Feasibility and Acceptability of Fear-Less: A Stepped-Care Program to Manage Fear of Cancer Recurrence in People with Metastatic Melanoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Measures
2.2.1. Demographics and Medical History
2.2.2. FCR Assessments
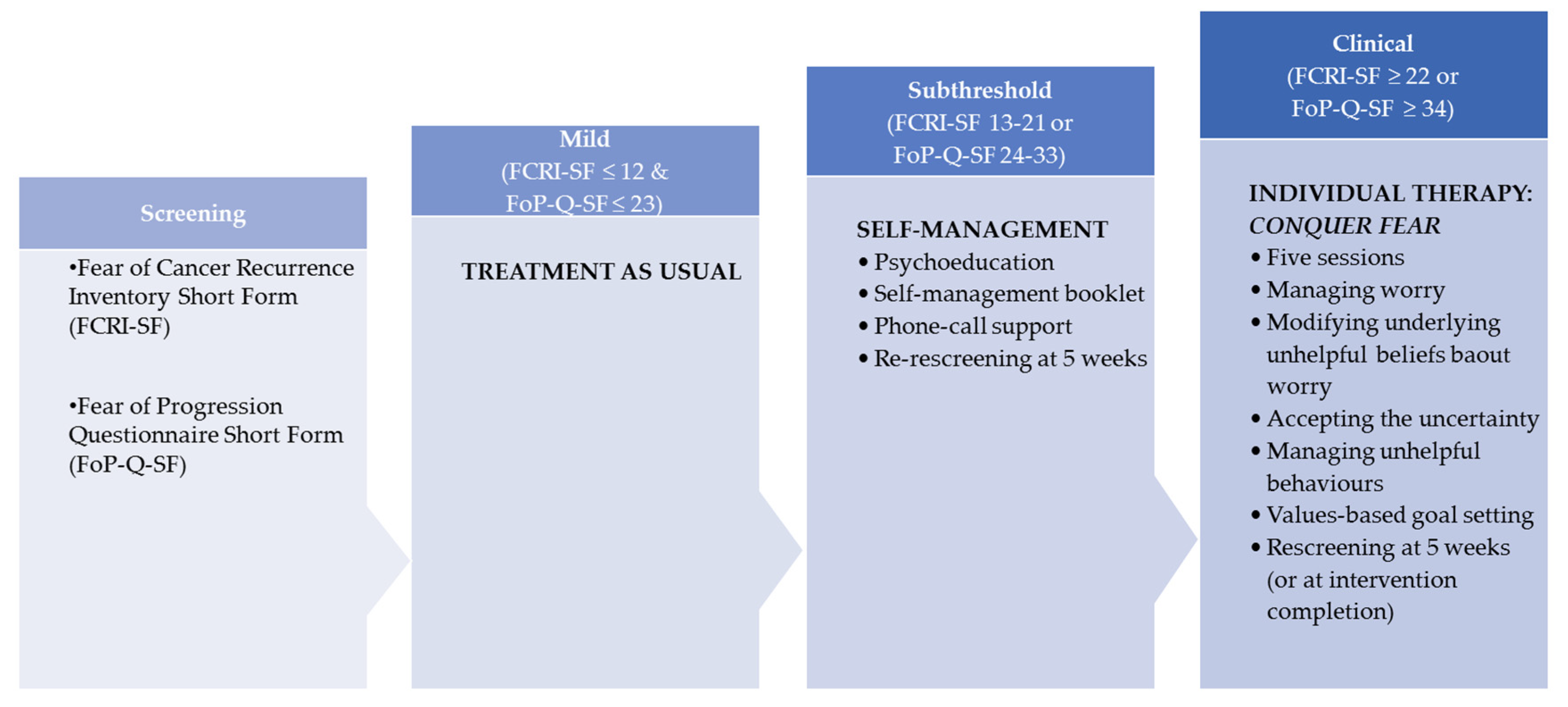
- Fear of Cancer Recurrence Inventory Short Form (FCRI-SF; [31]). The FCRI-SF is a 9-item self-report questionnaire that was used as a screening and outcome measure to assess FCR. The questionnaire assesses the presence, frequency, intensity, and duration of thoughts associated with FCR. Total scores range from 0 to 36, with higher scores indicating higher levels of FCR. A score of 13–21 was used to identify participants with subthreshold FCR [31,32], while a score of ≥22 was used to identify participants with high levels of FCR [32,33]. The FCRI-SF has shown strong internal consistency (alpha = 0.95), temporal stability (r = 0.89), and construct validity [31].
