Prevalence of Hangover Resistance According to Two Methods for Calculating Estimated Blood Alcohol Concentration (eBAC)
Abstract
:1. Introduction
2. Experimental Section
2.1. Method
2.2. Design
2.3. Participants
2.4. Measures
2.4.1. Demographics
2.4.2. Alcohol Consumption Questions
2.4.3. Estimated BAC (eBAC)
2.4.4. Single Item Hangover Sensitivity/Resistance
2.5. Procedure
2.6. Statistical Analysis
3. Results
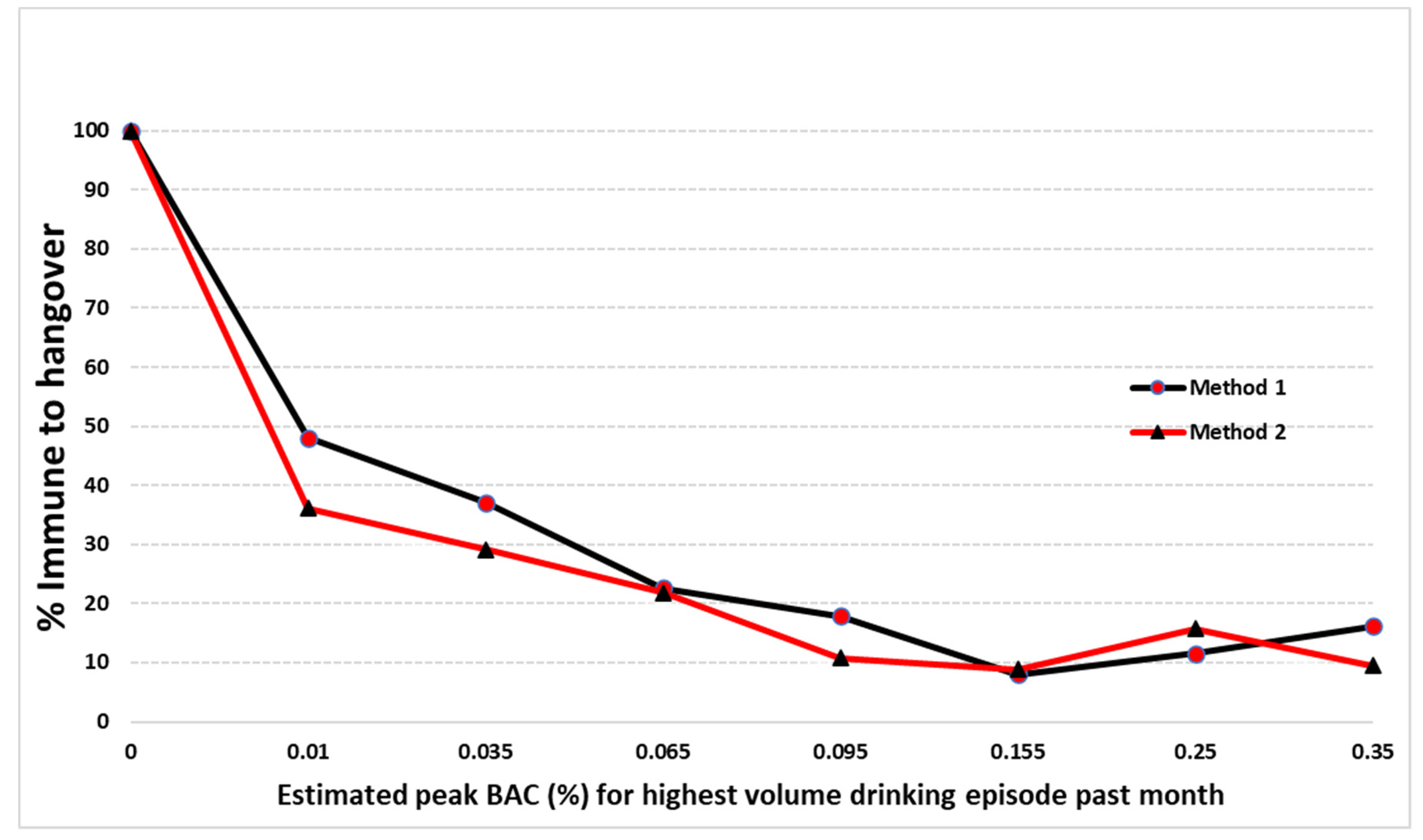
3.1. Method 1
3.2. Method 2
3.3. Comparison of Two Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Widmark Formula
Appendix B. eBAC Calculation Method 1
References
- Verster, J.C.; Scholey, A.; van de Loo, A.; Benson, S.; Stock, A.K. Updating the definition of the alcohol hangover. J. Clin. Med. 2020, 9, 823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verster, J.C.; Stephens, R.; Penning, R.; Rohsenow, D.; McGeary, J.; Levy, D.; McKinney, A.; Finnigan, F.; Piasecki, T.M.; Adan, A. The alcohol hangover research group consensus statement on best practice in alcohol hangover research. Curr. Drug Abuse Rev. 2010, 3, 116–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verster, J.C.; Kruisselbrink, L.D.; Slot, K.A.; Anogeianaki, A.; Adams, S.; Alford, C.; Arnoldy, L.; Ayre, E.; Balikji, S.; Benson, S. Sensitivity to experiencing alcohol hangovers: Reconsideration of the 0.11% Blood Alcohol Concentration (BAC) threshold for having a hangover. J. Clin. Med. 2020, 9, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiese, J.G.; Shlipak, M.G.; Browner, W.S. The alcohol hangover. Ann. Intern. Med. 2000, 132, 897–902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Penning, R.; McKinney, A.; Verster, J.C. Alcohol hangover symptoms and their contribution to the overall hangover severity. Alcohol Alcohol. 2012, 47, 248–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohsenow, D.J.; Howland, J.; Minsky, S.J.; Greece, J.; Almeida, A.; Roehrs, T.A. The Acute Hangover Scale: A new measure of immediate hangover symptoms. Addict. Behav. 2007, 32, 1314–1320. [Google Scholar] [CrossRef] [Green Version]
- Verster, J.C. The alcohol hangover–a puzzling phenomenon. Alcohol Alcohol. 2008, 43, 124–126. [Google Scholar] [CrossRef] [Green Version]
- van Schrojenstein Lantman, M.; van de Loo, A.J.; Mackus, M.; Verster, J.C. Development of a Definition for the Alcohol Hangover: Consumer Descriptions and Expert Consensus. Curr. Drug Abuse Rev. 2016, 9, 148–154. [Google Scholar] [CrossRef]
- Slutske, W.S.; Piasecki, T.M.; Hunt-Carter, E.E. Development and initial validation of the Hangover Symptoms Scale: Prevalence and correlates of Hangover Symptoms in college students. Alcohol Clin. Exp. Res. 2003, 27, 1442–1450. [Google Scholar] [CrossRef] [Green Version]
