Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting
Abstract
1. Introduction
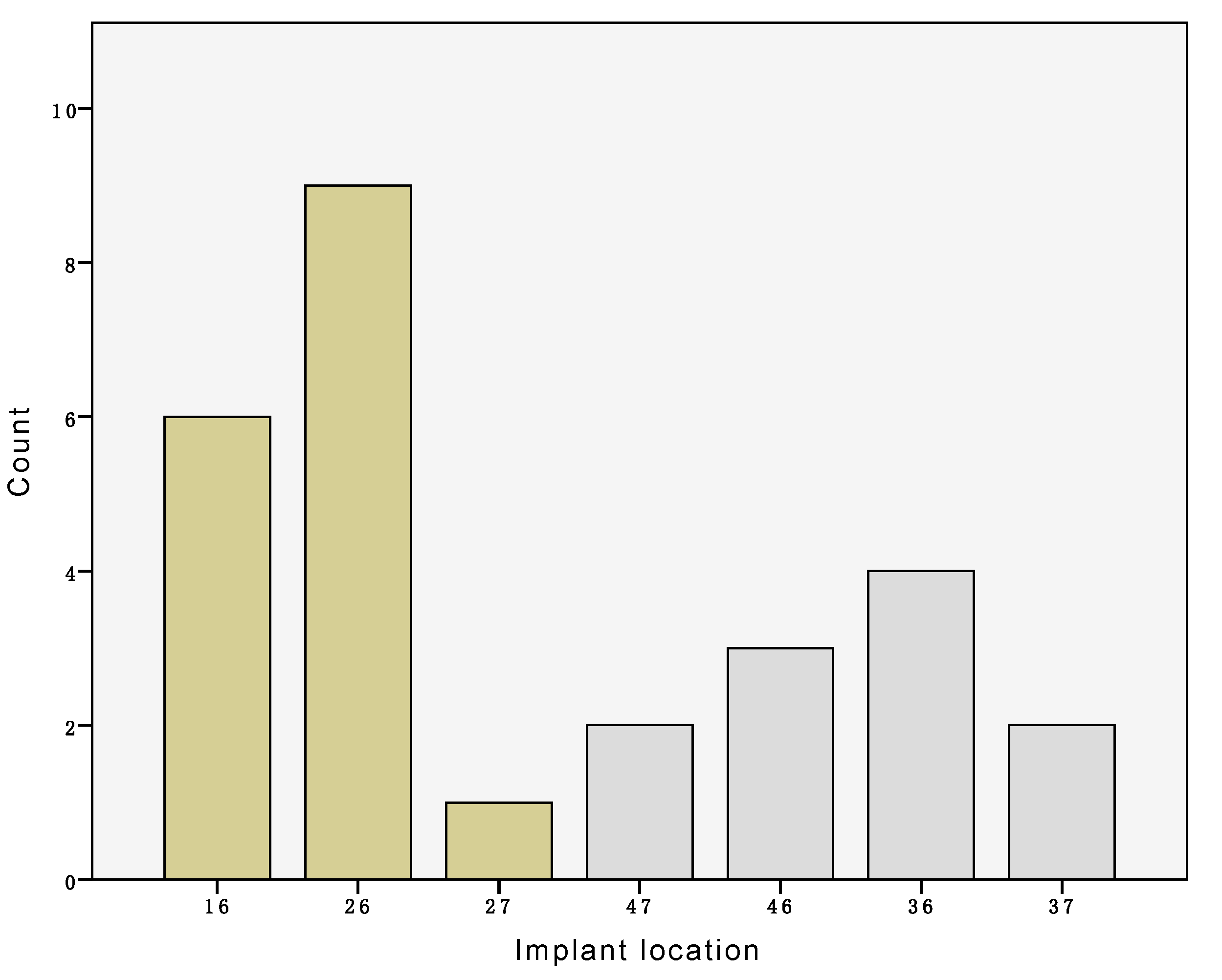
2. Experimental Section
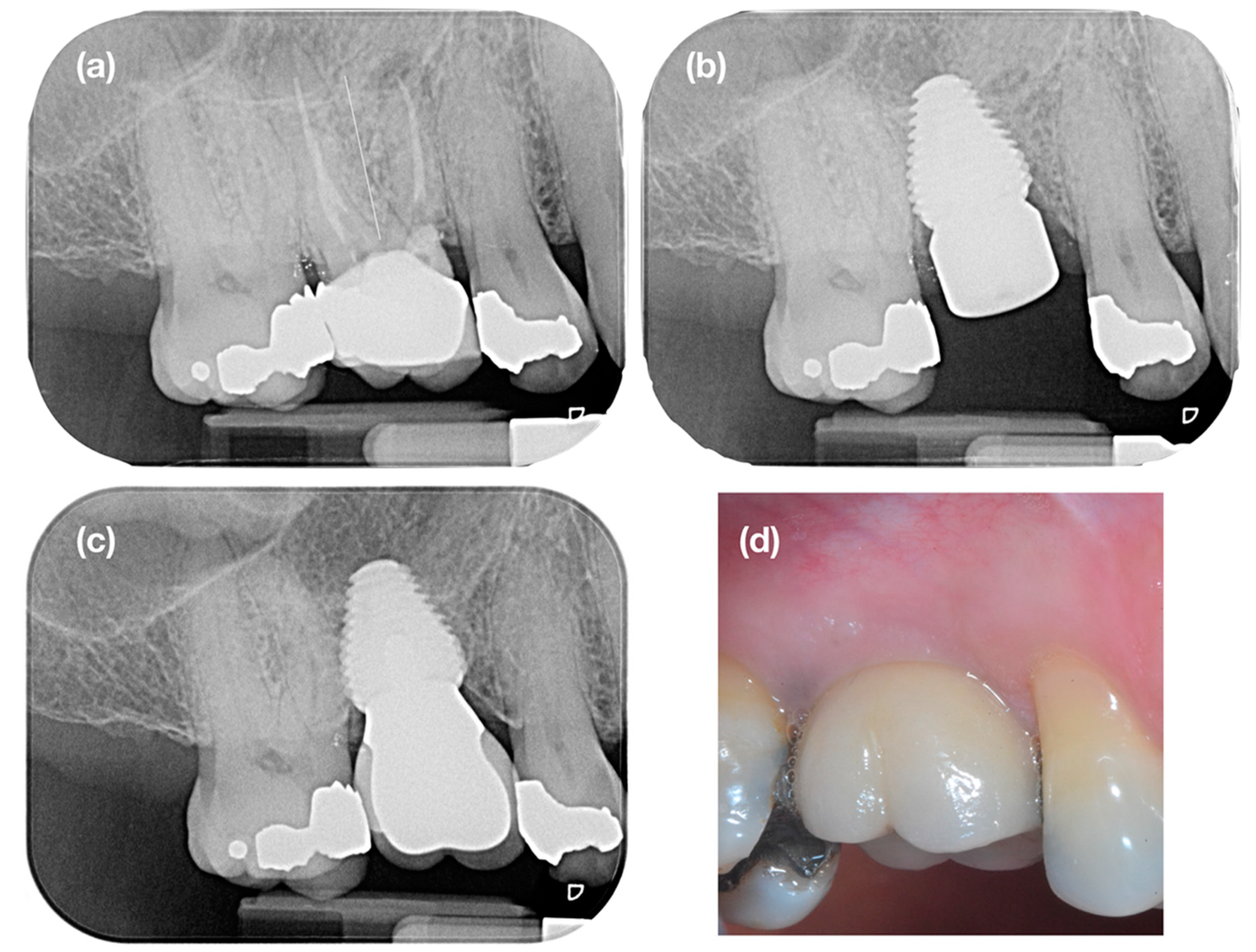
2.1. Clinical Procedure
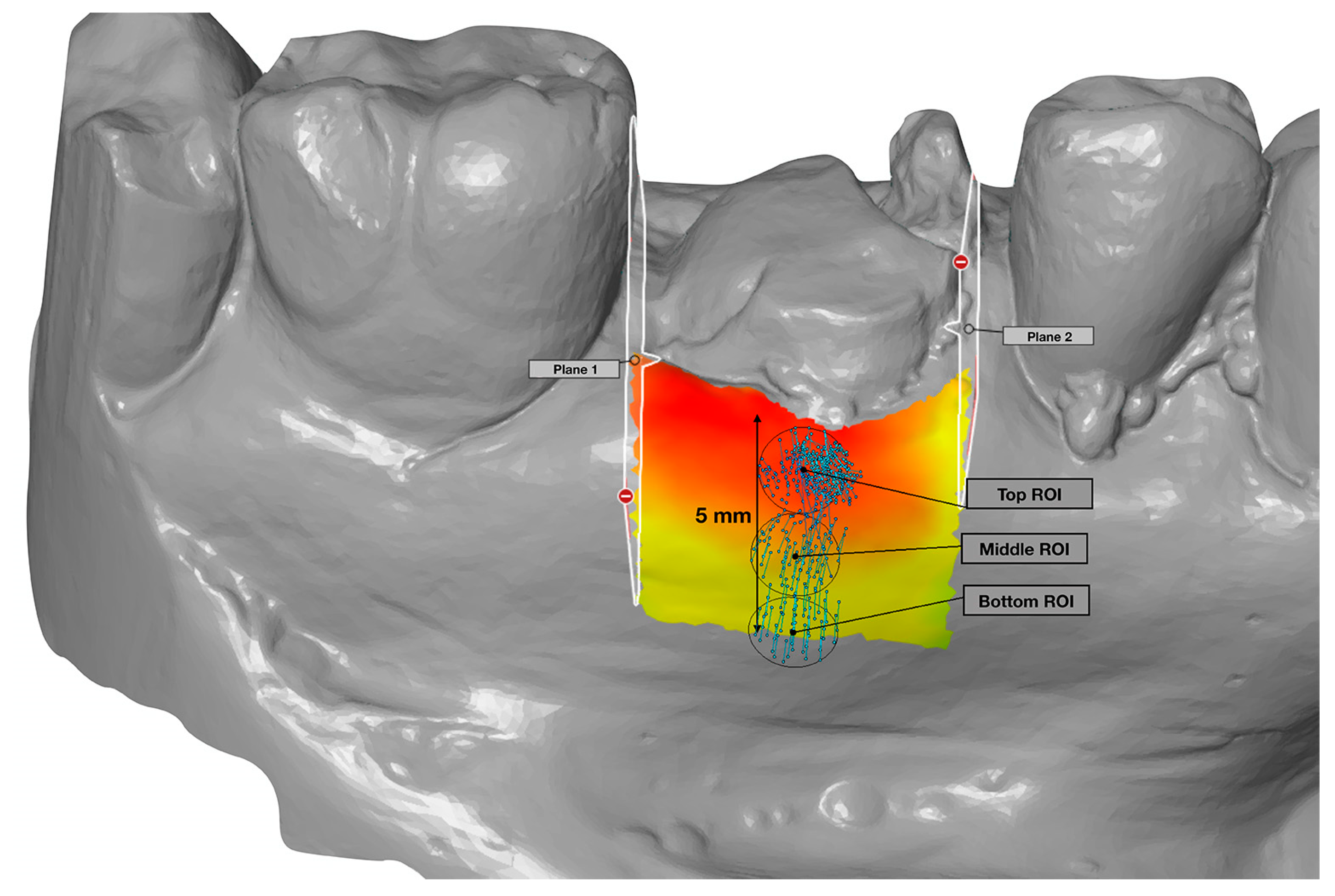
2.2. Data Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Trombelli, L.; Farina, R.; Marzola, A.; Bozzi, L.; Liljenberg, B.; Lindhe, J. Modeling and remodeling of human extraction sockets. J. Clin. Periodontol. 2008, 35, 630–639. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Bartee, B.K. Extraction site reconstruction for alveolar ridge preservation. Part 2: Membrane-assisted surgical technique. J. Oral Implantol. 2001, 27, 194–197. [Google Scholar] [CrossRef]
- Farina, R.; Pramstraller, M.; Franceschetti, G.; Pramstraller, C.; Trombelli, L. Alveolar ridge dimensions in maxillary posterior sextants: A retrospective comparative study of dentate and edentulous sites using computerized tomography data. Clin. Oral Implants Res. 2011, 22, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, L.; Devlin, H.; Ting, K.; Nishimura, I. Current perspectives in residual ridge remodeling and its clinical implications: A review. J. Prosthet. Dent. 1998, 80, 224–237. [Google Scholar] [CrossRef]
- Jeffcoat, M.K. Bone loss in the oral cavity. J. Bone Miner. Res. 1993, 8 (Suppl. S2), S467–S473. [Google Scholar] [CrossRef]
- Tallgren, A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J. Prosthet. Dent. 1972, 27, 120–132. [Google Scholar] [CrossRef]
- Lekovic, V.; Camargo, P.M.; Klokkevold, P.R.; Weinlaender, M.; Kenney, E.B.; Dimitrijevic, B.; Nedic, M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J. Periodontol. 1998, 69, 1044–1049. [Google Scholar] [CrossRef]
- Lekovic, V.; Kenney, E.B.; Weinlaender, M.; Han, T.; Klokkevold, P.; Nedic, M.; Orsini, M. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J. Periodontol. 1997, 68, 563–570. [Google Scholar] [CrossRef]
- Bressan, E.; Ferrarese, N.; Pramstraller, M.; Lops, D.; Farina, R.; Tomasi, C. Ridge Dimensions of the Edentulous Mandible in Posterior Sextants: An Observational Study on Cone Beam Computed Tomography Radiographs. Implant. Dent. 2017, 26, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Pinho, M.N.; Roriz, V.L.; Novaes, A.B., Jr.; Taba, M., Jr.; Grisi, M.F.; de Souza, S.L.; Palioto, D.B. Titanium membranes in prevention of alveolar collapse after