Comparison of Changes in the Condylar Volume and Morphology in Skeletal Class III Deformities Undergoing Orthognathic Surgery Using a Customized versus Conventional Miniplate: A Retrospective Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
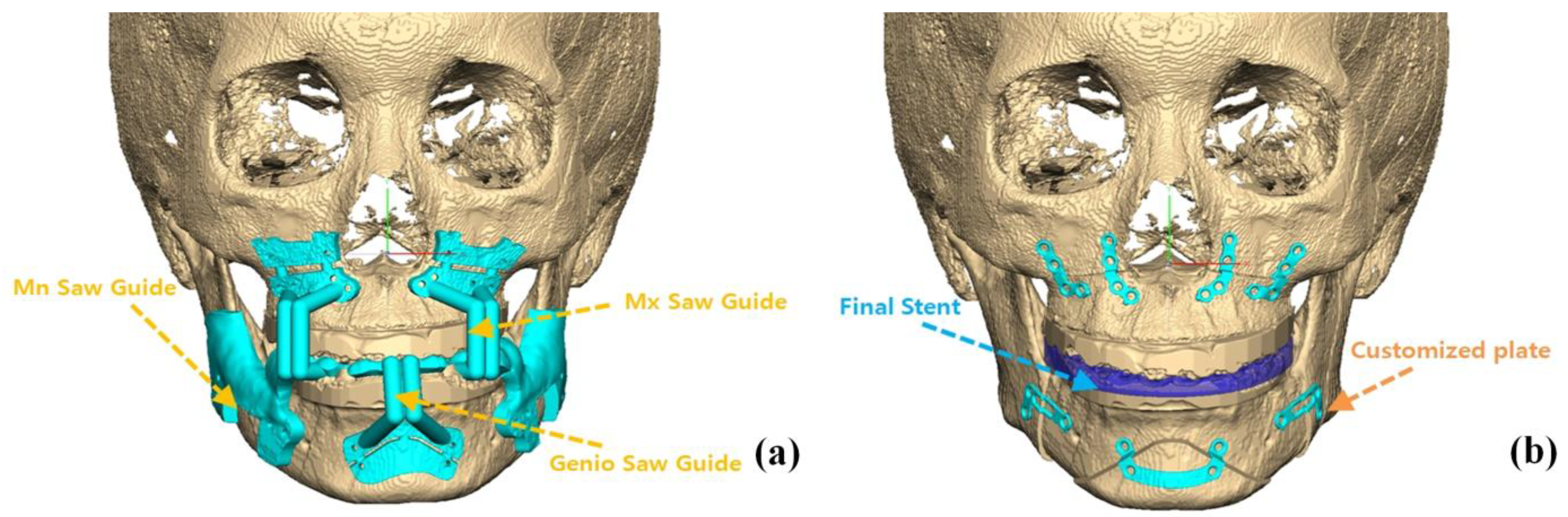
2.2. Treatment Protocols and CBCT Imaging
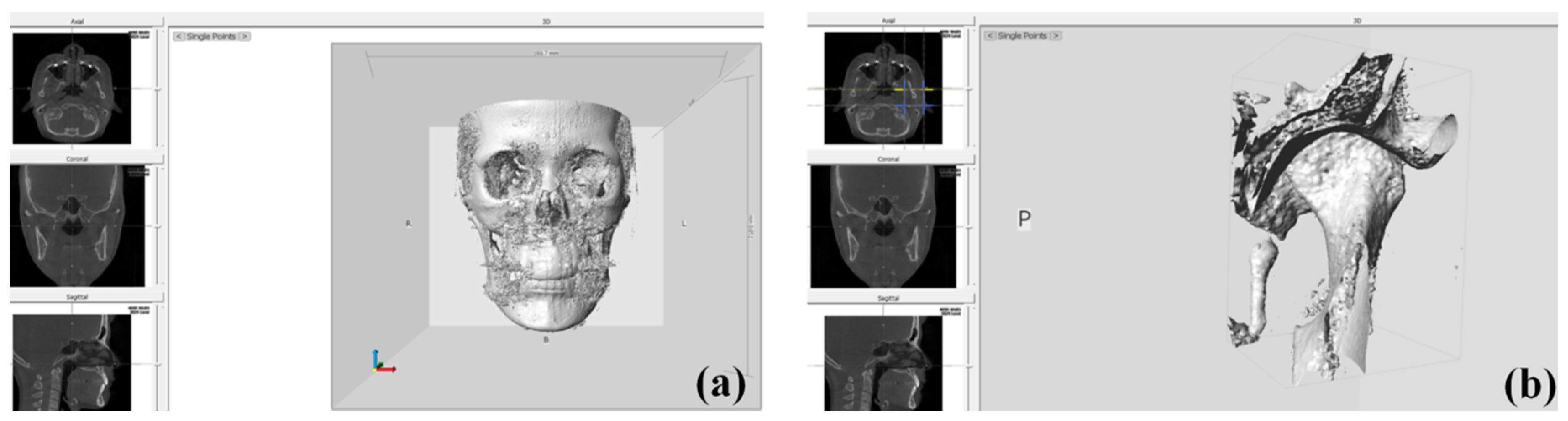
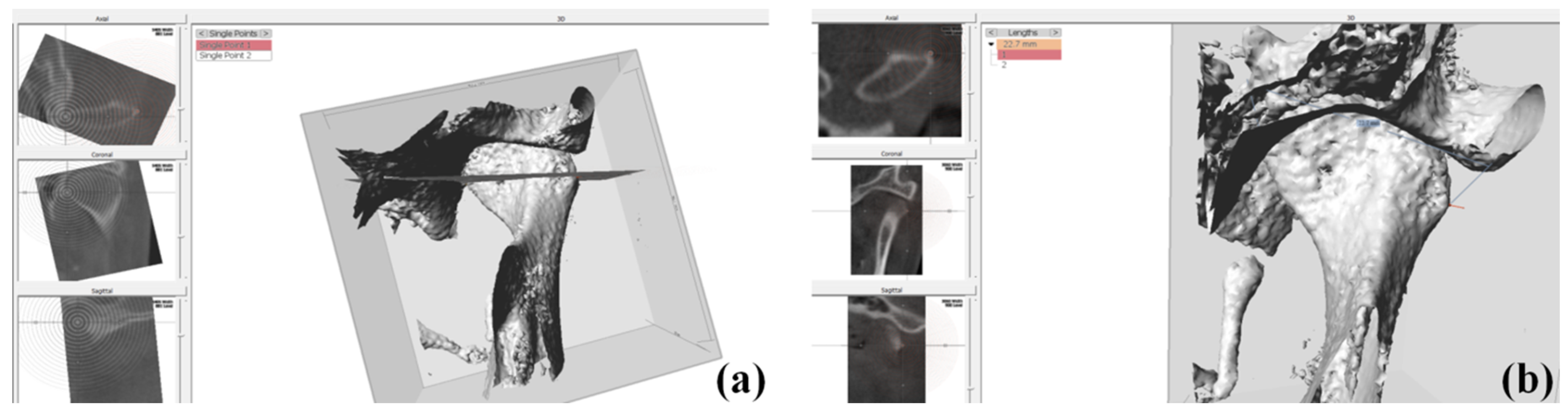
2.3. Condylar Volume Rendering
2.4. Evaluation of Skeletal Landmark Changes after Surgery
2.5. Statistical Analysis
3. Results
3.1. Condylar Morphological Changes (T0 vs.T2)
3.2. Skeletal Landmark Changes (T1 vs. T2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Trauner, R.; Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg. Oral Med. Oral Pathol. 1957, 10, 677–689. [Google Scholar] [CrossRef]
- Verhelst, P.J.; Van der Cruyssen, F.; Laat, A.D.; Jacobs, R.; Politis, C. The Biomechanical Effect of the Sagittal Split Ramus Osteotomy on the Temporomandibular Joint: Current Perspectives on the Remodeling Spectrum. Front. Physiol. 2019, 10, 1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Epker, B.N.; Wessberg, G.A. Mechanisms of early skeletal release following surgical advancement of the mandible. Br. J. Oral Surg. 1982, 20, 175–182. [Google Scholar] [CrossRef]
- Park, Y.W.; Kang, H.S.; Lee, J.H. Comparative study on long-term stability in mandibular sagittal split ramus osteotomy: Hydroxyapatite/poly-L-lactide mesh versus titanium miniplate. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joss, C.U.; Vassalli, I.M. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: A systematic review. J. Oral Maxillofac. Surg. 2009, 67, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Mobarak, K.A.; Espeland, L.; Krogstad, O.; Lyberg, T. Mandibular advancement surgery in high-angle and low-angle class II patients: Different long-term skeletal responses. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 368–381. [Google Scholar] [CrossRef]
- Da Silva, R.J.; Valadares Souza, C.V.; Souza, G.A.; Ambrosano, G.M.B.; Freitas, D.Q.; Sant’Ana, E.; de Oliveira-Santos, C. Changes in condylar volume and joint spaces after orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2018, 47, 511–517. [Google Scholar] [CrossRef]
