Predicting Predisposition to Tropical Diseases in Female Adults Using Risk Factors: An Explainable-Machine Learning Approach
Abstract
:1. Introduction
2. Methodology
2.1. Dataset Description and Data Preprocessing
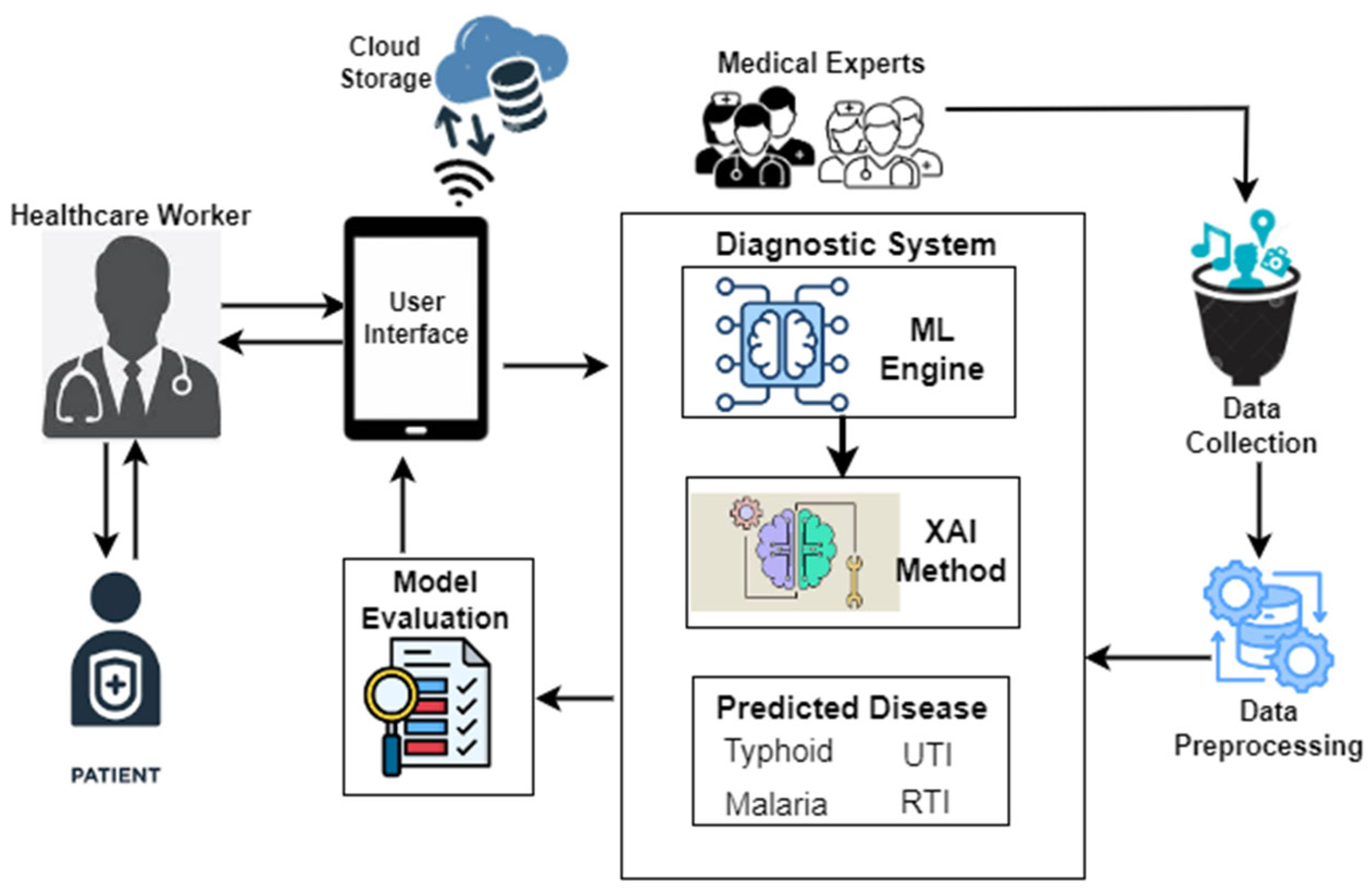
2.2. Prediction Model Development and Interpretability Approach
2.3. Prediction System Framework
2.4. Model Performance Metrics
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valdez, G.F.D.; Ajzoon, M.; Al Zuwameri, N. A Scoping Review of the Biological, Socioeconomic and Environmental Determinants of Overweight and Obesity Among Middle Eastern and Northern African Nationalities. Sultan Qaboos Univ. Med. J. 2024, 24, 20. [Google Scholar] [CrossRef] [PubMed]
- Lindert, J. Outside the Box–An Expanded View of Environmental Factors. ISEE Conf. Abstr. 2014, 26, 4440. [Google Scholar] [CrossRef]
- Winters-Miner, L.A.; Bolding, P.S.; Hilbe, J.M.; Goldstein, M.; Hill, T.; Nisbet, R.; Miner, G.D. Practical Predictive Analytics and Decisioning Systems for Medicine; Elsevier: Amsterdam, The Netherlands, 2015; pp. 757–794. [Google Scholar] [CrossRef]
- Mor, A.; Thomsen, R.W. Risk of Infections in Patients with Chronic Diseases. Open Infect. Dis. J. 2012, 6, 25–26. [Google Scholar] [CrossRef]
- Beldomenico, P.M.; Begon, M. Disease Spread, Susceptibility and Infection Intensity: Vicious Circles? Trends Ecol. Evol. 2010, 25, 21–27. [Google Scholar] [CrossRef]
- Okwa, O.O. Tropical Parasitic Diseases and Women. Ann. Afr. Med. 2007, 6, 157–163. [Google Scholar] [CrossRef]
- Michelim, L.; Bosi, G.R.; Comparsi, E. Urinary Tract Infection in Pregnancy: Review of Clinical Management. J. Clin. Nephrol. Res. 2016, 3, 1030. [Google Scholar]
- Sappenfield, E.; Jamieson, D.J.; Kourtis, A.P. Pregnancy and Susceptibility to Infectious Diseases. Infect. Dis. Obstet. Gynecol. 2013, 2013, 752852. [Google Scholar] [CrossRef]
- Singhal, T. Infections in Pregnancy. J. Clin. Infect. Dis. Soc. 2024, 2, 28–33. [Google Scholar] [CrossRef]
