Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy
Abstract
1. Introduction
2. Methods
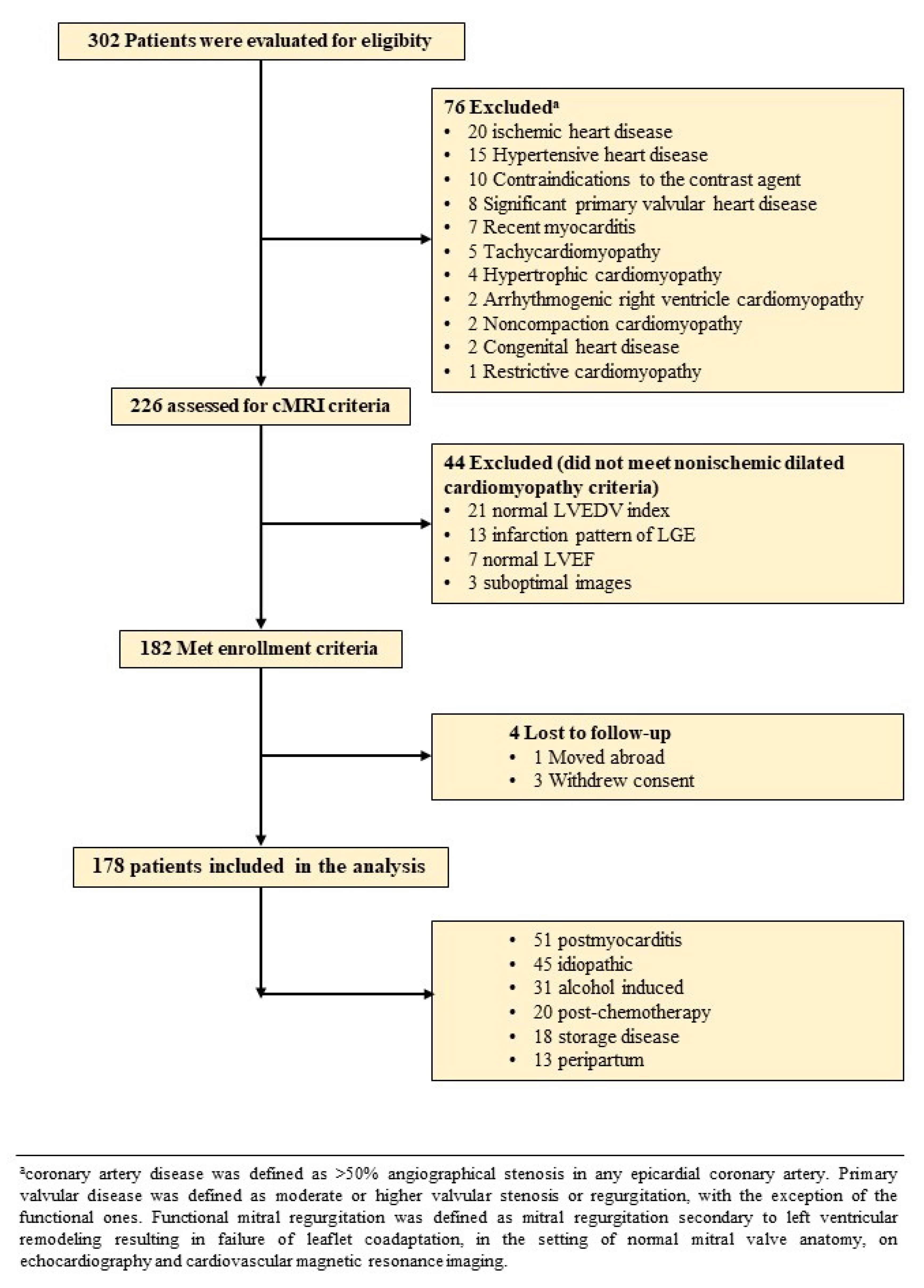
2.1. Study Population
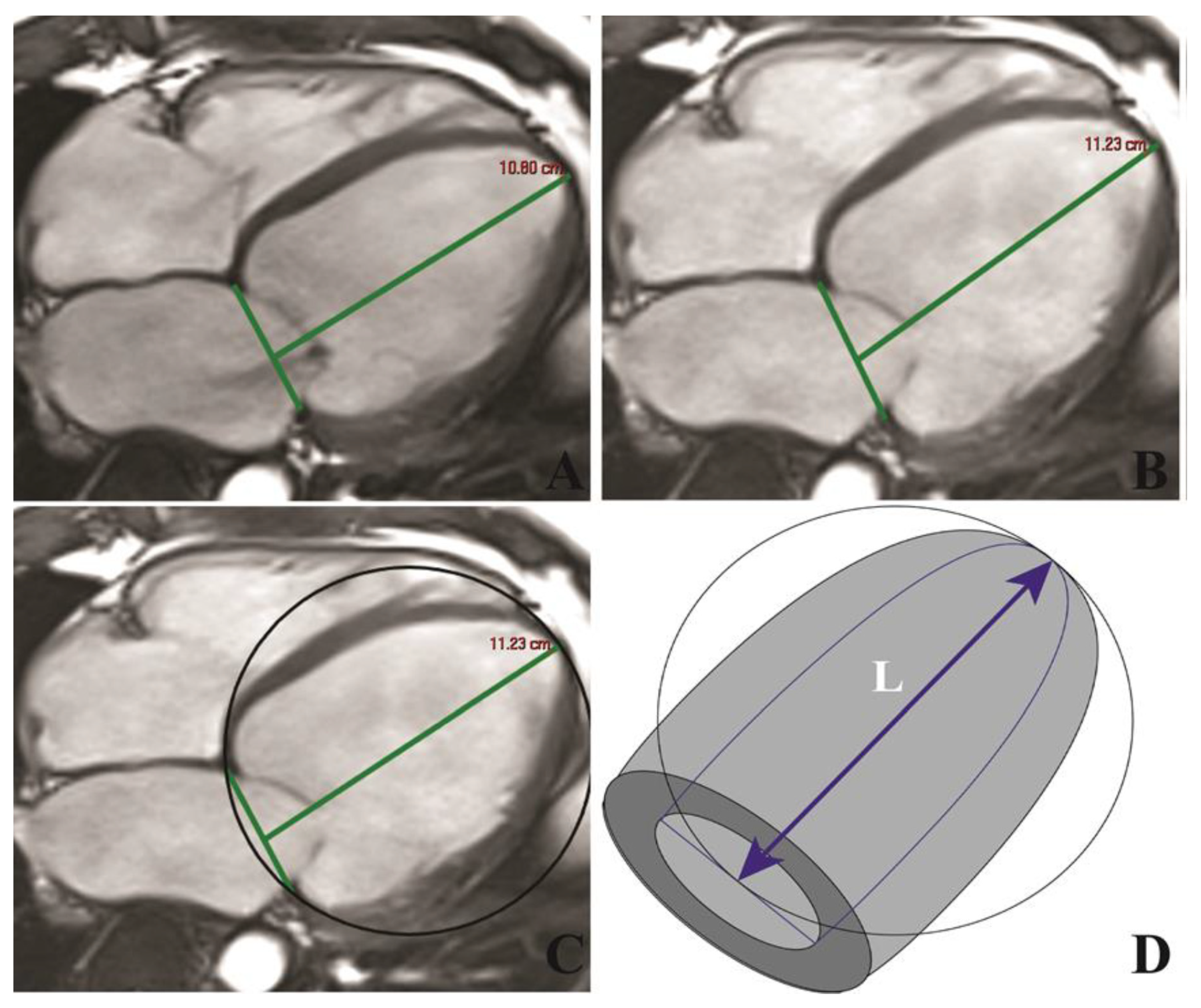
2.2. cMRI
2.3. Follow-Up of Clinical Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Reproducibility of cMRI Measurements
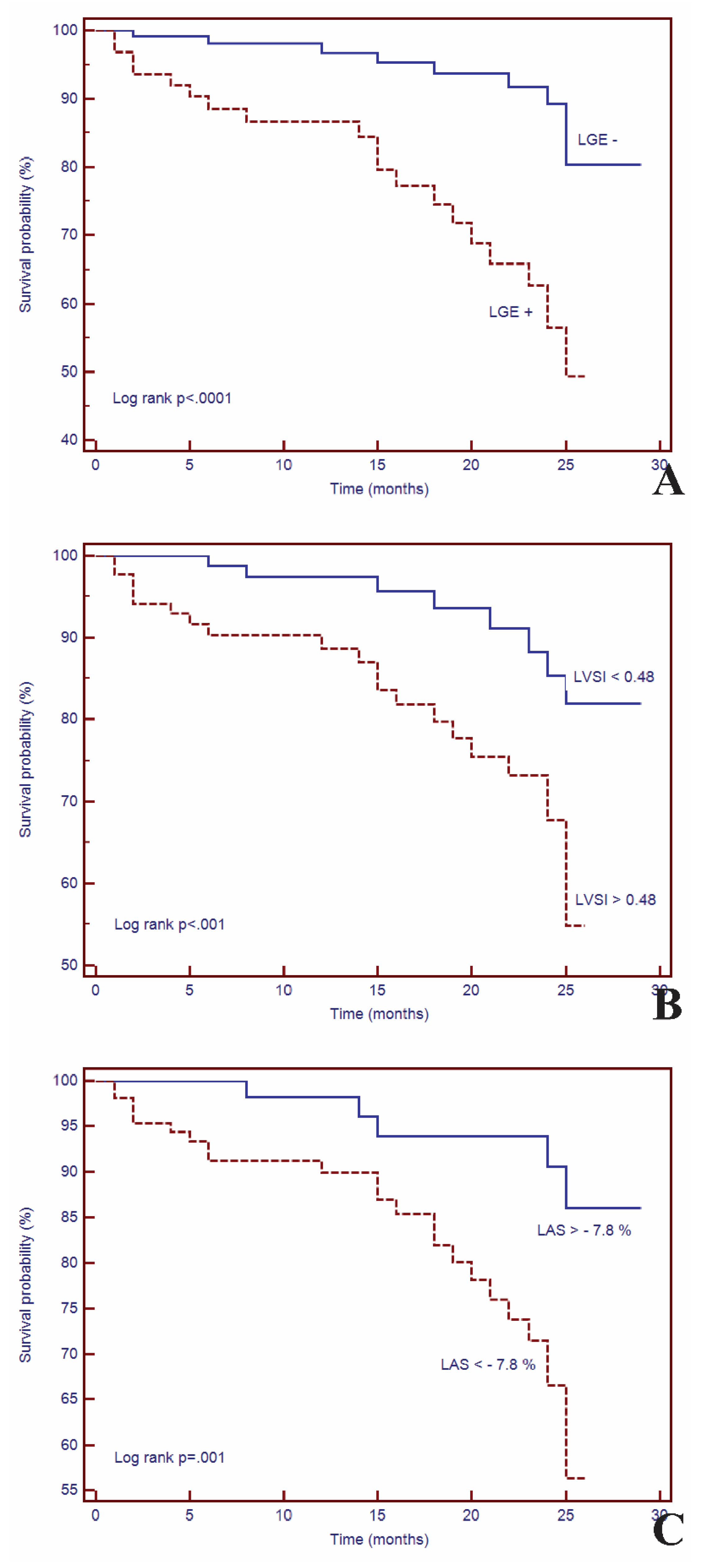
3.3. Survival Analysis
3.4. Univariate and Multivariate Cox Analysis
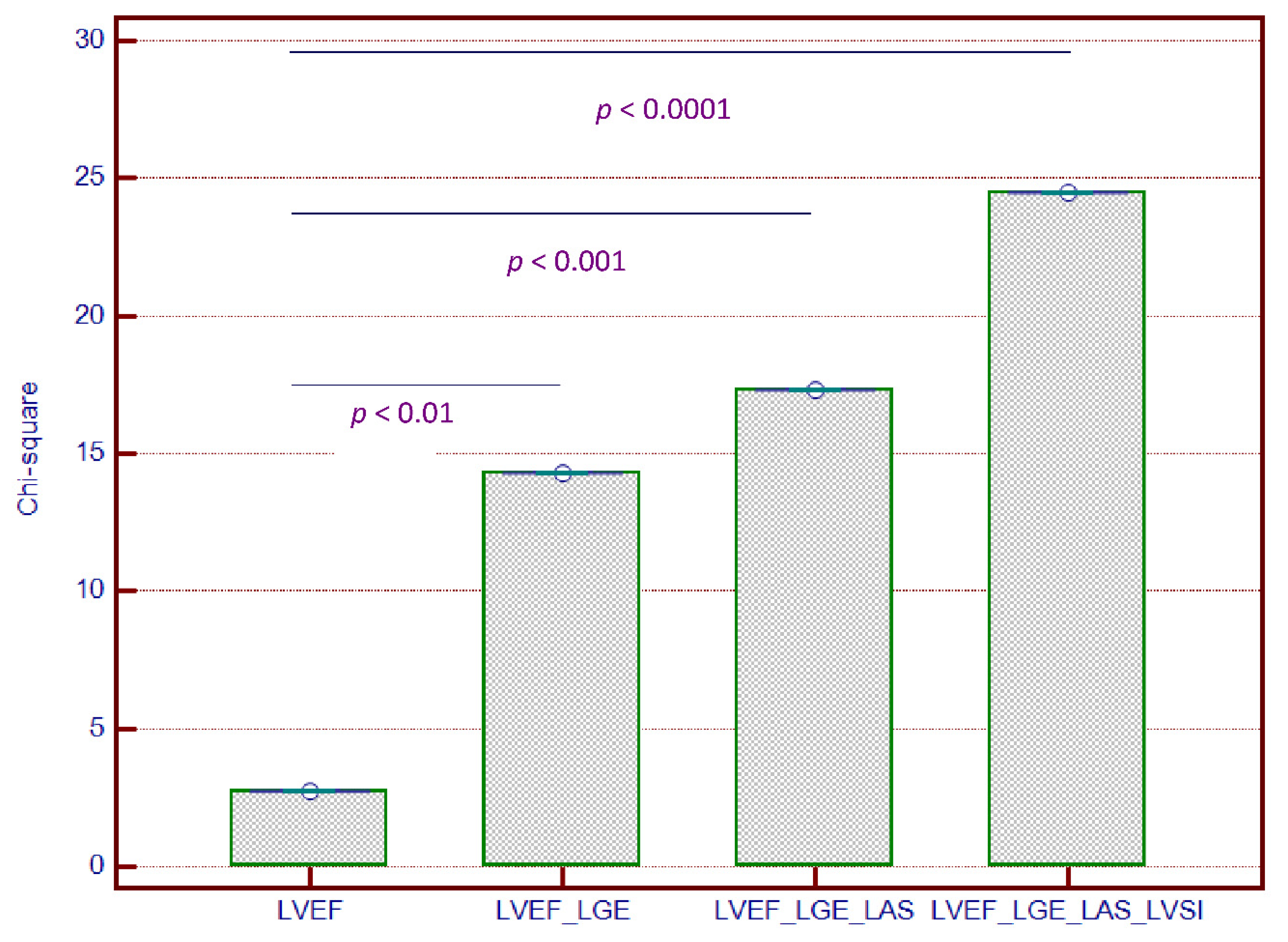
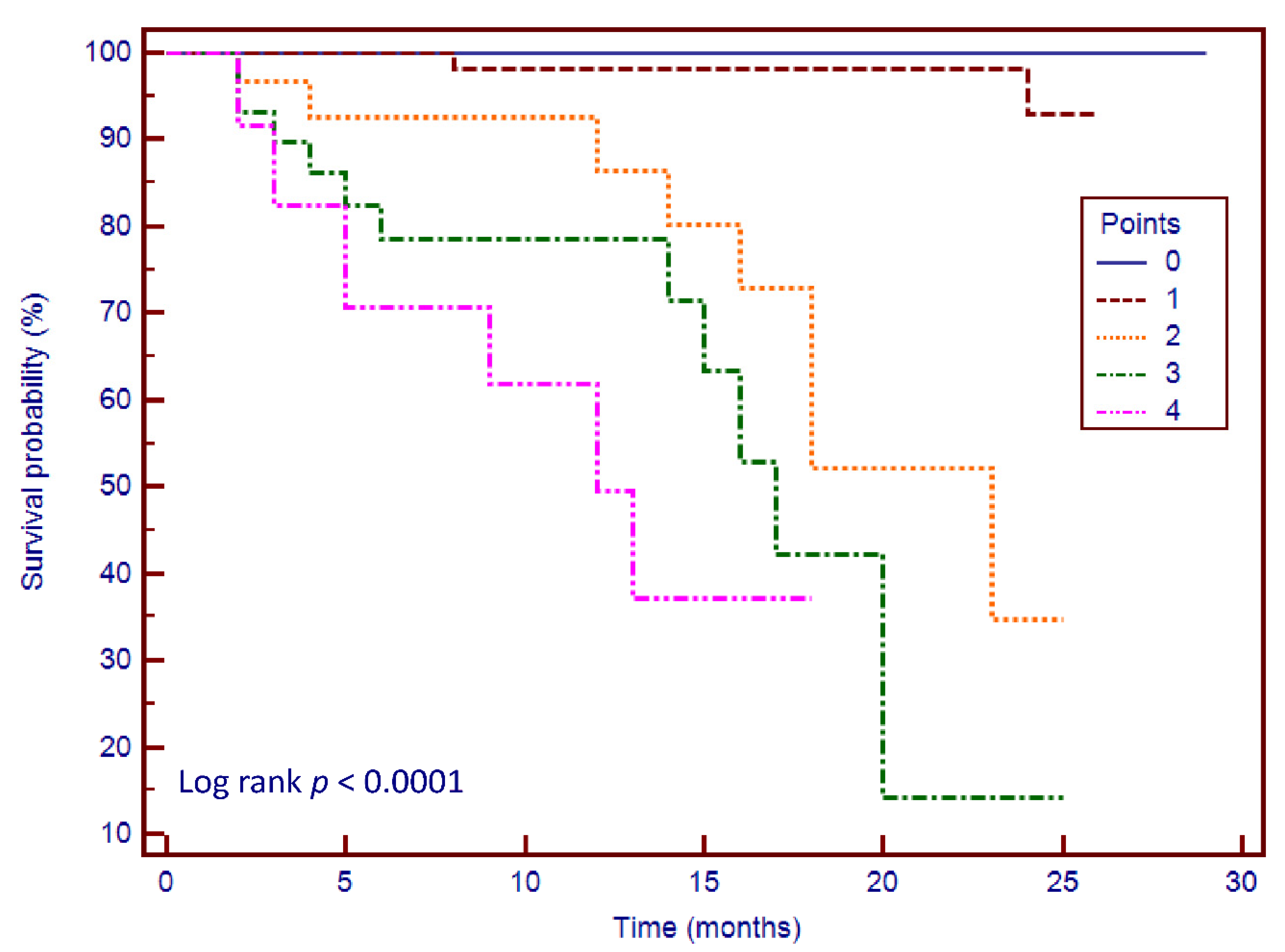
3.5. Incremental Predictive Value of cMRI-Based LV Geometry and Strain for Outcomes
3.6. Risk Stratification Scoring System
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pinto, Y.M.; Elliott, P.M.; Arbustini, E.; Adler, Y.; Anastasakis, A.; Böhm, M.; Duboc, D.; Gimeno, J.; de Groote, P.; Imazio, M.; et al. Proposal for a Revised Definition of Dilated Cardiomyopathy, Hypokinetic Non-Dilated Cardiomyopathy, and Its Implications for Clinical Practice: A Position Statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2016, 37, 1850–1858. [Google Scholar] [CrossRef] [PubMed]
- Felker, G.M.; Thompson, R.E.; Hare, J.M.; Hruban, R.H.; Clemetson, D.E.; Howard, D.L.; Baughman, K.L.; Kasper, E.K. Underlying Causes and Long-Term Survival in Patients with Initially Unexplained Cardiomyopathy. N. Engl. J. Med. 2000, 342, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Kadish, A.; Dyer, A.; Daubert, J.P.; Quigg, R.; Estes, N.A.M.; Anderson, K.P.; Calkins, H.; Hoch, D.; Goldberger, J.; Shalaby, A.; et al. Prophylactic Defibrillator Implantation in Patients with Nonischemic Dilated Cardiomyopathy. N. Engl. J. Med. 2004, 350, 2151–2158. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. J. Am. Coll. Cardiol. 2018, 72, e91–e220. [Google Scholar] [CrossRef]
- Buxton, A.E.; Ellison, K.E.; Lorvidhaya, P.; Ziv, O. Left Ventricular Ejection Fraction for Sudden Death Risk Stratification and Guiding Implantable Cardioverter-Defibrillators Implantation. J. Cardiovasc. Pharmacol. 2010, 55, 450–455. [Google Scholar]
- Iles, L.M.; Ellims, A.H.; Llewellyn, H.; Hare, J.L.; Kaye, D.M.; McLean, C.A.; Taylor, A.J. Histological Validation of Cardiac Magnetic Resonance Analysis of Regional and Diffuse Interstitial Myocardial Fibrosis. Eur. Heart J.Cardiovasc. Imaging 2015, 16, 14–22. [Google Scholar] [CrossRef]
