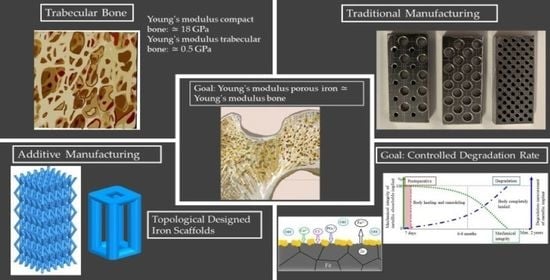
The degradation of metallic implants inside the body increases the ion content levels, causing cytotoxicity. To prevent cytotoxicity, the degradation rate needs to be controlled, and the absorption should occur at the same rate as the tissue is repaired [
3,
36], [
53]. The main challenge for iron is raise degradation rate by accelerating the process. High energy grain boundaries in iron alloys and finer microstructures attend to enhance the corrosion rate [
54,
55]. Further methods have been used to control the degradation rate, one of them making porous scaffolds and other alloying iron with specific elements, as Pd, Mn, Ca, Ag, which promote iron corrosion and improve mechanical properties [
54,
56]. The main process for degradation of porous iron scaffold in SBF is diffusion process [
54].
Grain refinement methods are currently for altering the way metals degrade. An advantage of these techniques is that the chemistry of the metal remains unchanged [
55]. Fine grained metals have also been discovered to provoke a weaker inflammatory response in hosts, with an overall better interaction. Ralston and Birbilis have introduced a relationship between the materials average grain size and its corrosion rate, similar to Hall-Petch equation, given by [
55]:
This equation represents the importance of the average grain size, d, to the corrosion current, I, since A is a constant value depending on the material purity and composition and B is also a constant depending on the media’ nature [
55].
5.1. Corrosion Mechanism of Iron in Physiological Conditions
Body fluids are an aqueous aggressive environment that provokes electrochemical corrosion of metals. Controlling the corrosion rate helps controlling the cytotoxicity by metals, achieving a balance between the release rate of corrosion products and the ability of the body to absorb and excrete them [
6]. The intimate link between degradation and mechanical integrity of the biodegradable iron implant is illustrated in
Figure 10 [
6,
34]. Ideally, degradation begins at a very slow rate to maintain optimal mechanical integrity of the implant and increases at the same rate the body is healing itself. A period of 6–12 months is expected for the remodelling process to be completed [
7]. It is important to emphasize that iron degradation should not be so fast that could cause an intolerable accumulation of degradation product around the implantation site. A total period of 12–24 months after implantation is considered reasonable for the stent to be totally degraded [
7,
34,
53].
The corrosion rate is determined by kinetic factors and corrosion tendencies are determined by thermodynamic factors [
57,
58]. Metal corrosion in vivo is predominantly driven by chloride ions present in body fluids, namely the contact with blood and interstitial fluid. The chloride ion concentration in plasma is 113 mEq L
−1 and in interstitial fluid is 117 mEq L
−1, despite the low value is capable of corroding metallic implants [
59]. In addition, chemicals such as amino acids and proteins found in body fluids tend to accelerate corrosion. The pH of the body fluid changes little acting as a buffer solution. Normal blood and interstitial fluids have a pH of around 7.35–7.45, although it can decrease near surface implantation areas and isoelectric points of biomolecules, such as proteins [
59].
Recent research made by Sharma et al. [
60] measured the pH increase in 28 days of additive manufactured porous iron in SBF solution. The results showed an increase in pH of 0.5 ± 0.05.
Li et al. [
21] observed an increase of pH 7.4 to 7.8 after 28 days immersion in r-SBF solution for an iron scaffold with 80% porosity made by direct metal printing.
A general representation of metallic interfaces reacting with body fluid is present in
Figure 11, where the metal reacts with the environment, release positive ions (M
n+) to the environment, keeping electrons (e
−) to the metal substrate. The contact of surface metal with body fluid results in oxidization of the metal to a more stable ion [
61]. The reactions lead to formation of a protective metal oxide layer on the surface (yellow spots). The interactions with the body fluids may lead to deposition of calcium phosphate on the metal oxide layer, which permit that cells adhere on the surface to form tissues [
61].
Metals with an electrode potential slightly higher than zero may, under certain environments inside the human body, be degraded [
37]. Specific parameters, such as surface film condition and environmental aspects (e.g., pH and flow), influence the degree of corrosion kinetics and degradation process. These can be reflected by Pilling-Bedworth ratio and Pourbaix diagram [
37].