- van Schrojenstein Lantman, M.; Mackus, M.; van de Loo, A.; Verster, J.C. The impact of alcohol hangover symptoms on cognitive and physical functioning, and mood. Hum. Psychopharmacol. 2017, 32, e2623. [Google Scholar] [CrossRef]
- Stephens, R.; Grange, J.A.; Jones, K.; Owen, L. A critical analysis of alcohol hangover research methodology for surveys or studies of effects on cognition. Psychopharmacology 2014, 231, 2223–2236. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C.; Van Der Maarel, M.A.; McKinney, A.; Olivier, B.; De Haan, L. Driving during alcohol hangover among Dutch professional truck drivers. Traffic Inj. Prev. 2014, 15, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Frone, M.R.; Verster, J.C. Alcohol hangover and the workplace: A need for research. Curr. Drug Abuse Rev. 2013, 6, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Ames, G.M.; Grube, J.W.; Moore, R.S. The relationship of drinking and hangovers to workplace problems: An empirical study. J. Stud. Alcohol 1997, 58, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Verster, J. Alcohol hangover frequency, severity and interventions among Dutch college students. Alcohol Clin. Exp. Res. 2006, 30, 157A. [Google Scholar]
- Piasecki, T.M.; Robertson, B.M.; Epler, A.J. Hangover and risk for alcohol use disorders: Existing evidence and potential mechanisms. Curr. Drug Abuse Rev. 2010, 3, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Rohsenow, D.J.; Howland, J.; Winter, M.; Bliss, C.A.; Littlefield, C.A.; Heeren, T.C.; Calise, T.V. Hangover sensitivity after controlled alcohol administration as predictor of post-college drinking. J. Abnorm. Psychol. 2012, 121, 270–275. [Google Scholar] [CrossRef] [Green Version]
- Cameron, E.; French, D.P. Predicting perceived safety to drive the morning after drinking: The importance of hangover symptoms. Drug Alcohol Rev. 2016, 35, 442–446. [Google Scholar] [CrossRef]
- Verster, J.C.; Bervoets, A.C.; de Klerk, S.; Vreman, R.A.; Olivier, B.; Roth, T.; Brookhuis, K.A. Effects of alcohol hangover on simulated highway driving performance. Psychopharmacology 2014, 231, 2999–3008. [Google Scholar] [CrossRef]
- Prat, G.; Adan, A.; Sanchez-Turet, M. Alcohol hangover: A critical review of explanatory factors. Hum. Psychopharmacol. 2009, 24, 259–267. [Google Scholar] [CrossRef]