- Halliday, B.P.; Gulati, A.; Ali, A.; Guha, K.; Newsome, S.; Arzanauskaite, M.; Vassiliou, V.S.; Lota, A.; Izgi, C.; Tayal, U.; et al. Association Between Midwall Late Gadolinium Enhancement and Sudden Cardiac Death in Patients With Dilated Cardiomyopathy and Mild and Moderate Left Ventricular Systolic Dysfunction. Circulation 2017, 135, 2106–2115. [Google Scholar] [CrossRef]
- Gulati, A.; Jabbour, A.; Ismail, T.F.; Guha, K.; Khwaja, J.; Raza, S.; Morarji, K.; Brown, T.D.H.; Ismail, N.A.; Dweck, M.R.; et al. Association of Fibrosis With Mortality and Sudden Cardiac Death in Patients with Nonischemic Dilated Cardiomyopathy. JAMA 2013, 309, 896. [Google Scholar] [CrossRef]
- Di Marco, A.; Anguera, I.; Schmitt, M.; Klem, I.; Neilan, T.G.; White, J.A.; Sramko, M.; Masci, P.G.; Barison, A.; Mckenna, P.; et al. Late Gadolinium Enhancement and the Risk for Ventricular Arrhythmias or Sudden Death in Dilated Cardiomyopathy. JACC Heart Fail. 2017, 5, 28–38. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Filho, O.R.; Mongeon, F.-P.; Mitchell, R.; Moreno, H.; Nadruz, W.; Kwong, R.; Jerosch-Herold, M. Role of Transcytolemmal Water-Exchange in Magnetic Resonance Measurements of Diffuse Myocardial Fibrosis in Hypertensive Heart Disease. Circ. Cardiovasc. Imaging 2013, 6, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Arenja, N.; Andre, F.; Riffel, J.H.; aus dem Siepen, F.; Hegenbart, U.; Schönland, S.; Kristen, A.V.; Katus, H.A.; Buss, S.J. Prognostic Value of Novel Imaging Parameters Derived from Standard Cardiovascular Magnetic Resonance in High Risk Patients with Systemic Light Chain Amyloidosis. J. Cardiovasc. Magn. Reson. 2019, 21, 53. [Google Scholar] [CrossRef]
- Tsadok, Y.; Friedman, Z.; Haluska, B.A.; Hoffmann, R.; Adam, D. Myocardial Strain Assessment by Cine Cardiac Magnetic Resonance Imaging Using Non-Rigid Registration. Magn. Reson. Imaging 2016, 34, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Li, W.; Zeng, R.; Sun, J.; Wan, K.; Xu, Y.; Cao, Y.; Zhang, Q.; Han, Y.; Chen, Y. Left Ventricular Spherical Index Is an Independent Predictor for Clinical Outcomes in Patients With Nonischemic Dilated Cardiomyopathy. JACC Cardiovasc. Imaging 2019, 12, 1578–1580. [Google Scholar] [CrossRef]