- Fear of Progression Questionnaire Short Form (FoP-Q-SF; [34]). The FoP-Q-SF is a 12-item self-report questionnaire used as a screening and outcome measure to assess the level of fear of cancer progression. Total scores range from 12 to 60. A cut-off score of 24–33 was used to suggest subthreshold levels of fear of progression [35] and a score ≥34 was used to identify participants with high levels of fear of progression [36]. FoP-Q-SF has shown high reliability (Cronbach’s alpha = 0.87 to 0.90), with evidence of construct validity [34,37].
2.2.3. Acceptability and Feasibility
- The Screening Survivor Experiences Survey was administered to all participants directly after screening. This seven-item measure included rating scales of the degree to which they agreed or disagreed that the screening questionnaires were easy to complete, easy to understand, and acceptable. Open-response items asked participants about how important they considered screening for FCR.
- The Self-Management Survivor Experiences Survey was administered after completion of the self-management intervention. The 13-item measure assessed participants’ previous experience of FCR support, the most and least useful aspects of the intervention, whether they would recommend the intervention and subjective changes in FCR.
- The Individual Therapy Survivor Experiences Survey was administered after the individual therapy. This 10-item measure assessed the participants’ previous FCR supports, experience of the individual therapy, whether they would recommend it, and subjective changes in FCR.
2.2.4. Operational Data
2.3. Study Procedures
2.3.1. Stepped Care Intervention
Step 1: Treatment as Usual
Step 2: Self-Management Intervention
Step 3. Individual Therapy
- Session 1: FCR-specific assessment and model to explain treatment, discussion of existential changes brought on by cancer, value identification and goal setting.
- Session 2: Discussion of the impact of vulnerability factors on FCR; rationale and practice of the Attention Training Technique.
- Session 3: Introduction to detached mindfulness.
- Session 4: Discussion of self-examination practices and medical surveillance, discussion of metacognitive beliefs that underpin FCR, and worry postponement.
- Session 5: Review of goal-setting task, consolidation of skills, and relapse prevention planning.
2.4. Data Analysis
3. Results
3.1. Stepped-Care Pathways
3.2. Feasibility and Acceptability
3.2.1. Screening
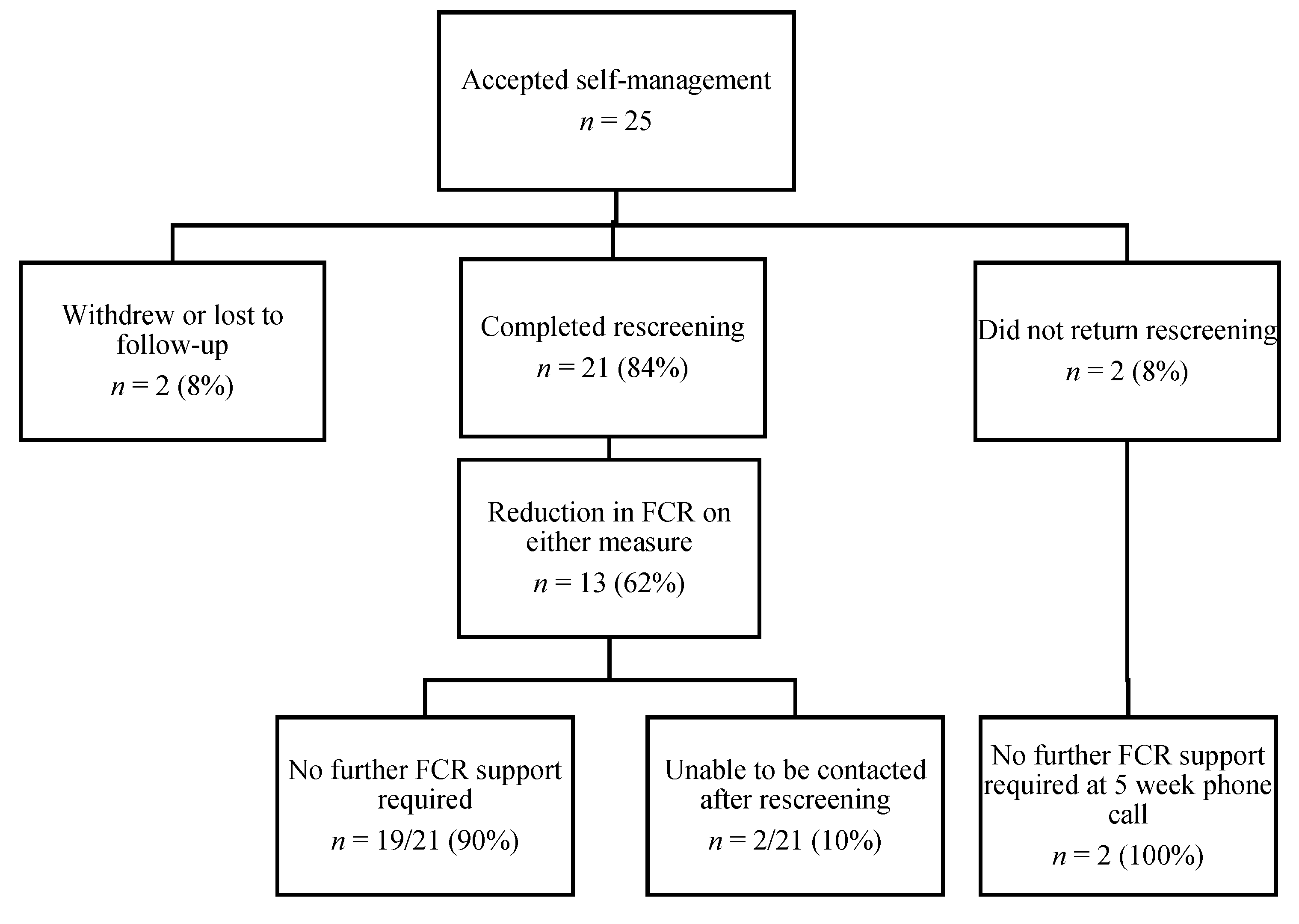
3.2.2. Self-Management Intervention
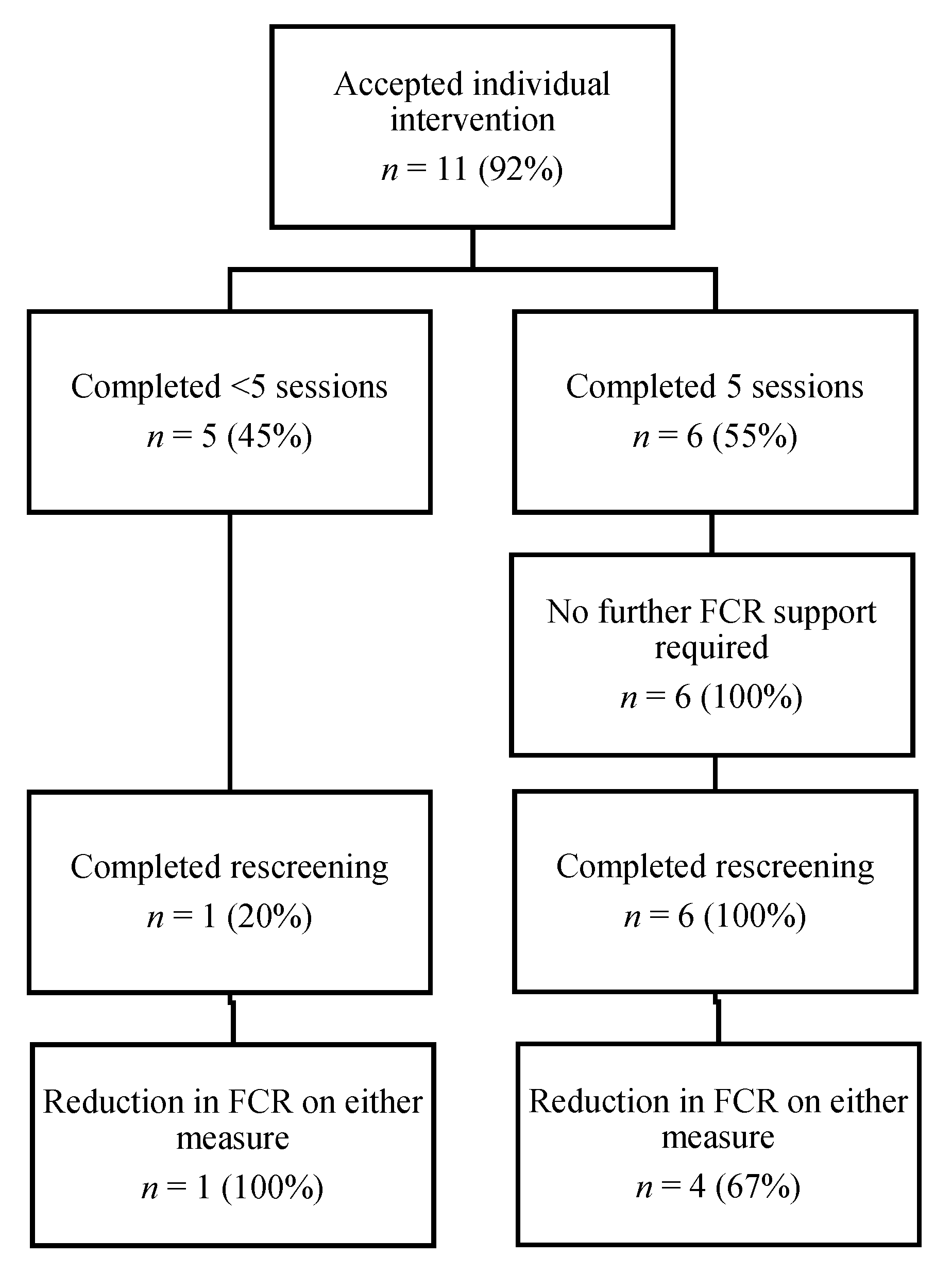
3.2.3. Individual Therapy
3.3. Impact