The electrochemical corrosion of iron in physiological environment happens in an oxygen absorption mode, and can be expressed through the following reactions [
56,
62,
63]:
Fe(OH)
3 is hydrolysed in the presence of oxygen and chloride ions. Fe(OH)
2 react with a part of FeO(OH), resulting in the formation of magnetite Fe
3O
4, a protective iron oxide layer, lowering the corrosion rate [
56]:
Hank’s solution is composed by phosphates, sulphates, chlorides, and carbonates (see
Table 9 and ref [
51]). During anodic oxidation, Fe
2+ ions may occur facilitating the formation of iron phosphate. The corrosion of pure iron in Hank’s solution increases the pH value, easing the precipitation and deposition of those phosphates. The proposed equilibrium equations are shown in Equations (9)–(16) [
56]:
Generally, Pourbaix diagrams predict the stability and corrosion of metals in aqueous solution at 25 °C [
37,
51]. The diagrams also indicate regions of potential and pH in which the metal is protected from severe corrosion [
37]. Moreover, diagrams provide the evidence of corrosion and the prediction of corrosion products.
Figure 12 illustrates the calculated Pourbaix diagram for pure iron in physiological concentrations (37 °C). The concentration of HPO
4−2 and HCO
−3 (CO
2(aq)) in the diagram are set to be identical to the concentrations in human blood plasma (0.001 mol L
−1 for HPO
4−2, and 0.027 mol L
−1 for CO
2(aq)) [
37].
As foreseen on diagrams, iron in physiological conditions (T = 37 °C, pH = 7.4 and E = 0.78 V) will react and form solid Fe2O3. Furthermore, HPO4−2 will exist, but no carbonate ion species are expected to be present under the same conditions.
For comparison purposes
Table 9 and
Table 10 displayed the body fluids composition and the composition of various simulated body fluids, respectively.
As can be remarked the differences in ions concentrations are significant for different simulated body fluids and consequently influence the degradation behaviour of pure iron and the obtained corrosion products [
2]. The interaction between pure iron and different kinds of ions and chemical species, as carbonates, chlorides is complex. The proposed equilibrium equations with HCO
3− are [
51]:
The presence of chloride ions enhances the corrosion rate of iron and passivation is not accomplished. Chloride ions have a predominant presence to the corrosion process in comparison with bicarbonate and carbonate ions. Degradation products do not homogeneously cover surface, and chloride ions concentrates in preferential sites without the formation of a passive layer. The water hydrolyses the metal chloride, forming hydroxide and free acids, causing a local pH decrease. Corrosion pits growth wider and deeper following an autocatalytic reaction. Hydrogen carbonates and carbonates ions passivation effect is decreased by the chloride ions. Chloride ions inhibit the coalescence and crystallization of passive films, as well as the average thickness of oxide films. The final degradation product is predominantly γ-FeOOH. The proposed equilibrium equations with Cl
− can occur as [
51,
64]:
Conversely, the interaction between phosphates species and iron species strongly depends on pH, concentration of dissolved oxygen and the concentration of phosphates and iron. The precipitation of fine iron phosphates is triggered with the FeOOH species surface, causing the adsorption of iron ions. Pitting is inhibited when the concentration of phosphate ions overlaps the chloride ions concentration. The proposed equilibrium equations with H2PO
4−/HPO
42− are [
51,
64]:
5.2. In Vitro and In Vivo Biocompatibility
One of the first important studies about iron biocompatibility and degradation in vivo in coronary application was reported by Peuster et al. [
65]. It was a one-year study in animal model, with pure iron and 316L stainless steel stents implanted in the aorta of pigs. Iron resulted to be a suitable metal for stent applications.