- Muthalaly, R.G.; Kwong, R.Y.; John, R.M.; van der Geest, R.J.; Tao, Q.; Schaeffer, B.; Tanigawa, S.; Nakamura, T.; Kaneko, K.; Tedrow, U.B.; et al. Left Ventricular Entropy Is a Novel Predictor of Arrhythmic Events in Patients With Dilated Cardiomyopathy Receiving Defibrillators for Primary Prevention. JACC Cardiovasc. Imaging 2019, 12, 1177–1184. [Google Scholar] [CrossRef]
- Kramer, C.M.; Barkhausen, J.; Flamm, S.D.; Kim, R.J.; Nagel, E. Standardized Cardiovascular Magnetic Resonance (CMR) Protocols 2013 Update. J. Cardiovasc. Magn. Reson. 2013, 15, 91. [Google Scholar] [CrossRef]
- Cerqueira, M.D.; Weissman, N.J.; Dilsizian, V.; Jacobs, A.K.; Kaul, S.; Laskey, W.K.; Pennell, D.J.; Rumberger, J.A.; Ryan, T.; Verani, M.S. Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart. Circulation 2002, 105, 539–542. [Google Scholar] [CrossRef]
- Bondarenko, O.; Beek, A.; Hofman, M.; Kühl, H.; Twisk, J.; van Dockum, W.; Visser, C.; van Rossum, A. Standardizing the Definition of Hyperenhancement in the Quantitative Assessment of Infarct Size and Myocardial Viability Using Delayed Contrast-Enhanced CMR. J. Cardiovasc. Magn. Reson. 2005, 7, 481–485. [Google Scholar] [CrossRef]
- Gao, P.; Yee, R.; Gula, L.; Krahn, A.D.; Skanes, A.; Leong-Sit, P.; Klein, G.J.; Stirrat, J.; Fine, N.; Pallaveshi, L.; et al. Prediction of Arrhythmic Events in Ischemic and Dilated Cardiomyopathy Patients Referred for Implantable Cardiac Defibrillator. Circ. Cardiovasc. Imaging 2012, 5, 448–456. [Google Scholar] [CrossRef]
- Piek, A.; de Boer, R.A.; Silljé, H.H.W. The Fibrosis-Cell Death Axis in Heart Failure. Heart Fail. Rev. 2016, 21, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Doltra, A.; Amundsen, B.; Gebker, R.; Fleck, E.; Kelle, S. Emerging Concepts for Myocardial Late Gadolinium Enhancement MRI. Curr. Cardiol. Rev. 2013, 9, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Lehrke, S.; Lossnitzer, D.; Schob, M.; Steen, H.; Merten, C.; Kemmling, H.; Pribe, R.; Ehlermann, P.; Zugck, C.; Korosoglou, G.; et al. Use of Cardiovascular Magnetic Resonance for Risk Stratification in Chronic Heart Failure: Prognostic Value of Late Gadolinium Enhancement in Patients with Non-Ischaemic Dilated Cardiomyopathy. Heart 2011, 97, 727–732. [Google Scholar] [CrossRef]