3.3.1. Self-Management Intervention
3.3.2. Individual Therapy
4. Discussion
4.1. Clinical Implications
4.2. Further Research
4.3. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhu, Z.; Liu, W.; Gotlieb, V. The rapidly evolving therapies for advanced melanoma—Towards immunotherapy, molecular targeted therapy, and beyond. Crit. Rev. Oncol. Hematol. 2016, 99, 91–99. [Google Scholar] [CrossRef]
- Balch, C.M.; Gershenwald, J.E.; Soong, S.J.; Thompson, J.F.; Atkins, M.B.; Byrd, D.R.; Buzaid, A.C.; Cochran, A.J.; Coit, D.G.; Ding, S.; et al. Final version of 2009 AJCC melanoma staging and classification. J. Clin. Oncol. 2009, 36, 6199–6206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Chiarion Sileni, V.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Schachter, J.; Long, G.V.; Arance, A.; Grob, J.J.; Mortier, L.; Daud, A.; Carlino, M.S.; McNeil, C.; Lotem, M.; et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2015, 372, 2521–2532. [Google Scholar] [CrossRef] [PubMed]
- Larkin, J.; Chiarion-Sileni, V.; Gonzalez, R.; Grob, J.J.; Rutkowski, P.; Lao, C.D.; Cowey, C.L.; Schadendorf, D.; Wagstaff, J.; Dummer, R.; et al. Five-Year Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2019, 381, 1535–1546. [Google Scholar] [CrossRef] [Green Version]
- Thewes, B.; Husson, O.; Poort, H.; Custers, J.A.E.; Butow, P.N.; McLachlan, S.A.; Prins, J.B. Fear of Cancer Recurrence in an Era of Personalized Medicine. J. Clin. Oncol. 2017, 35, 3275–3278. [Google Scholar] [CrossRef]
- Lebel, S.; Ozakinci, G.; Humphris, G.; Mutsaers, B.; Thewes, B.; Prins, J.; Dinkel, A.; Butow, P. University of Ottawa Fear of Cancer Recurrence Colloquium attendees. From normal response to clinical problem: Definition and clinical features of fear of cancer recurrence. Support Care Cancer 2016, 24, 3265–3268. [Google Scholar] [CrossRef] [Green Version]
- Lai-Kwon, J.; Khoo, C.; Lo, S.; Milne, D.; Mohamed, M.; Raleigh, J.; Smith, K.; Lisy, K.; Sandhu, S.; Jefford, M. The survivorship experience for patients with metastatic melanoma on immune checkpoint and BRAF-MEK inhibitors. J. Cancer Surviv. 2019, 13, 503–511. [Google Scholar] [CrossRef]
- Kasparian, N.A.; McLoone, J.K.; Butow, P.N. Psychological responses and coping strategies among patients with malignant melanoma: A systematic review of the literature. Arch. Dermatol. 2009, 145, 1415–1427. [Google Scholar] [CrossRef]
- Hart, S.L.; Latini, D.M.; Cowan, J.E.; Carroll, P.R.; CaPSURE Investigators. Fear of recurrence, treatment satisfaction, and quality of life after radical prostatectomy for prostate cancer. Support Care Cancer 2008, 16, 161–169. [Google Scholar] [CrossRef]