tooth extraction. Implant. Dent. 2006, 15, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Van der Weijden, F.; Dell’Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Bodic, F.; Hamel, L.; Lerouxel, E.; Basle, M.F.; Chappard, D. Bone loss and teeth. Jt. Bone Spine 2005, 72, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, J.; Zhao, D.; Wu, Y.; Xu, C. Evaluation of Outcomes of Dental Implants Inserted by Flapless or Flapped Procedure: A Meta-Analysis. Implant. Dent. 2018, 27, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, A.; Fine, N.; Binderman, I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J. Periodontol. 1994, 65, 79–83. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Bolz, W.; Huerzeler, M. Tissue alterations after tooth extraction with and without surgical trauma: A volumetric study in the beagle dog. J. Clin. Periodontol. 2008, 35, 356–363. [Google Scholar] [CrossRef]
- Blanco, J.; Nunez, V.; Aracil, L.; Munoz, F.; Ramos, I. Ridge alterations following immediate implant placement in the dog: Flap versus flapless surgery. J. Clin. Periodontol. 2008, 35, 640–648. [Google Scholar] [CrossRef]
- O’Neill, J.E.; Yeung, S.C. Do dental implants preserve and maintain alveolar bone? J. Investig. Clin. Dent. 2011, 2, 229–235. [Google Scholar] [CrossRef]
- Van Nimwegen, W.G.; Goene, R.J.; Van Daelen, A.C.; Stellingsma, K.; Raghoebar, G.M.; Meijer, H.J. Immediate implant placement and provisionalisation in the aesthetic zone. J. Oral Rehabil. 2016, 43, 745–752. [Google Scholar] [CrossRef]
- Arora, H.; Khzam, N.; Roberts, D.; Bruce, W.L.; Ivanovski, S. Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2-5 year follow up. Clin. Implant Dent. Relat. Res. 2017, 19, 694–702. [Google Scholar] [CrossRef]
- Covani, U.; Bortolaia, C.; Barone, A.; Sbordone, L. Bucco-lingual crestal bone changes after immediate and delayed implant placement. J. Periodontol. 2004, 75, 1605–1612. [Google Scholar] [CrossRef]
- Paolantonio, M.; Dolci, M.; Scarano, A.; d’Archivio, D.; di Placido, G.; Tumini, V.; Piattelli, A. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J. Periodontol. 2001, 72, 1560–1571. [Google Scholar] [CrossRef]
- Schultz, A.J. Guided tissue regeneration (GTR) of nonsubmerged implants in immediate extraction sites. Pract. Periodontics Aesthet. Dent. 1993, 5, 59–65, quiz 66. [Google Scholar]
