. Soc. Prev. Community Dent. 2016, 6, 161–166. [Google Scholar] [CrossRef]
- Consani, R.L.; Naoe, H.T.; Mesquita, M.F.; Sinhoreti, A.M.; Mendes, W.B. Effect of ridge-lap surface treatments on the bond of resin teeth to denture base. J. Adhes. Dent. 2011, 13, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.B.; Naveen, B.H.; Patil, N.P. Bonding acrylic teeth to acrylic resin denture bases: A review. Gerodontology 2006, 23, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Colebeck, A.C.; Monaco, E.A.; Pusateri, C.R.; Davis, E. Microtensile bond strength of different acrylic teeth to high-impact denture base resins. J. Prosthodont. 2015, 24, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Meloto, C.; Silva-Concílio, L.; Rodrigues-Garciai, R.; Canales, G.; Rizzatti-Barbosa, C. Effect of surface treatments on the bond strength of different resin teeth to complete denture base material. Acta Odontol. Lat. 2013, 26, 37–42. [Google Scholar]
- Chung, K.-H.; Chung, C.Y.; Chan, D.C.N. Effect of pre-processing surface treatments of acrylic teeth on bonding to the denture base. J. Oral Rehabil. 2008, 35, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, G.; Neisser, M.P.; Sinhoreti, M.A.C.; Machado, C. Evaluation of bond strength of denture teeth bonded to heat polymerized acrylic resin denture bases. Brazilian J. Oral Sci. 2004, 3, 458–464. [Google Scholar] [CrossRef]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture: A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Taczała, J.; Sawicki, J.; Pietrasik, J. Chemical modification of cellulose microfibres to reinforce poly(methyl methacrylate) used for dental application. Materials 2020, 13, 3807. [Google Scholar] [CrossRef]
- Alzarrug, F.A.; Dimitrijević, M.M.; Heinemann, R.M.J.; Radojević, V.; Stojanović, D.B.; Uskoković, P.S.; Aleksić, R. The use of different alumina fillers for improvement of the mechanical properties of hybrid PMMA composites. Mater. Des. 2015, 86, 575–581. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef] [PubMed]
- Marin, E.; Boschetto, F.; Zanocco, M.; Honma, T.; Zhu, W.; Pezzotti, G. Explorative study on the antibacterial effects of 3D-printed PMMA/nitrides composites. Mater. Des. 2021, 206, 109788. [Google Scholar] [CrossRef]
- Chladek, G.; Żmudzki, J.; Basa, K.; Pater, A.; Krawczyk, C.; Pakieła, W. Effect of silica filler on properties of PMMA resin. Arch. Mater. Sci. Eng. 2015, 71, 63–72. [Google Scholar]
- Alhotan, A.; Yates, J.; Zidan, S.; Haider, J.; Silikas, N. Flexural strength and hardness of filler-reinforced PMMA targeted for denture base application. Materials 2021, 14, 2659. [Google Scholar] [CrossRef] [PubMed]
- Taczała, J.; Fu, C.; Sawicki, J.; Pietrasik, J. Influence different amount of cellulose on the mechanical strength of dental acrylic resin. IOP Conf. Ser. Mater. Sci. Eng. 2019, 743, 012044. [Google Scholar] [CrossRef]
- Kato, H.; Matsumura, H.; Atsuta, M. Effect of etching and sandblasting on bond strength to sintered porcelain of unfilled resin. J. Oral Rehabil. 2000, 27, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Czepułkowska, W.; Klimek, L. Comparison of surface roughness of Ni-Cr alloy after abrasive blasting using Al2O3 and SiC. In The Book of Articles—National Scientific Conference “ Knowledge-Key to Success 2019”, 3rd ed.; Promovendi Foundation Publishing: Łódź, Poland, 2019; pp. 1–8. [Google Scholar]