- Ferguson, S.; Sidani, S. Protocol of a randomized controlled trial of the fear of recurrence therapy (FORT) intervention for women with breast or gynecological cancer. BMC Cancer 2016, 16. [Google Scholar] [CrossRef] [Green Version]
- Glynne-Jones, R.; Chait, I.; Thomas, S.F. When and how to discharge cancer survivors in long term remission from follow-up: The effectiveness of a contract. Clin. Oncol. 1997, 9, 25–29. [Google Scholar] [CrossRef]
- Tauber, N.M.; O’Toole, M.S.; Dinkel, A.; Galica, J.; Humphris, G.; Lebel, S.; Maheu, C.; Ozakinci, G.; Prins, J.; Sharpe, L.; et al. Effect of Psychological Intervention on Fear of Cancer Recurrence: A Systematic Review and Meta-Analysis. J. Clin. Oncol. 2019, 37, 2899–2915. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.N.; Turner, J.; Gilchrist, J.; Sharpe, L.; Smith, A.B.; Fardell, J.E.; Tesson, S.; O’Connell, R.; Girgis, A.; Gebski, V.J.; et al. Randomized Trial of ConquerFear: A Novel, Theoretically Based Psychosocial Intervention for Fear of Cancer Recurrence. J. Clin. Oncol. 2017, 35, 4066–4077. [Google Scholar] [CrossRef] [PubMed]
- Dieng, M.; Butow, P.N.; Costa, D.S.; Morton, R.L.; Menzies, S.W.; Mireskandari, S.; Tesson, S.; Mann, G.J.; Cust, A.E.; Kasparian, N.A. Psychoeducational Intervention to Reduce Fear of Cancer Recurrence in People at High Risk of Developing Another Primary Melanoma: Results of a Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 4405–4414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herschbach, P.; Book, K.; Dinkel, A.; Berg, P.; Waadt, S.; Duran, G.; Engst-Hastreiter, U.; Henrich, G. Evaluation of two group therapies to reduce fear of progression in cancer patients. Support Care Cancer 2010, 18, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Van de Wal, M.; Thewes, B.; Gielissen, M.; Speckens, A.; Prins, J. Efficacy of Blended Cognitive Behavior Therapy for High Fear of Recurrence in Breast, Prostate, and Colorectal Cancer Survivors: The SWORD Study, a Randomized Controlled Trial. J. Clin. Oncol. 2017, 35, 2173–2183. [Google Scholar] [CrossRef] [PubMed]
- Humphris, G.; Rogers, S. AFTER and beyond: Cancer recurrence fears and a test of an intervention in oral and oropharyngeal patients. Soc. Sci. Dent. 2012, 2, 29–38. [Google Scholar]
- Lichtenthal, W.G.; Corner, G.W.; Slivjak, E.T.; Roberts, K.E.; Li, Y.; Breitbart, W.; Lacey, S.; Tuman, M.; DuHamel, K.N.; Blinder, V.S.; et al. A pilot randomized controlled trial of cognitive bias modification to reduce fear of breast cancer recurrence. Cancer 2017, 123, 1424–1433. [Google Scholar] [CrossRef] [Green Version]