- Penning, R.; van Nuland, M.; Fliervoet, L.A.; Olivier, B.; Verster, J.C. The pathology of alcohol hangover. Curr. Drug Abuse Rev. 2010, 3, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Scholey, A.; Benson, S.; Kaufman, J.; Terpstra, C.; Ayre, E.; Verster, J.C.; Allen, C.; Devilly, G.J. Effects of Alcohol Hangover on Cognitive Performance: Findings from a Field/Internet Mixed Methodology Study. J. Clin. Med. 2019, 8, 440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verster, J.C.; van de Loo, A.J.; Adams, S.; Stock, A.-K.; Benson, S.; Scholey, A.; Alford, C.; Bruce, G. Advantages and Limitations of Naturalistic Study Designs and Their Implementation in Alcohol Hangover Research. J. Clin. Med. 2019, 8, 2160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prat, G.; Adan, A.; Perez-Pamies, M.; Sanchez-Turet, M. Neurocognitive effects of alcohol hangover. Addict. Behav. 2008, 33, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Hustad, J.T.; Carey, K.B. Using calculations to estimate blood alcohol concentrations for naturally occurring drinking episodes: A validity study. J. Stud. Alcohol 2005, 66, 130–138. [Google Scholar] [CrossRef]
- Widmark, E.M.P. Principles and Applications of Medicolegal Alcohol Determination; Biomedical Publications: Davis, CA, USA, 1981. [Google Scholar]
- Verster, J.C.; Slot, K.A.; Arnoldy, L.; van Lawick van Pabst, A.E.; van de Loo, A.J.; Benson, S.; Scholey, A. The Association between Alcohol Hangover Frequency and Severity: Evidence for Reverse Tolerance? J. Clin. Med. 2019, 8, 1520. [Google Scholar] [CrossRef] [Green Version]
- Watson, P.E.; Watson, I.D.; Batt, R.D. Prediction of blood alcohol concentrations in human subjects. Updat. Widmark Equ. J. Stud. Alcohol. 1981, 42, 547–556. [Google Scholar] [CrossRef]
- Gullberg, R.G.; Jones, A.W. Guidelines for estimating the amount of alcohol consumed from a single measurement of blood alcohol concentration: Re-evaluation of Widmark’s equation. Forensic Sci. Int. 1994, 69, 119–130. [Google Scholar] [CrossRef]
- Stowell, A.R.; Stowell, L.I. Estimation of blood alcohol concentrations after social drinking. J. Forensic Sci. 1998, 43, 14–21. [Google Scholar] [CrossRef]
- van Schrojenstein Lantman, M.; Mackus, M.; Roth, T.; Verster, J.C. Total sleep time, alcohol consumption, and the duration and severity of alcohol hangover. Nat. Sci. Sleep 2017, 9, 181–186. [Google Scholar] [CrossRef] [Green Version]
- van Schrojenstein Lantman, M.; van de Loo, A.J.; Mackus, M.; Kraneveld, A.D.; Brookhuis, K.A.; Garssen, J.; Verster, J.C. Susceptibility to alcohol hangovers: Not just a matter of being resilient. Alcohol Alcohol. 2018, 53, 241–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van de Loo, A.; Mackus, M.; van Schrojenstein Lantman, M.; Kraneveld, A.D.; Brookhuis, K.A.; Garssen, J.; Scholey, A.; Verster, J.C. Susceptibility to Alcohol Hangovers: The Association with Self-Reported Immune Status. Int. J. Environ. Res. Public Health 2018, 15, 1286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, A.; Hingson, R. The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Res. Health 2013, 35, 201–218. [Google Scholar]
