Effect of Type 2 Diabetes Mellitus on the Hypoxia-Inducible Factor 1-Alpha Expression. Is There a Relationship with the Clock Genes?
Abstract
1. Introduction
2. Material and Methods
2.1. Statement on Ethics
2.2. Design of the Study and Description of the Study Population
2.3. Gene expression by Real-Time Quantitative PCR.
2.4. Circulating Lactate and Pyruvate Measurement
2.5. Statistical Analysis
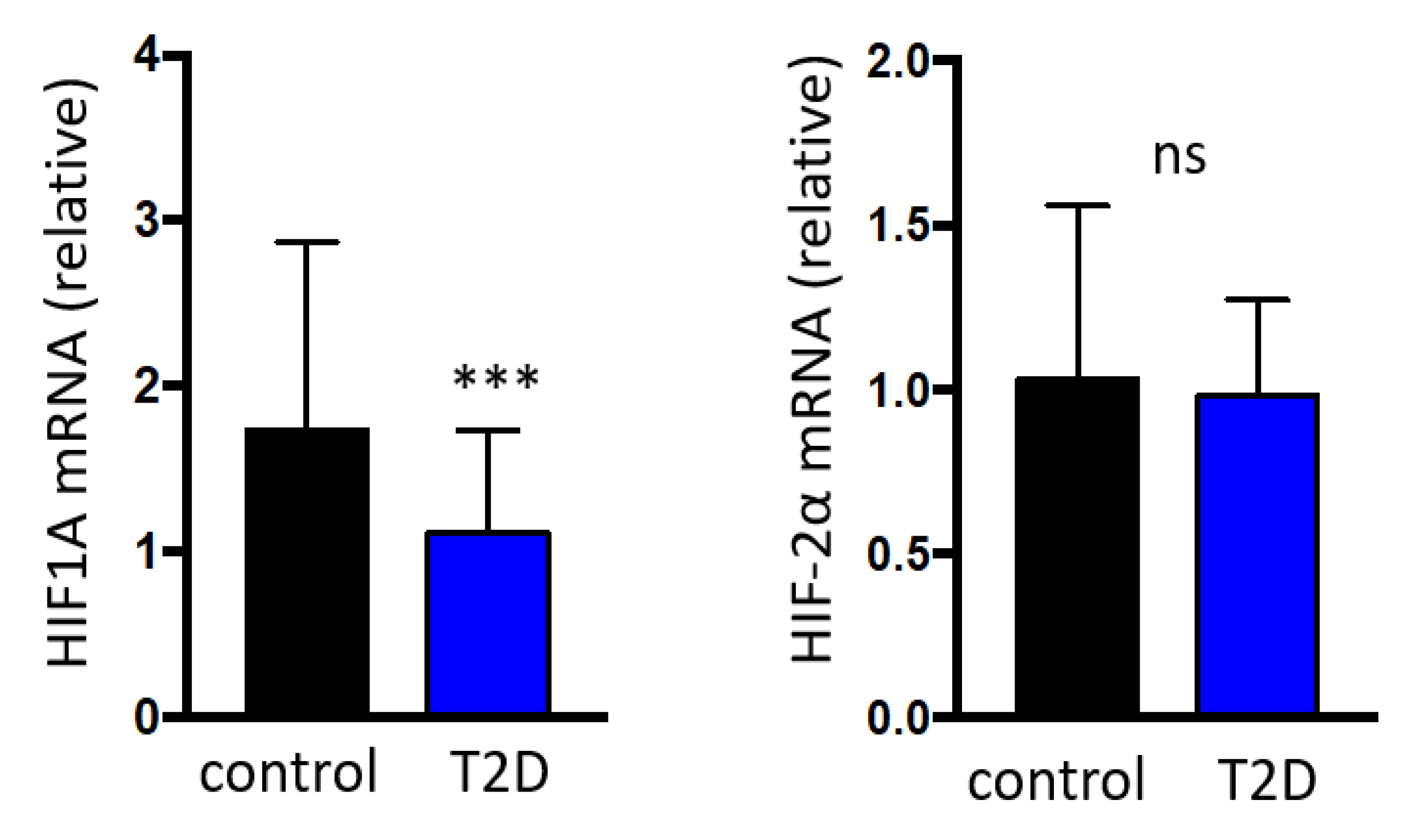
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sampol, G.; Lecube, A. Type 2 diabetes and the lung: A bidirectional relationship. Endocrinol. Nutr. 2012, 59, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Aurora, R.N.; Punjabi, N.M. Obstructive sleep apnoea and type 2 diabetes mellitus: A bidirectional association. Lancet Respir. Med. 2013, 1, 329–338. [Google Scholar] [CrossRef]
- Lecube, A.; Sampol, G.; Lloberes, P.; Romero, O.; Mesa, J.; Hernández, C.; Simó, R. Diabetes is an independent risk factor for severe nocturnal hypoxemia in obese patients. A case-control study. PLoS ONE 2009, 4, e4692. [Google Scholar] [CrossRef] [PubMed]
- Lecube, A.; Simó, R.; Pallayova, M.; Punjabi, N.M.; López-Cano, C.; Turino, C.; Hernández, C.; Barbé, F. Pulmonary function and sleep breathing: Two new targets for type 2 diabetes care. Endocr. Rev. 2017, 38, 550–573. [Google Scholar] [CrossRef] [PubMed]
- López-Cano, C.; Gutiérrez-Carrasquilla, L.; Sánchez, E.; González, J.; Yeramian, A.; Martí, R.; Hernández, M.; Cao, G.; Ribelles, M.; Gómez, X.; et al. Sympathetic hyperactivity and sleep disorders in individuals with type 2 diabetes. Front. Endocrinol. Lausanne 2019, 10, 752. [Google Scholar] [CrossRef]
- Pugh, C.W.; Ratcliffe, P.J. New horizons in hypoxia signaling pathways. Exp. Cell Res. 2017, 356, 116–121. [Google Scholar] [CrossRef]
- Wang, G.L.; Jiang, B.H.; Rue, E.A.; Semenza, G.L. Hypoxia inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc. Natl. Acad. Sci. USA 1995, 92, 5510–5514. [Google Scholar] [CrossRef]
- Kim, J.W.; Tchernyshyov, I.; Semenza, G.L.; Dang, C.V. HIF-1-mediated expression of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006, 3, 177–185. [Google Scholar] [CrossRef]
