Assessment of the Psychological Situation in Adults with Congenital Heart Disease
Abstract
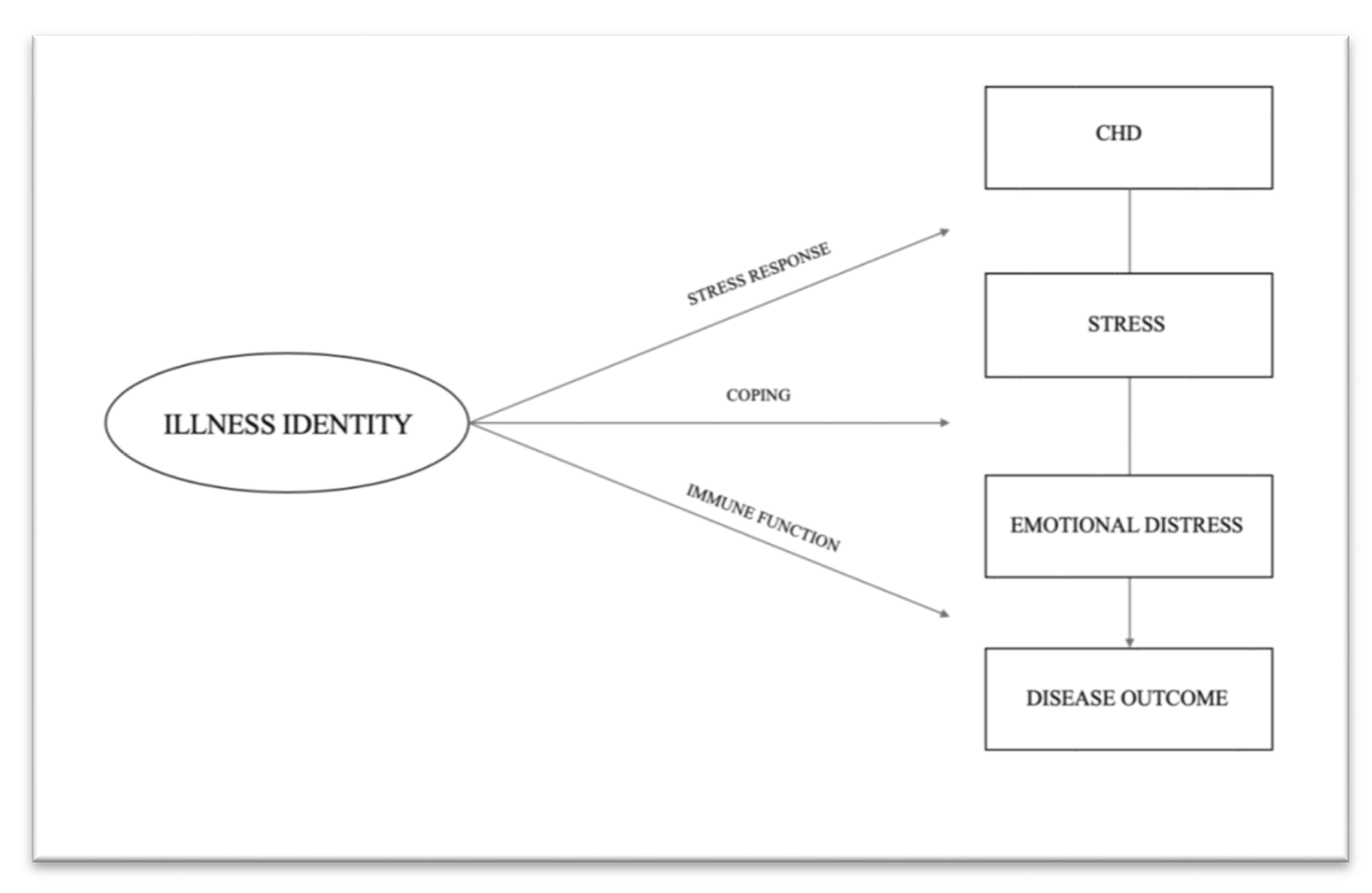
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Data Collection Procedures
2.3. Measures
2.3.1. Demographic and Clinical Information
2.3.2. Illness Identity
2.3.3. Depressive and Anxiety Symptoms
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Objective 1: Psychometric Properties of the IIQD
3.2.1. Reliability Analysis
3.2.2. Factorial Validity
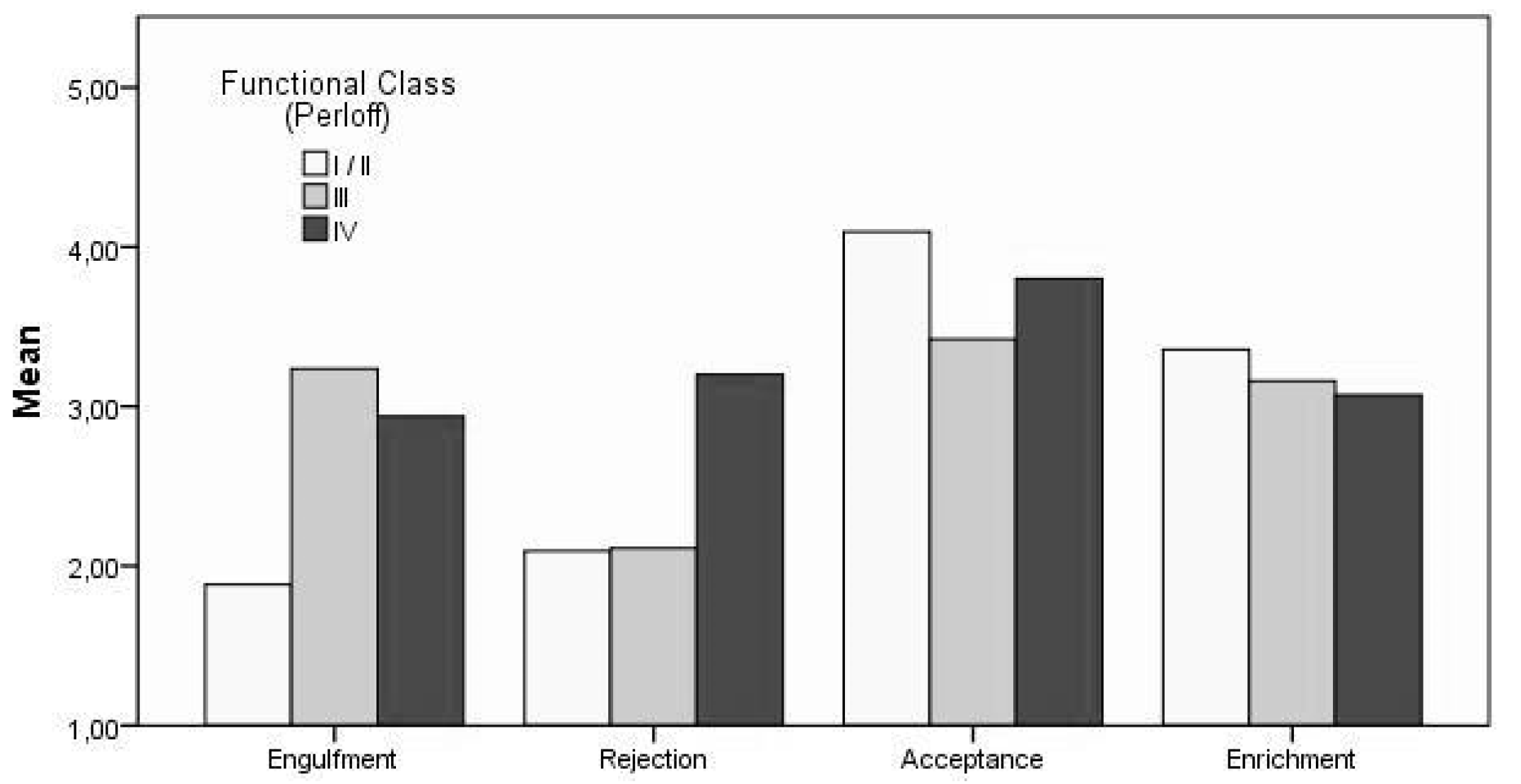
3.3. Objective 2: Associations Between Illness Identity and Clinical Parameters
3.4. Objective 3: Associations Between Illness Identity and Emotional Distress
4. Discussion
4.1. Objective 1: Psychometric Properties of the IIQD
4.2. Objective 2: Associations Between Illness Identity and Clinical Parameters
4.3. Objective 3: Associations Between Illness Identity and Emotional Distress
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Khairy, P. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2019, 73, e181–e192. [Google Scholar] [CrossRef]
- Neidenbach, R.C.; Lummert, E.; Vigl, M.; Zachoval, R.; Fischereder, M.; Engelhardt, A.; Hauser, M. Non-cardiac comorbidities in adults with inherited and congenital heart disease: Report from a single center experience of more than 800 consecutive patients. Cardiovasc. Diagn. Ther. 2018, 8, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Lui, G.K.; Saidi, A.; Bhatt, A.B.; Burchill, L.J.; Deen, J.F.; Earing, M.G.; Kovacs, A.H. Diagnosis and management of noncardiac complications in adults with congenital heart disease: A scientific statement from the American Heart Association. Circulation 2017, 136, e348–e392. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Desai, R.; Fong, H.K.; Sadolikar, A.; Samani, S.; Goyal, H. Extra-cardiac comorbidities or complications in adults with congenital heart disease: A nationwide inpatient experience in the United States. Cardiovasc. Diagn. Ther. 2018, 8, 814–819. [Google Scholar] [CrossRef] [PubMed]
- Andonian, C.; Beckmann, J.; Biber, S.; Ewert, P.; Freilinger, S.; Kaemmerer, H.; Neidenbach, R.C. Current research status on the psychological situation of adults with congenital heart disease. Cardiovasc. Diagn. Ther. 2018, 8, 799–804. [Google Scholar] [CrossRef]