- Jain, J.J. Changing Epidemiology of Infections in Pregnancy: A Global Perspective. In Infections and Pregnancy; Springer: Singapore, 2022; pp. 3–12. [Google Scholar] [CrossRef]
- Obeagu, E.I.; Obeagu, O.G. Malaria During Pregnancy: Effects on Maternal Morbidity and Mortality. Elite J. Nurs. Health Sci. 2024, 2, 50–68. [Google Scholar]
- Czajkowski, K.; Broś-Konopielko, M.; Teliga-Czajkowska, J. Urinary Tract Infection in Women. Menopause Rev. Przegląd Menopauzalny 2021, 20, 40–47. [Google Scholar] [CrossRef]
- Faraz, A.A.; Mendem, S.; Swamy, M.V.; Shubham, P.; Vinyas, M. Urinary Tract Infections in Women: Treatment Options and Antibiotic Resistance. J. Pharm. Sci. Res. 2020, 12, 875–879. [Google Scholar]
- Curtiss, N.; Meththananda, I.; Duckett, J. Urinary Tract Infection in Obstetrics and Gynaecology. Obstet. Ginecol. Reprod. Med. 2017, 27, 261–265. [Google Scholar] [CrossRef]
- Foxman, B. Urinary Tract Infection Syndromes: Occurrence, Recurrence, Bacteriology, Risk Factors, and Disease Burden. Infect. Dis. Clin. N. Am. 2014, 28, 1. [Google Scholar] [CrossRef] [PubMed]
- Tokatli, M.R.; Sisti, L.G.; Marziali, E.; Nachira, L.; Rossi, M.F.; Amantea, C.; Malorni, W. Hormones and Sex-Specific Medicine in Human Physiopathology. Biomolecules 2022, 12, 413. [Google Scholar] [CrossRef]
- Kareva, I. Immune Suppression in Pregnancy and Cancer: Parallels and Insights. Transl. Oncol. 2020, 13, 100759. [Google Scholar] [CrossRef]
- Mehta, S.; Mann, A. Pregnancy Changes Predisposing to Infections. In Infections and Pregnancy; Springer: Singapore, 2022; pp. 13–25. [Google Scholar] [CrossRef]
- Dawood, F.S.; Garg, S.; Fink, R.V.; Russell, M.L.; Regan, A.K.; Katz, M.A.; Fell, D.B. Epidemiology and Clinical Outcomes of Hospitalizations for Acute Respiratory or Febrile Illness and Laboratory-Confirmed Influenza among Pregnant Women during Six Influenza Seasons, 2010–2016. J. Infect. Dis. 2020, 221, 1703–1712. [Google Scholar] [CrossRef]
- Dirican, A.Ö.; Ceran, M.U.; Özçimen, E.E.; Çulha, A.A.; Abasıyanık, M.A.; Üstün, B.; Akgün, S. COVID-19 Infection and Women’s Health; Which Women Are More Vulnerable in Terms of Gynecological Health? Preprint 2023. [Google Scholar] [CrossRef]