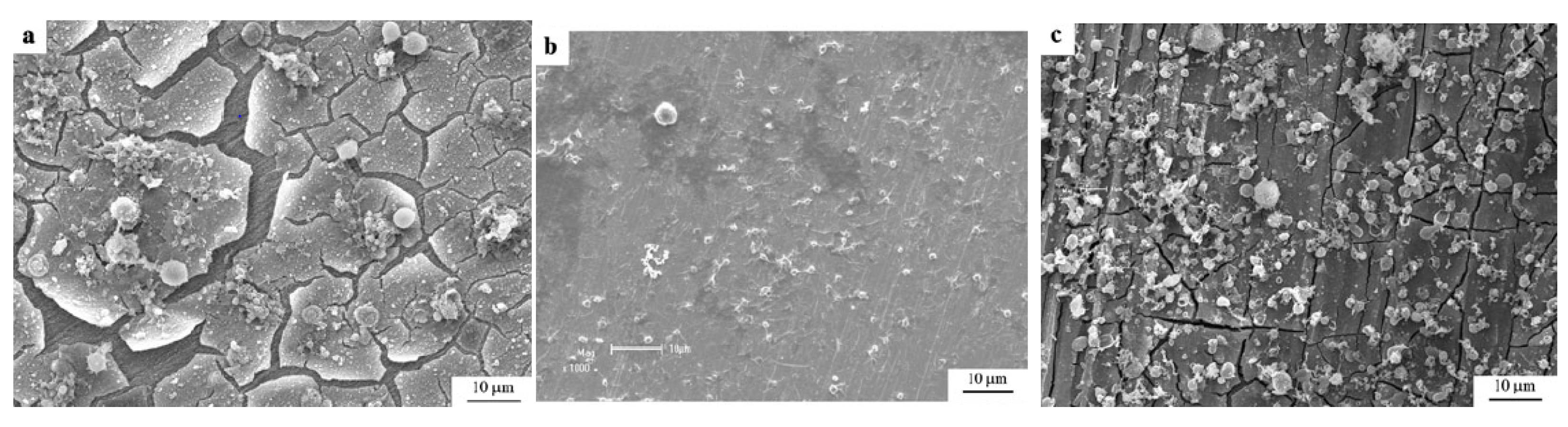
Zhang et al. [
62] at a pioneer study on iron compatibility with blood and cell compares 99.9 wt% purity iron with magnesium-manganese-zinc alloy and 316L stainless steel in Hank’s solution. ISO 10993-4 standard was followed in this research and the haemolysis assay resulted in a low haemolysis ratio for iron. For the haemolysis assay, rabbit whole blood with 3.8 wt% sodium citrate was utilized. The prothrombin time assay resulted in excellent anticoagulant iron, and platelet adhesion tests in iron showed impressive anti-platelets adhesion. During cells toxicity, iron ions presented toxicity to the stem marrow cell of mouse bone. The standard ISO 10993-4 recommends the value of 5% in the haemolysis ratio to not cause haemolysis to blood system. Iron presented a ratio of 2.44%, accepted by the standard and proving iron has excellent anti-haemolysis property.
Figure 13 illustrates the SEM images of platelet adhesion of iron, 316L stainless steel and Mg-alloy after 3 h immersed in rabbit blood plasma [
62]. The number density of platelets on the surface for pure iron was 940 ± 164, for 316L stainless steel was 7211 ± 633 and for Mg-Mn-Zn alloy was 10270 ± 918. This analysis shows the iron anti-platelet adhesion property. The electrochemical behavior of pure iron was studied by open circuit potential-time tests, to measure the biocorrosion properties. The parameters obtained were E
corr = −0.510 V, I
corr = 1.68 × 10
−5 A, E
b (break potential) = −0.40 V. The surface crystalline structure evaluated by XDR present phosphates as the main corrosion products, Mg
3(PO
4)
2, Ca
3(PO
4)
2 and Fe
3(PO
4)
2·8H
2O. Also, XPS spectra showed more Fe
2+ compared to Fe
3+. The increase of corrosion rate is time-dependent until a certain accumulation of products on the surface of iron. However no passivation stage was found at the Hank’s solution and no noble breakdown, possibly because the surface had not attained a protective film [
62].
Iron ions may produce reactive oxygen species in cells. Highly reactive oxygen species can react with the most molecules found in cells, making them toxic. Furthermore, free iron can react with unsaturated fatty acids, resulting in the formation of lipid hydroperoxides and subsequently alkoxyl and peroxyl radicals. These products are capable of causing cell death and impair cellular integrity. Despite these oxygen specimens are damaging, they are normally generated in reactions and the body has defensive strategies against it. However, iron level needs to be limited in cells. The iron concentration should be less than 0.075 mg/mL [
62].