- Otto, A.K.; Szczesny, E.C.; Soriano, E.C.; Laurenceau, J.P.; Siegel, S.D. Effects of a randomized gratitude intervention on death-related fear of recurrence in breast cancer survivors. Health Psychol. 2016, 35, 1320–1328. [Google Scholar] [CrossRef]
- Fardell, J.E.; Thewes, B.; Turner, J.; Gilchrist, J.; Sharpe, L.; Smith, A.; Girgis, A.; Butow, P. Fear of cancer recurrence: A theoretical review and novel cognitive processing formulation. J Cancer Surviv. 2016, 10, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.; Shaw, J.; Vaccaro, L.; Sharpe, L.; Dhillon, H.; Smith, B.; PoCoG FCR Interest Group. A research agenda for fear of cancer recurrence: A Delphi study conducted in Australia. Psychooncology 2019, 28, 989–996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.B.; Bamgboje-Ayodele, A.; Butow, P.; Klein, B.; Turner, J.; Sharpe, L.; Fardell, J.; Beatty, L.; Pearce, A.; Thewes, B.; et al. iConquerFear Community Advisory Group, Girgis, A. Development and usability evaluation of an online self-management intervention for fear of cancer recurrence (iConquerFear). Psychooncology 2020, 29, 98–106. [Google Scholar] [CrossRef]
- Lyhne, J.D.; Frostholm, L.; Fink, P.; Jensen, L.H. Study protocol: A randomized controlled trial comparing the efficacy of therapist guided internet-delivered cognitive therapy (TG-iConquerFear) with augmented treatment as usual in reducing fear of cancer recurrence in Danish colorectal cancer survivors. BMC Cancer 2020, 20, 223. [Google Scholar] [CrossRef] [PubMed]
- Lisy, K.; Langdon, L.; Piper, A.; Jefford, M. Identifying the most prevalent unmet needs of cancer survivors in Australia: A systematic review. Asia Pac. J. Clin. Oncol. 2019, 15, e68–e78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cancer Australia. Recommendations for the Identification and Management of Fear of Cancer Recurrence in Adult Cancer Survivors; Australian Government: Sydney, NSW, Australia, 2013.
- Bower, P.; Gilbody, S. Stepped care in psychological therapies: Access, effectiveness and efficiency. Narrative literature review. Br. J. Psychiatry. 2005, 186. [Google Scholar] [CrossRef] [Green Version]
- Zhou, E.S.; Michaud, A.L.; Recklitis, C.J. Developing efficient and effective behavioral treatment for insomnia in cancer survivors: Results of a stepped care trial. Cancer 2020, 126, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Kopelovich, S.L.; Strachan, E.; Sivec, H.; Kreider, V. Stepped Care as an Implementation and Service Delivery Model for Cognitive Behavioral Therapy for Psychosis. Community Ment. Health J. 2019, 55, 755–767. [Google Scholar] [CrossRef]