- Carey, K.B.; Hustad, J.T. Are retrospectively reconstructed blood alcohol concentrations accurate? Preliminary results from a field study. J. Stud. Alcohol 2002, 63, 762–766. [Google Scholar] [CrossRef]
- Howland, J.; Rohsenow, D.J.; Allensworth-Davies, D.; Greece, J.; Almeida, A.; Minsky, S.J.; Arnedt, J.T.; Hermos, J. The incidence and severity of hangover the morning after moderate alcohol intoxication. Addiction 2008, 103, 758–765. [Google Scholar] [CrossRef] [Green Version]
- Verster, J.C.; de Klerk, S.; Bervoets, A.C.; Darren Kruisselbrink, L. Can hangover immunity be really claimed? Curr. Drug Abuse Rev. 2013, 6, 253–254. [Google Scholar] [CrossRef]
- Kruisselbrink, L.D.; Bervoets, A.C.; de Klerk, S.; van de Loo, A.; Verster, J.C. Hangover resistance in a Canadian University student population. Addict. Behav. Rep. 2017, 5, 14–18. [Google Scholar] [CrossRef]
- Huntley, G.; Treloar, H.; Blanchard, A.; Monti, P.M.; Carey, K.B.; Rohsenow, D.J.; Miranda, R. An event-level investigation of hangovers’ relationship to age and drinking. Exp. Clin. Psychopharmacol. 2015, 23, 314–323. [Google Scholar] [CrossRef] [Green Version]
- Hogewoning, A.; Van de Loo, A.; Mackus, M.; Raasveld, S.; De Zeeuw, R.; Bosma, E.; Bouwmeester, N.; Brookhuis, K.; Garssen, J.; Verster, J. Characteristics of social drinkers with and without a hangover after heavy alcohol consumption. Subst. Abuse Rehabil. 2016, 7, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Forrest, A. The estimation of Widmark’s factor. J. Forensic Sci. Soc. 1986, 26, 249–252. [Google Scholar] [CrossRef]
- Seidl, S.; Jensen, U.; Alt, A. The calculation of blood ethanol concentrations in males and females. Int. J. Legal. Med. 2000, 114, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, L.; Cramer, Y.; Zink, P. Relevance of individual parameters in the calculation of blood alcohol levels in relation to the volume of intake. Blutalkohol 1987, 24, 192–198. [Google Scholar] [PubMed]
- Benson, S.; Ayre, E.; Garrisson, H.; Wetherell, M.A.; Verster, J.C.; Scholey, A. Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort. J. Clin. Med. 2020, 9, 1154. [Google Scholar] [CrossRef] [PubMed]
- Statistics, S.S. Available online: https://www.socscistatistics.com/tests/chisquare/default2.aspx (accessed on 22 August 2020).
