Economic Evaluation of Nature-Based Therapy Interventions—A Scoping Review
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- Study population: Human participants
- Concept/Phenomena of interest: Nature-based therapeutic intervention including an economic evaluation
- Source of evidence: All types of study design; peer-reviewed articles, reports, grey literature
- No restriction towards time limit
- Papers written in English, Danish, Swedish or Norwegian
2.3. Selecting Evidence
2.4. Critical Appraisal
2.5. Extracting Evidence
2.6. Analysis and Presentation of Results
3. Results
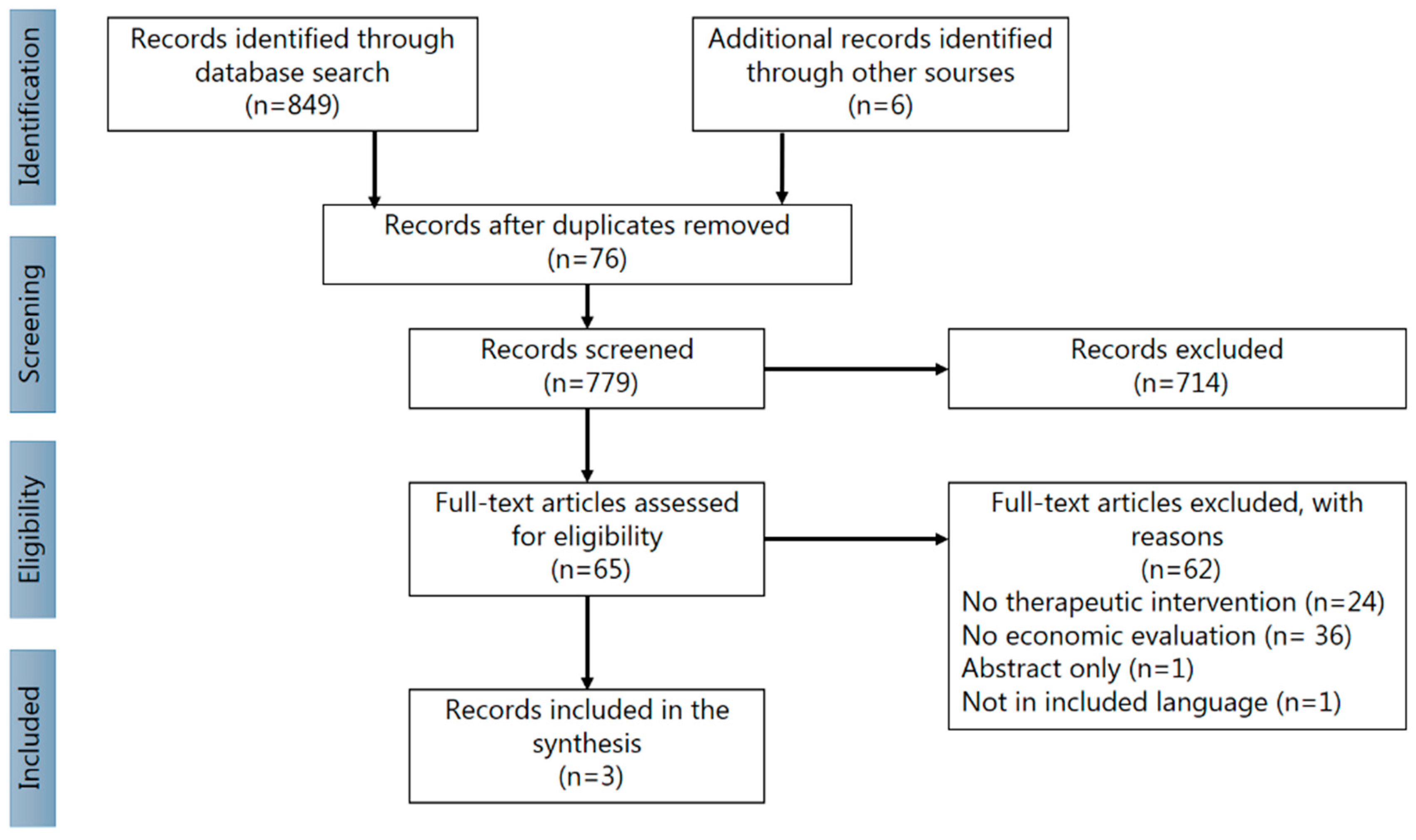
3.1. Identification of Potential Articles
3.2. Characteristics of Included Articles
- Pretty and Barton 2020
- 2.
