Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Design and Ethical Approval
2.2. Type of Participants and Inclusion Criteria
2.3. Cephalometric Analysis
2.4. Statistical Analysis
3. Results
3.1. Comparisons within Juvenile Idiopathic Arthritis (JIA) Patients
3.2. Comparisons within Control Patients
3.3. Comparisons between JIA Patients and Control Group
3.4. Comparisons between Non-Affected and Affected Side in JIA Patients and between Right and Left Side in Control Group
3.5. Other Clinical Evaluations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jordan, A.; McDonagh, J.E. Juvenile idiopathic arthritis: The paediatric perspective. Pediatr. Radiol. 2006, 36, 734–742. [Google Scholar] [CrossRef] [PubMed]
- Giancane, G.; Consolaro, A.; Lanni, S.; Davì, S.; Schiappapietra, B.; Ravelli, A.; Ruperto, N.; Martini, A. Juvenile Idiopathic Arthritis: Diagnosis and Treatment. Rheumatol. Ther. 2016, 3, 187–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Symmons, D.P.; Jones, M.; Osborne, J.; Sills, J.; Southwood, T.R.; Woo, P. Pediatric rheumatology in the United Kingdom: Data from the British Pediatric Rheumatology Group National Diagnostic Register. J. Rheumatol. 1996, 23, 1975–1980. [Google Scholar] [PubMed]
- Müller, L.; Kellenberger, C.J.; Cannizzaro, E.; Ettlin, D.; Schraner, T.; Bolt, I.B.; Saurenmann, R.K. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: A pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology 2009, 48, 680–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ugolini, A.; Doldo, T.; Huanca Ghislanzoni, L.T.; Mapelli, A.; Giorgetti, R.; Sforza, C.; Fastuca, R.; Lorusso, P.; Lagravère, M.O.; Michelotti, A.; et al. Dentoskeletal outcomes of a rapid maxillary expander with differential opening in patients with bilateral cleft lip and palate: A prospective clinical trial. Am. J. Orthod. Dentofac. Orthop. 2017, 150, 564–574. [Google Scholar]
- von Bremen, J.; Ruf, S. Orthodontic and dentofacial orthopedic management of juvenile idiopathic arthritis: A systematic review of the literature. Orthod. Craniofacial Res. 2011, 14, 107–115. [Google Scholar] [CrossRef]
- Billiau, A.D.; Hu, Y.; Verdonck, A.; Carels, C.; Wouters, C. Temporomandibular Joint Arthritis in Juvenile Idiopathic Arthritis: Prevalence, Clinical and Radiological Signs, and Relation to Dentofacial Morphology. J. Rheumatol. 2007, 34, 1925–1933. [Google Scholar]
- de Carvalho, R.T.; Braga, F.S.F.F.; Brito, F.; Capelli Junior, J.; Figueredo, C.M.; Sztajnbok, F.R. Temporomandibular joint alterations and their orofacial complications in patients with juvenile idiopathic arthritis. Rev. Bras. Reumatol. 2012, 52, 907–911. [Google Scholar]
- Hsieh, Y.J.; Darvann, T.A.; Hermann, N.V.; Larsen, P.; Liao, Y.F.; Bjoern-Joergensen, J.; Kreiborg, S. Facial morphology in children and adolescents with juvenile idiopathic arthritis and moderate to severe temporomandibular joint involvement. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 182–191. [Google Scholar] [CrossRef]