- Deng, L.X.; Khan, A.M.; Drajpuch, D.; Fuller, S.; Ludmir, J.; Mascio, C.E.; Kim, Y.Y. Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. Am. J. Cardiol. 2016, 117, 853–857. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Froelicher, E.S.; Blumenthal, J.A.; Carney, R.M.; Doering, L.V.; Frasure-Smith, N.; Vaccarino, V. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: Systematic review and recommendations: A scientific statement from the American Heart Association. Circulation 2014, 129, 1350–1369. [Google Scholar] [CrossRef]
- Park, J.-H.; Tahk, S.-J.; Bae, S.H. Depression and anxiety as predictors of recurrent cardiac events 12 months after percutaneous coronary interventions. J. Cardiovasc. Nurs. 2015, 30, 351–359. [Google Scholar] [CrossRef]
- Watkins, L.L.; Koch, G.G.; Sherwood, A.; Blumenthal, J.A.; Davidson, J.R.; O’Connor, C.; Sketch, M.H., Jr. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J. Am. Heart Assoc. 2013, 2, e000068. [Google Scholar] [CrossRef]
- Celano, C.M.; Millstein, R.A.; Bedoya, C.A.; Healy, B.C.; Roest, A.M.; Huffman, J.C. Association between anxiety and mortality in patients with coronary artery disease: A meta-analysis. Am. Heart J. 2015, 170, 1105–1115. [Google Scholar] [CrossRef]
- Oris, L.; Luyckx, K.; Rassart, J.; Goubert, L.; Goossens, E.; Apers, S.; Moons, P. Illness identity in adults with a chronic illness. J. Clin. Psychol. Med. Settings 2018, 25, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Vargas, S. Stress, coping, and health. In The Oxford Handbook of Health Psychology; Oxford University Press: Oxford, UK, 2011; pp. 162–188. [Google Scholar]
- Leventhal, H.; Idler, E.L.; Leventhal, E.A. The impact of chronic illness on the self system. Rutgers Ser. Self Soc. Identity 1999, 2, 185–208. [Google Scholar]
- Charmaz, K. The body, identity, and self: Adapting to impairment. Sociol. Q. 1995, 36, 657–680. [Google Scholar] [CrossRef]
- Schulman-Green, D.; Jaser, S.; Martin, F.; Alonzo, A.; Grey, M.; McCorkle, R.; Whittemore, R. Processes of self-management in chronic illness. J. Nurs. Scholarsh. 2012, 44, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Thiene, G.; Frescura, C. Anatomical and pathophysiological classification of congenital heart disease. Cardiovasc. Pathol. 2010, 19, 259–274. [Google Scholar] [CrossRef]
- World Medical Association. Ethical principles for medical research involving human subjects. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2001, 8, 221–223. [Google Scholar] [CrossRef]