- Kapoor, N.; Arora, S.; Kalra, S. Gender Disparities in People Living with Obesity-An Unchartered Territory. J. Midlife Health 2021, 12, 103–107. [Google Scholar] [CrossRef]
- Maccioni, L.; Weber, S.; Elgizouli, M. Obesity and Risk of Respiratory Tract Infections: Results of an Infection-Diary-Based Cohort Study. BMC Public Health 2018, 18, 271. [Google Scholar] [CrossRef]
- Asuquo, E.F.; Akpan-Idiok, P.A. The Exceptional Role of Women as Primary Caregivers for People Living with HIV/AIDS in Nigeria, West Africa. In Suggestions for Addressing Clinical and Non-Clinical Issues in Palliative Care, Caregiving and Home Care; IntechOpen: London, UK, 2020; pp. 101–115. [Google Scholar] [CrossRef]
- Zewdie, A.; Degefa, G.H.; Donacho, D.O. Health Risk Assessment of Indoor Air Quality, Sociodemographic and Kitchen Characteristics on Respiratory Health Among Women Responsible for Cooking in Urban Settings of Oromia Region, Ethiopia: A Community-Based Cross-Sectional Study. BMJ Open 2023, 13, e067678. [Google Scholar] [CrossRef]
- Saad, S. Women and Places; Female Street Vendors, Territorial Identity and Placemaking. J. Art Des. 2022, 2, 1–14. [Google Scholar] [CrossRef]
- Pradhan, S.; Raksha, G.S.; Akhil, P. Role of Women in Food and Agricultural Development: Breaking Barriers for Sustainable Growth. In Impact of Women in Food and Agricultural Development; IGI Global: Hershey, PA, USA, 2024; pp. 130–148. [Google Scholar] [CrossRef]
- Statista. Global Adult Literacy Rate from 2000 to 2022, by Gender. Available online: https://www.statista.com/statistics/1220131/global-adult-literacy-rate-by-gender/ (accessed on 21 September 2024).
- Jimoh, R.; Adamu, A.; Oyewobi, L.; Bajere, P. How Women Are Locked Out of Nigeria’s Construction Industry. The Conversation. 2024. Available online: https://theconversation.com/how-women-are-locked-out-of-nigerias-construction-industry-157643#:~:text=In%20Nigeria%2C%20women%20make%20up,ethics%20and%20values%20in%20Nigeria (accessed on 21 September 2024).