- Werbitt, M.J.; Goldberg, P.V. The immediate implant: Bone preservation and bone regeneration. Int. J. Periodontics Restor. Dent. 1992, 12, 206–217. [Google Scholar]
- Denissen, H.W.; Kalk, W.; Veldhuis, H.A.; van Waas, M.A. Anatomic consideration for preventive implantation. Int. J. Oral Maxillofac. Implant. 1993, 8, 191–196. [Google Scholar]
- Watzek, G.; Haider, R.; Mensdorff-Pouilly, N.; Haas, R. Immediate and delayed implantation for complete restoration of the jaw following extraction of all residual teeth: A retrospective study comparing different types of serial immediate implantation. Int. J. Oral Maxillofac. Implant. 1995, 10, 561–567. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Polyzos, I.P.; Felice, P.; Worthington, H.V. Timing of implant placement after tooth extraction: Immediate, immediate-delayed or delayed implants? A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 189–205. [Google Scholar]
- Tonetti, M.S.; Cortellini, P.; Graziani, F.; Cairo, F.; Lang, N.P.; Abundo, R.; Conforti, G.P.; Marquardt, S.; Rasperini, G.; Silvestri, M.; et al. Immediate versus delayed implant placement after anterior single tooth extraction: The timing randomized controlled clinical trial. J. Clin. Periodontol. 2017, 44, 215–224. [Google Scholar] [CrossRef]
- Maiorana, C.; Poli, P.P.; Deflorian, M.; Testori, T.; Mandelli, F.; Nagursky, H.; Vinci, R. Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix. J. Periodontal Implant. Sci 2017, 47, 194–210. [Google Scholar] [CrossRef]
- Mozzati, M.; Gallesio, G.; Staiti, G.; Iezzi, G.; Piattelli, A.; Mortellaro, C. Socket Preservation Using a Biomimetic Nanostructured Matrix and Atraumatic Surgical Extraction Technique. J. Craniofac. Surg. 2017, 28, 1042–1045. [Google Scholar] [CrossRef]
- Amato, F.; Polara, G.; Spedicato, G.A. Tissue Dimensional Changes in Single-Tooth Immediate Extraction Implant Placement in the Esthetic Zone: A Retrospective Clinical Study. Int. J. Oral Maxillofac Implant. 2018, 33, 439–447. [Google Scholar] [CrossRef]
- Ramaglia, L.; Sbordone, C.; Saviano, R.; Martuscelli, R.; Sbordone, L. Marginal masticatory mucosa dimensional changes in immediate post-extractive implants: A 2 year prospective cohort study. Clin. Oral Implant. Res. 2015, 26, 1495–1502. [Google Scholar] [CrossRef]
- Arora, H.; Ivanovski, S. Immediate and early implant placement in single-tooth gaps in the anterior maxilla: A prospective study on ridge dimensional, clinical, and aesthetic changes. Clin. Oral Implant. Res. 2018. [Google Scholar] [CrossRef]
