Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort
Abstract
1. Introduction
2. Experimental Section
2.1. Method
2.2. Design
2.3. Participants
2.4. Measures
2.4.1. Blood Alcohol Concentration (BAC)
2.4.2. Consensus Sleep Diary (CSD)
2.4.3. Alcohol Consumption Questions
2.4.4. Estimated BAC (eBAC)
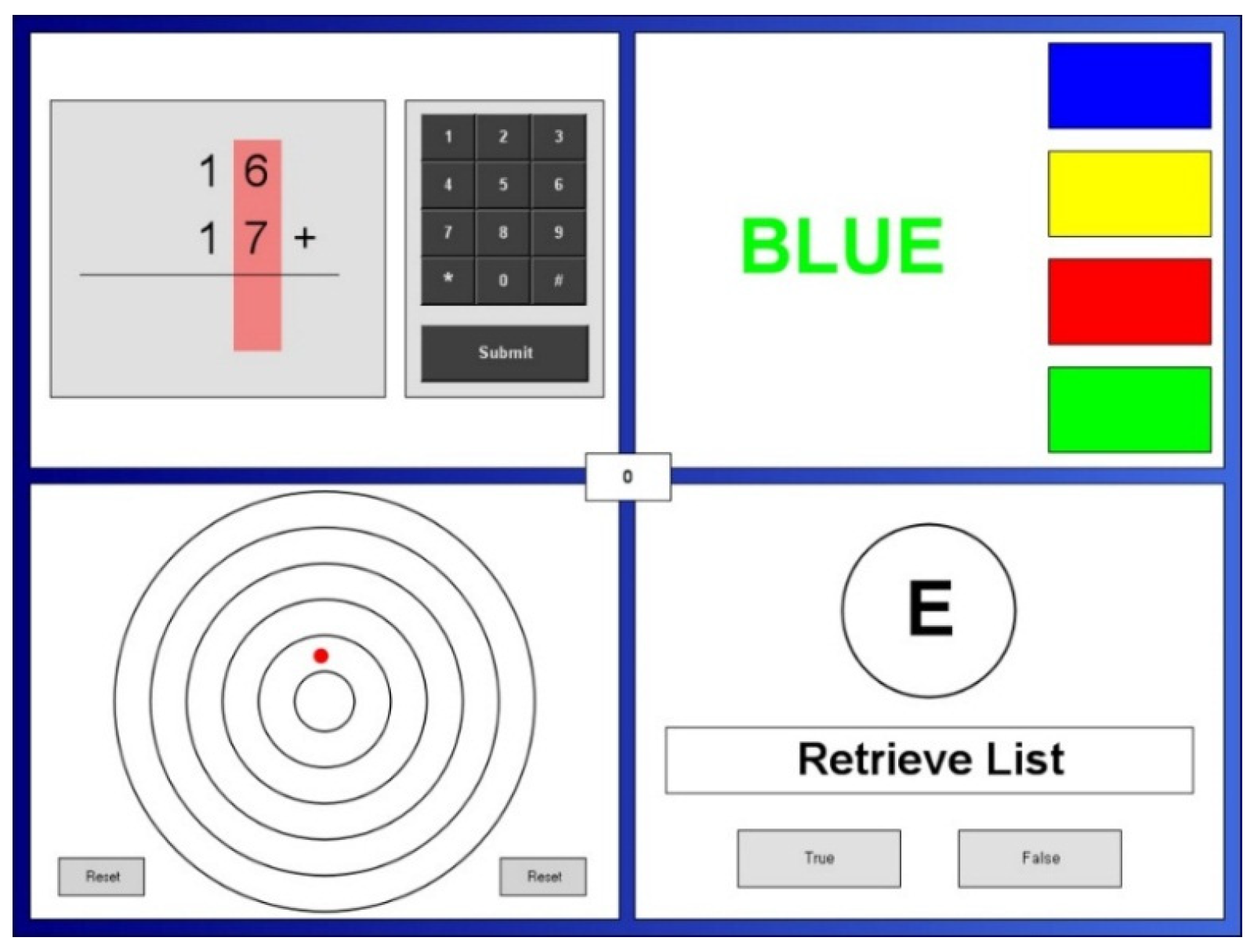
2.4.5. Multitasking Framework
2.4.6. NASA-Task Load Index (NASA-TLX)
2.4.7. Single Item Hangover Symptom Severity Score
2.4.8. Alcohol Hangover Severity Scale (AHSS)
2.4.9. Stress and Fatigue Visual Analogue Mood Scale (Stress and Fatigue VAMS)
2.4.10. Spielberger State-Trait Anxiety Inventory, State Portion (STAI-S)
2.4.11. Bond-Lader Visual Analogue Mood Scales (Bond-Lader VAMS)
2.5. Procedure
2.6. Statistical Analysis
3. Results
3.1. Consensus Sleep Diary (CSD)
3.2. eBAC
3.3. Hangover Symptom Severity
3.4. Multitasking Performance
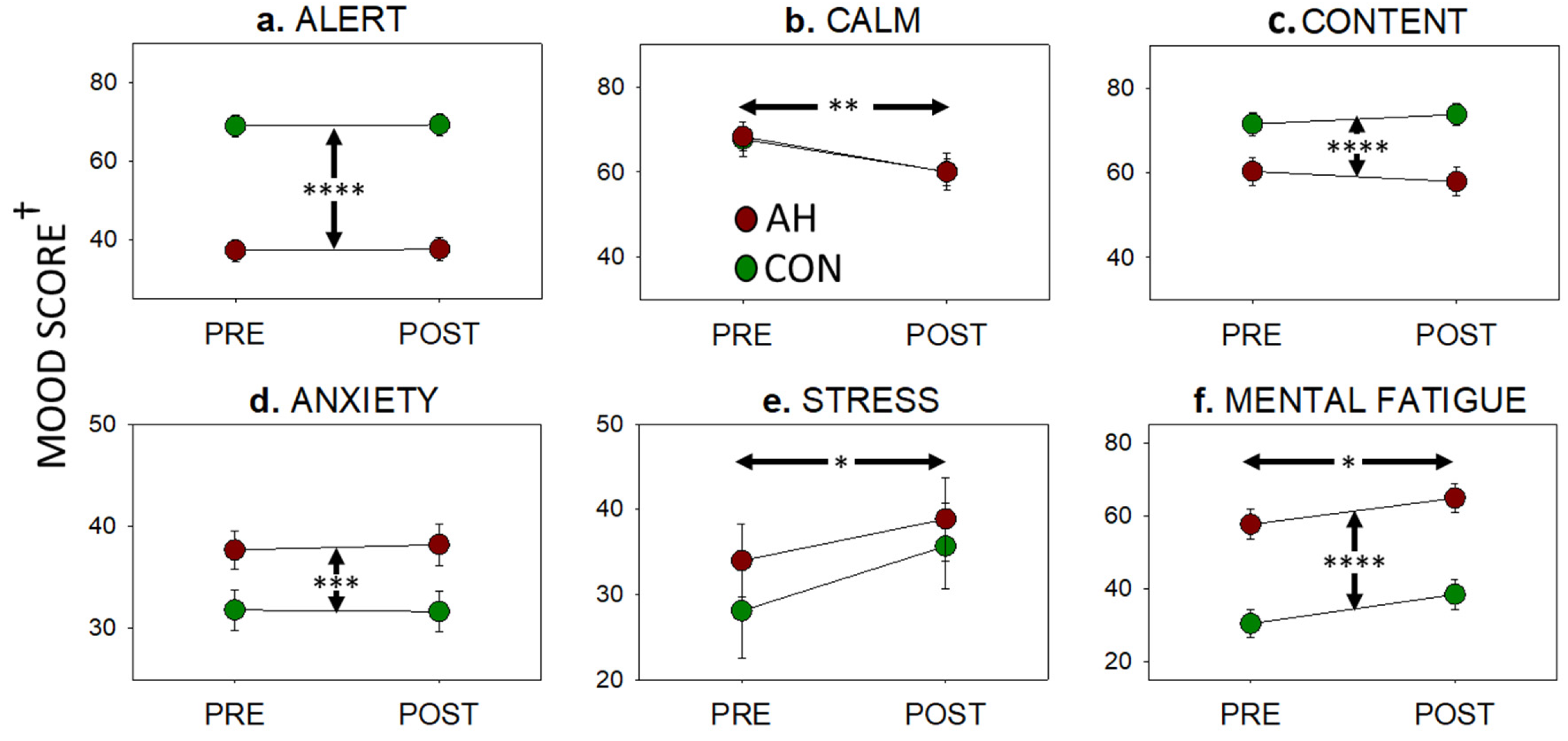
3.5. Mood
3.6. NASA-TLX
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Verster, J.C.; Stephens, R.; Penning, R.; Rohsenow, D.; McGeary, J.; Levy, D.; McKinney, A.; Finnigan, F.; Piasecki, T.M.; Adan, A. The alcohol hangover research group consensus statement on best practice in alcohol hangover research. Curr. Drug Abuse Rev. 2010, 3, 116. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C.; van de Loo, A.J.; Adams, S.; Stock, A.K.; Benson, S.; Scholey, A.; Alford, C.; Bruce, G. Advantages and Limitations of Naturalistic Study Designs and their Implementation in Alcohol Hangover Research. J. Clin. Med. 2019, 8, 2160. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C.; Scholey, A.; van de Loo, A.J.; Benson, S.; Stock, A.K. Updating the Definition of the Alcohol Hangover. J. Clin. Med. 2020, 9, 823. [Google Scholar] [CrossRef] [PubMed]
- Rohsenow, D.J.; Howland, J.; Minsky, S.J.; Greece, J.; Almeida, A.; Roehrs, T.A. The Acute Hangover Scale: A new measure of immediate hangover symptoms. Addict. Behav. 2007, 32, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.C. The alcohol hangover–A puzzling phenomenon. Alcohol Alcohol. 2008, 43, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Mc Kinney, A.; Coyle, K. Alcohol hangover effects on measures of affect the morning after a normal night’s drinking. Alcohol Alcohol. 2006, 41, 54–60. [Google Scholar] [CrossRef]
