Sex-Specific Prognostic Implications in Dilated Cardiomyopathy After Left Ventricular Reverse Remodeling
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Echocardiographic Evaluation
2.3. LVRR Definition and Study Outcome Measures
2.4. Statistical Analysis
3. Results
3.1. Left Ventricular Reverse Remodeling
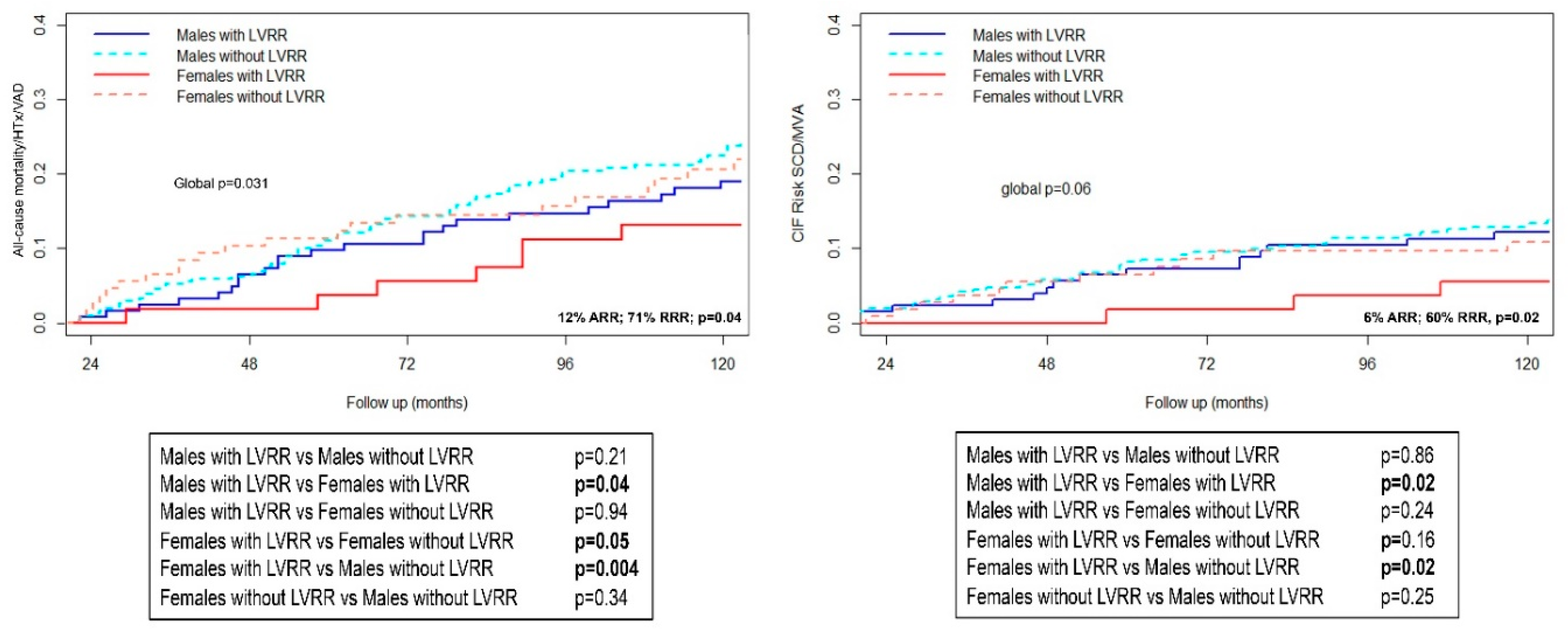
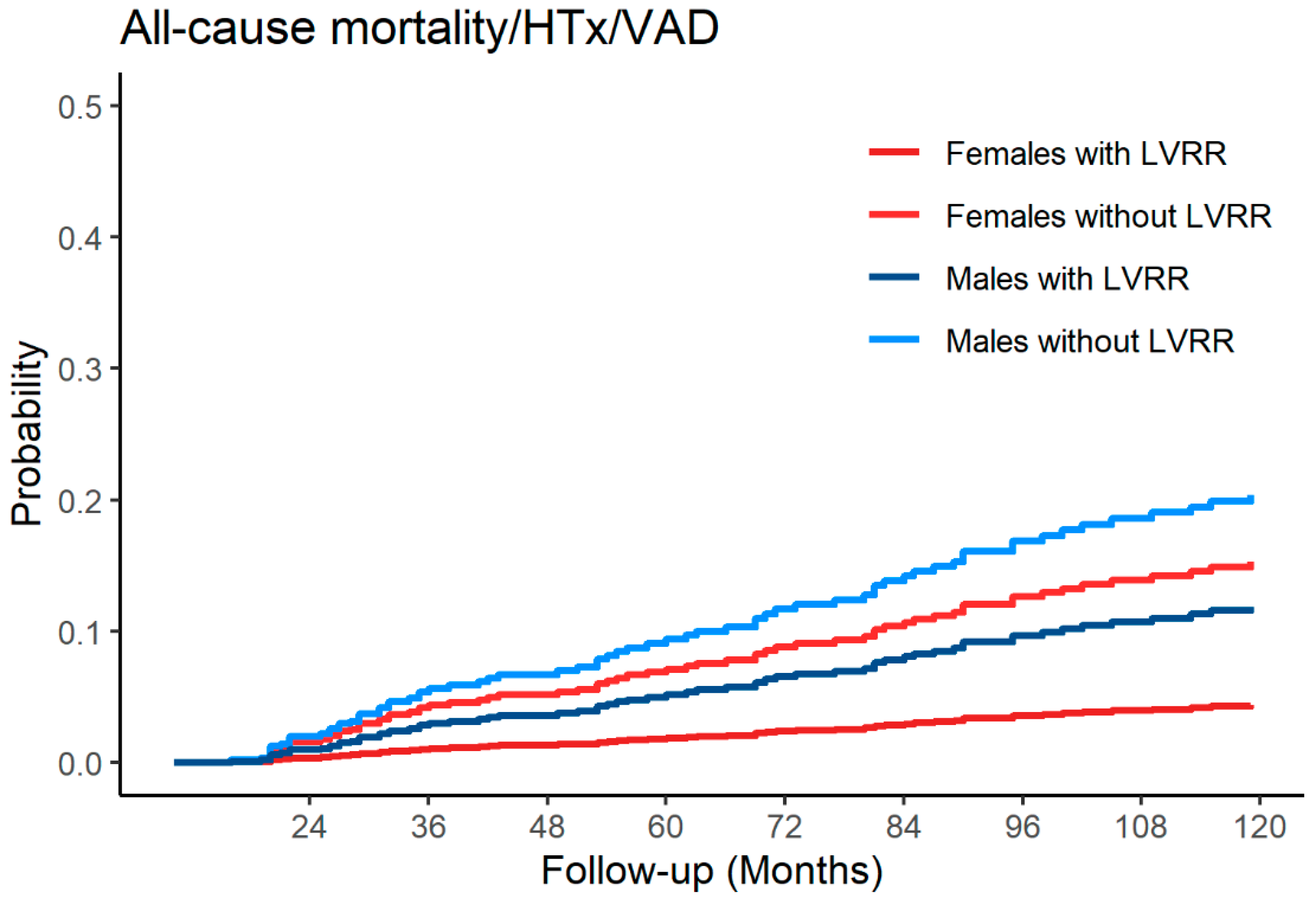
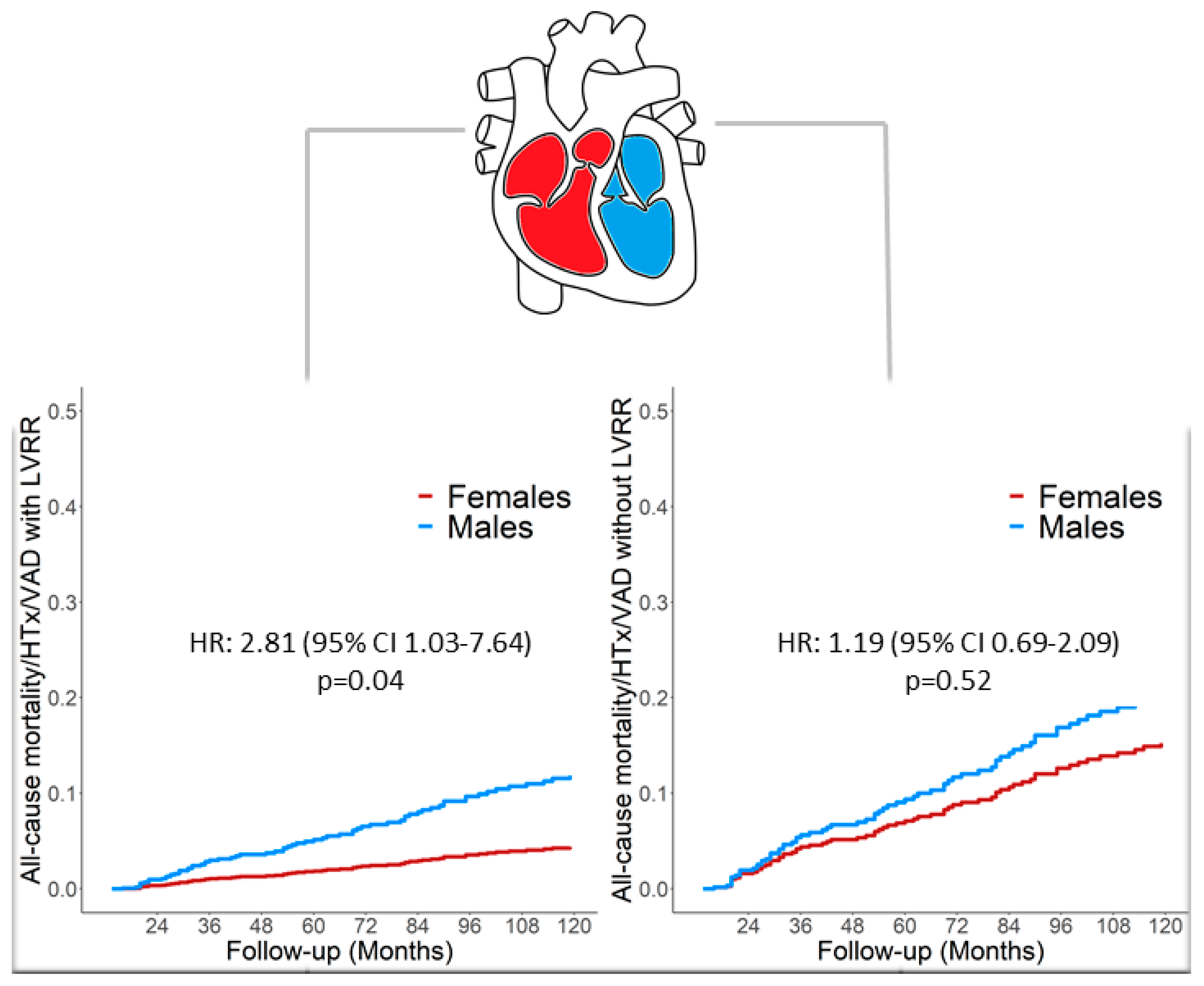
3.2. Outcomes
3.3. Multi-State Model Analysis
4. Discussion
Women and DCM, a Fairy Tale?
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Merlo, M.; Cannata, A.; Gobbo, M.; Stolfo, D.; Elliott, P.M.; Sinagra, G. Evolving concepts in dilated cardiomyopathy. Eur. J. Heart Fail. 2017, 20, 228–239. [Google Scholar] [CrossRef]
- Merlo, M.; Pivetta, A.; Pinamonti, B.; Merlo, M.; Pivetta, A.; Pinamonti, B.; Stolfo, D.; Zecchin, M.; Barbati, G.; Lenarda, A.D.; et al. Long-term prognostic impact of therapeutic strategies in patients with idiopathic dilated cardiomyopathy: Changing mortality over the last 30 years. Eur. J. Heart Fail. 2014, 16, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Merlo, M.; Cannata, A.; Vitagliano, A.; Zambon, E.; Lardieri, G.; Sinagra, G. Clinical management of dilated cardiomyopathy: Current knowledge and future perspectives. Expert Rev. Cardiovasc. Ther. 2016, 14, 137–340. [Google Scholar] [CrossRef][Green Version]
- Tayal, U.; Wage, R.; Newsome, S.; Manivarmane, R.; Izgi, C.; Muthumala, A.; Dungu, J.N.; Assomull, R.; Hatipoglu, S.; Halliday, B.P.; et al. Predictors of left ventricular remodelling in patients with dilated cardiomyopathy–a cardiovascular magnetic resonance study. Eur. J. Heart Fail. 2020. [Google Scholar] [CrossRef] [PubMed]