- Czepułkowska, W.; Klimek, L. The role of mechanical, chemical and physical bonds in metal-ceramic bond strength. Arch. Mater. Sci. Eng. 2018, 92, 5–14. [Google Scholar] [CrossRef]
- Golebiowski, M.; Wolowiec, E.; Klimek, L. Airborne-particle abrasion parameters on the quality of titanium-ceramic bonds. J. Prosthet. Dent. 2015, 113, 453–459. [Google Scholar] [CrossRef]
- Schneider, R.L.; Curtis, E.R.; Clancy, J.M. Tensile bond strength of acrylic resin denture teeth to a microwave- or heat-processed denture base. J. Prosthet. Dent. 2002, 88, 145–150. [Google Scholar] [CrossRef]
- Neppelenbroek, K.H.; Kuroishi, E.; Hotta, J.; Marques, V.R.; Moffa, E.B.; Soares, S.; Urban, V.M. Urban, Surface properties of multilayered, acrylic resin artificial teeth after immersion in staining beverages. J. Appl. Oral Sci. 2015, 23, 376–382. [Google Scholar] [CrossRef]
- Serra, G.; De Morais, L.S.; Elias, C.N. Surface morphology changes of acrylic resins during finishing and polishing phases. Dent. Press J. Orthod. 2013, 18, 26–30. [Google Scholar] [CrossRef][Green Version]
- Al-Kheraif, A.A.A. The effect of mechanical and chemical polishing techniques on the surface roughness of heat-polymerized and visible light-polymerized acrylic denture base resins. Saudi Dent. J. 2014, 26, 56–62. [Google Scholar] [CrossRef]
- Taczała, J.; Rak, K.; Sawicki, J.; Krasowski, M. Numerical analysis of the bond strength between two methacrylic polymers by surface modification. Materials 2021, 14, 3927. [Google Scholar] [CrossRef]
- Marra, J.; de Souza, R.; Barbosa, D.B.; Pero, A.; Compagnoni, M.A. Evaluation of the bond strength of denture base resins to acrylic resin teeth: Effect of thermocycling. J. Prosthodont. 2009, 18, 438–443. [Google Scholar] [CrossRef]
- Barbosa, D.B.; Barao, V.A.R.; Monteiro, D.; Compagnoni, M.A.; Marra, J. Bond strength of denture teeth to acrylic resin: Effect of thermocycling and polymerisation methods. Gerodontology 2008, 25, 237–244. [Google Scholar] [CrossRef]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Sokolowski, J.; Kleczewska, J.; Bociong, K. Ageing of dental composites based on methacrylate resins-A critical review of the causes and method of assessment. Polymers 2020, 12, 882. [Google Scholar] [CrossRef]
- Rupp, N.; Bowen, R.; Paffenbarger, G. Bonding cold-curing denture base acrylic resin to acrylic resin reeth. J. Am. Dent. Assoc. 1971, 83, 601–606. [Google Scholar] [CrossRef]
- Barpal, D.; Curtis, D.A.; Finzen, F.; Perry, J.; Gansky, S.A. Failure load of acrylic resin denture teeth bonded to high impact acrylic resins. J. Prosthet. Dent. 1998, 80, 666–671. [Google Scholar] [CrossRef]
- Patel, B.; Duran-Martinez, A.C.; Gurman, P.; Auciello, O.; Barao, V.; Campbell, S.; Sukotjo, C.; Mathew, M.T. Ultrananocrystalline diamond coatings for the dental implant: Electrochemical nature. Surf. Innov. 2017, 5, 106–117. [Google Scholar] [CrossRef]
- Chaturvedi, G.; Pawar, R. Effect of fluoride on nickel-titanium and stainless steel orthodontic archwires: An in-vitro study. J. Crit. Rev. 2020, 7, 781–785. [Google Scholar] [CrossRef]
- Fusayama/Meyer Artificial Saliva; MSDS 1700-0301; Pickering Laboratories: Mountain View, CA, USA, 25 June 2015.