- Warnes, C.A.; Liberthson, R.; Danielson, G.K.; Dore, A.; Harris, L.; Hoffman, J.I.; Webb, G.D. Task force 1: The changing profile of congenital heart disease in adult life. J. Am. Coll. Cardiol. 2001, 37, 1170–1175. [Google Scholar] [CrossRef]
- Oris, L.; Rassart, J.; Prikken, S.; Verschueren, M.; Goubert, L.; Moons, P.; Luyckx, K. Illness identity in adolescents and emerging adults with type 1 diabetes: Introducing the illness identity questionnaire. Diab. Care 2016, 39, 757–763. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Norton, S.; Cosco, T.; Doyle, F.; Done, J.; Sacker, A. The Hospital Anxiety and Depression Scale: A meta confirmatory factor analysis. J. Psychosom. Res. 2013, 74, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Perloff, J.K.; Warnes, C.A. Challenges posed by adults with repaired congenital heart disease. Circulation 2001, 103, 2637–2643. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Charmaz, K. From the “sick role” to stories of self: Understanding the self in illness. Rutgers Series Self Soc. Identity 1999, 2, 209–239. [Google Scholar]
- Kovacs, A.H.; Sears, S.F.; Saidi, A.S. Biopsychosocial experiences of adults with congenital heart disease: Review of the literature. Am. Heart J. 2005, 150, 193–201. [Google Scholar] [CrossRef]
- Kovacs, A.H.; Bendell, K.L.; Colman, J.; Harrison, J.L.; Oechslin, E.; Silversides, C. Adults with congenital heart disease: Psychological needs and treatment preferences. Congenit. Heart Dis. 2009, 4, 139–146. [Google Scholar] [CrossRef]
- Kovacs, A.H.; Saidi, A.S.; Kuhl, E.A.; Sears, S.F.; Silversides, C.; Harrison, J.L.; Nolan, R.P. Depression and anxiety in adult congenital heart disease: Predictors and prevalence. Int. J. Cardiol. 2009, 137, 158–164. [Google Scholar] [CrossRef]
- Sobczak, M.; Kasprzak, J.D.; Drygas, W. Psychocardiology—Introduction to a new scientific discipline. Kardiol. Pol. 2011, 69, 838–843. [Google Scholar]