- Vandeweghe, S.; Hattingh, A.; Wennerberg, A.; Bruyn, H.D. Surgical protocol and short-term clinical outcome of immediate placement in molar extraction sockets using a wide body implant. J. Oral Maxillofac. Res. 2011, 2, e1. [Google Scholar] [CrossRef]
- Vandeweghe, S.; Ackermann, A.; Bronner, J.; Hattingh, A.; Tschakaloff, A.; De Bruyn, H. A retrospective, multicenter study on a novo wide-body implant for posterior regions. Clin. Implant Dent. Relat. Res. 2012, 14, 281–292. [Google Scholar] [CrossRef]
- Hattingh, A.; Hommez, G.; De Bruyn, H.; Huyghe, M.; Vandeweghe, S. A prospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin. Implant Dent. Relat. Res. 2018, 20, 1009–1015. [Google Scholar] [CrossRef]
- Chen, S.T.; Darby, I.B.; Reynolds, E.C. A prospective clinical study of non-submerged immediate implants: Clinical outcomes and esthetic results. Clin. Oral Implant. Res. 2007, 18, 552–562. [Google Scholar] [CrossRef]
- Evans, C.D.; Chen, S.T. Esthetic outcomes of immediate implant placements. Clin. Oral Implant. Res. 2008, 19, 73–80. [Google Scholar] [CrossRef]
- Hattingh, A.C.; De Bruyn, H.; Ackermann, A.; Vandeweghe, S. Immediate Placement of Ultrawide-Diameter Implants in Molar Sockets: Description of a Recommended Technique. Int. J. Periodontics Restor. Dent. 2018, 38, 17–23. [Google Scholar] [CrossRef]
- Alqahtani, S.; Alsheraimi, A.; Alshareef, A.; Alsaban, R.; Alqahtani, A.; Almgran, M.; Eldesouky, M.; Al-Omar, A. Maxillary Sinus Pneumatization Following Extractions in Riyadh, Saudi Arabia: A Cross-sectional Study. Cureus 2020, 12, e6611. [Google Scholar] [CrossRef]
- Cavalcanti, M.C.; Guirado, T.E.; Sapata, V.M.; Costa, C.; Pannuti, C.M.; Jung, R.E.; Cesar Neto, J.B. Maxillary sinus floor pneumatization and alveolar ridge resorption after tooth loss: A cross-sectional study. Braz. Oral Res. 2018, 32, e64. [Google Scholar] [CrossRef]
- Pramstraller, M.; Schincaglia, G.P.; Vecchiatini, R.; Farina, R.; Trombelli, L. Alveolar ridge dimensions in mandibular posterior regions: A retrospective comparative study of dentate and edentulous sites using computerized tomography data. Surg. Radiol. Anat. 2018, 40, 1419–1428. [Google Scholar] [CrossRef]
- Smith, R.B.; Tarnow, D.P. Classification of molar extraction sites for immediate dental implant placement: Technical note. Int.. J. Oral Maxillofac. Implant. 2013, 28, 911–916. [Google Scholar] [CrossRef]