- Farronato, M.; Cavagnetto, D.; Abate, A.; Cressoni, P.; Fama, A.; Maspero, C. Assessment of condylar volume and ramus height in JIA patients with unilateral and bilateral TMJ involvement: Retrospective case-control study. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef]
- Ronchezel, M.V.; Hilario, M.O.E.; Goldenberg, J.; Lederman, H.M.; Faltin, K.; De Azevedo, M.F.; Naspitz, C.K. Temporomandibular joint and mandibular growth alterations in patients with juvenile rheumatoid arthritis. J. Rheumatol. 1995, 22, 1956–1961. [Google Scholar] [PubMed]
- Sidiropoulou-Chatzigianni, S.; Papadopoulos, M.A.; Kolokithas, G. Dentoskeletal morphology in children with juvenile idiopathic arthritis compared with healthy children. J. Orthod. 2001, 28, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Quartier, P. Current treatments for juvenile idiopathic arthritis. Jt. Bone Spine 2010, 77, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Te Veldhuis, E.C.; Te Veldhuis, A.H.; Koudstaal, M.J. Treatment management of children with juvenile idiopathic arthritis with temporomandibular joint involvement: A systematic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 581–589. [Google Scholar] [CrossRef]
- Stoustrup, P.; Pedersen, T.K.; Nørholt, S.E.; Resnick, C.M.; Abramowicz, S. Interdisciplinary Management of Dentofacial Deformity in Juvenile Idiopathic Arthritis. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 117–134. [Google Scholar] [CrossRef]
- Stoustrup, P.; Twilt, M.; Spiegel, L.; Kristensen, K.D.; Koos, B.; Pedersen, T.K.; Küseler, A.; Cron, R.Q.; Abramowicz, S.; Verna, C.; et al. Clinical orofacial examination in juvenile idiopathic arthritis: International consensus-based recommendations for monitoring patients in clinical practice and research studies. J. Rheumatol. 2017, 44, 326–333. [Google Scholar] [CrossRef]
- Kjellberg, H. Juvenile chronic arthritis. Dentofacial morphology, growth, mandibular function and orthodontic treatment. Swed. Dent. J. Suppl. 1995, 109, 1–56. [Google Scholar]
- González, M.F.O.; Pedersen, T.K.; Dalstra, M.; Herlin, T.; Verna, C. 3D evaluation of mandibular skeletal changes in juvenile arthritis patients treated with a distraction splint: A retrospective follow-up. Angle Orthod. 2016, 86, 846–853. [Google Scholar] [CrossRef] [Green Version]
- Macedo de Menezes, L.; Deon Rizzatto, S.M.; Martinelli Santayana de Lima, E.; Baccarin Matje, P.R.; Picarelli, M.M. Juvenile idiopatic arthritis in orthodontics: Case report with a 6-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 384–396. [Google Scholar] [CrossRef]
- Malandris, M.; Mahoney, E.K. Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition. Int. J. Paediatr. Dent. 2004, 14, 155–166. [Google Scholar] [CrossRef]
- McNamara, J.A.; Brudon, W.L. Orthodontic and Orthopedic Treatment in the Mixed Dentition; Needham Press: Ann Arbor, MI, USA, 1993. [Google Scholar]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Sagittal and vertical effects of rapid maxillary expansion in Class I, II, and III occlusions. Angle Orthod. 