- Fallahi, A.; Khadivi, N.; Roohpour, N.; Middleton, A.M.; Kazemzadeh-Narbat, M.; Annabi, N.; Khademhosseini, A.; Tamayol, A. Characterization, mechanistic analysis and improving the properties of denture adhesives. Dent. Mater. 2019, 34, 120–131. [Google Scholar] [CrossRef]
- Pytko-Polonczyk, J.J.; Jakubik, A.; Przeklasa-Bierowiec, A.; Muszynska, B. Artificial saliva and its use in biological experiments. J. Physiol. Pharmacol. 2017, 68, 807–813. [Google Scholar]
- Grzesik, W. Effect of the machine parts surface topography features on the machine service. Mechanik 2015, 88, 587–593. [Google Scholar] [CrossRef]
- Kłonica, M. The use of statistical elements in the research process on the example of measurements of selected parameters of surface roughness. Konferencja Przemysł 4.0 a Zarządzanie i Inżynieria Produkcji 2017, 1, 1–11. [Google Scholar]
- Dziubek, T.; Filip, M. Analysis and comparison of the accuracy of selected incremental manufacturing methods. Mechanik 2015, 12, 54–61. [Google Scholar] [CrossRef]
- Al-Rifaiy, M.Q. The effect of mechanical and chemical polishing techniques on the surface roughness of denture base acrylic resins. Saudi Dent. J. 2010, 22, 13–17. [Google Scholar] [CrossRef]
- Silesia Dental. Frezy. Available online: https://silesiadental.pl/produkty/protetyka-tradycyjna/produkty-do-obrobki/frezy/frezy/ (accessed on 1 September 2022).
- Acosta-Torres, L.S.; Barceló-Santana, F.H.; Álvarez-Gayosso, C.A.; Reyes-Gasga, J. Synthesis and characterization of poly (methyl methacrylate) polymerized by microwave energy or conventional water bath. J. Appl. Polym. Sci. 2008, 109, 3953–3960. [Google Scholar] [CrossRef]
- Okulus, Z. Preparation and Characterization of Dental Composite Materials; Poznan University of Technology: Poznań, Poland, 2016. [Google Scholar]
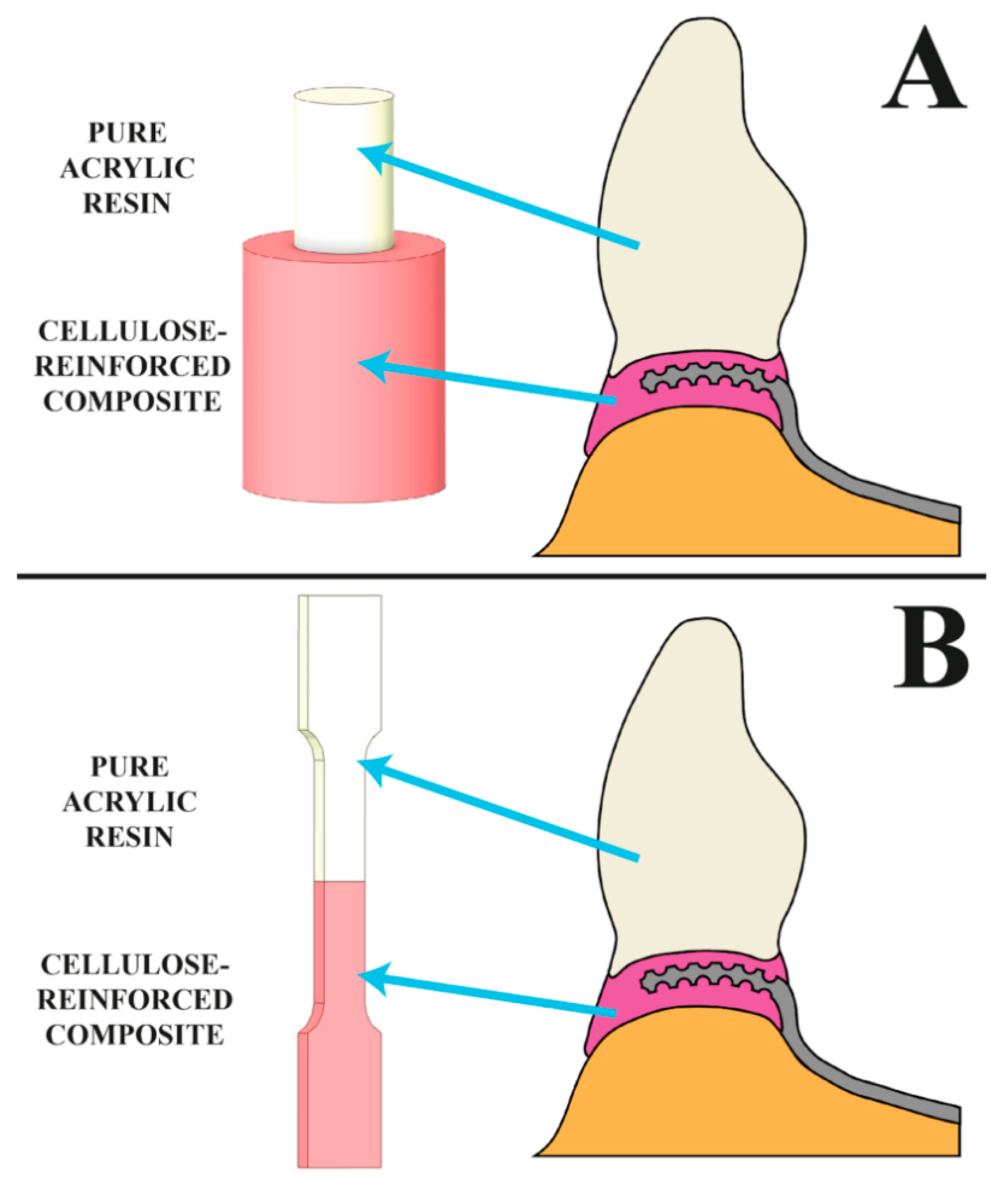



| Preparation of Surface | Symbol of the Group | Parameters |
|---|---|---|
| Without modification | X | - |
| Grooving | G | Width 0.20 mm, thickness 0.10 mm, the distance between the grooves 5.00 mm, force placed at an angle of 90°, speed 30,000 RPM. |
