Treatment of Mandible Fractures Using a Miniplate System: A Retrospective Analysis
Abstract
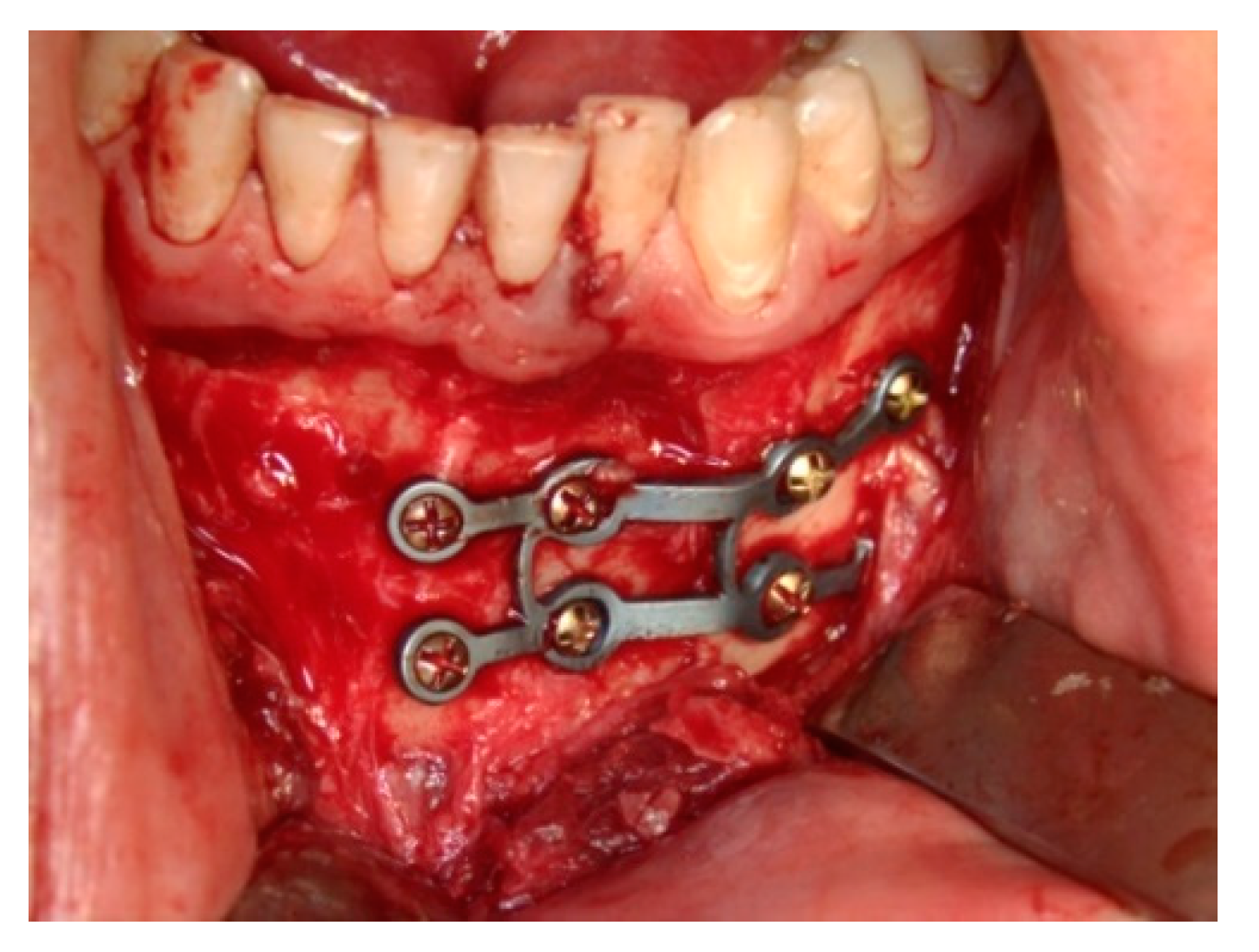
:1. Introduction
2. Experimental Section
2.1. Pre- and Intra-Operative Data Assessment
2.2. Surgical Procedure
2.3. Post-Operative Data Assessment
3. Results
3.1. Pre- and Intra-Operative Data Assessment
3.2. Fracture Assessment
3.3. Post-Operative Data Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sukegava, S.; Kanno, T.; Masui, M.; Sukegawa-Takahashi, Y.; Kishimoto, T.; Sato, A.; Furuki, Y. A retrospective comparative study of mandibular fracture treatment with internal fixation using reconstruction plate versus miniplates. J. Craniomaxillofac. Surg. 2019, 47, 1175–1180. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Junior, P.D.; Senko, R.A.; Momesso, N.R.; Izidoro, J.H.; Padovan, L.E.M.; Viswanath, A. Occlusal instability results in increased complication rates after treatment of mandibular fractures. J. Oral Maxillofac. Surg. 2020, 78, 1163.e1–1163.e7. [Google Scholar] [CrossRef] [PubMed]
- Gutta, R.; Tracy, K.; Johnson, C.; James, L.E.; Krishman, D.G.; Marciani, R. Outcomes of mandible fracture treatment at an academic tertiary hospital: A 5-year analysis. J. Oral Maxillofac. Surg. 2014, 72, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Ramos, A.; Semedo, T.; Mesnard, M. Study of fixation of a mandibular plate for favourable fractures of the mandibular angle: Numerical predictions. Br. J. Oral Maxillofac. Surg. 2020, 58, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Doshi, J.; Patel, C.; Prajapati, K.J.; Modi, D.; Shah, D.; Patel, M. A comparative study of three dimensional stainless steel plate versus two dimensional stainless steel miniplate in the management of mandibular symphysis and parasymphysis fracture. Nat. J. Integr. Res. Med. 2020, 11, 14–20. [Google Scholar]
- Checanovic, B.R. Fixation of mandibular angle fractures: In vitro biomechanical assessments and computer-based studies. Oral Maxillofac. Surg. 2013, 17, 251–268. [Google Scholar] [CrossRef]
- Moore, E.; Bayrak, S.; Moody, M.; Key, J.M.; Vural, E. Hardware removal rates for mandibular angle fractures: Comparing the 8-hole strut and champy plates. J. Craniofac. Surg. 2013, 24, 163–165. [Google Scholar] [CrossRef]
- Höfer, S.H.; Ha, L.; Ballon, A.; Sader, R.; Landes, C. Treatment of mandibular angle fractures line obliqua plate versus grid plate. J. Craniomaxillofac. Surg. 2012, 40, 807–811. [Google Scholar] [CrossRef]
- Wusiman, P.; Yarbag, A.; Mijiti, A.; Moming, A. Three dimensional versus standard miniplate fixation in management of mandibular fractures: A systematic review and meta-analysis. J. Craniomaxillofac. Surg. 2016, 44, 1646–1654. [Google Scholar] [CrossRef]
- Singh, A.; Arunkumar, K.V. Standard 3D titanium miniplate versus locking 3D miniplate in fracture of mandible: A prospective comparative study. J. Maxillofac. Oral Surg. 2016, 15, 164–172. [Google Scholar] [CrossRef]
