An Examination of Clinician Responses to Problem Gambling in Community Mental Health Services
Abstract
1. Introduction
2. Experimental Section
2.1. Design and Sample
2.2. Measures
2.3. Recruitment/Procedure
2.4. Data Analysis
3. Results
3.1. Gambling Problems as a Percentage of Clinician Caseloads
3.2. Previous Training in Problem Gambling
3.3. Gambling and Mental Illness Knowledge
3.4. Attitudes Towards Responding to Gambling Issues
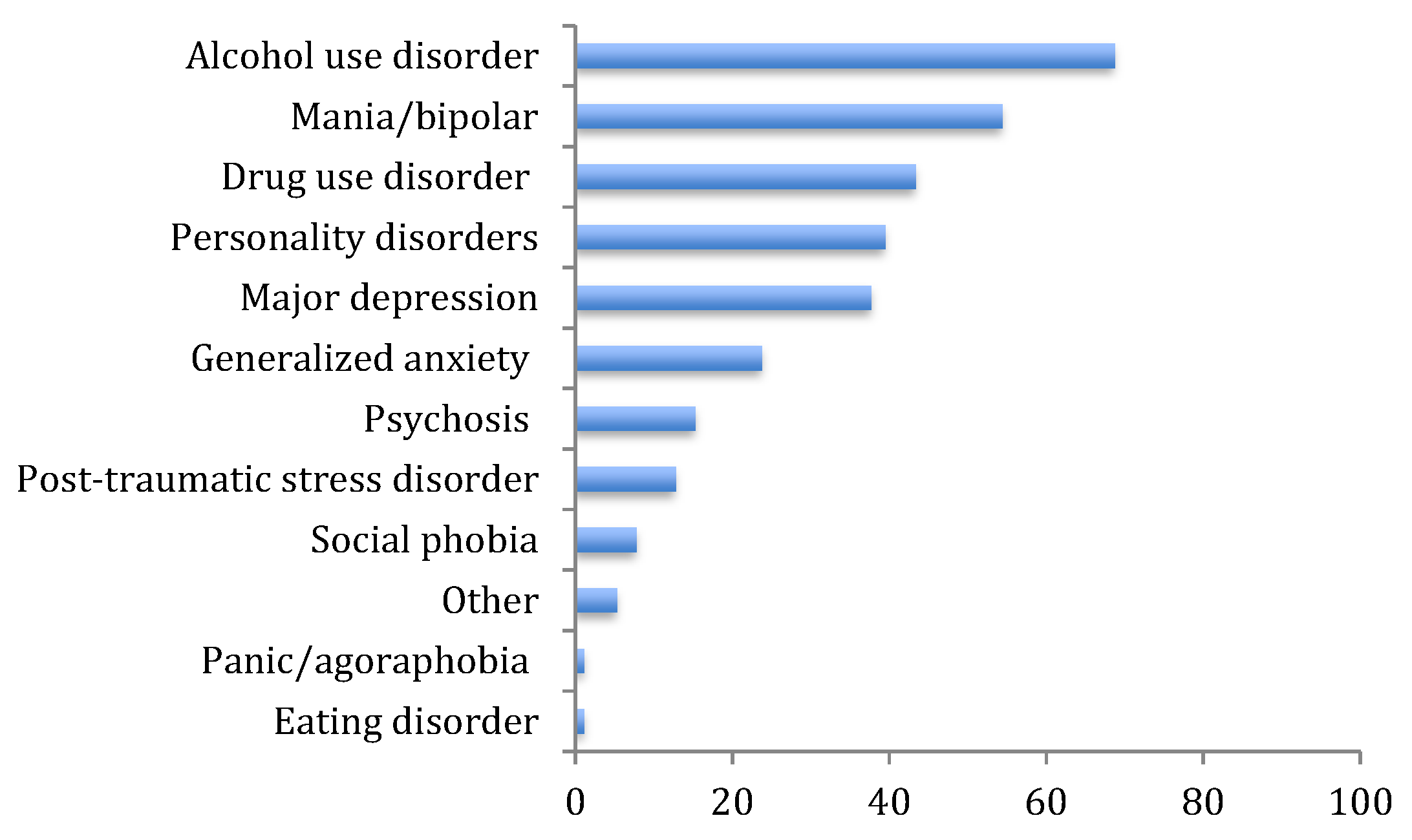
3.5. Comorbidity
3.6. Screening and Assessment
3.7. Actions Taken Following Identification
3.8. Referral
3.9. Treatment
3.10. Differences in Clinician Response by Profession
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Psychological Association (APA). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Arlington, VA, USA, 2013. [Google Scholar]
- Neal, P.; Delfabbro, P.H.; O’Neil, M. Problem Gambling and Harm: Towards a National Definition; Gambling Research Australia: Melbourne, Australia, 2005. [Google Scholar]
- Williams, R.J.; Volberg, R.A.; Stevens, R.M. The Population Prevalence of Problem Gambling: Methodological Influences, Standardized Rates, Jurisdictional Differences, and Worldwide Trends; Ontario Problem Gambling Research Centre: Guelph, ON, Canada; Ontario Ministry of Health and Long-Term Care: Toronto, ON, Canada, 2012.
- Dowling, N.A.; Youssef, G.; Jackson, A.C.; Pennay, D.; Francis, K.L.; Pennay, A.; Lubman, D.I. National estimates of Australian gambling prevalence: F indings from a dual-frame omnibus survey. Addiction 2016, 111, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Gainsbury, S.M.; Russell, A.; Hing, N.; Wood, R.; Lubman, D.I.; Blaszczynski, A. The prevalence and determinants of problem gambling in Australia: Assessing the impact of interactive gambling and new technologies. Psychol. Addict. Behav. 2014, 28, 769–779. [Google Scholar] [CrossRef]
- Queensland Government Statistician’s Office, Queensland Treasury. Australian Gambling Statistics; Queensland Government Statistician’s Office, Queensland Treasury: Toronto, ON, Canada, 2019.
- Rockloff, M.; Browne, M.; Hing, N.; Thorne, H.; Russell, A.; Greer, N.; Tran, K.; Brook, K.; Sproston, K. Victorian Population Gambling and Health Study 2018–2019; Victorian Responsible Gambling Foundation: North Melbourne, Australia, 2020. [Google Scholar]
- Lorains, F.K.; Cowlishaw, S.; Thomas, S.A. Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction 2011, 106, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Harrison, G.W.; Lau, M.I.; Ross, D. The Risk of Gambling Problems in the General Population: A Reconsideration. J. Gambl. Stud. 2019, 1–27. [Google Scholar] [CrossRef]