- Sree Raman, K.; Nucifora, G.; Leong, D.P.; Marx, C.; Shah, R.; Woodman, R.J.; Molaee, P.; Shirazi, M.G.; McGavigan, A.D.; De Pasquale, C.G.; et al. Long Term Prognostic Importance of Late Gadolinium Enhancement in First-Presentation Non-Ischaemic Dilated Cardiomyopathy. Int. J. Cardiol. 2019, 280, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Halliday, B.P.; Baksi, A.J.; Gulati, A.; Ali, A.; Newsome, S.; Izgi, C.; Arzanauskaite, M.; Lota, A.; Tayal, U.; Vassiliou, V.S.; et al. Outcome in Dilated Cardiomyopathy Related to the Extent, Location, and Pattern of Late Gadolinium Enhancement. JACC Cardiovasc. Imaging 2019, 12, 1645–1655. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.A.J.; Cornel, J.H.; van de Ven, P.M.; van Rossum, A.C.; Allaart, C.P.; Germans, T. The Prognostic Value of Late Gadolinium-Enhanced Cardiac Magnetic Resonance Imaging in Nonischemic Dilated Cardiomyopathy. JACC Cardiovasc. Imaging 2018, 11, 1274–1284. [Google Scholar] [CrossRef] [PubMed]
- Stolfo, D.; Merlo, M.; Pinamonti, B.; Barbati, G.; Di Lenarda, A.; Sinagra, G. Evolution of Left Ventricular Sphericity Index in Idiopathic Dilated Cardiomyopathy: Clinical and Prognostic Implications. Eur. Heart J. 2013, 34 (Suppl. 1), P1196. [Google Scholar] [CrossRef]
- Marchal, P.; Lairez, O.; Cognet, T.; Chabbert, V.; Barrier, P.; Berry, M.; Mejean, S.; Roncalli, J.; Rousseau, H.; Carrie, D.; et al. Relationship between Left Ventricular Sphericity and Trabeculation Indexes in Patients with Dilated Cardiomyopathy: A Cardiac Magnetic Resonance Study. Eur. Heart J.Cardiovasc. Imaging 2013, 14, 914–920. [Google Scholar] [CrossRef]
- Ben Halima, A.; Zidi, A. The Cardiac Magnetic Resonance Sphericity Index in the Dilated Cardiomyopathy: New Diagnostic and Prognostic Marker. Arch. Cardiovasc. Dis. Suppl. 2018, 10, 42. [Google Scholar] [CrossRef]
- Ambale-Venkatesh, B.; Yoneyama, K.; Sharma, R.K.; Ohyama, Y.; Wu, C.O.; Burke, G.L.; Shea, S.; Gomes, A.S.; Young, A.A.; Bluemke, D.A.; et al. Left Ventricular Shape Predicts Different Types of Cardiovascular Events in the General Population. Heart 2017, 103, 499–507. [Google Scholar] [CrossRef]