| Sandpaper | SP | Surface roughness by SiC (silicon carbide/carborundum) sandpaper with the gradation of 180 µm. |
| Sandblasting | SB | Sandblasting by Al2O3 with 110 µm particle size, at the 45°, the distance from the nozzle 15 mm and 0.4 MPa. |
| Carbide bur-parallel | CB_III | Carbide bur used in dental techniques with the same shape on whole geometry, red color, no. F93, L 16.0 mm, ⌀ 023 mm. Surface roughened in one direction. |
| Carbide bur-cross | CB_# | Carbide bur used in dental techniques with the same shape on whole geometry, red color, no. F93, L 16.0mm, ⌀ 023mm. Surface roughened in two directions. |
| Preparation of Surface | Environmental Impact | ||
|---|---|---|---|
| D—Dry (No Environmental Impact) | AF—Artificial Saliva | T—Thermocycling | |
| X—control specimen, no modifications | X.D, 5 x shear test X.D, 5 x tensile test | X.AF, 5 x shear test X.AF, 5 x tensile test | X.T, 5 x shear test X.T, 5 x tensile test |
| G—grooves | G.D, 5 x shear test G.D, 5 x tensile test | G.AF, 5 x shear test G.AF, 5 x tensile test | G.T, 5 x shear test G.T, 5 x tensile test |
| SP—sandpaper | SP.D, 5 x shear test SP.D, 5 x tensile test | SP.AF, 5 x shear test SP.AF, 5 x tensile test | SP.T, 5 x shear test SP.T, 5 x tensile test |
| SB—sandblasting | SB.D, 5 x shear test SB.D, 5 x tensile test | SB.AF, 5 x shear test SB.AF, 5 x tensile test | SB.T, 5 x shear test SB.T, 5 x tensile test |
| CB_III—preparation with carbide bur in one direction | CB_III.D, 5 x shear test CB_III.D, 5 x tensile test | CB_III.AF, 5 x shear test CB_III.AF, 5 x tensile test | CB_III.T, 5 x shear test CB_III.T, 5 x tensile test |
| CB_#—preparation with carbide bur in two directions | CB_#.D, 5 x shear test CB_#.D, 5 x tensile test | CB_#.AF, 5 x shear test CB_#.AF, 5 x tensile test | CB_III.T, 5 x shear test CB_III.T, 5 x tensile test |
| Composition | CAS No | Concentration (g/L) |
|---|---|---|
| Potassium chloride (KCl) | 7447-40-7 | 0.400 |
| Sodium chloride (NaCl) | 7647-14-5 | 0.400 |
| Calcium chloride dihydrate (CaCl2·2H2O) | 10035-04-8 | 0.906 |
| Monosodium phosphate dihydrate (NaH2PO4·2H2O) | 13472-35-0 | 0.690 |