- Dowling, N.A.; Cowlishaw, S.; Jackson, A.C.; Merkouris, S.S.; Francis, K.L.; Christensen, D.R. Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Aust. N. Z. J. Psychiatry 2015, 49, 519–539. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N.; Merkouris, S.; Greenwood, C.; Oldenhof, E.; Toumbourou, J.; Youssef, G. Early risk and protective factors for problem gambling: A systematic review and meta-analysis of longitudinal studies. Clin. Psychol. Rev. 2017, 51, 109–124. [Google Scholar] [CrossRef]
- Dowling, N.A.; Butera, C.A.; Merkouris, S.S.; Youssef, G.J.; Rodda, S.N.; Jackson, A.C. The Reciprocal Association between Problem Gambling and Mental Health Symptoms/Substance Use: Cross-Lagged Path Modelling of Longitudinal Cohort Data. J. Clin. Med. 2019, 8, 1888. [Google Scholar] [CrossRef]
- Cowlishaw, S.; Hakes, J.; Dowling, N.A. Gambling problems in treatment for affective disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J. Affect. Disord. 2016, 202, 110–114. [Google Scholar] [CrossRef][Green Version]
- Cowlishaw, S.; Hakes, J.K. Pathological and problem gambling in substance use treatment: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Am. J. Addict. 2015, 24, 467–474. [Google Scholar] [CrossRef]
- Haydock, M.; Cowlishaw, S.; Harvey, C.; Castle, D. Prevalence and correlates of problem gambling in people with psychotic disorders. Compr. Psychiatry 2015, 58, 122–129. [Google Scholar] [CrossRef]
- Kim, H.S.; Cassetta, B.D.; Hodgins, D.C.; McGrath, D.S.; Tomfohr-Madsen, L.M.; Tavares, H. Comorbid addictive behaviors in disordered gamblers with psychosis. Braz. J. Psychiatry 2018, 40, 441–443. [Google Scholar] [CrossRef] [PubMed]
- Biddle, D.; Hawthorne, G.; Forbes, D.; Coman, G. Problem gambling in Australian PTSD treatment-seeking veterans. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2005, 18, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, S.H.; Welsh, B.R.; Fulton, K.; Soczynska, J.K.; McIntyre, R.S.; O’Donovan, C.; Milev, R.; le Melledo, J.-M.; Bisserbe, J.-C.; Zimmerman, M. Frequency and correlates of gambling problems in outpatients with major depressive disorder and bipolar disorder. Can. J. Psychiatry 2010, 55, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Ferris, J.A.; Wynne, H.J. The Canadian Problem Gambling Index. Canadian Centre on Substance Abuse: Ottawa, ON, Canada, 2001. [Google Scholar]
- Manning, V.; Dowling, N.A.; Lee, S.; Rodda, S.; Garfield, J.B.B.; Volberg, R.; Kulkarni, J.; Lubman, D.I. Problem gambling and substance use in patients attending community mental health services. J. Behav. Addict. 2017, 6, 678–688. [Google Scholar] [CrossRef]
- Browne, M.; Greer, N.; Rawat, V.; Rockloff, M. A population-level metric for gambling-related harm. Int. Gambl. Stud. 2017, 17, 163–175. [Google Scholar] [CrossRef]
- Browne, M.; Langham, E.; Rawat, V.; Greer, N.; Li, E.; Rose, J.; Rockloff, M.; Donaldson, P.; Thorne, H.; Goodwin, B. Assessing Gambling-Related Harm in Victoria: A Public Health Perspective; Victorian Responsible Gambling Foundation: North Melbourne, Australia, 2016. [Google Scholar]