- Tallarico, M.; Xhanari, E.; Pisano, M.; Gatti, F.; Meloni, S.M. Molar replacement with 7 mm-wide diameter implants: To place the implant immediately or to wait 4 months after socket preservation? 1 year after loading results from a randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 169–178. [Google Scholar]
- Cosyn, J.; Hooghe, N.; De Bruyn, H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J. Clin. Periodontol. 2012, 39, 582–589. [Google Scholar] [CrossRef]
- Lops, D.; Chiapasco, M.; Rossi, A.; Bressan, E.; Romeo, E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket: 1-year prospective study. Clin. Oral Implant. Res. 2008, 19, 1135–1140. [Google Scholar] [CrossRef]
- Romeo, E.; Lops, D.; Rossi, A.; Storelli, S.; Rozza, R.; Chiapasco, M. Surgical and prosthetic management of interproximal region with single-implant restorations: 1-year prospective study. J. Periodontol. 2008, 79, 1048–1055. [Google Scholar] [CrossRef]
- Slagter, K.W.; den Hartog, L.; Bakker, N.A.; Vissink, A.; Meijer, H.J.; Raghoebar, G.M. Immediate placement of dental implants in the esthetic zone: A systematic review and pooled analysis. J. Periodontol. 2014, 85, e241–e250. [Google Scholar] [CrossRef]
- Cordaro, L.; Torsello, F.; Roccuzzo, M. Clinical outcome of submerged vs. non-submerged implants placed in fresh extraction sockets. Clin. Oral Implant. Res. 2009, 20, 1307–1313. [Google Scholar] [CrossRef]
- Kan, J.Y.; Rungcharassaeng, K.; Lozada, J.L.; Zimmerman, G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: A 2- to 8-year follow-up. Int. J. Oral Maxillofac. Implant. 2011, 26, 179–187. [Google Scholar]
- Chappuis, V.; Engel, O.; Shahim, K.; Reyes, M.; Katsaros, C.; Buser, D. Soft Tissue Alterations in Esthetic Postextraction Sites: A 3-Dimensional Analysis. J. Dent. Res. 2015, 94, 187S–193S. [Google Scholar] [CrossRef]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.P.; Buser, D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J. Dent. Res. 2013, 92, 195S–201S. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Gaveglio, L.; Gherlone, E.; Cardaropoli, G. Soft tissue contour changes at immediate implants: A randomized controlled clinical study. Int. J. Periodontics Restor. Dent. 2014, 34, 631–637. [Google Scholar] [CrossRef]