- Masuet-Aumatell, C.; Atouguia, J. Typhoid Fever Infection–Antibiotic Resistance and Vaccination Strategies: A Narrative Review. Travel Med. Infect. Dis. 2021, 40, 101946. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, B.; Varol, A. A Symptom-Based Machine Learning Model for Malaria Diagnosis in Nigeria. In Proceedings of the 2021 9th International Symposium on Digital Forensics and Security (ISDFS), Elazig, Turkey, 28–29 June 2021; IEEE: New York, NY, USA, 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Odion, P.O.; Ogbonnia, E.O. Web-Based Diagnosis of Typhoid and Malaria Using Machine Learning. Nigerian Defence Academy J. Military Sci. Interdiscip. Stud. 2024, 1, 89–103. [Google Scholar]
- Attai, K.; Ekpenyong, M.; Amannah, C.; Asuquo, D.; Ajuga, P.; Obot, O.; Johnson, E.; John, A.; Maduka, O.; Akwaowo, C.; et al. Enhancing the Interpretability of Malaria and Typhoid Diagnosis with Explainable AI and Large Language Models. Trop. Med. Infect. Dis. 2024, 9, 216. [Google Scholar] [CrossRef]
- Su, M.; Guo, J.; Chen, H.; Huang, J. Developing a Machine Learning Prediction Algorithm for Early Differentiation of Urosepsis from Urinary Tract Infection. Clin. Chem. Lab. Med. 2023, 61, 521–529. [Google Scholar] [CrossRef]
- Prakash, K.B.; Imambi, S.S.; Ismail, M.; Kumar, T.P.; Pawan, Y.N. Analysis, Prediction and Evaluation of COVID-19 Datasets Using Machine Learning Algorithms. Int. J. 2020, 8, 2199–2204. [Google Scholar] [CrossRef]
- Kumarakulasinghe, N.B.; Blomberg, T.; Liu, J.; Leao, A.S.; Papapetrou, P. Evaluating Local Interpretable Model-Agnostic Explanations on Clinical Machine Learning Classification Models. In Proceedings of the 2020 IEEE 33rd International Symposium on Computer-Based Medical Systems (CBMS), Rochester, MN, USA, 28–30 July 2020; IEEE: New York, NY, USA, 2020; pp. 7–12. [Google Scholar] [CrossRef]
- Attai, K.; Akwaowo, C.; Asuquo, D.; Esubok, N.E.; Nelson, U.A.; Dan, E.; Uzoka, F.M. Explainable AI Modelling of Comorbidity in Pregnant Women and Children with Tropical Febrile Conditions. Proc. Int. Conf. Artif. Intell. Appl. 2023, 152–159. [Google Scholar] [CrossRef]