| Sodium sulfide nonahydrate (Na2S·9H2O) | 1313-84-4 | 0.005 |
| Urea (CH2N2O) | 57-13-6 | 1.0 |
| Preparation of Surface | Shear Test [MPa] | Tensile Test [MPa] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D | AF | T | D | AF | T | |||||||
| a.s. | s.d. | a.s. | s.d. | a.s. | s.d. | a.s. | s.d. | a.s. | s.d. | a.s. | s.d. | |
| X | 8.70 | 0.67 | 7.74 | 0.56 | 12.60 | 0.15 | 12.64 | 1.51 | 18.48 | 0.20 | 12.24 | 0.60 |
| G | 11.60 | 0.73 | 15.86 | 1.02 | 13.78 | 0.59 | 15.76 | 2.00 | 21.40 | 4.41 | 18.24 | 1.95 |
| SP | 14.85 | 1.33 | 12.45 | 1.64 | 12.70 | 0.12 | 18.77 | 1.59 | 24.50 | 1.84 | 26.36 | 2.49 |
| SB | 15.54 | 0.10 | 15.72 | 1.40 | 16.12 | 1.30 | 21.26 | 0.56 | 23.16 | 3.85 | 28.44 | 5.45 |
| CB_III | 15.08 | 0.55 | 13.78 | 0.09 | 14.96 | 0.05 | 32.94 | 5.39 | 29.40 | 2.87 | 26.38 | 6.75 |
| CB_# | 17.78 | 0.67 | 19.54 | 0.56 | 18.58 | 0.15 | 37.62 | 1.51 | 31.30 | 0.20 | 24.46 | 0.60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taczała-Warga, J.; Sawicki, J.; Krasowski, M.; Sokołowski, J. The Effect of Acrylic Surface Preparation on Bonding Denture Teeth to Cellulose Fiber-Reinforced Denture Base Acrylic. J. Funct. Biomater. 2022, 13, 183. https://doi.org/10.3390/jfb13040183
Taczała-Warga J, Sawicki J, Krasowski M, Sokołowski J. The Effect of Acrylic Surface Preparation on Bonding Denture Teeth to Cellulose Fiber-Reinforced Denture Base Acrylic. Journal of Functional Biomaterials. 2022; 13(4):183. https://doi.org/10.3390/jfb13040183
Chicago/Turabian StyleTaczała-Warga, Joanna, Jacek Sawicki, Michał Krasowski, and Jerzy Sokołowski. 2022. "The Effect of Acrylic Surface Preparation on Bonding Denture Teeth to Cellulose Fiber-Reinforced Denture Base Acrylic" Journal of Functional Biomaterials 13, no. 4: 183. https://doi.org/10.3390/jfb13040183
APA StyleTaczała-Warga, J., Sawicki, J., Krasowski, M., & Sokołowski, J. (2022). The Effect of Acrylic Surface Preparation on Bonding Denture Teeth to Cellulose Fiber-Reinforced Denture Base Acrylic. Journal of Functional Biomaterials, 13(4), 183. https://doi.org/10.3390/jfb13040183