- Tian, J.; Wei, D.; Zhao, Y.; Di, P.; Jiang, X.; Lin, Y. Labial soft tissue contour dynamics following immediate implants and immediate provisionalization of single maxillary incisors: A 1-year prospective study. Clin. Implant Dent. Relat. Res. 2019, 21, 492–502. [Google Scholar] [CrossRef]
- Theye, C.E.G.; Hattingh, A.; Cracknell, T.J.; Oettle, A.C.; Steyn, M.; Vandeweghe, S. Dento-alveolar measurements and histomorphometric parameters of maxillary and mandibular first molars, using micro-CT. Clin. Implant Dent. Relat. Res. 2018, 20, 550–561. [Google Scholar] [CrossRef]
- Chen, S.T.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla--a systematic review. Int. J. Oral Maxillofac Implant. 2014, 29, 186–215. [Google Scholar] [CrossRef]
- De Bruyn, H.; Raes, F.; Cooper, L.F.; Reside, G.; Garriga, J.S.; Tarrida, L.G.; Wiltfang, J.; Kern, M. Three-years clinical outcome of immediate provisionalization of single Osseospeed() implants in extraction sockets and healed ridges. Clin. Oral Implant. Res. 2013, 24, 217–223. [Google Scholar] [CrossRef]
- Kinaia, B.M.; Ambrosio, F.; Lamble, M.; Hope, K.; Shah, M.; Neely, A.L. Soft Tissue Changes Around Immediately Placed Implants: A Systematic Review and Meta-Analyses With at Least 12 Months of Follow-Up After Functional Loading. J. Periodontol. 2017, 88, 876–886. [Google Scholar] [CrossRef]
- Hof, M.; Pommer, B.; Ambros, H.; Jesch, P.; Vogl, S.; Zechner, W. Does Timing of Implant Placement Affect Implant Therapy Outcome in the Aesthetic Zone? A Clinical, Radiological, Aesthetic, and Patient-Based Evaluation. Clin. Implant Dent. Relat. Res. 2015, 17, 1188–1199. [Google Scholar] [CrossRef]
- Checchi, V.; Felice, P.; Zucchelli, G.; Barausse, C.; Piattelli, M.; Pistilli, R.; Grandi, G.; Esposito, M. Wide diameter immediate post-extractive implants vs delayed placement of normal-diameter implants in preserved sockets in the molar region: 1-year post-loading outcome of a randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 263–278. [Google Scholar] [PubMed]
- Cecchinato, D.; Lops, D.; Salvi, G.E.; Sanz, M. A prospective, randomized, controlled study using OsseoSpeed implants placed in maxillary fresh extraction socket: Soft tissues response. Clin. Oral Implant. Res. 2015, 26, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Cecchinato, D.; Ferrus, J.; Salvi, G.E.; Ramseier, C.; Lang, N.P.; Lindhe, J. Implants placed in fresh extraction sockets in the maxilla: Clinical