- Eifert, G.H. Cardiophobia: A paradigmatic behavioural model of heart-focused anxiety and non-anginal chest pain. Behav. Res. Ther. 1992, 30, 329–345. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Allman, E.; Berry, D.; Nasir, L. Depression and coping in heart failure patients: A review of the literature. J. Cardiovasc. Nurs. 2009, 24, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Doering, L.V.; Dracup, K.; Caldwell, M.A.; Moser, D.K.; Erickson, V.S.; Fonarow, G.; Hamilton, M. Is coping style linked to emotional states in heart failure patients? J. Card. Fail. 2004, 10, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, R.B.; Blumenthal, J.A.; O’Connor, C.; Adams, K.; Hinderliter, A.; Dupree, C.; Sherwood, A. Coping styles in heart failure patients with depressive symptoms. J. Psychosom. Res. 2009, 67, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Dew, M.A.; Simmons, R.G.; Roth, L.H.; Schulberg, H.C.; Thompson, M.E.; Armitage, J.M.; Griffith, B.P. Psychosocial predictors of vulnerability to distress in the year following heart transplantation. Psychol. Med. 1994, 24, 929–945. [Google Scholar] [CrossRef]
- Felton, B.J.; Revenson, T.A. Coping with chronic illness: A study of illness controllability and the influence of coping strategies on psychological adjustment. J. Consult. Clin. Psychol. 1984, 52, 343–353. [Google Scholar] [CrossRef]
- Celano, C.M.; Daunis, D.J.; Lokko, H.N.; Campbell, K.A.; Huffman, J.C. Anxiety disorders and cardiovascular disease. Curr. Psychiatry Rep. 2016, 18, 101. [Google Scholar] [CrossRef]
- Stanton, A.L.; Revenson, T.A. Adjustment to chronic disease: Progress and promise in research. In The Oxford Handbook of Health Psychology; Oxford University Press: Oxford, UK, 2011; pp. 241–268. [Google Scholar]
- Adair, J.G. The Hawthorne effect: A reconsideration of the methodological artifact. J. Appl. Psychol. 1984, 69, 334. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: Berlin, Germany, 1984. [Google Scholar]

| Variables | Value |
|---|---|
| Age, years | 38.2 ± 12.5 (18−7318−73) |
| Gender (n = 229), n (%) | |
| Female | 103 (45.0) |
| Male | 126 (55.0) |
| BMI-values (n = 229), n (%) | |
| Underweight | 10 (4.4) |
| Normal weight | 107 (46.7) |
| Pre-obesity | 8 (3.4) |
| Obesity | 24 (10.4) |
| Marital status (n = 221), n (%) | |
| Married | 94 (42.5) |
| Divorced | 4 (1.8) |
| Engaged | 42 (19.0) |
| Single | 80 (36.2) |
| Widowed | 1 (0.5) |
| Level of school education (n = 217), n (%) | |
| No schooling completed | 11 (5.1) |
| Primary school degree | 55 (25.3) |
| Secondary school degree | 60 (27.6) |
| Vocational / polytechnic degree | 28 (12.9) |
| General University Entrance Qualification | 63 (29.0) |