2011, 81, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Cavagnetto, D.; Fama, A.; Giannini, L.; Galbiati, G.; Farronato, M. Hyrax versus transverse sagittal maxillary expander: An assessment of arch changes on dental casts. A retrospective study. Saudi Dent. J. 2019, 32, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Ciancaglini, R.; Gherlone, E.F.; Radaelli, G. Unilateral temporomandibular disorder and asymmetry of occlusal contacts. J. Prosthet. Dent. 2003, 89, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Ciancaglini, R.; Gherlone, E.F.; Redaelli, S.; Radaelli, G. The distribution of occlusal contacts in the intercuspal position and temporomandibular disorder. J. Oral Rehabil. 2002, 29, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yin, X. Occlusal risk factors associated with temporomandibular disorders in young adults with normal occlusions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Masi, M.; Lederman, H.M.; Yamashita, H.K.; de Arruda Aidar, L.A. Temporomandibular joint evaluation with magnetic resonance imaging in children with functional unilateral posterior crossbite, treated with rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 207–217. [Google Scholar] [CrossRef]
- Arat, F.E.; Arat, Z.M.; Tompson, B.; Tanju, S. Muscular and condylar response to rapid maxillary expansion. Part 3: Magnetic resonance assessment of condyle-disc relationship. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 830–836. [Google Scholar] [CrossRef]
- Leonardi, R.; Caltabiano, M.; Cavallini, C.; Sicurezza, E.; Barbato, E.; Spampinato, C.; Giordano, D. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion. Angle Orthod. 2012, 82, 1040–1046. [Google Scholar] [CrossRef] [Green Version]
- Baratieri, C.; Alves, M.; Bolognese, A.M.; Nojima, M.C.G.; Nojima, L.I. Changes in skeletal and dental relationship in Class II Division I malocclusion after rapid maxillary expansion: A prospective study. Dental Press J. Orthod. 2014, 19, 75–81. [Google Scholar] [CrossRef] [Green Version]
- Lima Filho, R.M.A.; Carlos, A.; Ruellas, O. Mandibular Behavior with Slow and Rapid Maxillary Expansion in Skeletal Class II Patients A Long-Term Study. Angle Orthod. 2007, 77, 625–631. [Google Scholar] [CrossRef]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Espansione rapida del palato: Conseguenze sul setto nasale—Minerva Stomatologica 2012 April;61:125-34—Minerva Medica—Riviste. Minerva Stomatol. 2012, 61, 125–134. [Google Scholar]
- Lanteri, V.; Cossellu, G.; Gianolio, A.; Beretta, M.; Lanteri, C.; Cherchi, C.; Farronato, G. Comparison between RME, SME and Leaf Expander in growing patients: A retrospective postero-anterior cephalometric study. Eur. J. Paediatr. Dent. 2018, 19, 199. [Google Scholar]
- Evangelista, K.; Ferrari-Piloni, C.; Barros, L.A.N.; Avelino, M.A.G.; Helena Soares Cevidanes, L.; de Oliveira Ruellas, A.C.; Valladares-Neto, J.; Silva, M.A.G. Three-dimensional assessment of craniofacial asymmetry in children with transverse maxillary deficiency after rapid maxillary expansion: A prospective study. Orthod. Craniofacial Res. 2020. [Google Scholar] [CrossRef]
- Cahill, A.M.; Baskin, K.M.; Kaye, R.D.; Arabshahi, B.; Cron, R.Q.; Dewitt, E.M.; Bilaniuk, L.; Towbin, R.B. CT-guided percutaneous steroid injection for management of inflammatory arthropathy of the temporomandibular joint in children. Am. J. Roentgenol. 2007, 188, 182–186. [Google Scholar] [CrossRef] [Green Version]