- Jansen, F.; Lissenberg-Witte, B.I.; Krebber, A.M.H.; Cuijpers, P.; de Bree, R.; Becker-Commissaris, A.; Smit, E.F.; van Straten, A.; Eeckhout, G.M.; Beekman, A.T.F.; et al. Stepped care targeting psychological distress in head and neck cancer and lung cancer patients: Which groups specifically benefit? Secondary analyses of a randomized controlled trial. Support Care Cancer 2019, 27, 4543–4553. [Google Scholar] [CrossRef] [Green Version]
- Simard, S.; Savard, J. Fear of Cancer Recurrence Inventory: Development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer 2009, 17, 241–251. [Google Scholar] [CrossRef]
- Fardell, J.E.; Jones, G.; Smith, A.B.; Lebel, S.; Thewes, B.; Costa, D.; Tiller, K.; Simard, S.; Feldstain, A.; Beattie, S.; et al. Exploring the screening capacity of the Fear of Cancer Recurrence Inventory-Short Form for clinical levels of fear of cancer recurrence. Psychooncology 2018, 27, 492–499. [Google Scholar] [CrossRef]
- Ng, D.W.L.; Kwong, A.; Suen, D.; Chan, M.; Or, A.; Ng, S.S.; Foo, C.C.; Fielding, B.F.S.; Lam, W.W.T. Fear of cancer recurrence among Chinese cancer survivors: Prevalence and associations with metacognition and neuroticism. Psychooncology 2019, 28, 1243–1251. [Google Scholar] [CrossRef]
- Mehnert, A.; Herschbach, P.; Berg, P.; Henrich, G.; Koch, U. Fear of progression in breast cancer patients—Validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z. Fur Psychosom. Med. Psychother. 2006, 52, 274–288. [Google Scholar] [CrossRef]
- Mehnert, A.; Berg, P.; Henrich, G.; Herschbach, P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology 2009, 18, 1273–1280. [Google Scholar] [CrossRef]
- Herschbach, P.; Berg, P.; Waadt, S.; Duran, G.; Engst-Hastreiter, U.; Henrich, G.; Book, K.; Dinkel, A. Group psychotherapy of dysfunctional fear of progression in patients with chronic arthritis or cancer. Psychother. Psychosom. 2010, 79, 31–38. [Google Scholar] [CrossRef]
- Hinz, A.; Mehnert, A.; Ernst, J.; Herschbach, P.; Schulte, T. Fear of progression in patients 6 months after cancer rehabilitation-a- validation study of the fear of progression questionnaire FoP-Q-12. Support Care Cancer 2015, 23, 1579–1587. [Google Scholar] [CrossRef]
- Tsai, W.Y.; Chi, Y.; Chen, C.M. Interval estimation of binomial proportion in clinical trials with a two-stage design. Stat. Med. 2008, 27, 15–35. [Google Scholar] [CrossRef] [Green Version]
- Butow, P.; Sharpe, L.; Thewes, B.; Turner, J.; Gilchrist, J.; Beith, J. Fear of Cancer Recurrence: A Practical Guide for Clinicians. Oncology 2018, 32, 32–38. [Google Scholar]