- Lin, H.H.; Chang, H.W.; Lo, L.J. Development of customized positioning guides using computer-aided design and manufacturing technology for orthognathic surgery. Int. J. Comput. Assist. Radiol. Surg. 2015, 10, 2021–2033. [Google Scholar] [CrossRef]
- Kim, Y.J.; Oh, K.M.; Hong, J.S.; Lee, J.H.; Kim, H.M.; Reyes, M.; Cevinades, L.H.; Park, Y.H. Do patients treated with bimaxillary surgery have more stable condylar positions than those who have undergone single-jaw surgery? J. Oral Maxillofac. Surg. 2012, 70, 2143–2152. [Google Scholar] [CrossRef]
- Brunso, J.; Franco, M.; Constantinescu, T.; Barbier, L.; Santamaria, J.A.; Alvarez, J. Custom-Machined Miniplates and Bone-Supported Guides for Orthognathic Surgery: A New Surgical Procedure. J. Oral Maxillofac. Surg. 2016, 74, 1061.e1–1061.e12. [Google Scholar] [CrossRef]
- Kim, J.W.; Kim, J.C.; Jeong, C.G.; Cheon, K.J.; Cho, S.W.; Park, I.Y.; Yang, B.E. The accuracy and stability of the maxillary position after orthognathic surgery using a novel computer-aided surgical simulation system. BMC Oral Health 2019, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Lo, L.J.; Weng, J.L.; Ho, C.T.; Lin, H.H. Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognathic surgery in patients with prognathism. PLoS ONE 2018, 13, e0200589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.H.; Cho, S.W.; Kim, J.W.; Ahn, H.J.; Kim, Y.H.; Yang, B.E. Three-dimensional assessment of condylar position following orthognathic surgery using the centric relation bite and the ramal reference line. Medicine 2019, 98, e14931. [Google Scholar] [CrossRef]
- Kim, J.W.; Kim, J.C.; Cheon, K.J.; Cho, S.W.; Kim, Y.H.; Yang, B.E. Computer-Aided Surgical Simulation for Yaw Control of the Mandibular Condyle and Its Actual Application to Orthognathic Surgery: A One-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2018, 15, 2380. [Google Scholar] [CrossRef] [Green Version]
- Wan, Y.; Jackson, T.; Chung, C.; Gao, F.; Blakey, G.; Nguyen, T. Comparison of condylar position in orthognathic surgery cases treated with virtual surgical planning vs. conventional model planning. Orthod. Craniofac. Res. 2019, 22, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: An update and extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulsen, H.U.; Karle, A. Computer tomographic and radiographic changes in the temporomandibular joints of two young adults with occlusal asymmetry, treated with the Herbst appliance. Eur. J. Orthod. 