Zhu et al. [
66] assessed the biocompatibility of pure iron and cytotoxicity on endothelial cells was performed in SBF solution for one month at 37 °C. The incubation time was almost 700 h, the degradation rate was at the highest 40 µg/(cm
2 h) and the mean rate was 20.4 µg/(cm
2 h). The corrosion was predominately uniform corrosion. Endothelial cells from human umbilical vein were cultured with 10% fetal bovine serum, penicillin and streptomycin. The cells were incubated with iron solution for three days, with concentrations varying from 0 until 2000 µg/mL. The accessed cell proliferation show non-toxicity until 50 µg/mL iron concentration [
66].
According to the literature [
67], the grain size and texture considerably affect interactions between cells and osteoblast functions and roughness also potentially influences cell growth. The attachment, orientation, migration and metabolism of the human cells are determined by the properties of the metallic implant of austenitic stainless steel. The roughness of the grains is an important factor with regard to osteoblast adhesion and protein adsorption. Proteins and focal adhesion points of cells also interact at a scale that enables them to activate signalling pathways within the cell. These pathways, in turn, have an impact on the lifespan of the cell. Increased cellular activity is implied by an increase in cell attachment and pre-osteoblast proliferation, as well as a stronger presence of fibronectin. This is turn is linked to the physico-chemical properties of the surface of the metallic implant. The attachment of cells to the implant and their growth on its surface—and thus the compatibility between them—is influenced by the chemical and morphological properties of the surface. Hydrophilicity, ionic bonding, electrostatic and van der Waals interactions are the most significant factors that drive adsorption of macromolecules and proliferation of cells on the implant surfaces. Protein adsorption, cell spreading, and cell proliferation may be assisted with high surface energy and high surface hydrophilicity and wettability. Those characteristics are controlled by the grain size of the metallic implant [
67].
Another study [
68] compared pure iron and cobalt chromium coronary stents in vivo in domestic pigs for 28 days. The morphometric comparison between these two types of coronaries resulted in less inflammation of iron compared to cobalt chromium, adding the vantage of iron being radio-opaque, while cobalt chromium is radiolucent. The stents did not cause harm to the vessel, no peripheral embolization or thrombosis were found with the angiography. Although the degradation of the iron coronary stents has not been evaluated, it is noticed the brown coloration of the tissue around the stent. A possible reason is the assimilation of iron salts by the tissue. The inflammation caused by iron stents and its degradation products was not worse than the inflammation caused by the cobalt chromium stent [
68].
A 36 month study was presented about the degradation, absorption and biocompatibility of a nitrided iron (Fe alloyed with 0.074 wt% N) coronary stent with 70 µm height [
69]. The device was compared with other stents made by PLLA-based, magnesium based, Co-Cr, pure iron scaffold and stainless steel. For in vitro corrosion tests, phosphate buffered saline (PBS) with pH at 7.4, flux speed at 25 ± 5 cm/s, oxygen at 4 ± 0.5 mg/L and temperature of 37 °C was used to simulate the inner environment of a coronary artery. For in vivo experiments, stents made by nitrited iron, pure iron and 316L stainless steel were implanted at the abdominal aortas of rabbits. Also, nitrited iron stents were allocated at the coronary artery of minipigs (porcines). Pure iron has lower mechanical strength in comparison with 316L stainless steel and Co-Cr alloy, alloys traditionally used for manufacturing permanent stents. Iron can stay implanted for 18 months, therefore the balance between strength, ductility and biodegradation is the key to accomplish a suitable iron stent. Some alloys can increase the corrosion rate and mechanical performance, but they compromise the cytocompatibility, so the element needs to be in lower concentrations. As Fe-Mn alloy the in vivo corrosion of nitrided iron stent, the results presented a higher corrosion rate for nitrited iron in comparison with pure iron. After 12 months the mass loss of nitrited iron was 44.5 ± 6.4 wt% while the mass loss for pure iron stent was 24.0 ± 5.6 wt%. The initial radial strength of nitrited iron stent was 171 ± 5 kPa, after six months of in vivo performance was proximately 150 kPa and after nine months it was above 120 kPa [
69]. The device performance of a coronary stent in terms of foreshortening, recoiling and crossing profile should be minimum. Side-branch accessibility and expansion diameter should be maximum as possible. Mechanical properties as radial strength should be between 110 and 170 kPa, high enough to support vessels lesion but still flexible, as clinically tested for stents Φ 3.0 × 18 mm. The studied nitrite iron stents presented better performance in comparison with the stents already in the market, such as, the Co-Cr alloy stent, the Mg-based stent and polymer-based stents [
69]. Corrosion products were identified by XPS and the results showed strong signals of C, O, Ca, P and Fe presented a binding energy of 709.8 eV and Fe
3+ binding energy was 712.31 eV. The degradation products identified by Raman analysis were Fe3O4, α-Fe2O3 and γ-FeOOH. The endothelialisation assess of nitrited iron stent was compared to a peer of 316L stainless steel after seven days inside a rabbit abdominal aorta, analysing the neointima coverage extend. Coronary stents are prejudicial to the endothelium, which is formed by a single layer at the vascular wall of endothelial cells [
69]. The damaged at the endothelium lead to neointimal hyperplasia and may lead to stent thrombosis [
70]. The analysis of endothelialisation was preformed to determine the neointimal hyperplasia 7 days after implantation, as illustrated in
Figure 14.