- Elsey et al. 2018
- (I)
- Social enterprise specializing in aquaponics (cultivating aquatic plants and animals), horticulture and skills building (n = 30) or comparison: Charity warehouse sorting secondhand clothes (n = 61).
- (II)
- A religious charity with emphasis on horticulture (n = 2) or the comparison intervention: unspecified projects (n = 2).
- (III)
- A family-run cattle farm focusing on rehabilitation (n = 18) or comparison: Different activity management: addressing alcohol misuse, domestic violence, anger management and driving under influence (n = 21). No data regarding the duration and frequency of the interventions were found.
- 3.
- CJC Consulting 2016
3.3. Summary
4. Discussion
4.1. Methodological Evaluation
4.2. Economic Evaluations in the Included Studies
4.3. Nature-Based Therapy
4.4. Strengths and Limitations
5. Future Perspectives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Duraiappah, A.K.; Naeem, S.; Agardy, T.; Ash, N.J.; Cooper, H.D.; Diaz, S.; Faith, D.P.; Mace, G.; McNeely, J.A.; Mooney, H.A.; et al. Ecosystems and Human Well-Being: Biodiversity Synthesis; A Report of the Millennium Ecosystem Assessment; World Resources Institute: Washington, DC, USA, 2005. [Google Scholar]
- Food and Agriculture Organization of the United States. Available online: https://www.fao.org/ecosystem-services-biodiversity/background/cultural-services/en/ (accessed on 10 March 2020).
- Hatala, A.R.; Njeze, C.; Morton, D.; Pearl, T.; Bird-Naytowhow, K. Land and nature as sources of health and resilience among Indigenous youth in an urban Canadian context: A photovoice exploration. BMC Public Health 2020, 20, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Pretty, J.; Barton, J.; Bharucha, Z.P.; Bragg, R.; Pencheon, D.; Wood, C.; Depledge, M.H. Improving health and well-being independently of GDP: Dividends of greener and prosocial economies. Int. J. Environ. Health Res. 2016, 26, 11–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.H.; Lo, Y.Y.C.; Wong, W.H.T.; Fung, C.S.C. The associations of body mass index with physical and mental aspects of health-related quality of life in Chinese patients with type 2 diabetes mellitus: Results from a cross-sectional survey. Health Qual. Life Outcomes 2013, 11, 142. [Google Scholar] [CrossRef] [Green Version]
- Alzheimer’s Association. Alzheimer’s disease facts and figures. Alzheimer Dement. 2016, 12, 459–509. [Google Scholar] [CrossRef]
- Rojas-Rueda, D.; Nieuwenhuijsen, M.; Gascon, M.; Perez-Leon, D.; Mudu, P. Green spaces and mortality: A systematic review and meta-analysis of cohort studies. Lancet Planet. Health 2019, 3, e469–e477. [Google Scholar] [CrossRef] [Green Version]
- Rogerson, M.; Brown, D.K.; Sandercock, G.; Wooller, J.-J.; Barton, J. A comparison of four typical green exercise environments and prediction of psychological health outcomes. Perspect. Public Health 2015, 136, 171–180. [Google Scholar] [CrossRef]
- Ji, J.S.; Zhu, A.; Bai, C.; Wu, C.-D.; Yan, L.; Tang, S.; Zeng, Y.; James, P. Residential greenness and mortality in oldest-old women and men in China: A longitudinal cohort study. Lancet Planet. Health 2019, 3, e17–e25. [Google Scholar] [CrossRef] [Green Version]
- Grahn, P.; Stigsdotter, U.A. Landscape planning and stress. Urban For. Urban Green. 2003, 2, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Stigsdotter, U.K.; Corazon, S.S.; Sidenius, U.; Nyed, P.K.; Larsen, H.B.; Fjorback, L.O. Efficacy of nature-based therapy for individuals with stress-related illnesses: Randomised controlled trial. Br. J. Psychiatry 2018, 213, 404–411. [Google Scholar] [CrossRef]
- The Lancet Global Heath. Mental health matters. Lancet Glob. Health 2020, 8, e1352. [Google Scholar] [CrossRef]
- Buckley, R.; Brough, P.; Hague, L.; Chauvenet, A.; Fleming, C.; Roche, E.; Sofija, E.; Harris, N. Economic value of protected areas via visitor mental health. Nat. Commun. 2019, 10, 5005–5010. [Google Scholar] [CrossRef] [PubMed]
- Hinde, S.; Bojke, L.; Coventry, P. The Cost Effectiveness of Ecotherapy as a Healthcare Intervention, Separating the Wood from the Trees. Int. J. Environ. Res. Public Health 2021, 18, 11599. [Google Scholar] [CrossRef]