- Prat, G.; Adan, A.; Sanchez-Turet, M. Alcohol hangover: A critical review of explanatory factors. Hum. Psychopharmacol. 2009, 24, 259–267. [Google Scholar] [CrossRef]
- Wiese, J.G.; Shlipak, M.G.; Browner, W.S. The alcohol hangover. Ann. Intern Med. 2000, 132, 897–902. [Google Scholar] [CrossRef]
- Takahashi, M.; Li, W.; Koike, K.; Sadamoto, K. Clinical effectiveness of KSS formula, a traditional folk remedy for alcohol hangover symptoms. J. Nat. Med. 2010, 64, 487–491. [Google Scholar] [CrossRef]
- Verster, J.C.; van Duin, D.; Volkerts, E.R.; Schreuder, A.H.; Verbaten, M.N. Alcohol hangover effects on memory functioning and vigilance performance after an evening of binge drinking. Neuropsychopharmacology 2003, 28, 740–746. [Google Scholar] [CrossRef]
- Finnigan, F.; Schulze, D.; Smallwood, J.; Helander, A. The effects of self-administered alcohol-induced ‘hangover’in a naturalistic setting on psychomotor and cognitive performance and subjective state. Addiction 2005, 100, 1680–1689. [Google Scholar] [CrossRef]
- Slutske, W.S.; Piasecki, T.M.; Hunt-Carter, E.E. Development and initial validation of the Hangover Symptoms Scale: Prevalence and correlates of hangover symptoms in college students. Alcohol. Clin. Exp. Res. 2003, 27, 1442–1450. [Google Scholar] [CrossRef]
- Kim, D.-J.; Kim, W.; Yoon, S.-J.; Choi, B.-M.; Kim, J.-S.; Go, H.J.; Kim, Y.-K.; Jeong, J. Effects of alcohol hangover on cytokine production in healthy subjects. Alcohol 2003, 31, 167–170. [Google Scholar] [CrossRef]
- Anderson, S.; Dawson, J. Neuropsychological correlates of alcoholic hangover. S. Afr. J. Sci. 1999, 95, 145. [Google Scholar]
- Roehrs, T.; Yoon, J.; Roth, T. Nocturnal and next-day effects of ethanol and basal level of sleepiness. Hum. Psychopharmacol. Clin. Exp. 1991, 6, 307–311. [Google Scholar] [CrossRef]
- Howland, J.; Rohsenow, D.J.; Littlefield, C.A.; Almeida, A.; Heeren, T.; Winter, M.; Bliss, C.A.; Hunt, S.; Hermos, J. The effects of binge drinking on college students’ next-day academic test-taking performance and mood state. Addiction 2010, 105, 655–665. [Google Scholar] [CrossRef] [PubMed]
- McKinney, A.; Coyle, K.; Penning, R.; Verster, J.C. Next day effects of naturalistic alcohol consumption on tasks of attention. Hum. Psychopharmacol. Clin. Exp. 2012, 27, 587–594. [Google Scholar] [CrossRef]
- Grange, J.A.; Stephens, R.; Jones, K.; Owen, L. The effect of alcohol hangover on choice response time. J. Psychopharmacol. 2016, 30, 654–661. [Google Scholar] [CrossRef]