- University of Uyo Teaching Hospital; Mount Royal University. NFRF Project Patient Dataset with Febrile Diseases [Data Set]; Zenodo: Bern, Switzerland, 2024. [Google Scholar] [CrossRef]
- Yousefi, M.; Rahmani, K.; Rajabi, M.; Reyhani, A.; Moudi, M. Random Forest Classifier for High Entropy Alloys Phase Diagnosis. Afr. Mat. 2024, 35, 57. [Google Scholar] [CrossRef]
- Palimkar, P.; Shaw, R.N.; Ghosh, A. Machine Learning Technique to Prognosis Diabetes Disease: Random Forest Classifier Approach. In Advanced Computing and Intelligent Technologies; Bianchini, M., Piuri, V., Das, S., Shaw, R.N., Eds.; Springer: Singapore, 2022; Volume 218, pp. 317–327. [Google Scholar] [CrossRef]
- Asselman, A.; Khaldi, M.; Aammou, S. Enhancing the Prediction of Student Performance Based on the Machine Learning XGBoost Algorithm. Interact. Learn. Environ. 2021, 31, 3360–3379. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, L.; Bhatti, U.A.; Huang, M. Interpretable Machine Learning for Personalized Medical Recommendations: A LIME-Based Approach. Diagnostics 2023, 13, 2681. [Google Scholar] [CrossRef]


| Age Range | Frequency |
|---|---|
| 13 years to 18 years | 182 |
| 19 years to 35 years | 978 |
| 36 years to 50 years | 425 |
| 51 years to 65 years | 260 |
| 66 years and above | 106 |
| Total | 1951 |
| Pregnant Patients | Frequency |
| 0–3 months | 135 |
| 4–6 months | 184 |
| 7–9 months | 86 |
| Total | 405 |
| Nursing mothers | Frequency |
| 0–3 months | 26 |
| 4–6 months | 35 |
| 7–9 months | 28 |
| over 9 months | 61 |
| Total | 150 |
| Environmental Factors | Abbreviation |
|---|---|
| Poor environmental condition | PECON |
| Overcrowding | OVCRW |
| Travel to endemic region | TRVENRG |
| Exposure to mosquito bite | EXPMQBT |
| Indoor air pollution | EXPIDARPOL |
| Smoking exposure | SMSCHNSM |
| Contact with an infected person | DRCOIFPS |
| Skin puncture | SKPUPR |
| Socioeconomic Factors | |
| Street vendor | STRVEN |
| Poor personal hygiene | PPHYG |
| Intravenous drug use | IVNDRUS |
| Low fluid intake | LWFLIN |
| Biological Factors | |
| Genetic condition | GNCN |
| High blood pressure | HIBP |
| High cholesterol level | HICOLV |
| Underlying chronic illness | UNCHRIL |
| Allergy | ALG |
| Diseases | |
| Malaria | MAL |