- Naor, L.; Mayseless, O. Therapeutic factors in nature-based therapies: Unraveling the therapeutic benefits of integrating nature in psychotherapy. Psychotherapy 2021, 58, 576–590. [Google Scholar] [CrossRef]
- Christiana, R.W.; Besenyi, G.M.; Gustat, J.; Horton, T.H.; Penbrooke, T.L.; Schultz, C.L. A Scoping Review of the Health Benefits of Nature-Based Physical Activity. J. Health Eat. Act. Living 2021, 1, 142–160. [Google Scholar] [CrossRef]
- Pryor, A.; Harper, N.; Carpenter, C. Outdoor Therapy: Benefits, Mechanisms and Principles for Activating Health, Wellbeing, and Healing in Nature. In Outdoor Environmental Education in Higher Education; Springer: Cham, Switzerland, 2021; pp. 123–134. [Google Scholar] [CrossRef]
- Corazon, S.S.; Poulsen, D.V.; Sidenius, U.; Gramkow, M.C.; Dorthe, D.; Stigsdotter, U.K. Konceptmanual for Nacadias Naturbaserede Terapi; Copenhagen University, Institut for Geoscience and Natural Resource Management: Copenhagen, Denmark, 2018. [Google Scholar]
- Corazon, S.S.; Stigsdotter, U.K.; Jensen, A.G.C.; Nilsson, K.S.B. Development of the nature-based therapy concept for patients with stress-related illness at the Danish healing forest garden nacadia. J. Am. Soc. Hortic. Sci. 2010, 20, 18. [Google Scholar]
- Poulsen, D.V.; Stigsdotter, U.K.; Davidsen, A.S. “That Guy, Is He Really Sick at All?” An Analysis of How Veterans with PTSD Experience Nature-Based Therapy. Healthcare 2018, 6, 64. [Google Scholar] [CrossRef] [Green Version]
- Sidenius, U.; Stigsdotter, U.K.; Poulsen, D.V.; Bondas, T. “I look at my own forest and fields in a different way”: The lived experience of nature-based therapy in a therapy garden when suffering from stress-related illness. Int. J. Qual. Stud. Health Well-Being 2017, 12, 1324700. [Google Scholar] [CrossRef] [Green Version]
- Clark, A.M. What are the components of complex interventions in healthcare? Theorizing approaches to parts, powers and the whole intervention. Soc. Sci. Med. 2013, 93, 185–193. [Google Scholar] [CrossRef]
- Kannampallil, T.G.; Schauer, G.F.; Cohen, T.; Patel, V.L. Considering complexity in healthcare systems. J. Biomed. Inform. 2011, 44, 943–947. [Google Scholar] [CrossRef] [Green Version]
- Chaudhury, P.; Banerjee, D. “Recovering with Nature”: A Review of Ecotherapy and Implications for the COVID-19 Pandemic. Front. Public Health 2020, 8, 604440. [Google Scholar] [CrossRef]
- Vibholm, A.P.; Christensen, J.R.; Pallesen, H. Occupational therapists and physiotherapists experiences of using nature-based rehabilitation. Physiother Theory Pract. 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Vujcic, M.; Tomicevic-Dubljevic, J.; Grbic, M.; Lecic-Tosevski, D.; Vukovic, O.; Toskovic, O. Nature based solution for improving mental health and well-being in urban areas. Environ. Res. 2017, 158, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Neumann, P.J.; Sanders, G.D. Cost-Effectiveness Analysis 2.0. N. Engl. J. Med. 2017, 376, 203–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, R. Cost-benefit analysis. BMJ 1993, 307, 924–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elley, R.; Kerse, N.; Arroll, B.; Swinburn, B.; Ashton, T.; Robinson, E. Cost-effectiveness of physical activity counselling in general practice. N. Z. Med. J. 2004, 117, U1216. [Google Scholar] [PubMed]
- Lindsäter, E.; Axelsson, E.; Salomonsson, S.; Santoft, F.; Ljótsson, B.; Åkerstedt, T.; Lekander, M.; Hedman-Lagerlöf, E. Cost-Effectiveness of Therapist-Guided Internet-Based Cognitive Behavioral Therapy for Stress-Related Disorders: Secondary Analysis of a Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e14675. [Google Scholar] [CrossRef]
- Dendale, P.; Hansen, D.; Berger, J.; Lamotte, M. Long-term cost-benefit ratio of cardiac rehabilitation after percutaneous coronary intervention. Acta Cardiol. 2008, 63, 451–456. [Google Scholar] [CrossRef]
- Segal, L.; Twizeyemariya, A.; Zarnowiecki, D.; Niyonsenga, T.; Bogomolova, S.; Wilson, A.; O’Dea, K.; Parletta, N. Cost effectiveness and cost-utility analysis of a group-based diet intervention for treating major depression—The HELFIMED trial. Nutr. Neurosci. 2020, 23, 770–778. [Google Scholar] [CrossRef]