- Schiffman, E.L.; Ohrbach, R.; Truelove, E.L.; Tai, F.; Anderson, G.C.; Pan, W.; Gonzalez, Y.M.; John, M.T.; Sommers, E.; List, T.; et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: Methods used to establish and validate revised Axis I diagnostic algorithms. J. Orofac. Pain 2010, 24, 63–78. [Google Scholar]
- Petty, R.E.; Southwood, T.R.; Manners, P.; Baum, J.; Glass, D.N.; Goldenberg, J.; He, X.; Maldonado-Cocco, J.; Orozco-Alcala, J.; Prieur, A.M.; et al. International League of Associations for Rheumatology Classification of Juvenile Idiopathic Arthritis: Second Revision, Edmonton, 2001. J. Rheumatol. 2004, 31, 390. [Google Scholar]
- Rongo, R.; Alstergren, P.; Ammendola, L.; Bucci, R.; Alessio, M.; D’Antò, V.; Michelotti, A. Temporomandibular joint damage in juvenile idiopathic arthritis: Diagnostic validity of diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2019, 46, 450–459. [Google Scholar] [CrossRef]
- Caprioglio, A.; Bergamini, C.; Franchi, L.; Vercellini, N.; Zecca, P.A.; Nucera, R.; Fastuca, R. Prediction of Class II improvement after rapid maxillary expansion in early mixed dentition. Prog. Orthod. 2017, 18, 9. [Google Scholar] [CrossRef] [Green Version]
- Farronato, G.; Carletti, V.; Maspero, C.; Farronato, D.; Giannini, L.; Bellintani, C. Craniofacial growth in children affected by juvenile idiopathic arthritis involving the temporomandibular joint: Functional therapy management. J. Clin. Pediatr. Dent. 2009, 33, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Comparison of the dental and skeletal effects of two different rapid palatal expansion appliances for the correction of the maxillary asymmetric transverse discrepancies. Minerva Stomatol. 2012, 61, 45–55. [Google Scholar]
- Athanasiou, A.E. Orthodontic Cephalometry; Mosby-Wolfe: London, UK, 1995. [Google Scholar]
- Resnick, C.M.; Frid, P.; Norholt, S.E.; Stoustrup, P.; Peacock, Z.S.; Kaban, L.B.; Pedersen, T.K.; Abramowicz, S. An Algorithm for Management of Dentofacial Deformity Resulting From Juvenile Idiopathic Arthritis: Results of a Multinational Consensus Conference. J. Oral Maxillofac. Surg. 2019, 77, 1152.e1–1152.e33. [Google Scholar] [CrossRef] [Green Version]
- Thilander, B.; Wahlund, S.; Lennartsson, B. The effect of early interceptive treatment in children with posterior cross-bite. Eur. J. Orthod. 1984, 6, 25–34. [Google Scholar] [CrossRef]
- Brunetto, D.P.; Sant’Anna, E.F.; Machado, A.W.; Moon, W. Non-surgical treatment of transverse deficiency in adults using microimplant-assisted rapid palatal expansion (MARPE). Dental Press J. Orthod. 2017, 22, 110–125. [Google Scholar] [CrossRef] [Green Version]
- Alyessary, A.S.; Othman, S.A.; Yap, A.U.J.; Radzi, Z.; Rahman, M.T. Effects of non-surgical rapid maxillary expansion on nasal structures and breathing: A systematic review. Int. Orthod. 2019, 17, 12–19. [Google Scholar] [CrossRef]
- Galbiati, G.; Maspero, C.; Giannini, L.; Tagliatesta, C.; Farronato, G. Functional evaluation in young patients undergoing orthopedical interceptive treatment. Minerva Stomatol. 2016. [Google Scholar]