- Nakamori, S.; Ismail, H.; Ngo, L.H.; Manning, W.J.; Nezafat, R. Left Ventricular Geometry Predicts Ventricular Tachyarrhythmia in Patients with Left Ventricular Systolic Dysfunction: A Comprehensive Cardiovascular Magnetic Resonance Study. J. Cardiovasc. Magn. Reson. 2017, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Gjesdal, O.; Almeida, A.L.C.; Hopp, E.; Beitnes, J.O.; Lunde, K.; Smith, H.-J.; Lima, J.A.C.; Edvardsen, T. Long Axis Strain by MRI and Echocardiography in a Postmyocardial Infarct Population. J. Magn. Reson. Imaging 2014, 40, 1247–1251. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.; Backhaus, S.J.; Stiermaier, T.; Kowallick, J.T.; Stulle, A.; Koschalka, A.; Lotz, J.; Kutty, S.; Bigalke, B.; Gutberlet, M.; et al. Fast Manual Long-Axis Strain Assessment Provides Optimized Cardiovascular Event Prediction Following Myocardial Infarction. Eur. Heart J.Cardiovasc. Imaging 2019, 20, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Gjesdal, O.; Yoneyama, K.; Mewton, N.; Wu, C.; Gomes, A.S.; Hundley, G.; Prince, M.; Shea, S.; Liu, K.; Bluemke, D.A.; et al. Reduced Long Axis Strain Is Associated with Heart Failure and Cardiovascular Events in the Multi-Ethnic Study of Atherosclerosis. J. Magn. Reson. Imaging 2016, 44, 178–185. [Google Scholar] [CrossRef]
- Agoston-Coldea, L.; Bheecarry, K.; Cionca, C.; Petra, C.; Strimbu, L.; Ober, C.; Lupu, S.; Fodor, D.; Mocan, T. Incremental Predictive Value of Longitudinal Axis Strain and Late Gadolinium Enhancement Using Standard CMR Imaging in Patients with Aortic Stenosis. J. Clin. Med. 2019, 8, 165. [Google Scholar] [CrossRef]
- Riffel, J.H.; Keller, M.G.P.; Rost, F.; Arenja, N.; Andre, F.; aus dem Siepen, F.; Fritz, T.; Ehlermann, P.; Taeger, T.; Frankenstein, L.; et al. Left Ventricular Long Axis Strain: A New Prognosticator in Non-Ischemic Dilated Cardiomyopathy? J. Cardiovasc. Magn. Reson. 2016, 18, 36. [Google Scholar] [CrossRef]
- Kano, N.; Okumura, T.; Hiraiwa, H.; Watanabe, N.; Kondo, T.; Fukaya, K.; Sawamura, A.; Morimoto, R.; Bando, Y.; Murohara, T. Prognostic Impact of Combination of Sphericity Index and Late Gadolinium Enhancement on Cardiac Magnetic Resonance in Patients with Dilated Cardiomyopathy. J. Card. Fail. 2016, 22, S177. [Google Scholar] [CrossRef]