- McKinney, A.; Coyle, K. Next-day effects of alcohol and an additional stressor on memory and psychomotor performance. J. Stud. Alcohol Drugs 2007, 68, 446–454. [Google Scholar] [CrossRef]
- McKinney, A.; Coyle, K. Next day effects of a normal night’s drinking on memory and psychomotor performance. Alcohol Alcohol. 2004, 39, 509–513. [Google Scholar] [CrossRef]
- Gunn, C.; Mackus, M.; Griffin, C.; Munafò, M.R.; Adams, S. A systematic review of the next-day effects of heavy alcohol consumption on cognitive performance. Addiction 2018, 113, 2182–2193. [Google Scholar] [CrossRef]
- Langner, R.; Willmes, K.; Chatterjee, A.; Eickhoff, S.B.; Sturm, W. Energetic effects of stimulus intensity on prolonged simple reaction-time performance. Psychol. Res. 2010, 74, 499–512. [Google Scholar] [CrossRef]
- Collins, W.E.; Chiles, W.D. Laboratory performance during acute alcohol intoxication and hangover. Hum. Factors J. Hum. Factors Ergon. Soc. 1980, 22, 445–462. [Google Scholar] [CrossRef]
- Collins, W.E. Performance Effects of Alcohol Intoxication and Hangover at Ground Level and at Simulated Altitude; Civil Aerospace Medical Institute: Oklahoma City, OK, USA, October 1979. [Google Scholar]
- Verster, J.C.; Bervoets, A.C.; de Klerk, S.; Vreman, R.A.; Olivier, B.; Roth, T.; Brookhuis, K.A. Effects of alcohol hangover on simulated highway driving performance. Psychopharmacology 2014, 231, 2999–3008. [Google Scholar] [CrossRef]
- Törnros, J.; Laurell, H. Acute and Hang-over Effects of Alcohol on Simulated Driving Performance; VTI Särtryck 169; Statens Väg-och Trafikinstitut: Linköping, Sweden, 1991. [Google Scholar]
- Yesavage, J.A.; Leirer, V.O. Hangover effects on aircraft pilots 14 hours after alcohol ingestion: A preliminary report. Am. J. Psychiatry 1986, 143, 1546–1550. [Google Scholar]
- Yesavage, J.A.; Dolhert, N.; Taylor, J.L. Flight simulator performance of younger and older aircraft pilots: Effects of age and alcohol. J. Am. Geriatr. Soc. 1994, 42, 577–582. [Google Scholar] [CrossRef]
- Dzubak, C.M. Multitasking: The good, the bad, and the unknown. J. Assoc. Tutoring Prof. 2008, 1, 1–12. [Google Scholar]
- Wetherell, M.A.; Carter, K. The multitasking framework: The effects of increasing workload on acute psychobiological stress reactivity. Stress Health 2014, 30, 103–109. [Google Scholar] [CrossRef]