and radiographic outcomes from a 3-year follow-up examination. Clin. Oral Implant. Res. 2014, 25, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Farmer, M.; Darby, I. Ridge dimensional changes following single-tooth extraction in the aesthetic zone. Clin. Oral Implant. Res. 2014, 25, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Iasella, J.M.; Greenwell, H.; Miller, R.L.; Hill, M.; Drisko, C.; Bohra, A.A.; Scheetz, J.P. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: A clinical and histologic study in humans. J. Periodontol. 2003, 74, 990–999. [Google Scholar] [CrossRef]
- Murugesan, A.; Sivakumar, A. Comparison of accuracy of mesiodistal tooth measurements made in conventional study models and digital models obtained from intraoral scan and desktop scan of study models. J. Orthod. 2020. [Google Scholar] [CrossRef]
- Tomita, Y.; Uechi, J.; Konno, M.; Sasamoto, S.; Iijima, M.; Mizoguchi, I. Accuracy of digital models generated by conventional impression/plaster-model methods and intraoral scanning. Dent. Mater. J. 2018, 37, 628–633. [Google Scholar] [CrossRef]
- Osnes, C.A.; Wu, J.H.; Venezia, P.; Ferrari, M.; Keeling, A.J. Full arch precision of six intraoral scanners in vitro. J. Prosthodont. Res. 2020, 64, 6–11. [Google Scholar] [CrossRef]
- Schmidt, A.; Klussmann, L.; Wostmann, B.; Schlenz, M.A. Accuracy of Digital and Conventional Full-Arch Impressions in Patients: An Update. J. Clin. Med. 2020, 9, 688. [Google Scholar] [CrossRef]
- Fageeh, H.N.; Meshni, A.A.; Jamal, H.A.; Preethanath, R.S.; Halboub, E. The accuracy and reliability of digital measurements of gingival recession versus conventional methods. BMC Oral Health 2019, 19, 154. [Google Scholar] [CrossRef]
- Lehmann, K.M.; Kasaj, A.; Ross, A.; Kammerer, P.W.; Wagner, W.; Scheller, H. A new method for volumetric evaluation of gingival recessions: A feasibility study. J. Periodontol. 2012, 83, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, K.M.; Kasaj, A.; Ross, A.; Willershausen, I.; Schmidtmann, I.; Staedt, H.; Scheller, H. A novel method for evaluating periodontal recession: A feasibility study. Int. J. Comput. Dent. 2011, 14, 297–307. [Google Scholar] [PubMed]
- Schneider, D.; Ender, A.; Truninger, T.; Leutert, C.; Sahrmann, P.; Roos, M.; Schmidlin, P. Comparison between clinical and digital soft tissue measurements. J. Esthet. Restor. Dent. 2014, 26, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Blanco, J.; Carral, C.; Argibay, O.; Linares, A. Implant placement in fresh extraction sockets. Periodontol. 2000 2019, 79, 151–167. [Google Scholar] [CrossRef] [PubMed]