- Berrett-Abebe, J.; Cadet, T.; Nekhlyudov, L.; Vitello, J.; Maramaldi, P. Impact of an Interprofessional Primary Care Training on Fear of Cancer Recurrence on Clinicians’ Knowledge, Self-Efficacy, Anticipated Practice Behaviors, and Attitudes Toward Survivorship Care. J. Cancer Educ. 2019, 34, 505–511. [Google Scholar] [CrossRef]
- van Helmondt, S.J.; van der Lee, M.L.; van Woezik, R.A.M.; Lodder, P.; de Vries, J. No effect of CBT-based online self-help training to reduce fear of cancer recurrence: First results of the CAREST multicenter randomized controlled trial. Psychooncology 2020, 29, 86–97. [Google Scholar] [CrossRef]
- Sharpe, L.; Turner, J.; Fardell, J.E.; Thewes, B.; Smith, A.B.; Gilchrist, J.; Beith, J.; Girgis, A.; Tesson, S.; Day, S.; et al. Psychological intervention (ConquerFear) for treating fear of cancer recurrence: Mediators and moderators of treatment efficacy. J. Cancer Surviv. 2019, 13, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, J.G.E.; Atema, V.; Mewes, J.C.; van Leeuwen, M.; Oldenburg, H.S.A.; van Beurden, M.; Hunter, M.S.; van Harten, W.H.; Aaronson, N.K.; Retèl, V.P. Cost-utility, cost-effectiveness, and budget impact of Internet-based cognitive behavioral therapy for breast cancer survivors with treatment-induced menopausal symptoms. Breast Cancer Res. Treat. 2019, 178, 573–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thewes, B.; Lebel, S.; Seguin Leclair, C.; Butow, P. A qualitative exploration of fear of cancer recurrence (FCR) amongst Australian and Canadian breast cancer survivors. Support Care Cancer 2016, 24, 2269–2276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curran, L.; Sharpe, L.; MacCann, C.; Butow, P. Testing a model of fear of cancer recurrence or progression: The central role of intrusions, death anxiety and threat appraisal. J. Behav. Med. 2020, 43, 225–236. [Google Scholar] [CrossRef]
- Thewes, B.; Butow, P.; Zachariae, R.; Christensen, S.; Simard, S.; Gotay, C. Fear of cancer recurrence: A systematic literature review of self-report measures. Psychooncology 2012, 21, 571–587. [Google Scholar] [CrossRef] [PubMed]

| FCR Screening Subcategories N = 61 | Total Sample | |||
|---|---|---|---|---|
| No FCR | Subthreshold FCR | Clinical FCR | ||
| n (%) | 22 (36%) | 27 (44%) | 12 (20%) | 61 |
| Age | ||||
| Mean (SD) | 69.2 (9.6) | 60.0 (10.7) | 50.3 (5.4) | 61.4 (11.6) |
| Minimum | 47 | 36 | 39 | 36 |
| Maximum | 82 | 76 | 60 | 82 |
| Sex | ||||
| Male (%) | 16(73%) | 19 (70%) | 6 (50%) | 41 (67%) |
| Female (%) | 6 (27%) | 8 (30%) | 6 (50%) | 20 (33%) |
| Treatment Agent Currently or Previously Received | ||||