2000, 22, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Eggensperger, N.; Raditsch, T.; Taghizadeh, F.; Iizuka, T. Mandibular setback by sagittal split ramus osteotomy: A 12-year follow-up. Acta Odontol. Scand. 2005, 63, 183–188. [Google Scholar] [CrossRef]
- Huang, C.S.; de Villa, G.H.; Liou, E.J.; Chen, Y.R. Mandibular remodeling after bilateral sagittal split osteotomy for prognathism of the mandible. J. Oral Maxillofac. Surg. 2006, 64, 167–172. [Google Scholar] [CrossRef]
- Proffit, W.R.; Phillips, C.; Dann, C.T.; Turvey, T.A. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. I. Mandibular setback. Int. J. Adult Orthodon. Orthognath. Surg. 1991, 6, 7–18. [Google Scholar]
- Song, H.S.; Choi, S.H.; Cha, J.Y.; Lee, K.J.; Yu, H.S. Comparison of changes in the transverse dental axis between patients with skeletal Class III malocclusion and facial asymmetry treated by orthognathic surgery with and without presurgical orthodontic treatment. Korean J. Orthod. 2017, 47, 256–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, H.H.; Lonic, D.; Lo, L.J. 3D printing in orthognathic surgery—A literature review. J. Formos. Med. Assoc. 2018, 117, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Oth, O.; Durieux, V.; Orellana, M.F.; Glineur, R. Genioplasty with surgical guide using 3D-printing technology: A systematic review. J. Clin. Exp. Dent. 2020, 12, e85–e92. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Hwang, D.S.; Song, J.M.; Kim, U.K. Comparison of time and cost between conventional surgical planning and virtual surgical planning in orthognathic surgery in Korea. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 35. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.H.; Bailey, L.J.; Tucker, G.R.; Styner, M.A., Jr.; Mol, A.; Phillips, C.L.; Proffit, W.R.; Turvey, T. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac. Radiol. 2005, 34, 369–375. [Google Scholar] [CrossRef] [Green Version]
- Cevidanes, L.H.; Oliveira, A.E.; Grauer, D.; Styner, M.; Proffit, W.R. Clinical application of 3D imaging for assessment of treatment outcomes. Semin. Orthod. 2011, 17, 72–80. [Google Scholar] [CrossRef] [Green Version]