- Merlo, M.; Pyxaras, S.A.; Pinamonti, B.; Barbati, G.; Di Lenarda, A.; Sinagra, G. Prevalence and prognostic significance of left ventricular reverse remodeling in dilated cardiomyopathy receiving tailored medical treatment. J. Am. Coll. Cardiol. 2011, 57, 1468–1476. [Google Scholar] [CrossRef] [PubMed]
- Cannatà, A.; Fabris, E.; Merlo, M. Sex differences in the long-term prognosis of dilated cardiomyopathy. Can. J. Cardiol. 2019, 36, 37–44. [Google Scholar] [CrossRef]
- Halliday, B.P.; Gulati, A.; Ali, A.; Simon, N.; Amrit, L.; Upasana, T.; Vassilios, S.V.; Monika, A.; Cemil, I.; Kaushiga, K.; et al. Sex- and age-based differences in the natural history and outcome of dilated cardiomyopathy. Eur. J. Heart Fail. 2018, 20, 1392–1400. [Google Scholar] [CrossRef]
- De Bellis, A.; De Angelis, G.; Fabris, E.; Cannata, A.; Merlo, M.; Sinagra, G. Gender-related differences in heart failure: Beyond the “one-size-fits-all” paradigm. Heart Fail. Rev. 2020, 25, 245–255. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Héctor, B.; John, G.F.C.; Andrew, J.S.C.; Volkmar, F.; José, R.; Veli-Pekka, H.; Ewa, A.J.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar]
- Brignole, M.; Auricchio, A.; Baron-Esquivias, G. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 2013, 34, 2281–2329. [Google Scholar]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Pierre, B.; Giuseppe, B.; Ole, B.; John, C.; Jean-Claude, D.; Victoria, D.; Perry, M.E.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the european association of cardiovascular imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef]
- Kajimoto, K.; Sato, N. Investigators of the acute decompensated heart failure syndromes, r. sex differences in New York heart association functional classification and survival in acute heart failure patients with preserved or reduced ejection fraction. Can. J. Cardiol. 