- Mihalopoulos, C.; Chatterton, M.L. Cost-Effectiveness of Interventions for Anxiety and Depressive Disorders; Springer International Publishing: Cham, Switzerland, 2017; pp. 283–298. [Google Scholar]
- Coventry, P.A.; Brown, J.; Pervin, J.; Brabyn, S.; Pateman, R.; Breedvelt, J.; Gilbody, S.; Stancliffe, R.; McEachan, R.; White, P. Nature-based outdoor activities for mental and physical health: Systematic review and meta-analysis. SSM-Popul. Health 2021, 16, 100934. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI É vid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Hinde, S.; Spackman, E. Bidirectional citation searching to completion: An exploration of literature searching methods. Pharmacoeconomics 2015, 33, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.H.; Carswell, C.; Caulley, L.; Chaiyakunapruk, N.; Greenberg, D.; Loder, E.; et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 Explanation and Elaboration: A Report of the ISPOR CHEERS II Good Practices Task Force. Value Health 2022, 25, 10–31. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.A.; Ratajeski, M.A.; Bertolet, M. Grey Literature Searching for Health Sciences Systematic Reviews: A Prospective Study of Time Spent and Resources Utilized. Évid. Based Libr. Inf. Pract. 2014, 9, 28–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Pretty, J.; Barton, J. Nature-Based Interventions and Mind–Body Interventions: Saving Public Health Costs Whilst Increasing Life Satisfaction and Happiness. Int. J. Environ. Res. Public Health 2020, 17, 7769. [Google Scholar] [CrossRef]
- Elsey, H.; Farragher, T.; Tubeuf, S.; Bragg, R.; Elings, M.; Brennan, C.; Gold, R.; Shickle, D.; Wickramasekera, N.; Richardson, Z.; et al. Assessing the impact of care farms on quality of life and offending: A pilot study among probation service users in England. BMJ Open 2018, 8, e019296. [Google Scholar] [CrossRef]
- CJC Consulting. Branching Out Economic Study Extension. 2016. Available online: https://forestry.gov.scot/images/corporate/pdf/branching-out-report-2016.pdf (accessed on 11 October 2021).
- Dayson, C.; Bashir, N.; Bennett, E.; Sanderson, E. The Rotherham Social Prescribing Service For People with Long-Term Health Conditions; Sheffield Hallam University: Sheffield, UK, 2016. [Google Scholar]
- Beatton, T. The Origins of Happiness: The Science of Well-Being over the Life Course; Andrew, E., Clark, S.F., Richard, L., Nattavudh, P., George, W., Eds.; Princeton University Press: Princeton, NJ, USA, 2018. [Google Scholar]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef] [Green Version]
- Mayer, F.S.; Frantz, C.M. The connectedness to nature scale: A measure of individuals’ feeling in community with nature. J. Environ. Psychol. 2004, 24, 503–515. [Google Scholar] [CrossRef] [Green Version]
- Nisbet, E.K.; Zelenski, J.M.; Murphy, S.A. The Nature Relatedness scale: Linking individuals’ connection with nature to environmental concern and behavior. Environ. Behavior. 2009, 41, 715–740. [Google Scholar] [CrossRef]
- Huo, T.; Guo, Y.; Shenkman, E.; Muller, K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: A report from the wellness incentive and navigation (WIN) study. Health Qual. Life Outcomes 2018, 16, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallegos-Riofrío, C.A.; Arab, H.; Carrasco-Torrontegui, A.; Gould, R.K. Chronic deficiency of diversity and pluralism in research on nature’s mental health effects: A planetary health problem. Curr. Res. Environ. Sustain. 2022, 100148. [Google Scholar] [CrossRef]
- Cuschieri, S. The CONSORT statement. Saudi J. Anaesth. 2019, 13, S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Östlund, U.; Kidd, L.; Wengström, Y.; Rowa-Dewar, N. Combining qualitative and quantitative research within mixed method research designs: A methodological review. Int. J. Nurs. Stud. 2011, 48, 369–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Citation details, country of origin (where study was conducted) Publication type Study design Recruitment method Participants Number (enrolled/completed) Intervention Control Duration of the interventions Outcomes Type of economic evaluation Resource use and costs Perspective of the economic evaluation Time horizon of the evaluation Discount rate Results |