- Cevidanes, L.H.; Styner, M.A.; Proffit, W.R. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 611–618. [Google Scholar] [CrossRef] [Green Version]
- Schilling, J.; Gomes, L.C.; Benavides, E.; Nguyen, T.; Paniagua, B.; Styner, M.; Boen, V.; Gonçalves, J.R.; Cevidanes, L.H. Regional 3D superimposition to assess temporomandibular joint condylar morphology. Dentomaxillofac. Radiol. 2014, 43, 20130273. [Google Scholar] [CrossRef]
- Ikeda, R.; Oberoi, S.; Wiley, D.F.; Woodhouse, C.; Tallman, M.; Tun, W.W.; McNeill, C.; Miller, J.A.; Hatcher, D. Novel 3-dimensional analysis to evaluate temporomandibular joint space and shape. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 416–428. [Google Scholar] [CrossRef] [Green Version]
- Cevidanes, L.H.; Bailey, L.J.; Tucker, S.F.; Styner, M.A.; Mol, A.; Phillips, C.L.; Proffit, W.R.; Turvey, T. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Hadjidakis, D.J.; Androulakis, I.I. Bone remodeling. Ann. N. Y. Acad. Sci. 2006, 1092, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Miura, K.; Yoshida, M.; Yamaguchi, K.; Yoshida, R.; Asahina, I. Sonographic evaluation of bone formation after sagittal split ramus osteotomy. J. Ultrasound Med. 2016, 35, 395–400. [Google Scholar] [CrossRef] [PubMed]




| Anchor Points | Description |
|---|---|
| Medial point (red) | A most prominent point on the medial contour of the mandibular condyle |
| Lateral point (yellow) | A most prominent point on the lateral contour of the mandibular condyle |
| Posterior point (white) | A most prominent point on the posterior contour of the condyle where the cortication tapers to an even thickness |
| Height | Distance between the most superior part of the condylar head to a line through medial and lateral anchor point in coronal slice |
| Diameter | Distance between the most prominent point on the medial to the lateral side of the mandibular condyle in coronal slice |
| Width | Distance between the point on the posterior to the anterior contour of the condyle in axial slice |
| Condylar head volume | The volume of condyle above the plane consisting of anchor points |
| Joint space volume | The volume of fossa above the plane consisting of anchor points |