- McNamara, J.A.; Lione, R.; Franchi, L.; Angelieri, F.; Cevidanes, L.H.S.; Darendeliler, M.A.; Cozza, P. The role of rapid maxillary expansion in the promotion of oral and general health. Prog. Orthod. 2015, 16, 33. [Google Scholar] [CrossRef] [Green Version]
- Maspero, C.; Fama, A.; Cavagnetto, D.; Abate, A.; Farronato, M. Treatment of dental dilacerations. J. Biol. Regul. Homeost. Agents 2019, 33, 1623–1628. [Google Scholar]
- Maspero, C.; Abate, A.; Cavagnetto, D.; Fama, A.; Stabilini, A.; Farronato, G.; Farronato, M. Operculectomy and spontaneous eruption of impacted second molars: A retrospective study. J. Biol. Regul. Homeost. Agents 2019, 33, 1909. [Google Scholar]
- Fama, A.; Cavagnetto, D.; Abate, A.; Mainardi, E.; De Filippis, A.; Esposito, L. Treatment of dental dilacerations. Narrative review. Dent. Cadmos 2020, in press. [Google Scholar]
- Sharma, D.S.; Srivastava, S.; Tandon, S. Preventive orthodontic approach for functional mandibular shift in early mixed dentition: A case report. J. Oral Biol. Craniofacial Res. 2019, 9, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Kjellberg, H.; Kiliaridis, S.; Thilander, B. Dentofacial growth in orthodontically treated and untreated children with juvenile chronic arthritis (JCA). A comparison with angle Class II division 1 subjects. Eur. J. Orthod. 1995, 17, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Portelli, M.; Matarese, G.; Militi, A.; Lo Giudice, G.; Nucera, R.; Lucchese, A. Temporomandibular joint involvement in a cohort of patients with Juvenile Idiopatic Arthritis and evaluation of the effect induced by functional orthodontic appliance: Clinical and radiographic investigation. Eur. J. Paediatr. Dent. 2014, 15, 63–66. [Google Scholar]
- Maspero, C.; Abate, A.; Bellincioni, F.; Cavagnetto, D.; Lanteri, V.; Costa, A.; Farronato, M. Comparison of a tridimensional cephalometric analysis performed on 3T-MRI compared with CBCT: A pilot study in adults. Prog. Orthod. 2019, 20, 40. [Google Scholar] [CrossRef]
- Maspero, C.; Farronato, M.; Bellincioni, F.; Annibale, A.; Machetti, J.; Abate, A.; Cavagnetto, D. Three-dimensional evaluation of maxillary sinus changes in growing subjects: A retrospective cross-sectional study. Materials 2020, 13, 1007. [Google Scholar] [CrossRef] [Green Version]
- Farronato, M.; Maspero, C.; Lanteri, V.; Fama, A.; Ferrati, F.; Pettenuzzo, A.; Farronato, D. Current state of the art in the use of augmented reality in dentistry: A systematic review of the literature. BMC Oral Health 2019, 19, 135. [Google Scholar] [CrossRef] [Green Version]
- Wendling, L.K.; McNamara, J.A.; Franchi, L.; Baccetti, T. A prospective study of the short-term treatment effects of the acrylic-splint rapid maxillary expander combined with the lower Schwarz appliance. Angle Orthod. 2005, 75, 7–14. [Google Scholar]
- Isola, G.; Perillo, L.; Migliorati, M.; Matarese, M.; Dalessandri, D.; Grassia, V.; Alibrandi, A.; Matarese, G. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur. J. Orthod. 2019, 41, 117–124. [Google Scholar] [CrossRef]
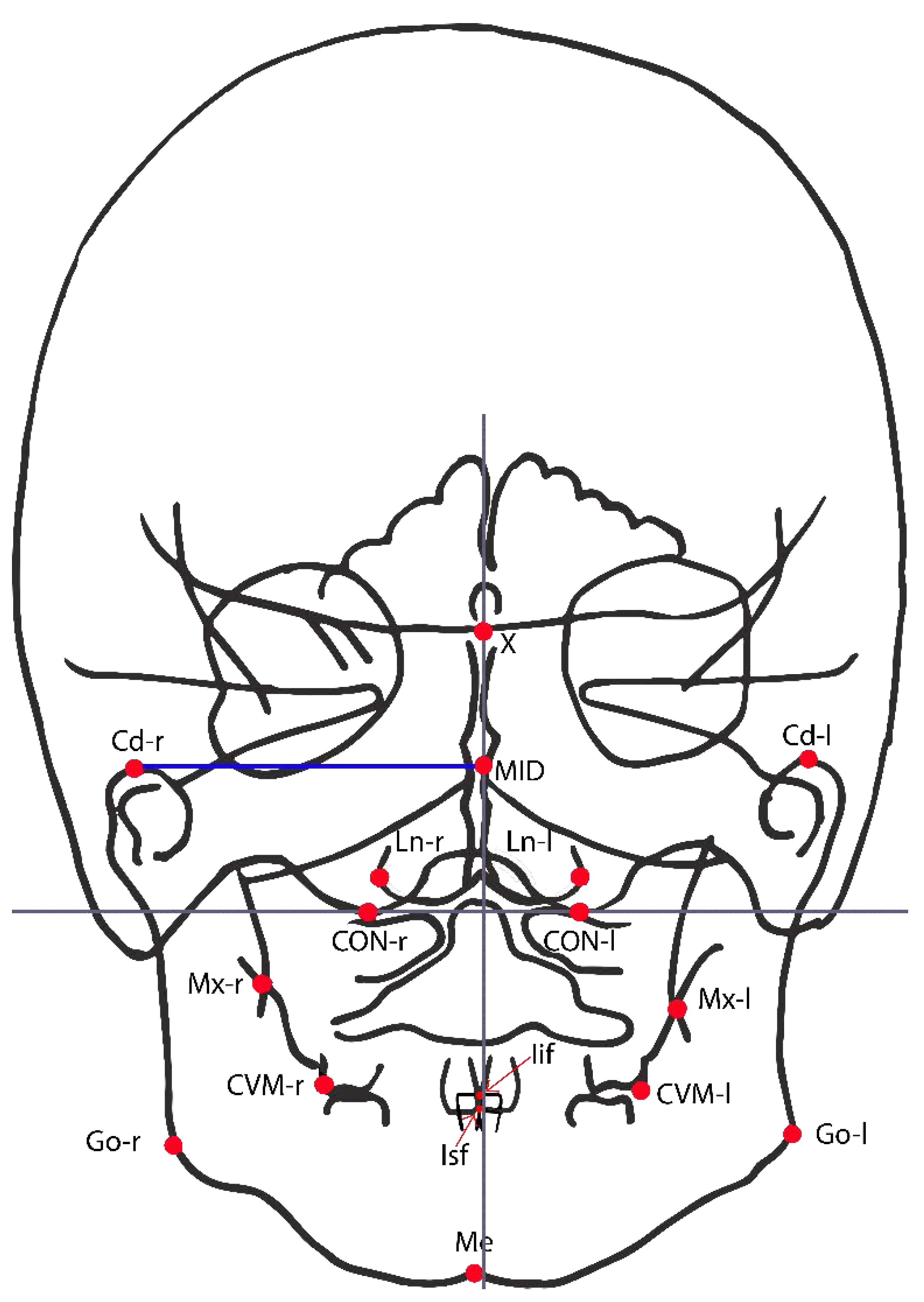