| Publication Type | Study Design | Recruitment Method | Participants | Number (Enrolled/Completed) | Intervention | Control | Duration of the Interventions | Outcomes | |
|---|---|---|---|---|---|---|---|---|---|
| Pretty and Barton 2020 (41) England | |||||||||
| Green Light Trust | Peer-reviewed | Not clear | Social prescription from general practitioner, but no further description | Vulnerable youngsters | 32 | Woodland Therapy Including natural history learning, craft activities, preparing and cooking food, led discussions and walking in woodlands. | None | 10–12 weeks | Life satisfaction/happiness (S/H) Benefits from preventing loneliness Intervention costs Method: Cost-benefit analysis Time horizon of the evaluation: Year 1 and year 10. Perspective of economic evaluation: limited societal perspective (financial and intangible benefits) Other: Annual discount rates of 3.5% and inflation of 2% applied per year Results: Intervention cost: £960 per person per program (based on pers comm with Green Light Trust) Benefit-cost ratios are calculated for year 1(1.71–15.8) and year 10 (12.9–27.1) |
| Ecominds | Adults with mental health challenges | 328 | Nature-Based Interventions consisting of counselling sessions, cognitive behavioural therapy, or psychotherapy including informal therapy of the NBI-programme. | None | No data on: Frequency of the sessions, intensity, volume and duration of the sessions | Life satisfaction/happiness (LS/H) Benefits from preventing loneliness | |||
| Trust Links Growing Together | Adults with mental health needs, learning disabilities or other disabilities. | 154 | Therapeutic horticulture as well as a range of peer-support and vocationalactivities including music, art, creative writing, yoga relaxation, cooking and crafts. | None | 1 to 2 days per week (50–100 times per year) | life satisfaction/happiness (S/H) Benefits from preventing loneliness | |||
| Elsey et al., 2018 (42) England | |||||||||
| Peer-reviewed | A quasi-experimental feasibility pilot study | Offenders (over 18 years of age) undertaking community orders | Intervention: 30/15 Control: 61/37 | A social enterprise specialising in aquaponics, horticulture and skills building | Charity warehouse sorting secondhand clothes | Not described | Primary: Clinical Outcome in Routine Evaluation—Outcome Measure (CORE-OM) Secondary: CORE-6D Mental well-being: Waarwick-Edinberg Mental Well-being Scale (WEMWBS) Smoking, alcohol, drug use, diet and physical activity. The connectedness to nature scale, The Nature Relatedness scale. Tailor-made social-care and health-resource use. Probation service data and police records. At start and after 6 months. Results: No significant difference was found in the mean CORE-6D index score at baseline and 6-month follow-up between the care farm group (mean 0.835 (SD 0.118)) and the control group 0.849 (SD 0.122). | ||
| Intervention: 2/2 Control: 2/2 | A religious charity with emphasis on horticulture | Multiple comparator projects during their community order. | |||||||
| Interventio: 18/8 Control: 21/20 | A family-run cattle farm focusing on rehabilitation | Different activity management: addressing alcohol misuse, domestic violence, anger management and drink-driving. | |||||||
| CJC Consulting, 2016 (43) Scotland | |||||||||
| Commissioned report, not peer reviewed. | Adults experiencing severe and enduring mental health problems | 305/102 | Three hours of activity per week in a woodland setting over 12 weeks. Physical activity e.g., health walks and talks, tai chi, conservation activities, rhododendron clearance and bird box construction, bush craft, fire lighting and shelter building. | None | 12 weeks Around 3 h per week | SF-6D (derived from SF-12) collected pre-program, immediate post-program, 3-month post-program QALY (based on SF-6D) Results: QALY based on the entire period (2011–2015) cost per QALY was £17,276 (based on costs £392). | |||
| Resource Use and Costs | Type of Economic Evaluation | Time Horizon of the Evaluation | Perspective of Economic Evaluation | Discount Rate | Results | |
|---|---|---|---|---|---|---|