| Landmarks | Original Terms | Definitions |
|---|---|---|
| S | Sella | Center of the pituitary fossa of the sphenoid bone |
| N | Nasion | The most anterior point of the nasofrontal suture |
| B | B point | The point of maximum concavity in the midline of the alveolar process of mandible |
| Pog | Pogonion | The most anterior point of the symphysis of the mandible |
| Me | Menton | The most inferior point on the symphysis of the mandible |
| SNB | SN to NB | The angle between the SN plane and a plane connecting the NB |
| VRP | Vertical Reference plane | The plane perpendicular to the FH plane passing through the nasion |
| HRP | Horizontal reference plane | The plane parallel to the FH plane passing through the nasion |
| Variables | Non-Customized (n = 10) | Customized (n = 10) |
|---|---|---|
| Age | 25.2 ± 4.66 | 24.8 ± 3.88 |
| Sex | ||
| Male | 5(50%) | 6(60%) |
| Female | 5(50%) | 4(40%) |
| Surgery | ||
| Lefort I | 6(60%) | 6(60%) |
| Genioplasty | 3(30%) | 4(40%) |
| BSSRO | 10(100%) | 10(100%) |
| Time | Non-Customized | Customized | ||||
|---|---|---|---|---|---|---|
| Right | Left | p-Value 1 | Right | Left | p-Value 1 | |
| Height (mm) | ||||||
| T0 | 7.67 ± 1.43 | 7.01 ± 1.21 | 0.279 | 9.06 ± 1.32 | 8.68 ± 1.66 | 0.578 |
| T2 | 7.25 ± 1.7 | 6.65 ± 1.43 | 0.404 | 9.68 ± 0.87 | 9.06 ± 1.63 | 0.302 |
| Diameter (mm) | ||||||
| T0 | 20.95 ± 2.13 | 21 ± 1.45 | 0.952 | 21.73 ± 1.97 | 21.23 ± 2.86 | 0.185 |
| T2 | 20.62 ± 2.08 | 20.96 ± 1.7 | 0.693 | 21.49 ± 2.14 | 21.27 ± 3.1 | 0.856 |
| Width (mm) | ||||||
| T0 | 7.15 ± 0.7 | 7.46 ± 1.21 | 0.492 | 9.65 ± 1.75 | 8.74 ± 2.63 | 0.374 |
| T2 | 7.38 ± 0.66 | 7.34 ± 1.37 | 0.935 | 9.94 ± 1.6 | 9.04 ± 2.67 | 0.372 |
| Condylar head volume (mm3) | ||||||
| T0 | 593.52 ± 174.01 | 483.55 ± 169.12 | 0.169 | 775.83 ± 152.22 | 664.84 ± 271.17 | 0.274 |
| T2 | 578.58 ± 180.55 | 485.03 ± 191.52 | 0.276 | 799.83 ± 181.02 | 694.47 ± 224.99 | 0.264 |
| Joint space volume (mm3) | ||||||
| T0 | 1001.91 ± 304.04 | 701.22 ± 282.43 | <0.05 * | 1019.38 ± 264.03 | 942.91 ± 339.15 | 0.581 |
| T2 | 1082.44 ± 474.55 | 785.17 ± 284.17 | 0.106 | 1087.5 ± 159 | 1022.43 ± 328.15 | 0.582 |
| Side | Non-Customized | Customized | Between-Group (p-Value 2) | ||
|---|---|---|---|---|---|