- Hochuli-Vieira, E.; Ha, T.K.L.; Pereira-Filho, V.A.; Landes, C.A. Use of rectangular grid miniplates for fracture fixation at the mandibular angle. J. Oral Maxillofac. Surg. 2011, 69, 1436–1441. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; El-Shawkawy, T.M.; El-Ghareeb, T.I.; Chrcanovic, B.R. Three-dimensional versus standard miniplate fixation in the management of mandibular angle fractures: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2014, 43, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Ellis, E. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2014, 72, 2197–2211. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, S.; Singh, M.; Modi, P.; Walia, E.; Aggarwal, R. Comparison of 3D plate and locking plate in treatment of mandibular fracture-A clinical study. Oral Maxillofac. Surg. 2017, 21, 383–390. [Google Scholar] [CrossRef]
- Zhan, S.; Jiang, Y.; Cheng, Z.; Ye, J. A meta-analysis comparing the 2.0mm locking plate system with the 2mm nonlocking plate system in treatment of mandible fractures. J. Craniofac. Surg. 2014, 25, 2094–20197. [Google Scholar] [CrossRef]
- Spiessl, B. Internal Fxation of the Mandible; Springer: New York, NY, USA, 1989. [Google Scholar]
- Champy, M.; Lodde, J.P.; Schmitt, R.; Jaeger, J.K.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J. Maxillofac. Surg. 1978, 6, 14–21. [Google Scholar] [CrossRef]
- Silajiding, K.; Wusiman, P.; Yusufu, B.; Moming, A. Three dimensional versus standard miniplate fixation in the management of mandibular fractures: A meta-analysis of randomized controlled trials. Kaohsiung J. Med. Sci. 2017, 33, 462–472. [Google Scholar] [CrossRef]
- De Oliveira, J.C.S.; Moura, L.B.; Menezes, J.D.S.; Gabrielli, A.C.; Pereira Filho, V.A.; Hichuli-Vieira, E. Three-dimensional strut plate for the treatment of mandibular fractures: A systematic review. Int. J. Oral Maxillofac. Surg. 2018, 47, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Wei, B.; Gu, D.; Yin, G.; Xu, D.; Zhang, X.; Kong, D. The 3-dimensional miniplate is more effective than the standard miniplate for the management of mandibular fractures: A meta-analysis. Eur. J. Med. Res. 2017, 22, 5. [Google Scholar] [CrossRef]
- Mohd, Y.Q.; Redy, S.; Sinha, R.; Agarwal, A.; Fatima, U.; Abidullah, M. Three-dimensional miniplate: For the management of mandibular parasymphysis fractures. Ann. Maxillofac. Surg. 2019, 9, 333–3339. [Google Scholar] [CrossRef]
- Gooday, R.H.B. Management of fractures of the mandibular body and symphysis. Oral Maxillofac. Surg. Clin. N. Am. 2013, 25, 601–616. [Google Scholar] [CrossRef] [PubMed]
- Stacey, D.H.; Doyle, J.F.; Mount, D.L. Management of mandible fractures. Plast. Reconstr. Surg. 2006, 117, 48. [Google Scholar] [CrossRef] [PubMed]
- An, W.; Ainiwaer, A.; Wusiman, P.; Ali, G.; Moming, A. Surgical management of mandibular angle fractures. J. Craniofac. Surg. 2018, 29, 1702–1708. [Google Scholar] [CrossRef] [PubMed]