- Consulting, S.; Hare, S. Study of Gambling and Health in Victoria: Findings from the Victorian Prevalence Study 2014; Victorian Responsible Gambling Foundation: North Melbourne, Australia, 2015. [Google Scholar]
- Evans, L.; Delfabbro, P.H. Motivators for Change and Barriers to Help-Seeking in Australian Problem Gamblers. J. Gambl. Stud. 2005, 21, 133–155. [Google Scholar] [CrossRef]
- Suurvali, H.; Hodgins, D.; Toneatto, T.; Cunningham, J. Treatment Seeking among Ontario Problem Gamblers: Results of a Population Survey. Psychiatr. Serv. 2008, 59, 1343–1346. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Holzinger, A.; Matschinger, H. Emotional reactions to people with mental illness. Epidemiol. Psychiatr. Sci. 2010, 19, 26–32. [Google Scholar] [CrossRef]
- Linz, S.J.; Sturm, B.A. The phenomenon of social isolation in the severely mentally ill. Perspect. Psychiatr. Care 2013, 49, 243–254. [Google Scholar] [CrossRef]
- Dowling, N.A.; Merkouris, S.S.; Manning, V.; Volberg, R.; Lee, S.J.; Rodda, S.N.; Lubman, D.I. Screening for problem gambling within mental health services: A comparison of the classification accuracy of brief instruments. Addiction 2018, 113, 1088–1104. [Google Scholar] [CrossRef]
- Sanju, G.; Gerada, C. Problem gamblers in primary care: Can GPs do more? Br. J. Gen. Pract. 2011, 61, 248. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thomas, S.A.; Piterman, L.; Jackson, A.C. Problem gambling: What do general practitioners need to know and do about it? Med. J. Aust. 2008, 189, 135–136. [Google Scholar] [CrossRef] [PubMed]
- Tolchard, B.; Thomas, L.; Battersby, M. GPs and Problem Gambling: Can they Help with Identification and Early Intervention? J. Gambl. Stud. 2007, 23, 499–506. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Christensen, M.H.; Patsdaughter, C.A.; Babington, L.M. Health care providers’ experiences with problem gamblers. J. Gambl. Stud. 2001, 17, 71–79. [Google Scholar] [CrossRef]
- Achab, S.; Chatton, A.; Khan, R.; Thorens, G.; Penzenstadler, L.; Zullino, D.; Khazaal, Y. Early detection of pathological gambling: Betting on GPs’ beliefs and attitudes. BioMed Res. Int. 2014. [Google Scholar] [CrossRef]
- Rowan, M.S.; Galasso, C.S. Identifying office resource needs of Canadian physicians to help prevent, assess and treat patients with substance use and pathological gambling disorders. J. Addict. Dis. 2000, 19, 43–58. [Google Scholar] [CrossRef]
- Roberts, A.; Bowden-Jones, H.; Roberts, D.; Sharman, S. Should GPs routinely screen for gambling disorders? Br. J. Gen. Pract. 2019. [Google Scholar] [CrossRef]
- Rodda, S.; Manning, V.; Dowling, N.; Lee, S.; Lubman, D. Barriers and facilitators of responding to problem gambling: Perspectives from Australian mental health services. J. Gambl. Stud. 2018, 34, 307–320. [Google Scholar] [CrossRef]