- Wetherell, M.A.; Hyland, M.E.; Harris, J.E. Secretory immunoglobulin A reactivity to acute and cumulative acute multi-tasking stress: Relationships between reactivity and perceived workload. Biol. Psychol. 2004, 66, 257–270. [Google Scholar] [CrossRef]
- Wetherell, M.A.; Atherton, K.; Grainger, J.; Brosnan, R.; Scholey, A.B. The effects of multitasking on psychological stress reactivity in recreational users of cannabis and MDMA. Hum. Psychopharmacol. Clin. Exp. 2012, 27, 167–176. [Google Scholar] [CrossRef]
- Wetherell, M.A.; Sidgreaves, M.C. Secretory immunoglobulin-A reactivity following increases in workload intensity using the Defined Intensity Stressor Simulation (DISS). Stress Health J. Int. Soc. Investig. Stress 2005, 21, 99–106. [Google Scholar] [CrossRef]
- Scholey, A.B.; Owen, L.; Gates, J.; Rodgers, J.; Buchanan, T.; Ling, J.; Heffernan, T.; Swan, P.; Stough, C.; Parrott, A.C. Hair MDMA samples are consistent with reported ecstasy use: Findings from a study investigating effects of ecstasy on mood and memory. Neuropsychobiology 2011, 63, 15–21. [Google Scholar] [CrossRef]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The Consensus Sleep Diary: Standardizing Prospective Sleep Self-Monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef]
- Forrest, A. The estimation of Widmark’s factor. J. Forensic Sci. Soc. 1986, 26, 249–252. [Google Scholar] [CrossRef]
- Watson, P.E.; Watson, I.D.; Batt, R.D. Prediction of blood alcohol concentrations in human subjects. Updating the Widmark Equation. J. Stud. Alcohol. 1981, 42, 547–556. [Google Scholar] [CrossRef]
- Seidl, S.; Jensen, U.; Alt, A. The calculation of blood ethanol concentrations in males and females. Int. J. Leg. Med. 2000, 114, 71–77. [Google Scholar] [CrossRef]
- Widmark, E.M.P. Principles and Applications of Medicolegal Alcohol Determination; Biomedical Publications: Davis, CA, USA, 1981. [Google Scholar]
- Ulrich, L.; Cramer, Y.; Zink, P. Relevance of individual parameters in the calculation of blood alcohol levels in relation to the volume of intake. Blutalkohol 1987, 24, 192. [Google Scholar]