- Khavanin, N.; Jazayeri, H.; Xu, T.; Pedreira, R.; Lopez, J.; Reddy, S.; Shamliyan, T.; Peacock, Z.; Dorafshar, A. Management of teeth in the line of mandibular angle fractures treated with open reduction and internal fixation: A systematic review and meta-analysis. Plast. Reconstr. Surg. 2019, 144, 1393–1402. [Google Scholar] [CrossRef]

| Patient’s Data | Number of Patients (n) | |
|---|---|---|
| Gender | ||
| Male | 247 | |
| Female | 89 | |
| Age | ||
| 11–20 | 102 | |
| 21–40 | 157 | |
| 41–60 | 61 | |
| >60 | 16 | |
| Co-morbidities | ||
| Cardiovascular disease or coagulation alterations | 49 | |
| Respiratory diseases | 31 | |
| Infectious disease | 8 | |
| Diabetes mellitus, Osteoporosis or Tumor | 5 | |
| Medication | ||
| Thyroid hormones or symphatomimetic drugs | 10 | |
| Angiotensinconverting-enzyme (ACE) inhibitors | 07 | |
| Acetylsalicylic acid (ASS) and Beta-Blocker drugs | 06 | |
| Anti-depressant and anti-epileptics | 4 | |
| Insulin | 3 | |
| Benzodiazepines, opioids or coumarin anticoagulant therapy | 2 |
| Mandibular Fractures | Number of Patients (n) | |
|---|---|---|
| Localization | ||
| Anterior mandible | 159 | |
| Mandibular angle | 129 | |
| Mandibular body | 108 | |
| Mandibular displacement | ||
| None | 83 | |
| Weak | 152 | |
| Moderate | 118 | |
| Strong | 38 |
| Post-Operative Complications | Number of Patients (n) | |
|---|---|---|
| Minor complications | ||
| Infections | Total: 10 | |
| - Abscess | 6 | |
| - Fistula | 2 | |
| - Local infiltration | 1 | |
| - Osteomyelitis | 1 | |
| Dehiscence or healing complications | 26 | |
| Plate exposition | 2 | |
| Sensibility disturbance | Total: 156 | |
| - Before plate removal | 156 | |
| - After plate removal | 22 | |
| Screw loosening | 6 | |
| Major complications | ||
| Pseudoarthrosis | 2 | |
| New platting | 5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bohner, L.; Beiglboeck, F.; Schwipper, S.; Lustosa, R.M.; Pieirna Marino Segura, C.; Kleinheinz, J.; Jung, S. Treatment of Mandible Fractures Using a Miniplate System: A Retrospective Analysis. J. Clin. Med. 2020, 9, 2922. https://doi.org/10.3390/jcm9092922
Bohner L, Beiglboeck F, Schwipper S, Lustosa RM, Pieirna Marino Segura C, Kleinheinz J, Jung S. Treatment of Mandible Fractures Using a Miniplate System: A Retrospective Analysis. Journal of Clinical Medicine. 2020; 9(9):2922. https://doi.org/10.3390/jcm9092922
Chicago/Turabian StyleBohner, Lauren, Fabian Beiglboeck, Stephanie Schwipper, Rômulo Maciel Lustosa, Carla Pieirna Marino Segura, Johannes Kleinheinz, and Susanne Jung. 2020. "Treatment of Mandible Fractures Using a Miniplate System: A Retrospective Analysis" Journal of Clinical Medicine 9, no. 9: 2922. https://doi.org/10.3390/jcm9092922
APA StyleBohner, L., Beiglboeck, F., Schwipper, S., Lustosa, R. M., Pieirna Marino Segura, C., Kleinheinz, J., & Jung, S. (2020). Treatment of Mandible Fractures Using a Miniplate System: A Retrospective Analysis. Journal of Clinical Medicine, 9(9), 2922. https://doi.org/10.3390/jcm9092922