| Immunotherapies (%) | 18 (82%) | 19 (70%) | 6 (50%) | 43 (70%) |
| Targeted therapies (%) | 2 (9%) | 6 (22%) | 3 (25%) | 11 (18%) |
| Both immunotherapies and targeted therapies (%) | 2 (9%) | 2 (7%) | 3 (25%) | 7 (11%) |
| Treatment Status | ||||
| Having active treatment (%) | 14 (64%) | 14 (52%) | 9 (75%) | 37 (61%) |
| Treatment stopped a (%) | 8 (36%) | 13 (48%) | 3 (25%) | 24 (39%) |
| FCRI-SF | ||||
| Mean (SD) | 6.95 (3.12) | 17.22 (5.37) | 23.42 (4.93) | 14.74 (7.77) |
| Range | 0, 11 | 6, 33 | 12, 31 | 0, 33 |
| FoP-Q-SF | 16.82 (3.79) | 26.37 (6.41) | 38.92 (9.26) | |
| Mean (SD) | 25.39 (10.12) | |||
| Range | 12–23 | 15–43 | 20–54 | 12–54 |
| Self-Management | Individual Therapy | |
|---|---|---|
| n | 21 | 7 |
| FCRI-SF | ||
| Pre-intervention mean (SD) | 17.67 (6.03) | 24.29 (4.19) |
| Post-intervention mean (SD) | 16.90 (7.69) | 20.57 (6.35) |
| FoP-Q-SF | ||
| Pre-intervention mean (SD) | 29.14 (8.21) | 37.29 (8.56) |
| Post-intervention mean (SD) | 29.00 (7.79) | 33.71 (7.87) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lynch, F.A.; Katona, L.; Jefford, M.; Smith, A.B.; Shaw, J.; Dhillon, H.M.; Ellen, S.; Phipps-Nelson, J.; Lai-Kwon, J.; Milne, D.; et al. Feasibility and Acceptability of Fear-Less: A Stepped-Care Program to Manage Fear of Cancer Recurrence in People with Metastatic Melanoma. J. Clin. Med. 2020, 9, 2969. https://doi.org/10.3390/jcm9092969
Lynch FA, Katona L, Jefford M, Smith AB, Shaw J, Dhillon HM, Ellen S, Phipps-Nelson J, Lai-Kwon J, Milne D, et al. Feasibility and Acceptability of Fear-Less: A Stepped-Care Program to Manage Fear of Cancer Recurrence in People with Metastatic Melanoma. Journal of Clinical Medicine. 2020; 9(9):2969. https://doi.org/10.3390/jcm9092969
Chicago/Turabian StyleLynch, Fiona A, Lynda Katona, Michael Jefford, Allan Ben Smith, Joanne Shaw, Haryana M Dhillon, Steve Ellen, Jo Phipps-Nelson, Julia Lai-Kwon, Donna Milne, and et al. 2020. "Feasibility and Acceptability of Fear-Less: A Stepped-Care Program to Manage Fear of Cancer Recurrence in People with Metastatic Melanoma" Journal of Clinical Medicine 9, no. 9: 2969. https://doi.org/10.3390/jcm9092969
APA StyleLynch, F. A., Katona, L., Jefford, M., Smith, A. B., Shaw, J., Dhillon, H. M., Ellen, S., Phipps-Nelson, J., Lai-Kwon, J., Milne, D., Russell, L., Dax, V., Diggens, J., Kent, H., Button-Sloan, A., Elliott, J., Shackleton, M., Burridge, H., & Ftanou, M. (2020). Feasibility and Acceptability of Fear-Less: A Stepped-Care Program to Manage Fear of Cancer Recurrence in People with Metastatic Melanoma. Journal of Clinical Medicine, 9(9), 2969. https://doi.org/10.3390/jcm9092969