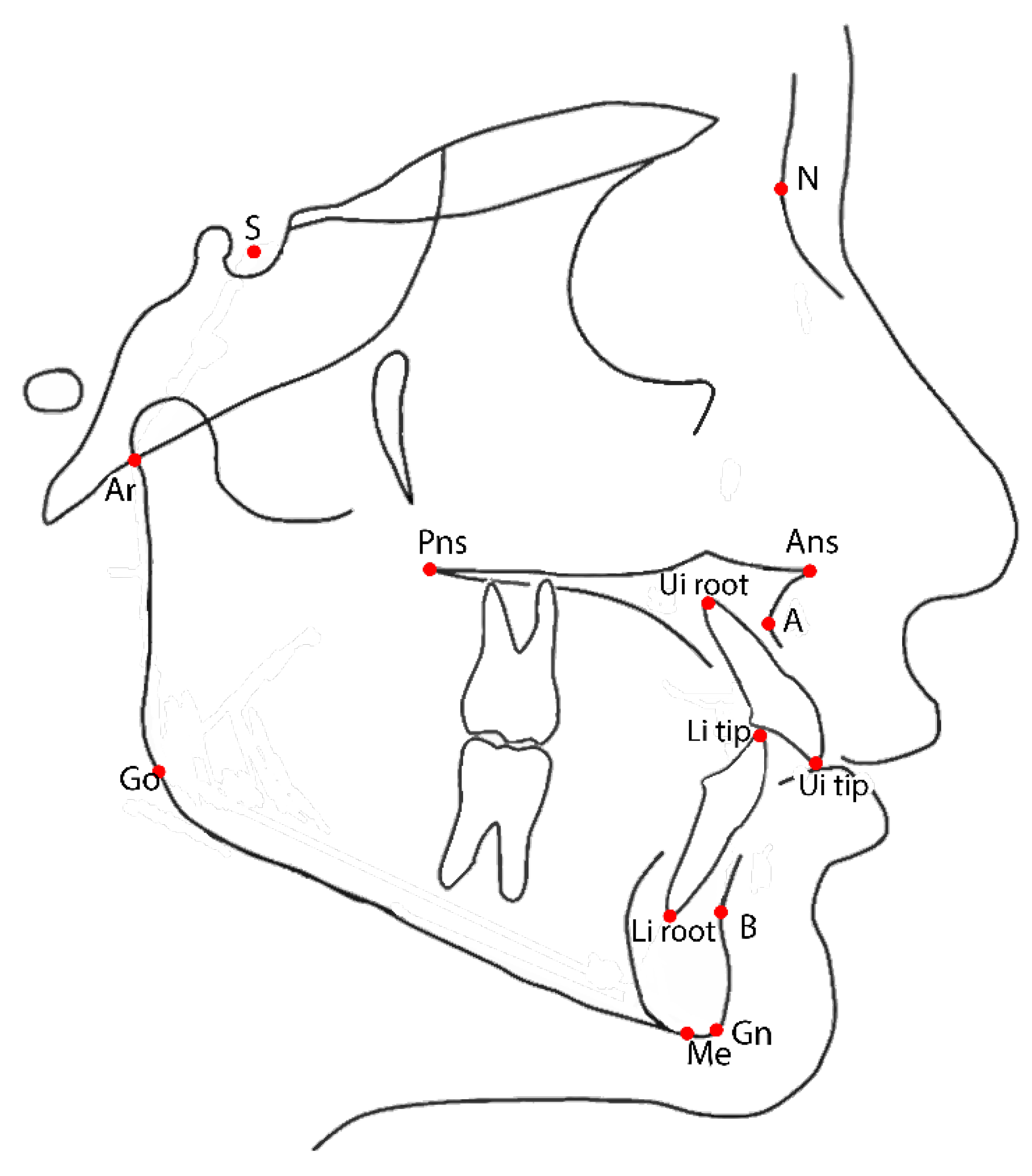
| Postero-Anterio Cephalogram | Lateral Cephalogram | ||
|---|---|---|---|
| Mx r/l | Maxillary transverse dimension | SNA | Angle between lines S-N and N-A |
| CVM + r/l | First permanent molar transvers dimension. | SNB | Angle between lines S-N and N-B |
| Nl r/l | Maximal horizontal diameter of the nasal cavity | ANB | Angle between lines A-N and N-B |
| CdNA-MID | Distance of the non-affected condyle to the axis of symmetry (in control patients it is by convention the distance from the more distant one to the axis of symmetry and the axis of symmetry) | SN-GoGn | Angle between lines S-N and Go-Gn |
| Cd A-MID | Distance of the affected condyle to the axis of symmetry (in control patients it is by convention the distance from the closer one to the axis of symmetry and the axis of symmetry) | AnsPns-GoGn | Angle between lines Ans-Pns and Go-Gn |
| ΔCd NA/A-MID | Linear difference between the distance of the non-affected and affected condyle to the axis of symmetry | SN-AnsPns | Angle between lines S-N and Ans-Pns |
| Go NA-MID | Distance of the non-affected gonion to the axis of symmetry (in control patients it is by convention the distance from the more distant one to the axis of symmetry and the axis of symmetry) | NSAr | Angle between N-S and S-Ar (“Articular angle”) |
| Go A-MID | Distance of the non-affected gonion to the axis of symmetry (in control patients it is by convention the distance from the closer one to the axis of symmetry and the axis of symmetry) | SArGo | Angle between S-Ar and Ar-Go (“Articular angle”) |
| ΔGo NA/A-MID | Linear difference between the distance of the non-affected and affected gonion to the axis of symmetry | ArGoGn | Angle between lines Ar-Go and Go-Me (“Total gonial angle”) |
| Me-MID | Distance of the point menton to the axis of symmetry | NGoGn | Angle between lines N-Go and Go-Gn (“Inferior gonial angle”) |
| Iif-MID | Distance of the point incision inferior frontale to the axis of symmetry | ArGoN | Angle between lines Ar-Go and Go-N (“Superior gonial angle”) |
| Isf-MID | Distance of the point incision superior frontale to the axis of symmetry | Jarabak’ssum | Sum of total, superior and inferior gonial angle |
| U1-SN | Angle between line through long axis of upper central incisor and S-N line | ||
| U1-AnsPns | Angle between line through long axis of upper central incisor and Ans-Pns line | ||
| IMPA | Angle between line through long axis of upper central incisor and Go-Gn line | ||
| U1-L1 | Angle between lines through long axis of upper and lower central incisors | ||
| Measurements | T0 (n = 25) | T1 (n = 25) | ΔT1−T0 | p Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Postero-anterior cephalogram | ||||||
| Mx r/l | 59.24 | 3.03 | 62.31 | 2.55 | 3.07 | <0.01 * |
| Cvm+r/l | 56.31 | 2.73 | 62.40 | 2.88 | 6.08 | <0.01 * |
| NLr-l | 26.79 | 3.41 | 29.71 | 3.22 | 2.92 | <0.01 * |
| Cd NA-MID | 45.21 | 2.25 | 46.22 | 2.71 | 1.12 | NS |
| Cd A-MID | 42.81 | 2.17 | 44.71 | 2.83 | 1.81 | <0.01 * |
| ΔCd NA/A-MID | 2.41 | 1.79 | 1.72 | 1.37 | −0.69 | 0.039 * |
| Go NA-MID | 41.92 | 3.26 | 43.15 | 2.56 | 1.23 | 0.043 * |