- Scholey, A.; Haskell, C.; Robertson, B.; Kennedy, D.; Milne, A.; Wetherell, M. Chewing gum alleviates negative mood and reduces cortisol during acute laboratory psychological stress. Physiol. Behav. 2009, 97, 304–312. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Little, W.; Scholey, A.B. Attenuation of laboratory-induced stress in humans after acute administration of Melissa officinalis (Lemon Balm). Psychosom. Med. 2004, 66, 607–613. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Pace, S.; Haskell, C.; Okello, E.J.; Milne, A.; Scholey, A.B. Effects of cholinesterase inhibiting sage (Salvia officinalis) on mood, anxiety and performance on a psychological stressor battery. Neuropsychopharmacology 2006, 31, 845. [Google Scholar] [CrossRef]
- Benson, S.; Downey, L.A.; Stough, C.; Wetherell, M.; Zangara, A.; Scholey, A. An acute, double-blind, placebo-controlled cross-over study of 320 mg and 640 mg doses of Bacopa monnieri (CDRI 08) on multitasking stress reactivity and mood. Phytother. Res. 2014, 28, 551–559. [Google Scholar] [CrossRef]
- Hart, S. Development of a multi-dimensional workload rating scale: Results of empirical and theoretical research. Hum. Ment. Workload. 1988, 52, 139–183. [Google Scholar]
- Penning, R.; McKinney, A.; Bus, L.D.; Olivier, B.; Slot, K.; Verster, J.C. Measurement of alcohol hangover severity: Development of the Alcohol Hangover Severity Scale (AHSS). Psychopharmacology 2013, 225, 803–810. [Google Scholar] [CrossRef]
- Spielberger, C.; Gorsuch, R.; Lushene, R. The State Trait Anxiety Inventory Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1969. [Google Scholar]
- Bond, A.; Lader, M. The use of analogue scales in rating subjective feelings. Br. J. Med. Psychol. 1974, 47, 211–218. [Google Scholar] [CrossRef]
- Morris, S.B.; DeShon, R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods 2002, 7, 105. [Google Scholar] [CrossRef]
- Verster, J.C.; Kruisselbrink, L.D.; Slot, K.A.; Anogeianaki, A.; Adams, S.; Alford, C.; Arnoldy, L.; Ayre, E.; Balikji, S.; Benson, S. Sensitivity to experiencing alcohol hangovers: Reconsideration of the 0.11% Blood Alcohol Concentration (BAC) threshold for having a hangover. J. Clin. Med. 2020, 9, 179. [Google Scholar] [CrossRef] [PubMed]
- Rohsenow, D.J.; Howland, J.; Minsky, S.J.; Arnedt, J.T. Effects of heavy drinking by maritime academy cadets on hangover, perceived sleep, and next-day ship power plant operation. J. Stud. Alcohol. 2006, 67, 406–415. [Google Scholar] [CrossRef]
- van Schrojenstein Lantman, M.; Roth, T.; Roehrs, T.; Verster, J.C. Alcohol Hangover, Sleep Quality, and Daytime Sleepiness. Sleep Vigil. 2017, 1, 37–41. [Google Scholar] [CrossRef]