- Lubman, D.; Manning, V.; Dowling, N.A.; Rodda, S.; Lee, S.; Garde, E.; Merkouris, S.; Volberg, R. Problem Gambling in People Seeking Treatment for Mental Illness; Victorian Responsible Gambling Foundation: North Mebourne, Australia, 2017. [Google Scholar]
- Hides, L.; Lubman, D.; Elkins, K.; Catania, L.; Rogers, N. Feasibility and acceptability of a mental health screening tool and training programme in the youth alcohol and other drug (AOD) sector. Drug Alcohol Rev. 2007, 26, 509–515. [Google Scholar] [CrossRef]
- Corney, R. Continuing Professional Development for General Practitioners in the United Kingdom. J. Gambl. Issues 2011. [Google Scholar] [CrossRef][Green Version]
- Sullivan, S.; Arroll, B.; Coster, G.; Abbott, M.; Adams, P. Problem gamblers: Do GPs want to intervene? N. Z. Med. J. 2000, 113, 204–207. [Google Scholar] [PubMed]
- Sullivan, S.; McCormick, R.; Lamont, M.; Penfold, A. Problem gambling: Patients affected by their own or another’s gambling may approve of help from general practitioners. N. Z. Med. J. 2007, 120, U2605, 2601–2608. [Google Scholar]
- Temcheff, C.E.; Derevensky, J.L.; St-Pierre, R.A.; Gupta, R.; Martin, I. Beliefs and attitudes of mental health professionals with respect to gambling and other high risk behaviors in schools. Int. J. Ment. Health Addict. 2014, 12, 716–729. [Google Scholar] [CrossRef]
- Suurvali, H.; Cordingley, J.; Hodgins, D.C.; Cunningham, J. Barriers to seeking help for gambling problems: A review of the empirical literature. J. Gambl. Stud. 2009, 25, 407–424. [Google Scholar] [CrossRef] [PubMed]
- Tavares, H.; Zilberman, M.L.; Beites, F.J.; Gentil, V. Brief communications: Gender differences in gambling progression. J. Gambl. Stud. 2001, 17, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.A.; Merkouris, S.S.; Radermacher, H.L.; Dowling, N.A.; Misso, M.L.; Anderson, C.J.; Jackson, A.C. Australian guideline for treatment of problem gambling: An abridged outline. Med. J. Aust. 2011, 195, 664–665. [Google Scholar] [CrossRef]
- Lubman, D.I.; Hides, L.; Elkins, K. Developing integrated models of care within the youth Alcohol and Other Drug sector. Australas. Psychiatry 2008, 16, 363–366. [Google Scholar] [CrossRef]
- PGRTC. Guideline for Screening, Assessment and Treatment in Problem and Pathological Gambling; Problem Gambling Research and Treatment Centre: Clayton, Australia, 2011. [Google Scholar]
- Armstrong, A.; Carroll, M. Gambling Activity in Australia; Australian Gambling Research Centre, Australian Institute of Family Studies: Melbourne, Australia, 2017. [Google Scholar]
- Dowling, N.; Merkouris, S.; Dias, S.; Rodda, S.; Manning, V.; Youssef, G.; Lubman, D.; Volberg, R. The diagnostic accuracy of brief screening instruments for problem gambling: A systematic review and meta-analysis. Clin. Psychol. Rev. 2019, 74, 101784. [Google Scholar] [CrossRef]