| Enteric fever (typhoid fever) | ENFVR |
| Urinary tract infection | UTI |
| Respiratory tract infection | RTI |
| Disease | Positive Cases (n, %) | Negative Cases (n, %) |
|---|---|---|
| Malaria | 1371 (70.3%) | 580 (29.7%) |
| Typhoid fever | 565 (29%) | 1386 (71%) |
| Urinary tract infection | 542 (28%) | 1409 (72%) |
| Respiratory tract infection | 465 (24%) | 1486 (76%) |
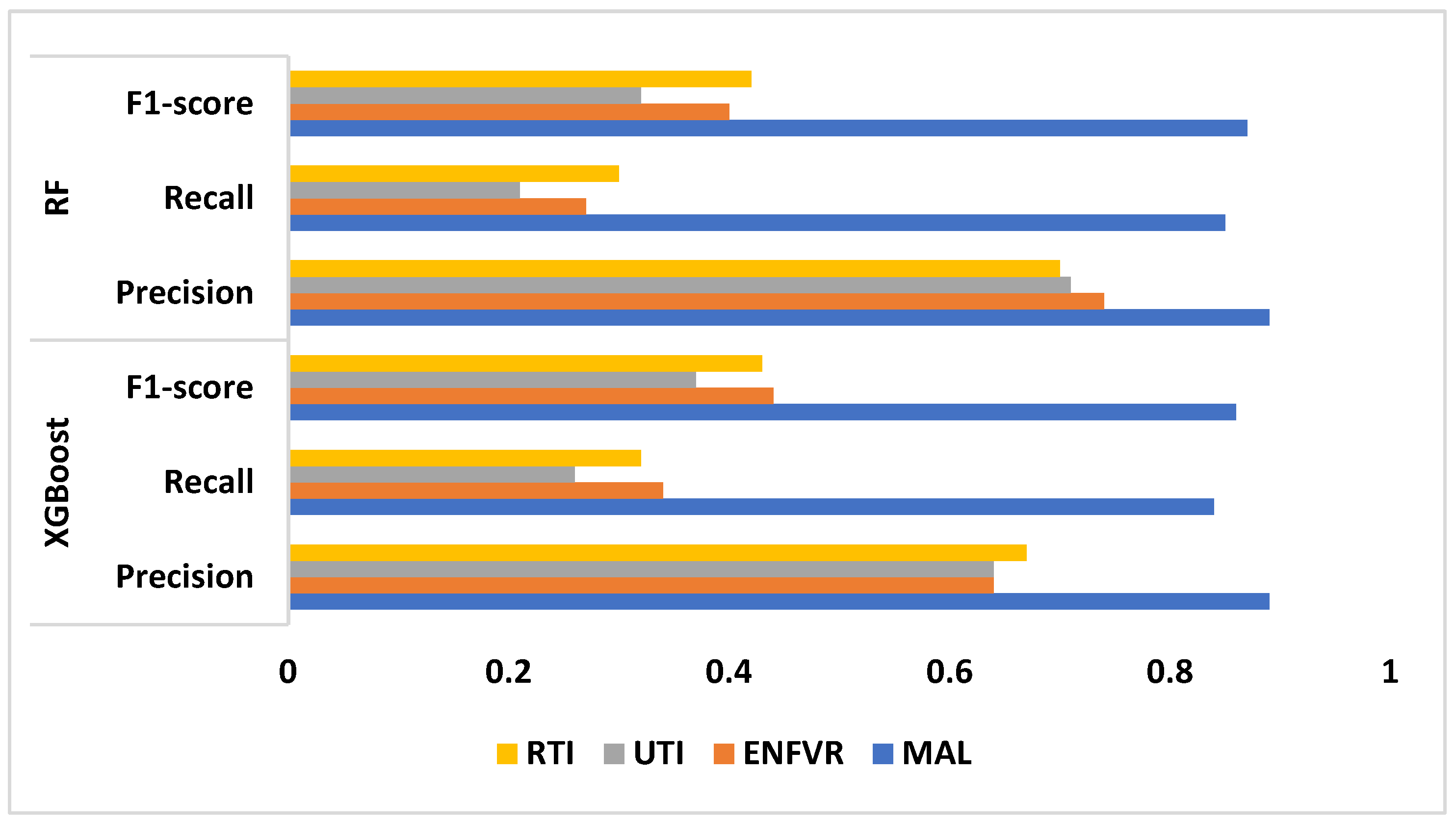
| MAL | ENFVR | UTI | RTI | ||
|---|---|---|---|---|---|
| XGBoost | Precision | 0.89 | 0.64 | 0.64 | 0.67 |
| Recall | 0.84 | 0.34 | 0.26 | 0.32 | |
| F1 score | 0.86 | 0.44 | 0.37 | 0.43 | |
| AUC-ROC | 0.66 | ||||
| RF | Precision | 0.89 | 0.74 | 0.71 | 0.70 |
| Recall | 0.85 | 0.27 | 0.21 | 0.30 | |
| F1 score | 0.87 | 0.40 | 0.32 | 0.42 | |
| AUC-ROC | 0.65 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attai, K.F.; Amannah, C.; Ekpenyong, M.; Baadel, S.; Obot, O.; Asuquo, D.; Attai, E.; Uzoka, F.-V.; Dan, E.; Akwaowo, C.; et al. Predicting Predisposition to Tropical Diseases in Female Adults Using Risk Factors: An Explainable-Machine Learning Approach. Information 2025, 16, 520. https://doi.org/10.3390/info16070520
Attai KF, Amannah C, Ekpenyong M, Baadel S, Obot O, Asuquo D, Attai E, Uzoka F-V, Dan E, Akwaowo C, et al. Predicting Predisposition to Tropical Diseases in Female Adults Using Risk Factors: An Explainable-Machine Learning Approach. Information. 2025; 16(7):520. https://doi.org/10.3390/info16070520
Chicago/Turabian StyleAttai, Kingsley Friday, Constance Amannah, Moses Ekpenyong, Said Baadel, Okure Obot, Daniel Asuquo, Ekerette Attai, Faith-Valentine Uzoka, Emem Dan, Christie Akwaowo, and et al. 2025. "Predicting Predisposition to Tropical Diseases in Female Adults Using Risk Factors: An Explainable-Machine Learning Approach" Information 16, no. 7: 520. https://doi.org/10.3390/info16070520
APA StyleAttai, K. F., Amannah, C., Ekpenyong, M., Baadel, S., Obot, O., Asuquo, D., Attai, E., Uzoka, F.-V., Dan, E., Akwaowo, C., & Uzoka, F.-M. (2025). Predicting Predisposition to Tropical Diseases in Female Adults Using Risk Factors: An Explainable-Machine Learning Approach. Information, 16(7), 520. https://doi.org/10.3390/info16070520