- Roehrs, T.; Roth, T. Sleep, sleepiness, and alcohol use. Alcohol Res. Health 2001, 25, 101–109. [Google Scholar]
- Ebrahim, I.O.; Shapiro, C.M.; Williams, A.J.; Fenwick, P.B. Alcohol and sleep I: Effects on normal sleep. Alcohol. Clin. Exp. Res. 2013, 37, 539–549. [Google Scholar] [CrossRef]
- Thakkar, M.M.; Sharma, R.; Sahota, P. Alcohol disrupts sleep homeostasis. Alcohol 2015, 49, 299–310. [Google Scholar] [CrossRef]
- Verster, J.C.; van de Loo, A.J.; Benson, S.; Scholey, A.; Stock, A.K. The assessment of overall hangover severity. J. Clin. Med. 2020, 9, 786. [Google Scholar] [CrossRef]
- Wetherell, M.A.; Craw, O.; Smith, K.; Smith, M.A. Psychobiological responses to critically evaluated multitasking. Neurobiol. Stress 2017, 7, 68–73. [Google Scholar] [CrossRef]
- Wolff, N.; Gussek, P.; Stock, A.K.; Beste, C. Effects of high-dose ethanol intoxication and hangover on cognitive flexibility. Addict. Biol. 2018, 23, 503–514. [Google Scholar] [CrossRef]
- Monsell, S.; Driver, J. Control of Cognitive Processes: Attention and Performance XVIII; MIT Press: Cambrigde, MA, USA, 2000; Volume 18. [Google Scholar]
- Tipple, C.; Benson, S.; Scholey, A. A review of the physiological factors associated with alcohol hangover. Curr. Drug Abuse Rev. 2016, 9, 93–98. [Google Scholar] [CrossRef]
- Tiplady, B.; Franklin, N.; Scholey, A. Effect of ethanol on judgments of performance. Br. J. Psychol. 2004, 95, 105–118. [Google Scholar] [CrossRef]
- van de Loo, A.; Mackus, M.; van Schrojenstein Lantman, M.; Kraneveld, A.; Brookhuis, K.; Garssen, J.; Scholey, A.; Verster, J. Susceptibility to alcohol hangovers: The association with self-reported immune status. Int. J. Environ. Res. Public Health 2018, 15, 1286. [Google Scholar] [CrossRef]
- van de Loo, A.J.; van Schrojenstein Lantman, M.; Mackus, M.; Scholey, A.; Verster, J.C. Impact of mental resilience and perceived immune functioning on the severity of alcohol hangover. BMC Res. Notes 2018, 11, 526. [Google Scholar] [CrossRef]
- White, A.; Hingson, R. The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013, 35, 201–218. [Google Scholar]
- Leitz, J.R.; Morgan, C.J.; Bisby, J.A.; Rendell, P.G.; Curran, H.V. Global impairment of prospective memory following acute alcohol. Psychopharmacology 2009, 205, 379–387. [Google Scholar] [CrossRef]