- Karlsson, A.; Håkansson, A. Gambling disorder, increased mortality, suicidality, and associated comorbidity: A longitudinal nationwide register study. J. Behav. Addict. 2018, 7, 1091–1099. [Google Scholar] [CrossRef]
- Thomas, A.C.; Staiger, P.K. Introducing mental health and substance use screening into a community-based health service in Australia: Usefulness and implications for service change. Health Soc. Care Community 2012, 20, 635–644. [Google Scholar] [CrossRef]
- Thomas, A.C.; Staiger, P.K.; McCabe, M. Implementation and evaluation of brief depression and anxiety screening in clients contacting a drug and alcohol service. Drug Alcohol Rev. 2012, 31, 303–310. [Google Scholar] [CrossRef] [PubMed]
- van der Maas, M.; Shi, J.; Elton-Marshall, T.; Hodgins, D.C.; Sanchez, S.; Lobo, D.S.; Hagopian, S.; Turner, N.E. Internet-based interventions for problem gambling: Scoping review. JMIR Ment. Health 2019, 6, e65. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.M.; Maybery, D. Dual diagnosis discourse in Victoria Australia: The responsiveness of mental health services. J. Dual Diagn. 2014, 10, 139–144. [Google Scholar] [CrossRef]
- Savic, M.; Best, D.; Manning, V.; Lubman, D.I. Strategies to facilitate integrated care for people with alcohol and other drug problems: A systematic review. Subst. Abus. Treat. Prev. Policy 2017, 12, 19. [Google Scholar] [CrossRef] [PubMed]
| Total Sample (n = 281) | |
|---|---|
| Age (years), mean (range) | 40.10 (20–67 years) |
| Male (n, %) | 77 (27.4) |
| Profession (n, %) | |
| Medical | 62 (22.1%) |
| Nurse | 78 (27.8%) |
| Social worker | 31 (11.0%) |
| Psychologist | 17 (6.0%) |
| Occupational therapist | 17 (6.0%) |
| Support worker | 56 (19.9%) |
| Other | 17 (6.0%) |
| Missing | 3 (1.1%) |
| Type of service (n, %) | |
| Public mental health service (adult) | 203 (72.3%) |
| Private mental health service | 10 (3.6%) |
| Primary healthcare | 23 (8.2%) |
| MHCSS/PDRSS | 45 (16.0%) |
| Practice duration (years), mean (range) | 12.1 (<1 year–40 years) |
| Strongly Agree/Agree | Uncertain | Disagree/Strongly Disagree | Missing | |
|---|---|---|---|---|
| Problem gambling and mental illness commonly occur together | 178 (63.3%) | 83 (29.5%) | 20 (7.1%) | 0 |
| Problem gambling can worsen a patient’s mental illness | 265 (94.3%) | 14 (5.0%) | 1 (0.4%) | 1 (0.3%) |
| I understand what causes and/or maintains problem gambling issues | 125 (44.4%) | 115(38.9%) | 40 (14.2%) | 1 (0.4%) |
| I am aware of screening and assessment tools available for detection of problem gambling | 32 (11.4%) | 64 (22.8%) | 184 (65.4%) | 1 (0.4%) |
| Strongly Agree/Agree | Uncertain | Strongly Disagree /Disagree | Missing | |
|---|---|---|---|---|
| There is no point conducting gambling screening as my service does not treat problem gamblers | 13 (4.7%) | 29 (10.3%) | 237 (84.3%) | 2 (0.7%) |
| Gambling disorder is not really a mental health disorder | 17 (6.1%) | 44 (15.7%) | 219 (78.0%) | 1 (0.4%) |