| 4 Months | 12 Months | ||
|---|---|---|---|
| Buccal horizontal reduction | |||
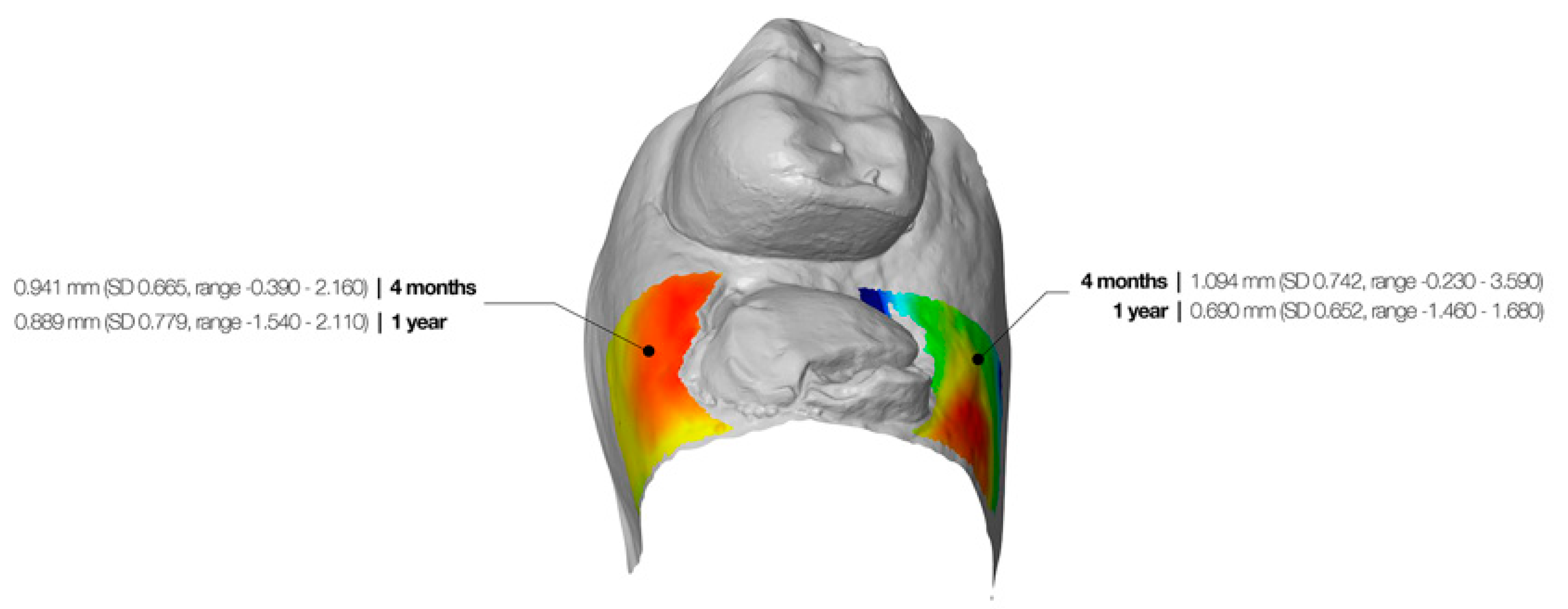
| 0.94 mm (SD 0.67, range −0.39–2.16) | 0.89 mm (SD 0.78, range −1.54–2.11) | p = 0.933 | |
| Buccal midfacial reduction | |||
| Top 2 mm ROI | 1.53 mm (SD 0.96, range −0.42–3.85) | 1.43 mm (SD 0.74, range 0.05–3.23) | p = 0.195 |
| Middle 2 mm ROI | 1.31 mm (SD 0.73, range −0.09–2.79) | 1.59 mm (SD 0.81, range 0.09–3.15) | p = 0.010 |
| Bottom 2 mm ROI | 0.86 mm (SD 0.62, range 0.10–2.78) | 1.33 mm (SD 0.76, range −0.23–2.88) | p = 0.001 |
| Overall | 1.23 mm (SD 0.71, range −0.09–3.14) | 1.45 mm (SD 0.70, range 0.18–3.09) | p = 0.013 |
| Palatal/Lingual horizontal reduction | |||
| 1.09 mm (SD 0.74, range −0.23–3.59) | 0.69 mm (SD 0.65, range −1.46–1.68) | p = 0.001 | |
| Palatal/Lingual midfacial reduction | |||
| Top 2 mm ROI | 1.68 mm (SD 0.81, range 0.48–3.62) | 1.18 mm (SD 0.81, range −0.32–2.97) | p = 0.010 |
| Middle 2 mm ROI | 1.51 mm (SD 0.73, range 0.22–3.62) | 1.35 mm (SD 0.72, range 0.30–3.32) | p = 0.186 |
| Bottom 2 mm ROI | 1.11 mm (SD 0.92, range 0.20–4.02) | 0.97 mm (SD 0.68, range 0.09–3.10) | p = 0.302 |
| Overall | 1.43 mm (SD 0.74, range 0.34–3.75) | 1.16 mm (SD 0.67, range 0.23–3.13) | p = 0.044 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hattingh, A.; De Bruyn, H.; Van Weehaeghe, M.; Hommez, G.; Vandeweghe, S. Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting. J. Clin. Med. 2020, 9, 2504. https://doi.org/10.3390/jcm9082504
Hattingh A, De Bruyn H, Van Weehaeghe M, Hommez G, Vandeweghe S. Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting. Journal of Clinical Medicine. 2020; 9(8):2504. https://doi.org/10.3390/jcm9082504
Chicago/Turabian StyleHattingh, André, Hugo De Bruyn, Manù Van Weehaeghe, Geert Hommez, and Stefan Vandeweghe. 2020. "Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting" Journal of Clinical Medicine 9, no. 8: 2504. https://doi.org/10.3390/jcm9082504
APA StyleHattingh, A., De Bruyn, H., Van Weehaeghe, M., Hommez, G., & Vandeweghe, S. (2020). Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting. Journal of Clinical Medicine, 9(8), 2504. https://doi.org/10.3390/jcm9082504