- Crego, A.; Holguín, S.R.; Parada, M.; Mota, N.; Corral, M.; Cadaveira, F. Binge drinking affects attentional and visual working memory processing in young university students. Alcohol. Clin. Exp. Res. 2009, 33, 1870–1879. [Google Scholar] [CrossRef] [PubMed]

| Item | Condition | t-Value | p-Value | Cohen’s d | |
|---|---|---|---|---|---|
| Control | Hangover | ||||
| Single-Item Severity Scale | |||||
| ‘How severe is your hangover?’ | 0.05(0.16) | 4.67(2.36) | 10.07 | <0.001 | 3.07 |
| Alcohol Hangover Severity Scale | |||||
| Fatigue | 2.40(2.36) | 7.36(2.18) | 9.08 | <0.001 | 1.82 |
| Apathy | 0.56(0.96) | 3.64(2.80) | 5.69 | <0.001 | 1.35 |
| Concentration problems | 1.00(1.41) | 5.88(2.22) | 10.54 | <0.001 | 2.20 |
| Clumsiness | 0.68(0.90) | 4.72(3.14) | 6.46 | <0.001 | 1.54 |
| Confusion | 0.48(1.12) | 3.48(3.20) | 5.30 | <0.001 | 1.38 |
| Thirst | 1.44(2.20) | 6.24(2.51) | 8.86 | <0.001 | 1.78 |
| Sweating | 0.40(1.04) | 1.20(1.94) | 2.02 | 0.055 | - |
| Shivering | 0.16(0.62) | 1.84(3.00) | 2.80 | 0.010 | 0.69 |
| Stomach pain | 0.08(0.28) | 2.36(2.84) | 4.04 | <0.001 | 1.10 |
| Nausea | 0.40(1.00) | 3.12(2.76) | 4.95 | <0.001 | 1.14 |
| Dizziness | 0.36(0.91) | 4.28(2.64) | 7.50 | <0.001 | 1.75 |
| Heart pounding | 0.40(1.23) | 2.24(2.52) | 3.71 | 0.001 | 0.82 |
| Total score | 0.70(0.74) | 3.86(1.83) | 8.90 | <0.001 | 2.03 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benson, S.; Ayre, E.; Garrisson, H.; Wetherell, M.A.; Verster, J.C.; Scholey, A. Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort. J. Clin. Med. 2020, 9, 1154. https://doi.org/10.3390/jcm9041154
Benson S, Ayre E, Garrisson H, Wetherell MA, Verster JC, Scholey A. Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort. Journal of Clinical Medicine. 2020; 9(4):1154. https://doi.org/10.3390/jcm9041154
Chicago/Turabian StyleBenson, Sarah, Elizabeth Ayre, Harriet Garrisson, Mark A Wetherell, Joris C Verster, and Andrew Scholey. 2020. "Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort" Journal of Clinical Medicine 9, no. 4: 1154. https://doi.org/10.3390/jcm9041154
APA StyleBenson, S., Ayre, E., Garrisson, H., Wetherell, M. A., Verster, J. C., & Scholey, A. (2020). Alcohol Hangover and Multitasking: Effects on Mood, Cognitive Performance, Stress Reactivity, and Perceived Effort. Journal of Clinical Medicine, 9(4), 1154. https://doi.org/10.3390/jcm9041154