| Go A-MID | 39.27 | 3.38 | 41.68 | 2.79 | 2.41 | <0.001 * |
| ΔGo NA/A-MID | 2.65 | 1.34 | 1.47 | 1.18 | −1.18 | 0.015 * |
| Me-MID | 2.97 | 1.79 | 1.93 | 1.80 | −1.04 | 0.021 * |
| Iif-MID | 2.23 | 0.85 | 1.13 | 0.71 | −1.1 | <0.001 * |
| Isf-MID | 1.23 | 0.81 | 0.95 | 0.6 | −0.28 | NS |
| Lateral cephalogram | ||||||
| SNA | 80.08 | 3.74 | 79.7 | 3.25 | −0.38 | NS |
| SNB | 75.14 | 3.72 | 76.12 | 3.35 | 0.98 | NS |
| ANB | 4.93 | 1.79 | 3.62 | 1.95 | −1.36 | 0.035 * |
| SN-GoGn | 35.27 | 4.06 | 35.93 | 4.31 | 0.66 | NS |
| AnsPns-GoGn | 26.83 | 4.77 | 27.18 | 5.04 | 0.35 | NS |
| SN-AnsPns | 10.45 | 3.48 | 10.55 | 2.79 | 0.27 | NS |
| NSAr | 123.99 | 7.78 | 125.04 | 7.14 | 1.05 | NS |
| SArGo | 146.14 | 7.15 | 145.5 | 6.29 | −0.62 | NS |
| ArGoGn | 130.45 | 4.18 | 130.2 | 3.98 | −0.45 | NS |
| NGoGn | 76.85 | 5.93 | 77.26 | 3.39 | 0.42 | NS |
| ArGoN | 53.62 | 3.89 | 52.84 | 3.80 | −0.85 | NS |
| Jarabak’s sum | 400.08 | 4.37 | 400.45 | 4.69 | 0.43 | NS |
| U1-SN | 103.45 | 5.83 | 104.5 | 10.03 | 0.95 | NS |
| U1-AnsPns | 115.33 | 5.95 | 117.24 | 9.29 | 1.23 | NS |
| IMPA | 87.03 | 5.97 | 87.7 | 5.09 | 0.76 | NS |
| U1-L1 | 129.7 | 9.25 | 128.1 | 10.96 | 1.53 | NS |
| Measurements | T0 (n = 25) | T1 (n = 25) | ΔT1−T0 | p Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Postero-anterior cephalogram | ||||||
| Mx r/l | 58.53 | 2.92 | 61.47 | 2.07 | 2.94 | <0.01 * |
| Cvm+r/l | 56.31 | 0.68 | 61.98 | 0.78 | 5.67 | <0.01 * |
| NLr-l | 27.74 | 2.91 | 31.03 | 2.88 | 3.29 | <0.01 * |
| Cd NA-MID | 46.75 | 1.88 | 48.33 | 2.19 | 1.58 | NS |
| Cd A-MID | 47.56 | 2.07 | 49.02 | 2.36 | 1.46 | NS |
| ΔCd NA/A-MID | 0.81 | 1.09 | 0.69 | 0.97 | −0.12 | NS |
| Go r-MID | 44.22 | 1.95 | 45.55 | 1.84 | 1.28 | NS |
| Go l-MID | 43.43 | 2.68 | 44.95 | 1.93 | 1.52 | NS |
| ΔGo r/l-MID | 0.77 | 0.84 | 0.55 | 1.18 | −0.22 | NS |
| Me-MID | 0.72 | 1.37 | 0.33 | 1.51 | −0.39 | NS |
| Iif-MID | 1.05 | 1.85 | 0.26 | 1.74 | −0.75 | 0.042 * |
| Isf-MID | 1.03 | 0.81 | 0.73 | 0.6 | −0.32 | NS |
| Lateral cephalogram | ||||||
| SNA | 83.52 | 4.99 | 83.26 | 5.12 | −0.26 | NS |
| SNB | 78.48 | 6.47 | 79.03 | 6.15 | 0.55 | NS |
| ANB | 6.24 | 2.95 | 5.22 | 2.37 | −1.02 | 0.047 * |
| SN-GoGn | 34.96 | 6.07 | 34.61 | 5.98 | −0.34 | NS |
| AnsPns- GoGn | 27.74 | 4.74 | 27.83 | 5.87 | 0.09 | NS |
| SN- AnsPns | 7.61 | 2.84 | 7.04 | 2.99 | −0.56 | NS |
| NSAr | 124.00 | 5.66 | 124.13 | 5.36 | 0.13 | NS |
| SArGo | 139.91 | 6.37 | 141.09 | 6.15 | 1.17 | NS |
| ArGoGn | 132.61 | 5.95 | 131.43 | 4.81 | −1.18 | NS |
| NGoGn | 76.91 | 4.91 | 76.04 | 4.43 | −0.87 | NS |
| ArGoN | 55.78 | 4.01 | 55.39 | 4.49 | −1.92 | NS |
| Jarabak’s sum | 396.52 | 6.78 | 396.61 | 5.84 | 0.09 | NS |
| U1-SN | 103.61 | 9.07 | 105.74 | 8.34 | 2.13 | NS |
| U1-AnsPns | 111.00 | 10.42 | 112.39 | 8.73 | 1.39 | NS |
| IMPA | 89.57 | 6.07 | 90.26 | 7.81 | 0.70 | NS |
| U1-L1 | 129.39 | 9.35 | 127.78 | 8.64 | −1.61 | NS |
| Measurements | JIA ΔT1−T0 (n = 25) | ControlΔT1−T0 (n = 25) | ΔJIA-Control (mean) | p Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Postero-anterior cephalogram | ||||||
| Mx r/l | 3.07 | 2.19 | 2.94 | 1.84 | 0.13 | NS |