| All Patients n = 178 | LGE− n = 114 | LGE+ n = 64 | p-Value | |
|---|---|---|---|---|
| Clinical characteristics | ||||
| - Age, mean (SD), years | 48 (14.4) | 47 (15.0) | 45 (13.4) | NS |
| - Male gender, n (%) | 133 (74.7) | 83 (72.8) | 50 (78.1) | NS |
| - Body-mass index, kg/m2 | 27.4 (4.8) | 27.3 (4.4) | 27.5 (5.7) | NS |
| - Heart rate, mean (SD), bpm | 73 (16.0) | 71 (14.3) | 76 (18.3) | <0.05 |
| - Systolic blood pressure, mean (SD), mmHg | 133 (18.9) | 134 (18.4) | 130 (19.5) | NS |
| - Hypertension, n (%) | 98 (55.1) | 69 (60.5) | 29 (45.5) | <0.05 |
| - Diabetes mellitus, n (%) | 58 (32.5) | 41 (35.9) | 17 (26.5) | NS |
| - Dyslipidemia, n (%) | 104 (58.4) | 67 (58.8) | 37 (57.8) | NS |
| - Smoking, n (%) | 58 (32.5) | 39 (34.2) | 19 (29.6) | NS |
| - NYHA functional class I/II/III, n | 29/59/27 | 19/39/19 | 10/20/8 | <0.05 |
| Electrocardiogram | ||||
| - Atrial fibrillation, n (%) | 26 (14.6) | 18 (15.7) | 8 (12.5) | NS |
| - Left bundle branch block, n (%) | 15 (8.4) | 10 (8.7) | 5 (7.8) | NS |
| - Right bundle branch block, n (%) | 17 (9.5) | 12 (10.5) | 5 (7.8) | NS |
| - Significant Q waves, n (%) | 21 (11.8) | 14 (12.3) | 7 (10.9) | NS |
| Medications | ||||
| - Beta-blockers, n (%) | 142 (79.7) | 91 (79.8) | 51 (79.6) | NS |
| - ACEIs or ARBs, n (%) | 130 (73.0) | 84 (73.6) | 46 (71.8) | NS |
| - Calcium channel blockers, n (%) | 28 (15.7) | 18 (15.7) | 10 (15.6) | NS |
| - Statins, n (%) | 105 (58.9) | 67 (58.7) | 38 (59.3) | NS |
| - Antiplatelet therapy, n (%) | 68 (38.2) | 44 (38.5) | 25 (37.5) | NS |
| - Diuretics, n (%) | 111 (62.3) | 70 (61.4) | 41 (64.0) | NS |
| - Digitalis, n (%) | 13 (7.3) | 8 (7.0) | 5 (7.8) | NS |
| Biomarker levels | ||||
| - NT-proBNP, median (IQR), pg/mL | 2639.5 (378–11,960) | 2600 (378–9893) | 2679 (570–11,960) | NS |
| - eGFR, mean (SD), ml/min/1.73 m2 | 87.1 (21.2) | 87.7 (20.4) | 86.1 (22.6) | NS |
| Echocardiography | ||||
| - E/E’ ratio, mean (SD) | 9.27 (2.5) | 8.2 (2.4) | 12.3 (2.6) | <0.001 |
| - DT, mean (SD), ms | 217 (56.7) | 215 (53.4) | 221 (63.1) | NS |
| - sPAP, mean (SD), mmHg | 30.8 (12.0) | 30.1 (12.5) | 32.2 (11.0) | NS |