- Cheng, K.; Ho, K.; Stokes, R.; Scott, C.; Lau, S.M.; Hawthorne, W.J.; O’Connell, P.J.; Loudovaris, T.; Kay, T.W.; Kulkarni, R.N.; et al. Hypoxia-inducible factor-1alpha regulates beta cell function in mouse and human islets. J. Clin. Investig. 2010, 120, 2171–2183. [Google Scholar] [CrossRef]
- Roenneberg, T.; Merrow, M. The circadian clock and human health. Curr. Biol. 2016, 26, R432–R443. [Google Scholar] [CrossRef]
- Kalsbeek, A.; Yi, C.X.; La Fleur, S.E.; Fliers, E. The hypothalamic clock and its control of glucose homeostasis. Trends Endocrinol. Metab. 2010, 21, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.A. Circadian clock-mediated control of stem cell division and differentiation: Beyond night and day. Development 2014, 141, 3105–3111. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Ramsey, K.M.; Marcheva, B.; Bass, J. Circadian rhythms, sleep, and metabolism. J. Clin. Investig. 2011, 121, 2133–2141. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Jamshed, H.; Peterson, C.M. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 2018, 84, 11–27. [Google Scholar] [CrossRef]
- Vieira, E.; Burris, T.P.; Quesada, I. Clock genes, pancreatic function, and diabetes. Trends Mol. Med. 2014, 20, 685–693. [Google Scholar] [CrossRef]
- Froy, O.; Garaulet, M. The circadian clock in white and brown adipose tissue: Mechanistic, endocrine, and clinical aspects. Endocronol. Rev. 2018, 39, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Stenvers, D.J.; Scheer, F.A.J.L.; Schrauwen, P.; La Fleur, S.E.; Kalsbeek, A. Circadian clocks and insulin resistance. Nat. Rev. Endocrinol. 2019, 15, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.Y.; Lin, P.W.; Lin, H.C.; Lin, P.M.; Chen, I.Y.; Friedman, M.; Hung, C.F.; Salapatas, A.M.; Lin, M.C.; Lin, S.F. Alternations of circadian clock genes expression and oscillation in obstructive sleep apnea. J. Clin. Med. 2019, 8, 1634. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.P.; Smales, C.; Wu, H.; Hussain, M.V.; Mohamed, Y.A.; Morimoto, M.; Shea, S.A. The circadian system contributes to apnea lengthening across the night in obstructive sleep apnea. Sleep 2015, 38, 1793–1801. [Google Scholar] [CrossRef]
- Amplification Efficiency of TaqMan Gene Expression Assays. Applied Biosystems Application Note Can Be Found Online. Available online: http://docs.appliedbiosystems.com/pebiodocs/00113186.pdf (accessed on 13 August 2020).