2020, 36, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Kajimoto, K.; Minami, Y.; Otsubo, S.; Sato, N.; Investigators of the Acute Decompensated Heart Failure Syndromes, R. Sex differences in left ventricular cavity dilation and outcomes in acute heart failure patients with left ventricular systolic dysfunction. Can. J. Cardiol. 2018, 34, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.J. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann. Statist. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
- Therneau, T.M.; Grambsch, P.M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994, 81, 515–526. [Google Scholar]
- Meyer, S.; van der Meer, P.; van Tintelen, J.P.; van den Berg, M.P. Sex differences in cardiomyopathies. Eur. J. Heart Fail. 2014, 16, 238–247. [Google Scholar] [CrossRef]
- Mosca, L.; Barrett-Connor, E.; Wenger, N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011, 124, 2145–2154. [Google Scholar] [CrossRef]
- Lam, C.S.P.; Arnott, C.; Beale, A.L. Sex differences in heart failure. Eur. Heart J. 2019, 40, 3859–3868. [Google Scholar] [CrossRef]
- Lainscak, M.; Milinkovic, I.; Polovina, M. Sex and age related differences in the management and outcomes of chronic heart failure: An analysis of patients from the ESC HFA EORP Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2020, 22, 92–102. [Google Scholar] [CrossRef]
- Boheler, K.R.; Volkova, M.; Morrell, C.; Rahul, G.; Yi, Z.; Kenneth, M.; Anne-Marie, S.; Edward, G.L. Sex- and age-dependent human transcriptome variability: Implications for chronic heart failure. Proc. Natl. Acad. Sci. USA 2003, 100, 2754–2759. [Google Scholar] [CrossRef]