| Cardiovascular magnetic resonance | ||||
| - LVEDV index, mean (SD), mL/m2 | 132.3 (34.5) | 124.8 (30.2) | 145.5 (37.8) | <0.001 |
| - LVESV index, mean (SD), mL/m2 | 87.5 (34.4) | 78.6 (29.6) | 103.5 (36.8) | <0.001 |
| - LVM index, mean (SD), g/m2 | 86.7 (20.6) | 83.7 (19.6) | 92.0 (21.6) | <0.01 |
| - LVEF, mean (SD), % | 35.0 (9.3) | 37.8 (7.7) | 29.9 (9.7) | <0.001 |
| - LAV index, mean (SD), mL/m2 | 55.8 (21.3) | 53.1 (20.4) | 60.6 (22.2) | <0.05 |
| - LAS, mean (SD), % | −9.6 (5.3) | −10.7 (5.4) | −7.8 (4.6) | <0.001 |
| - LVSI, mean (SD) | 0.40 (0.12) | 0.38 (0.11) | 0.43 (0.13) | <0.001 |
| - TAPSE, mean (SD), mm | 18.6 (5.2) | 19.5 (5.3) | 16.9 (4.7) | 0.001 |
| - RVEDV index, mean (SD), mL/m2 | 53.4 (21.2) | 52.7 (19.2) | 54.7 (24.4) | NS |
| - RVESV index, mean (SD), mL/m2 | 29.0 (15.5) | 27.2 (11.9) | 32.2 (20.0) | <0.01 |
| - RVEF, mean (SD), % | 46.8 (9.55) | 49.0 (8.7) | 42.8 (9.7) | <0.01 |
| - LV-LGE mass median (IQR), g | 30.5 (1–88) | |||
| - LV-LGE mass/LVM, median (IQR), % | 17.2 (0.6–54) |
| Parameters | Coefficient Kappa | 95% Confidence Interval | Standard Error |
|---|---|---|---|
| Inter-observer | |||
| LVEF | 0.91 | 0.872 to 0.941 | 0.026 |
| LAS | 0.97 | 0.909 to 0.989 | 0.012 |
| LGE | 0.88 | 0.771 to 0.939 | 0.066 |
| LVSI | 0.93 | 0.856 to 0.952 | 0.029 |
| Intra-observer | |||
| LVEF | 0.98 | 0.977 to 0.992 | 0.009 |
| LAS | 0.98 | 0.967 to 0.991 | 0.004 |
| LGE | 0.90 | 0.835 to 0.948 | 0.023 |
| LVSI | 0.92 | 0.871 to 0.928 | 0.032 |
| No Events n = 147 | Events n = 31 | Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|---|---|
| Unadjusted HR (95% CI) | p Value | Adjusted HR (95% CI) | p Value | |||
| Age, years | 48 (13.8) | 48 (17.5) | 1.00 (0.98–1.03) | NS | ||
| Male gender, n, % | 111 (75.5) | 22 (37.9) | 1.14 (0.53–2.48) | NS | ||
| Body-mass index, kg/m2 | 27.7 (4.8) | 25.8 (4.5) | 0.94 (0.87–1.01) | NS | ||
| Systolic blood pressure | 134 (19.2) | 130 (17.4) | 0.99 (0.97–1.01) | NS | ||
| NT-proBNP, pg/mL | 2564 (378–11960) | 2834 (834–9892) | 1.00 (0.99–1.01) | NS | ||
| eGFR, ml/min/1.73 m2 | 86.3 (20.1) | 91.0 (25.9) | 1.01 (0.97–1.03) | NS | ||
| LVEDV index, mL/m2 | 131.4 (35.6) | 136.6 (32.7) | 1.01 (0.99–1.01) | NS | ||