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The MIQE guidelines: Minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef]
- von Allmen, D.C.; Francey, L.J.; Rogers, G.M.; Ruben, M.D.; Cohen, A.P.; Wu, G.; Schmidt, R.E.; Ishman, S.L.; Amin, R.S.; Hogenesch, J.B.; et al. Circadian dysregulation: The next frontier in obstructive sleep apnea research. Otolaryngol. Head Neck Surg. 2018, 159, 948–955. [Google Scholar] [CrossRef] [PubMed]
- Chilov, D.; Hofer, T.; Bauer, C.; Wenger, R.H.; Gassmann, M. Hypoxia affects expression of circadian genes PER1 and CLOCK in mouse brain. FASEB J. 2001, 15, 2613–2622. [Google Scholar] [CrossRef]
- Ghorbel, M.T.; Coulson, J.M.; Murphy, D. Cross-talk between hypoxic and circadian pathways: Cooperative roles for hypoxia-inducible factor 1alpha and CLOCK in transcriptional activation of the vasopressin gene. Mol. Cell Neurosci. 2003, 22, 396–404. [Google Scholar] [CrossRef]
- Dimova, E.Y.; Jakupovic, M.; Kubaichuk, K.; Mennerich, D.; Chi, T.F.; Tamanini, F.; Oklejewicz, M.; Hänig, J.; Byts, N.; Mäkelä, K.A.; et al. The circadian clock protein cry1 is a negative regulator of HIF-1α. iScience 2019, 13, 284–304. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, H.; Harris, A.L. Advances in hypoxia-inducible factor biology. Cell Metab. 2018, 27, 281–298. [Google Scholar] [CrossRef] [PubMed]
- Peek, C.B.; Levine, D.C.; Cedernaes, J.; Taguchi, A.; Kobayashi, Y.; Tsai, S.J.; Bonar, N.A.; McNulty, M.R.; Ramsey, K.M.; Bass, J. Circadian clock interaction with HIF1a mediates oxygenic metabolism and anaerobic glycolysis in skeletal muscle. Cell Metab. 2017, 25, 86–92. [Google Scholar] [CrossRef]
- Wu, Y.; Tang, D.; Liu, N.; Xiong, W.; Huang, H.; Li, Y.; Ma, Z.; Zhao, H.; Chen, P.; Qi, X.; et al. Reciprocal regulation between the circadian clock and hypoxia signaling at the genome level in mammals. Cell Metab. 2017, 25, 73–85. [Google Scholar] [CrossRef]
- Adamovich, Y.; Ladeuix, B.; Golik, M.; Koeners, M.P.; Asher, G. Rhythmic oxygen levels reset circadian clocks through HIF1a. Cell Metab. 2017, 25, 93–101. [Google Scholar] [CrossRef]
- Ando, H.; Takamura, T.; Matsuzawa-Nagata, N.; Shima, K.R.; Eto, T.; Misu, H.; Shiramoto, M.; Tsuru, T.; Irie, S.; Fujimura, A.; et al. Clock gene expression in peripheral leucocytes of patients with type 2 diabetes. Diabetologia 2009, 52, 329–335. [Google Scholar] [CrossRef]
- Eckel-Mahan, K.; Sassone-Corsi, P. Metabolism and the circadian clock converge. Physiol. Rev. 2013, 93, 107–135. [Google Scholar] [CrossRef]
- Kalsbeek, A.; Fliers, E. Circadian and endocrine rhythms. Best Pract. Res. Clin. Endocrinol. Metab. 2017, 31, 443. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, H.; Li, Y.; Tao, X.; Sun, J. Poor sleep quality is associated with dawn phenomenon and impaired circadian clock gene expression in subjects with type 2 diabetes mellitus. Int. J. Endocrinol. 2017, 2017, 4578973. [Google Scholar] [CrossRef] [PubMed]