- Kaneda, R.; Takada, S.; Yamashita, Y. Genome-wide histone methylation profile for heart failure. Genes Cells 2009, 14, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Feridooni, H.A.; Dibb, K.M.; Howlett, S.E. How cardiomyocyte excitation, calcium release and contraction become altered with age. J. Mol. Cell Cardiol. 2015, 83, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Cannata, A.; Camparini, L.; Sinagra, G.; Giacca, M.; Loffredo, F.S. Pathways for salvage and protection of the heart under stress: Novel routes for cardiac rejuvenation. Cardiovasc. Res. 2016, 111, 142–153. [Google Scholar] [CrossRef] [PubMed]

| Total Cohort | |||
|---|---|---|---|
| 605 Patients | |||
| Female | Male | p-Value | |
| n | 165 | 440 | |
| Age, (mean ± SD) | 51 ± 14 | 47 ± 15 | 0.007 |
| SBP, (mean ± SD) | 123 ± 18 | 127 ± 50 | 0.39 |
| NYHA III/IV, n (%) | 20 (13%) | 34 (8%) | 0.11 |
| Familial History of DCM, n (%) | 37 (23%) | 109 (26%) | 0.45 |
| Sinus Rhythm, n (%) | 138 (90%) | 348 (86%) | 0.19 |
| LBBB, n (%) | 52 (34%) | 101 (25%) | 0.02 |
| QRS Length, (mean ± SD) | 116 ± 35 | 115 ± 35 | 0.69 |
| LVEDDI, mm/m2 (mean ± SD) | 34 ± 5 | 31 ± 5 | <0.001 |
| LVEDVI, mL/m2 (mean ± SD) | 78 ± 31 | 81 ± 32 | 0.42 |
| Normal Volumes *, n (%) | 50 (32%) | 223 (53%) | 0.001 |
| Mild Dilation *, n (%) | 13 (8%) | 80 (19%) | |
| Moderate Dilation *, n (%) | 37 (24%) | 30 (7%) | |
| Severe Dilation *, n (%) | 55 (35%) | 89 (21%) | |
| Moderate-Severe Dilation, n (%) | 92 (59%) | 119 (28%) | <0.001 |
| LVEF %, (mean ± SD) | 40 ± 12 | 41 ± 11 | 0.50 |
| RFP, n (%) | 12 (11%) | 28 (9%) | 0.57 |
| RV Dysfunction, n (%) | 9 (8%) | 39 (11%) | 0.29 |
| ACE-I/ARBs, n (%) | 122 (82%) | 343 (85%) | 0.51 |
| β-blockers, n (%) | 135 (85%) | 368 (87%) | 0.41 |
| MRAs, n (%) | 22 (14%) | 57 (14%) | 0.89 |
| ICD during follow-up, n (%) | 39 (24%) | 140 (32%) | 0.06 |
| CRT during follow-up, n (%) | 19 (12%) | 59 (13%) | 0.59 |
| Male with LVRR | Male without LVRR | Females with LVRR | Females without LVRR | |