| Pretty and Barton, 2020 (41) | ||||||
| Green Light Trust | Intervention costs (based on pers comm with Green Light Trust) Costs prevented from reduced public services use Cost prevented from reduced loneliness Benefits created from increased LS/H | Assessment of benefit and costs | Year 1 and year 10. | Limited societal perspective (financial and intangible benefits) | Annual discount rates of 3.5% and inflation of 2% applied per year | Intervention cost: £960 per person per program Total economic benefit per person: £13,642–£14,332 Year 1) and £14,332–£24,568 (year 10) Benefit-cost ratios are calculated for year 1(1.71–15.8) and year 10 (12.9–27.1) |
| Ecominds | Cost prevented from reduced loneliness Benefits created from increased LS/H | Assessment of benefits | Year 1 and year 10. | Limited societal perspective (intangible benefits) | Annual discount rates of 3.5% and inflation of 2% applied per year | No intervention costs reported. Total economic benefit per person: £7264 (year 1) and £9280 (year 10) No benefit-cost ratio is calculated |
| Trust Links Growing Together | Intervention costs (based on pers comm with Trust Link) Cost prevented from reduced loneliness Benefits created from increased LS/H | Assessment of benefit and costs | Year 1 and year 10. | Limited societal perspective (intangible benefits) | Annual discount rates of 3.5% and inflation of 2% applied per year | Intervention cost: £1130 per person per year Total economic benefit per person: £7264 (year 1) and £9280 (year 10) Benefit-cost ratios are calculated for year 1(6.42) and year 10 (7.61) |
| Elsey et al., 2018 (42) | ||||||
| Intervention costs: Supervision of probation service users and travel costs Healthcare costs: Health service visits, hospital services and medication use (self-reported). Social service costs: social service visits (self-reported) | Feasibility study of a cost-effectiveness analysis (cost-outcome description). | 6 months | Health and social-care perspective | Discount rate: Not mentioned | Average costs of resource use within the past month: £95.74 for the control group and £ 67.23 for the care farms group. No significant difference was found in the mean CORE-6D index score at baseline and 6-month follow-up between the care farm group (mean 0.835 (SD 0.118)) and the control group 0.849 (SD 0.122). | |
| CJC Consulting, 2016 (43) | ||||||
| Cost related directly to the intervention (staff costs, delivery agents’ costs, set-up costs, travel costs, service users’ costs) | Partial cost-utility analysis comparing costs relative to changes in outcome (QALY) pre and post program participation | 3 months | Not explicitly mentioned | Discount rate: Not mentioned | Mean QALY gain of 0.0495 (2011/2012), 0.00347 (2014/2015) and 0.02269 (2011–2015) Cost per person attending at least one session of £426 (2011/12) and £392 (2014/15) Cost per QALY (2011/12—based on costs £426) £8,600. Using the estimated QALY based on the entire period (2011–2015) cost per QALY is £17,276 (based on costs £392). | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Busk, H.; Sidenius, U.; Kongstad, L.P.; Corazon, S.S.; Petersen, C.B.; Poulsen, D.V.; Nyed, P.K.; Stigsdotter, U.K. Economic Evaluation of Nature-Based Therapy Interventions—A Scoping Review. Challenges 2022, 13, 23. https://doi.org/10.3390/challe13010023
Busk H, Sidenius U, Kongstad LP, Corazon SS, Petersen CB, Poulsen DV, Nyed PK, Stigsdotter UK. Economic Evaluation of Nature-Based Therapy Interventions—A Scoping Review. Challenges. 2022; 13(1):23. https://doi.org/10.3390/challe13010023
Chicago/Turabian StyleBusk, Henriette, Ulrik Sidenius, Line Planck Kongstad, Sus Sola Corazon, Christina Bjørk Petersen, Dorthe Varning Poulsen, Patrik Karlsson Nyed, and Ulrika Karlsson Stigsdotter. 2022. "Economic Evaluation of Nature-Based Therapy Interventions—A Scoping Review" Challenges 13, no. 1: 23. https://doi.org/10.3390/challe13010023
APA StyleBusk, H., Sidenius, U., Kongstad, L. P., Corazon, S. S., Petersen, C. B., Poulsen, D. V., Nyed, P. K., & Stigsdotter, U. K. (2022). Economic Evaluation of Nature-Based Therapy Interventions—A Scoping Review. Challenges, 13(1), 23. https://doi.org/10.3390/challe13010023