A homogeneous endothelium layer was formed with the nitride iron coronary, lowering the risk of stent thrombosis. The 316L stainless steel coronary seemed to interrupt the endothelium natural recover [
69]. The follow-up local tissue response for the minipigs and the rabbits, 53 months and 36 months, respectively, showed no pathologic changes or abnormalities of the organs. After 53 months of nitrited iron stent implementation, the images by Micro-CT 2D presented a non-uniform degradation and absorption inside the porcine coronary. The corrosion products presented a moving tendency from
in situ and peri-stent areas to tunica externa, also known as tunica adventitia, the outermost layer of the blood vessel. To essay the biosorption of the corrosion products, the in vivo analysis of the stents in minipigs was chosen because porcine coronary artery is closer to human coronary artery and the life time of a minipig is higher than a rabbit. At body fluid environment with pH 7.4, it is difficult to dissolve Fe
3O
4, Fe
3(PO
4)
2, Fe
2O
3, Fe(OH)
3 and FeOOH. Following the Pourbaix diagram of iron corrosion at a pH of 7.4 and phosphate physiological environment, Fe(OH)
3, FeOOH, Fe
2O
3 (non-magnetic) present a steady state. Other types of corrosion products with lower stability is Fe
3(PO
4)
2 and Fe
3O
4, because of their slow reaction kinetics. The natural organism low concentration of iron ions could make these corrosion products easily absorbed, since the solubility equilibrium convey towards the concentration of iron ions. The bioresorption of hydroxides and ferric oxides in body solubility, is slow and long-term. The insoluble products, resulted from iron corrosion, could take five to six years to complete bioresorption [
69].
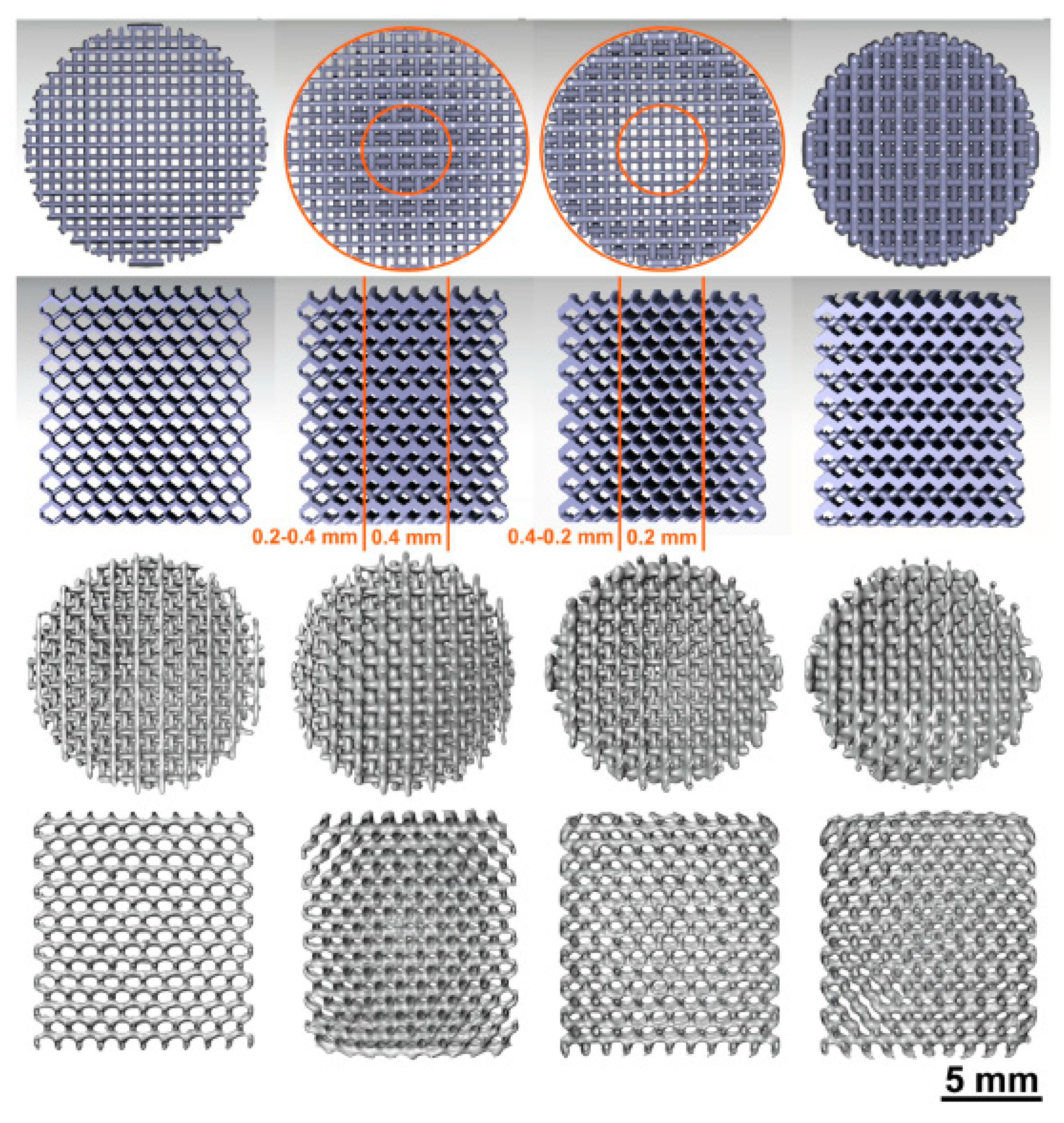
Li et al. [
21] were the first authors to report a study on the topological ordered porous iron made by direct metal printing, using a diamond unit cell. Evaluated the in vitro corrosion of iron scaffolds in r-SBF at 37 °C for 28 days.
Figure 15 represents the iron corrosion and weight loss after 28 days. The iron scaffold had a weight reduction of 3.1% after sample cleaning.
The corrosion products’ morphology and composition showed iron carbonate (FeCO