|---|---|---|---|---|
| Median follow-up, months (IQR) | 187 (122–269) | 136 (80–202) | 199 (123–278) | 135 (72–222) |
| All-cause mortality/HTx/VAD | 0.17 | 0.18 | 0.05 | 0.18 |
| CV death/HTx/VAD | 0.11 | 0.13 | 0.04 | 0.15 |
| Death for pump failure | 0 | 0.04 | 0.04 | 0.2 |
| Heart Transplantation | 0.05 | 0.05 | 0 | 0.10 |
| VAD | 0.007 | 0.003 | 0 | 0 |
| SCD | 0.06 | 0.03 | 0 | 0.04 |
| SCD/MVA | 0.10 | 0.12 | 0.04 | 0.12 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannata, A.; Manca, P.; Nuzzi, V.; Gregorio, C.; Artico, J.; Gentile, P.; Pio Loco, C.; Ramani, F.; Barbati, G.; Merlo, M.; et al. Sex-Specific Prognostic Implications in Dilated Cardiomyopathy After Left Ventricular Reverse Remodeling. J. Clin. Med. 2020, 9, 2426. https://doi.org/10.3390/jcm9082426
Cannata A, Manca P, Nuzzi V, Gregorio C, Artico J, Gentile P, Pio Loco C, Ramani F, Barbati G, Merlo M, et al. Sex-Specific Prognostic Implications in Dilated Cardiomyopathy After Left Ventricular Reverse Remodeling. Journal of Clinical Medicine. 2020; 9(8):2426. https://doi.org/10.3390/jcm9082426
Chicago/Turabian StyleCannata, Antonio, Paolo Manca, Vincenzo Nuzzi, Caterina Gregorio, Jessica Artico, Piero Gentile, Carola Pio Loco, Federica Ramani, Giulia Barbati, Marco Merlo, and et al. 2020. "Sex-Specific Prognostic Implications in Dilated Cardiomyopathy After Left Ventricular Reverse Remodeling" Journal of Clinical Medicine 9, no. 8: 2426. https://doi.org/10.3390/jcm9082426
APA StyleCannata, A., Manca, P., Nuzzi, V., Gregorio, C., Artico, J., Gentile, P., Pio Loco, C., Ramani, F., Barbati, G., Merlo, M., & Sinagra, G. (2020). Sex-Specific Prognostic Implications in Dilated Cardiomyopathy After Left Ventricular Reverse Remodeling. Journal of Clinical Medicine, 9(8), 2426. https://doi.org/10.3390/jcm9082426