| Detecting problem gambling does not require a formal screen; it can just be addressed if a patient mentions it | 40 (14.2%) | 56 (19.9%) | 183 (65.1%) | 2 (0.7%) |
| Use of standardized screening tools is only necessary if a patient mentions gambling | 34 (12.1%) | 70 (24.9%) | 173 (61.6%) | 4 (1.4%) |
| People accessing mental health treatment do not want to be screened for gambling problems | 27 (9.6%) | 101 (35.9%) | 151 (53.7%) | 2 (0.7%) |
| There are too many more important issues to screen for problem gambling | 30 (10.7%) | 41 (14.6%) | 207 (70.7%) | 3 (1.1%) |
| Problem gambling does not co-occur with mental health problems often enough to bother screening | 8 (2.8%) | 50 (17.8%) | 220 (78.3%) | 3 (1.1%) |
| There is not enough time to conduct problem gambling screening or assessment in my workplace | 65 (20.9%) | 75 (24.1%) | 167 (53.7%) | 4 (1.3%) |
| Screening/assessment and referral for problem gambling is not part of my job | 20 (7.1%) | 36 (12.8%) | 222 (79.0%) | 3 (1.1%) |
| It is important to identify gambling problems among mental health patients | 253 (90%) | 13 (4.6%) | 12 (4.9%) | 1 (0.4%) |
| A brief problem gambling screen would be a useful part of my routine clinical practice | 111 (75.1%) | 43 (15.3%) | 26 (9.2%) | 1 (0.4%) |
| Sample (n = 281) | Strongly Agree/Agree | Uncertain | Disagree/Strongly Disagree | Missing |
|---|---|---|---|---|
| I have a good understanding about the Gambler’s Help service system and the programs available | 65 (23.2%) | 65 (23.1%) | 150 (53.3%) | 1 (0.4%) |
| I understand the types of treatments that have proven helpful for PG | 62 (22.0%) | 79 (28.1%) | 129 (49.5%) | 1 (0.4%) |
| Mental health and PG clinicians can effectively work together to support patients | 134 (83.3%) | 35 (12.5%) | 10 (3.5%) | 2 (0.7%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manning, V.; Dowling, N.A.; Rodda, S.N.; Cheetham, A.; Lubman, D.I. An Examination of Clinician Responses to Problem Gambling in Community Mental Health Services. J. Clin. Med. 2020, 9, 2075. https://doi.org/10.3390/jcm9072075
Manning V, Dowling NA, Rodda SN, Cheetham A, Lubman DI. An Examination of Clinician Responses to Problem Gambling in Community Mental Health Services. Journal of Clinical Medicine. 2020; 9(7):2075. https://doi.org/10.3390/jcm9072075
Chicago/Turabian StyleManning, Victoria, Nicki A. Dowling, Simone N. Rodda, Ali Cheetham, and Dan I. Lubman. 2020. "An Examination of Clinician Responses to Problem Gambling in Community Mental Health Services" Journal of Clinical Medicine 9, no. 7: 2075. https://doi.org/10.3390/jcm9072075
APA StyleManning, V., Dowling, N. A., Rodda, S. N., Cheetham, A., & Lubman, D. I. (2020). An Examination of Clinician Responses to Problem Gambling in Community Mental Health Services. Journal of Clinical Medicine, 9(7), 2075. https://doi.org/10.3390/jcm9072075