- Moreira, S.; Rodrigues, R.; Barros, A.; Pejanovic, N.; Neves-Costa, A.; Pedroso, D.; Pereira, C.; Fernandes, D.; Valenca Rodrigues, J.; Barbara, C.; et al. Changes in expression of the clock gene in obstructive sleep apnea syndrome patients are not reverted by continuous positive airway pressure treatment. Front. Med. Lausanne 2017, 4, 187. [Google Scholar] [CrossRef] [PubMed]
- Pugh, C.W. Modulation of the hypoxic response. Adv. Exp. Med. Biol. 2016, 903, 259–271. [Google Scholar] [PubMed]
- Vieira, E.; Marroquí, L.; Figueroa, A.L.; Merino, B.; Fernandez-Ruiz, R.; Nadal, A.; Burris, T.P.; Gomis, R.; Quesada, I. Involvement of the clock gene rev-erb alpha in the regulation of glucagon secretion in pancreatic alpha-cells. PLoS ONE 2013, 8, e69939. [Google Scholar] [CrossRef]
- Barnea, M.; Haviv, L.; Gutman, R.; Chapnik, N.; Madar, Z.; Froy, O. Metformin affects the circadian clock and metabolic rhythms in a tissue-specific manner. BiochimBiophys. Acta 2012, 1822, 1796–1806. [Google Scholar] [CrossRef]
- Hawley, J.A.; Lundby, C.; Cotter, J.D.; Burke, L.M. Maximizing cellular adaptation to endurance exercise in skeletal muscle. Cell Metab. 2018, 27, 962–976. [Google Scholar] [CrossRef]


| Type 2 Diabetes | Non-Type 2 Diabetes | p | |
|---|---|---|---|
| n | 62 | 67 | - |
| Age (Years) | 57.3 ± 10.0 | 58.8 ± 9.4 | 0.381 |
| Women, n (%) | 32 (51.6) | 17 (25.3) | 0.003 |
| BMI (Kg/m2) | 33.6 ± 6.2 | 28.6 ± 6.6 | <0.001 |
| Hba1c (%) | 8.4 ± 1.8 | 5.4 ± 0.3 | <0.001 |
| Hba1c (mmol/mol) | 68.9 ± 19.8 | 35.6 ± 3.7 | <0.001 |
| Fasting Glucose (mmol/L) | 8.6 ± 3.1 | 4.9 ± 1.3 | <0.001 |
| Total Cholesterol (mmol/L) | 45.7 ± 10.6 | 53.5 ± 15.8 | 0.173 |
| HDL Cholesterol (mmol/L) | 11.7 ± 3.1 | 14.8 ± 5.2 | 0.018 |
| LDL Cholesterol (mmol/L) | 26.8 ± 9.1 | 35.3 ± 7.5 | 0.426 |
| Triglycerides (mmol/L) | 2.1 ± 1.2 | 1.3 ± 0.7 | 0.006 |
| Hypertension, n (%) | 50 (80.6) | 13 (24.0) | <0.001 |
| Smoking Habit, n (%) | 23 (37.0) | 22 (32.8) | 0.348 |
| Cardiovascular Disease, n (%) | 1 (0.01) | 2 (0.002) | 0.518 |
| Retinopathy, n (%) | 16 (25.8) | - | <0.001 |
| Nephropathy, n (%) | 20 (32.2) | - | <0.001 |
| Lactate (uM/L) | 2102.1 ± 688.2 | 1730.4 ± 694.4 | 0.013 |
| Pyruvate (uM/L) | 61.9 ± 25.6 | 50.3 ± 23.1 | 0.026 |
| HbA1c | HIF-1α | |||
|---|---|---|---|---|
| r | p | r | p | |
| HIF-1α | −0.358 | <0.001 | - | - |
| HIF-2α | −0.168 | 0.058 | 0.615 | < 0.001 |
| PER1 | −0.313 | <0.001 | 0.833 | <0.001 |
| PER2 | −0.438 | <0.001 | 0.868 | <0.001 |
| PER3 | −0.328 | <0.001 | 0.657 | <0.001 |
| RORA | −0.256 | 0.003 | 0.758 | <0.001 |