- Davis, C.G.; Thake, J.; Vilhena, N. Social desirability biases in self-reported alcohol consumption and harms. Addict. Behav. 2010, 35, 302–311. [Google Scholar] [CrossRef] [PubMed]
| Full Sample | Hangover Resistant | Hangover Sensitive | |
|---|---|---|---|
| Age | 23.10(4.7) | 22.95(5.1) | 23.14(4.6) |
| Height (m) | 1.71(0.1) | 1.69(0.1) * | 1.71(0.1) * |
| Weight (kg) | 70.57(15.6) | 69.93(17.7) | 70.77(15.0) |
| Standard drinks per occasion | 5.25(3.9) | 3.40(2.6) * | 5.83(4.1) * |
| Days used alcohol (30 days) | 6.97(6.7) | 4.93(6.1) * | 7.60(6.8) * |
| Days drunk (30 days) | 2.43(3.5) | 0.95(2.4) * | 2.90(3.6) * |
| Days binge (30 days) | 3.22(4.3) | 1.50(3.5) * | 3.76(4.4) * |
| Greatest number of drinks (30 days) | 7.87(6.1) | 4.72(4.8) * | 8.85(6.1) * |
| Consumption duration (hours) | 5.16(3.5) | 3.68(3.0) * | 5.62(3.5) * |
| Alcohol consumed (grams) | 78.67(61.1) | 47.23(48.1) * | 88.54(61.4) * |
| eBAC (Method 1) (N = 955) eBAC (Method 2) (N= 942) | 0.12(0.1) 0.10(0.1) | 0.08(0.1) * 0.07(0.1) * | 0.13(0.1) * 0.11(0.1) * |
| eBAC Range | % No Hangover Method 1 | % No Hangover Method 2 | χ2 | p | |
|---|---|---|---|---|---|
| Group 1 | 0 ≤ BAC < 0.02% | 48.0 (36/75) | 36.1 (53/147) | 2.95 | 0.09 |
| Group 2 | 0.02% ≤ BAC < 0.05% | 37.1 (62/167) | 29.1 (53/182) | 2.53 | 0.11 |
| Group 3 | 0.05% ≤ BAC < 0.08% | 22.6 (33/146) | 21.9 (30/137) | 0.02 | 0.89 |
| Group 4 | 0.08% ≤ BAC < 0.11% | 17.9 (22/123) | 10.8 (13/120) | 2.45 | 0.12 |
| Group 5 | 0.11 ≤ BAC < 0.20% | 8.0 (22/275) | 8.9 (22/246) | 0.15 | 0.70 |
| Group 6 | 0.20 ≤ BAC < 0.30% | 11.5 (15/131) | 15.7 (14/89) | 0.85 | 0.36 |
| Group 7 | 0.30 ≤ BAC < 0.40% | 16.2 (6/37) | 9.5 (2/21) | 0.50 | 0.48 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terpstra, C.; Scholey, A.; Verster, J.C.; Benson, S. Prevalence of Hangover Resistance According to Two Methods for Calculating Estimated Blood Alcohol Concentration (eBAC). J. Clin. Med. 2020, 9, 2823. https://doi.org/10.3390/jcm9092823
Terpstra C, Scholey A, Verster JC, Benson S. Prevalence of Hangover Resistance According to Two Methods for Calculating Estimated Blood Alcohol Concentration (eBAC). Journal of Clinical Medicine. 2020; 9(9):2823. https://doi.org/10.3390/jcm9092823
Chicago/Turabian StyleTerpstra, Chantal, Andrew Scholey, Joris C. Verster, and Sarah Benson. 2020. "Prevalence of Hangover Resistance According to Two Methods for Calculating Estimated Blood Alcohol Concentration (eBAC)" Journal of Clinical Medicine 9, no. 9: 2823. https://doi.org/10.3390/jcm9092823
APA StyleTerpstra, C., Scholey, A., Verster, J. C., & Benson, S. (2020). Prevalence of Hangover Resistance According to Two Methods for Calculating Estimated Blood Alcohol Concentration (eBAC). Journal of Clinical Medicine, 9(9), 2823. https://doi.org/10.3390/jcm9092823