| LVESV index, mL/m2 | 86.4 (34.5) | 93.1 (33.8) | 1.05 (0.98–1.07) | NS | ||
| LVM index, g/m2 | 87.0 (20.7) | 85.2 (20.8) | 0.99 (0.97–1.01) | NS | ||
| LVEF, % | 35.5 (9.2) | 32.4 (9.4) | 0.97 (0.93–1.01) | NS | ||
| LAV index, mL/m2 | 54.7 (21.7) | 61.3 (18.6) | 1.01 (1.00–1.03) | NS | ||
| LGE+ | 43 (29.2) | 21 (67.7) | 4.03 (1.90–8.52) | <0.0001 | 1.77 (2.79–12.51) | <0.0001 |
| LGE mass, g | 11.3 (10.6) | 28.8 (19.3) | 1.23 (1.90–4.52) | <0.0001 | 1.43 (1.01–6.12) | <0.001 |
| LAS, % | −10.0 (5.6) | −7.8 (3.6) | 1.19 (1.01–2.18) | <0.001 | 1.32 (1.54–9.14) | 0.001 |
| LVSI, % | 0.38 (0.11) | 0.48 (0.13) | 2.13 (1.05–8.11) | <0.001 | 1.17 (1.14–7.19) | <0.01 |
| E/E’ ratio | 9.1 (2.3) | 15.7 (4.8) | 1.08 (0.95–1.22) | <0.05 | 1.02 (0.92–1.01) | NS |
| TAPSE, mm | 18.8 (5.2) | 17.4 (5.4) | 0.77 (0.70–0.84) | NS | ||
| RVEDV index, mL/m2 | 53.3 (19.7) | 53.8 (27.6) | 1.00 (0.98–1.02) | NS | ||
| RVESV index, mL/m2 | 28.2 (13.5) | 32.4 (13.9) | 1.02 (1.00–1.04) | NS | ||
| RVEF, % | 47.5 (9.3) | 43.4 (10.2) | 0.84 (0.79–0.88) | NS | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cojan-Minzat, B.O.; Zlibut, A.; Muresan, I.D.; Cionca, C.; Horvat, D.; Kiss, E.; Revnic, R.; Florea, M.; Ciortea, R.; Agoston-Coldea, L. Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy. J. Clin. Med. 2020, 9, 1997. https://doi.org/10.3390/jcm9061997
Cojan-Minzat BO, Zlibut A, Muresan ID, Cionca C, Horvat D, Kiss E, Revnic R, Florea M, Ciortea R, Agoston-Coldea L. Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy. Journal of Clinical Medicine. 2020; 9(6):1997. https://doi.org/10.3390/jcm9061997
Chicago/Turabian StyleCojan-Minzat, Bianca Olivia, Alexandru Zlibut, Ioana Danuta Muresan, Carmen Cionca, Dalma Horvat, Eva Kiss, Radu Revnic, Mira Florea, Razvan Ciortea, and Lucia Agoston-Coldea. 2020. "Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy" Journal of Clinical Medicine 9, no. 6: 1997. https://doi.org/10.3390/jcm9061997
APA StyleCojan-Minzat, B. O., Zlibut, A., Muresan, I. D., Cionca, C., Horvat, D., Kiss, E., Revnic, R., Florea, M., Ciortea, R., & Agoston-Coldea, L. (2020). Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy. Journal of Clinical Medicine, 9(6), 1997. https://doi.org/10.3390/jcm9061997