3) and iron protoxide (FeO) and FTIR also presented hydroxides and phosphates. Scanning electron microscope (SEM) analysis of the external structure,
Figure 16, reveal a white layer at the surface only after 1 day of immersion. From day 7, the structure surface presented shiny white loose degradation products, and after 28 days, these degradation products covered surface structure almost completely. The scaffold geometry interfered with the degradation at the center and at the periphery region. The degradation products at day 7 were thinner and more condensed at the centre. At the periphery, the degradations products were loose and thicker. The periphery region presented more phosphorus and calcium [
21].
Spot 1, spherically shaped and containing C, O, Ca and Fe
Spot 2, feather shaped and containing C, O and Fe.
The mechanical properties of AM iron remain similar to the properties of trabecular bone even after 28 days of biodegradation, which is an advantage compared to other metals. The degradation rate of the topological scaffolds was found to be 12 times larger than the one of compact iron. A suitable cytocompatibility was also observed. Another mechanical requirement for an orthopaedic material that lasts from weeks to one year is to have a strain in the interval 1.1 to 2.1, [
1], which was adequate [
21].
Moreover, in vitro cytocompatibility and degradation of iron porous scaffolds obtained using Fe-30Mn powder and binder jet printing point out a significantly faster degradation rate of the Fe-30Mn alloy compared to pure iron [
24].
Li et al. [
41] studied the corrosion caused by fatigue of iron ordered scaffolds, produced by selective laser melting (SLM), finding a revised simulated body fluid with cyclic load and degradation. One of the obligations of bone substituting biomaterials is the mechanical loading resistance, therefore with a good resistance to fatigue fracture. 70% of yield stress in air and 65% of yield stress in r-SBF, mainly due to iron’s ductility and slow degradation. Cyclic loading increased the degradation rate of iron, but a high fatigue strength remains, among others mechanical and chemical properties. This study present iron as a suitable bioactive bone implant [
41].