| Cvm+r/l | 6.08 | 3.77 | 5.67 | 2.86 | 0.41 | NS |
| NLr-l | 2.92 | 2.32 | 3.29 | 2.21 | 0.37 | NS |
| Cd NA-MID | 1.12 | 2.33 | 1.58 A | 1.87 | -0.46 | NS |
| Cd A-MID | 1.81 | 2.15 | 1.46 B | 1.98 | 0.35 | NS |
| ΔCd NA/A-MID | −0.69 | 1.72 | −0.12 A,B | 0.66 | -0.57 | 0.034 * |
| Go NA-MID | 1.23 | 2.12 | 1.28 A | 1.25 | -0.05 | NS |
| Go A-MID | 2.41 | 1.52 | 1.53 B | 1.16 | 0.89 | 0.026 * |
| ΔGo NA/A-MID | −1.18 | 1.49 | −0.22 A,B | 1.67 | -0.96 | 0.037 * |
| Me-MID | −1.04 | 0.93 | −0.39 | 0.85 | 0.65 | 0.013 * |
| Iif-MID | −1.1 | 0.66 | −0.75 | 0.43 | -0.35 | NS |
| Isf-MID | −0.28 | 0.59 | −0.32 | 0.69 | 0.04 | NS |
| Lateral cephalogram | ||||||
| SNA | −0.38 | 3.73 | −0.26 | 5.03 | 0.12 | NS |
| SNB | 0.98 | 2.95 | 0.35 | 6.98 | −0.63 | NS |
| ANB | −1.36 | 1.73 | −1.02 | 2.50 | 0.34 | NS |
| SN-GoGn | 0.66 | 1.77 | −0.34 | 2.67 | −1 | NS |
| AnsPns-GoGn | 0.35 | 4.48 | 0.09 | 3.22 | −0.36 | NS |
| SN-AnsPns | 0.27 | 4.82 | −0.56 | 2.95 | −0.83 | NS |
| NSAr | 1.05 | 3.03 | 0.13 | 4.98 | −0.92 | NS |
| SArGo | −0.62 | 8.52 | 1.17 | 5.52 | 1.79 | NS |
| ArGoGn | −0.45 | 4.71 | −1.18 | 3.99 | −0.73 | NS |
| NGoGn | 0.42 | 3.84 | −0.87 | 2.60 | 1.29 | NS |
| ArGoN | −0.85 | 3.62 | −1.92 | 3.54 | −1.07 | NS |
| Jarabak’s sum | 0.43 | 1.68 | 0.09 | 3.42 | −0.34 | NS |
| U1-SN | 0.95 | 7.43 | 2.13 | 9.79 | 1.18 | NS |
| U1-AnsPns | 1.23 | 7.26 | 1.39 | 10.31 | 0.16 | NS |
| IMPA | 0.76 | 5.24 | 0.70 | 5.73 | −0.06 | NS |
| U1-L1 | 1.53 | 6.51 | −1.61 | 8.91 | −3.14 | NS |
| Measurements | Non-Affected | Affected | Δ Non Affected–Affected | p Value | ||
| Mean | SD | Mean | SD | |||
| JIA patients | ||||||
| Cd-MID T0 | 45.21 | 2.25 | 42.81 | 2.17 | 2.41 | <0.001 * |
| Cd-MID T1 | 46.22 | 2.71 | 44.71 | 2.83 | 1.51 | NS |
| Go-MID T0 | 41.92 | 3.26 | 39.27 | 3.38 | 2.65 | 0.007 * |
| Go-MID T1 | 43.15 | 2.56 | 41.68 | 2.79 | 1.46 | NS |
| Measurements | Right | Left | Δ Non affected- Affected | pvalue | ||
| Mean | SD | Mean | SD | |||
| Control group | ||||||
| Cd-MID T0 | 46.75 | 1.88 | 47.56 | 2.07 | −0.81 | NS |
| Cd-MID T1 | 48.33 | 2.19 | 49.02 | 2.36 | −0.69 | NS |
| Go-MID T0 | 44.22 | 1.95 | 43.43 | 2.68 | 0.79 | NS |
| Go-MID T1 | 45.55 | 1.84 | 44.95 | 1.93 | 0.61 | NS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maspero, C.; Cavagnetto, D.; Abate, A.; Cressoni, P.; Farronato, M. Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms. J. Clin. Med. 2020, 9, 1159. https://doi.org/10.3390/jcm9041159
Maspero C, Cavagnetto D, Abate A, Cressoni P, Farronato M. Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms. Journal of Clinical Medicine. 2020; 9(4):1159. https://doi.org/10.3390/jcm9041159
Chicago/Turabian StyleMaspero, Cinzia, Davide Cavagnetto, Andrea Abate, Paolo Cressoni, and Marco Farronato. 2020. "Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms" Journal of Clinical Medicine 9, no. 4: 1159. https://doi.org/10.3390/jcm9041159
APA StyleMaspero, C., Cavagnetto, D., Abate, A., Cressoni, P., & Farronato, M. (2020). Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms. Journal of Clinical Medicine, 9(4), 1159. https://doi.org/10.3390/jcm9041159