| ARNTL | −0.293 | 0.001 | 0.776 | <0.001 |
| CLOCK | −0.327 | <0.001 | 0.814 | <0.001 |
| CRY1 | −0.301 | 0.001 | 0.834 | <0.001 |
| CRY2 | −0.279 | 0.001 | 0.817 | <0.001 |
| Model 1 | β | Beta 95% CI | p |
| Hba1c (%) | −0.226 | −0.323 (−0.344 to −0.109) | <0.001 |
| Gender (Female/Male) | 0.069 | - | 0.433 |
| BMI (Kg/m2) | 0.041 | - | 0.635 |
| Age (Years) | 0.013 | - | 0.878 |
| Constant | - | 3.363 (2.523 to 4.204) | <0.001 |
| R2 = 0.104 | |||
| Model 2 | Β | Beta 95% CI | p |
| PER1 | 0.519 | 0.307 (0.262 to 0.351) | <0.001 |
| PER2 | 0.254 | 0.345 (0.125 to 0.566) | 0.002 |
| CRY2 | 0.227 | 0.540 (0.198 to 0.882) | 0.002 |
| CLOCK | 0.192 | 0.328 (0.075 to 0.580) | 0.011 |
| PER3 | −0.160 | −0.363 (−0.581 to −0.145) | 0.001 |
| Gender (Female/Male) | 0.051 | - | 0.058 |
| RORA | −0.075 | - | 0.221 |
| Hba1c (%) | −0.033 | - | 0.245 |
| CRY1 | −0.084 | - | 0.372 |
| BMI (Kg/m2) | −0.008 | - | 0.750 |
| ARNTL | −0.017 | - | 0.823 |
| Age (Years) | 0.000 | - | 1.000 |
| Constant | - | −0.223 (−0.429 to −0.017) | 0.034 |
| R2 = 0.920 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Cano, C.; Gutiérrez-Carrasquilla, L.; Barbé, F.; Sánchez, E.; Hernández, M.; Martí, R.; Ceperuelo-Mallafre, V.; Dalmases, M.; Fernández-Veledo, S.; Vendrell, J.; et al. Effect of Type 2 Diabetes Mellitus on the Hypoxia-Inducible Factor 1-Alpha Expression. Is There a Relationship with the Clock Genes? J. Clin. Med. 2020, 9, 2632. https://doi.org/10.3390/jcm9082632
López-Cano C, Gutiérrez-Carrasquilla L, Barbé F, Sánchez E, Hernández M, Martí R, Ceperuelo-Mallafre V, Dalmases M, Fernández-Veledo S, Vendrell J, et al. Effect of Type 2 Diabetes Mellitus on the Hypoxia-Inducible Factor 1-Alpha Expression. Is There a Relationship with the Clock Genes? Journal of Clinical Medicine. 2020; 9(8):2632. https://doi.org/10.3390/jcm9082632
Chicago/Turabian StyleLópez-Cano, Carolina, Liliana Gutiérrez-Carrasquilla, Ferran Barbé, Enric Sánchez, Marta Hernández, Raquel Martí, Vicky Ceperuelo-Mallafre, Mireia Dalmases, Sonia Fernández-Veledo, Joan Vendrell, and et al. 2020. "Effect of Type 2 Diabetes Mellitus on the Hypoxia-Inducible Factor 1-Alpha Expression. Is There a Relationship with the Clock Genes?" Journal of Clinical Medicine 9, no. 8: 2632. https://doi.org/10.3390/jcm9082632
APA StyleLópez-Cano, C., Gutiérrez-Carrasquilla, L., Barbé, F., Sánchez, E., Hernández, M., Martí, R., Ceperuelo-Mallafre, V., Dalmases, M., Fernández-Veledo, S., Vendrell, J., Hernández, C., Simó, R., & Lecube, A. (2020). Effect of Type 2 Diabetes Mellitus on the Hypoxia-Inducible Factor 1-Alpha Expression. Is There a Relationship with the Clock Genes? Journal of Clinical Medicine, 9(8), 2632. https://doi.org/10.3390/jcm9082632