5.3. Influence of Surface Treatments on Biodegradation Behaviour
Surface treatments are used primarily to enhance the biocompatibility of iron, increase the corrosion rate, and also aimed for an uniform corrosion of iron. The surface functionalization of iron to improve its biocompatibility is reported in studies including ion implantation with tantalum, with lanthanum, formation of Fe-O film, plasma nitriding, coatings with calcium phosphates and polymeric coatings [
1,
48,
71]. Cytocompatibility and osseointegration are bioactivities improved by coating the metallic surface [
56].
Huang and Zheng [
48] measured pure iron degradation by coating with platinum (Pt) discs arrayed in pattern by photolithography and evaporation by electron beam. The patterned was adopted to control the degradation rate and regulate cells proliferation and adhesion. Platinum was chosen for its hemocompatibility and high corrosion potential, forming galvanic cells with pure iron. Platinum presents cytotoxicity but the chemical stability prevents for ions released into the body. The platinum discs had two designs, one with 20 µm diameter, the nearest space between discs was 5 µm and the thickness was approximately 285 nm (Φ20 µm × S5 µm). The second design was Φ4 µm × S4 µm with thickness around 80 nm [
48]. Electrochemical corrosion tests in Hank’s solution demonstrated significantly increase the corrosion current density (I
corr) and decrease of corrosion potential (E
corr) as listed on
Table 11, that also present the corrosion rate in static immersion for 42 days. The higher degradation of coated iron in comparison with pure iron is a consequence of galvanic cells formed between platinum discs and iron matrix [
48].
Platinum discs improved degradation rate and biocompatibility of pure iron, as the results of cytotoxicity tests with cell viabilities, human umbilical vein endothelial cells and human vascular smooth muscle cells. Haemolysis and platelet adhesion, followed by ASTM F756-08, was analyzed and the risk of thrombosis caused by pure iron can be decreased by the platelet adhesion on Pt coated
Figure 17 illustrates the hemolysis percentage and number of adhered platelets found in this study [
48].
Aiming the improvement of iron biocompatibility, surface modification with hydroxyapatite as a coating presents great outcomes. Hydroxyapatite is widely used as coating for metallic protheses, since hydroxyapatite is the main mineral constituent of bone and presents outstanding bone integration [
23]. The in vivo osteointegration and the cytocompatibility of the protheses are affected by the bonding between coating and substrate and the morphology of the coating. The morphology is expected to be homogenous and uniform, also with high strength bonding and most of all the coating must improve biocompatibility. Nano-Plotter 3D printing iron scaffolds with tailored mechanical behaviour and were coated with nanostructured hydroxyapatite by hydrothermal method, as illustrated in
Figure 18 [
23].
The coating successfully reduced the release of Fe ions, to below 2 mg/L for 120 µm hydroxyapatite thickness, increasing the cytocompatibility of rabbit bone marrow mesenchymal stem cells (rBMSCs). The study compared the osteogenic differentiation with the analysis of alkaline phosphatase in scaffolds with and without hydroxyapatite coating. The results showed an increased activity of alkaline phosphatase (ALP) activity of rBMSCs with the hydroxyapatite coating, indicating a osteogenic bioactivity of AM iron scaffolds [
23].
Another perspective about the coated porous structures is the improvement of antibacterial coating response compared to solid implants, partly because of a higher specific surface area [
72]. Iron foams were coated with polyethyleneimine (PEI), an organic polymer with biological applications which was also used to enhance the cytocompatibility of iron and its degradability [
13].
Hong et al. fabricated by binder-jet 3D printing alloys with Fe-35 wt% Mn and Fe-34 wt% Mn-1 wt% Ca, evaluating the cytocompatibility and degradation behaviour [
32]. The mechanical properties tests were conducted following ASTM E8-04 and the electrochemical corrosion tests were performed with Hank’s solution HBSS H1387, at 37.4 °C. The corrosion current density I
corr and the corrosion potential E
corr were determined by Tafel analysis from potentiodynamic polarization curves, as illustrated in
Figure 19 [
32].
The calculate corrosion current density increase as the alloy elements Ca and Mg concentrations rises in the alloy and corrosion potential follows a more negative value trend as Ca and Mg concentrations rises (
Table 12).
The cell viability of the 3D Fe-alloys, as presented in
Figure 20, were evaluated by murine osteoblast-like MC3T3-E1 cell line, at 37.4 °C for 72 h, with live cells as green light. The analysis suggested better cytocompatibility for Fe-Mn-1Ca and Fe-Mn-2Ca in comparison with the alloys incorporating magnesium [
32].