| Diff. | p-Value 1 | Diff. | p-Value 1 | ||
| Height (mm) | |||||
| Right | −0.42 ± 1.11 | 0.262 | 0.62 ± 1.31 | 0.169 | 0.071 |
| Left | −0.36 ± 0.58 | 0.083 | 0.38 ± 0.58 | 0.067 | <0.05 * |
| Diameter (mm) | |||||
| Right | −0.33 ± 0.63 | 0.133 | −0.24 ± 0.69 | 0.3 | 0.765 |
| Left | −0.04 ± 0.44 | 0.779 | 0.04 ± 0.56 | 0.827 | 0.727 |
| Width (mm) | |||||
| Right | 0.23 ± 0.51 | 0.188 | 0.29 ± 1.2 | 0.463 | 0.886 |
| Left | −0.12 ± 0.42 | 0.388 | 0.3 ± 0.65 | 0.177 | 0.102 |
| Condylar head volume (mm3) | |||||
| Right | −14.94 ± 82.34 | 0.58 | 24 ± 114.72 | 0.525 | 0.395 |
| Left | 1.48 ± 74.98 | 0.952 | 29.63 ± 124.01 | 0.469 | 0.547 |
| Joint space volume (mm3) | |||||
| Right | 80.53 ± 253.54 | 0.341 | 68.12 ± 254.54 | 0.419 | 0.914 |
| Left | 83.95 ± 124.98 | <0.05 * | 79.52 ± 206.1 | 0.253 | 0.954 |
| Parameters | Non-Customized | Customized | Between-Group (p-Value 2) | ||
|---|---|---|---|---|---|
| Diff. | p-Value 1 | Diff. | p-Value 1 | ||
| N-perp to pog (mm) ¶ | 0.46 ± 2.35 | 0.551 | 0.75 ± 1.61 | 0.174 | 0.751 |
| HRP to Me (mm) § | 0.61 ± 1.05 | 0.099 | 1.08 ± 1.55 | 0.055 | 0.438 |
| SNB (°) §§ | 0.68 ± 1.44 | 0.169 | 0.47 ± 0.8 | 0.096 | 0.692 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, Y.N.; Park, I.-Y.; Kim, J.-C.; Byun, S.-H.; Yang, B.-E. Comparison of Changes in the Condylar Volume and Morphology in Skeletal Class III Deformities Undergoing Orthognathic Surgery Using a Customized versus Conventional Miniplate: A Retrospective Analysis. J. Clin. Med. 2020, 9, 2794. https://doi.org/10.3390/jcm9092794
Lim YN, Park I-Y, Kim J-C, Byun S-H, Yang B-E. Comparison of Changes in the Condylar Volume and Morphology in Skeletal Class III Deformities Undergoing Orthognathic Surgery Using a Customized versus Conventional Miniplate: A Retrospective Analysis. Journal of Clinical Medicine. 2020; 9(9):2794. https://doi.org/10.3390/jcm9092794
Chicago/Turabian StyleLim, You Na, In-Young Park, Jong-Cheol Kim, Soo-Hwan Byun, and Byoung-Eun Yang. 2020. "Comparison of Changes in the Condylar Volume and Morphology in Skeletal Class III Deformities Undergoing Orthognathic Surgery Using a Customized versus Conventional Miniplate: A Retrospective Analysis" Journal of Clinical Medicine 9, no. 9: 2794. https://doi.org/10.3390/jcm9092794