| Financial standing (n = 223), n (%) | |
| Poor | 21 (9.4) |
| Fair | 61 (27.4) |
| Good | 141 (63.2) |
| Variables | Value |
|---|---|
| Cyanosis (n = 229), n (%) | |
| Acyanotic | 221 (96.5) |
| Cyanotic | 8 (3.5) |
| Functional Class (Perloff) (n = 229), n (%) | |
| I/II | 218 (95.2) |
| III | 9 (3.9) |
| IV | 2 (.9) |
| Severity code of CHD according to Warnes classification (n = 214), n (%) | |
| Simple | 54 (23.6) |
| Intermediate | 88 (38.4) |
| Severe | 72 (31.4) |
| Severity code of miscellaneous CHD (n = 15), n (%) | |
| Simple | 2 (13.3) |
| Severe | 13 (86.7) |
| Leading diagnosis (n = 229), n (%) | |
| Complex congenital heart defects | 75 (32.8) |
| Post-tricuspid shunts | 18 (7.9) |
| Left heart malformation | 44 (19.2) |
| Right heart malformation | 39 (17.0) |
| Pre-tricuspid shunts | 35 (15.3) |
| Other | 18 (7.9) |
| Previous heart surgery (n = 229), n (%) | |
| No | 70 (30.6) |
| Yes | 159 (69.4) |
| Latent Construct | # Items | Cronbach’s α |
|---|---|---|
| IIQD | ||
| Rejection | 5 | 0.79 |
| Acceptance | 5 | 0.88 |
| Engulfment | 8 | 0.93 |
| Enrichment | 7 | 0.90 |
| IIQD: German version of Illness Identity Questionnaire |
| Effect | Wilks’ λ | F | Sig. | Partial η2 |
|---|---|---|---|---|
| Warnes | 0.87 | 3.48 | 0.001 | 0.064 |
| Engulfment | - | 2.35 | 0.098 | 0.022 |
| Rejection | - | 2.83 | 0.061 | 0.027 |
| Acceptance | - | 5.41 | 0.005 | 0.050 |
| Enrichment | - | 1.38 | 0.253 | 0.013 |
| Functional Class (Perloff) | 0.87 | 3.62 | 0.000 | 0.067 |
| Engulfment | - | 10.56 | 0.000 | 0.093 |
| Rejection | - | 1.99 | 0.139 | 0.019 |
| Acceptance | - | 2.18 | 0.115 | 0.021 |
| Enrichment | - | .51 | 0.601 | 0.005 |
| Warnes * Functional Class (Perloff) | 0.916 | 1.51 | 0.114 | 0.029 |
| Variable | M | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
|---|---|---|---|---|---|---|---|---|---|
| 1. Engulfment | 1.94 | 1.01 | 1 | ||||||
| 2. Rejection | 2.10 | 0.94 | 0.38 ** | 1 | |||||
| 3. Acceptance | 4.06 | 0.97 | −0.41 ** | −0.49 ** | 1 | ||||
| 4. Enrichment | 3.34 | 1.01 | −0.13 * | −0.27 ** | 0.36 ** | 1 | |||
| 5. HADS-Anxiety | 7.97 | 4.06 | 0.61 ** | 0.40 ** | −0.39 ** | −0.27 ** | 1 | ||
| 6. HADS-Depression | 7.91 | 4.05 | 0.68 ** | 0.32 ** | −0.41 ** | −0.34 ** | 0.66 ** | 1 | |
| 7. Need for information | 3.08 | .72 | 0.11 | −0.09 | 0.04 | 0.18 ** | 0.01 | −0.01 | 1 |
| DV: Anxiety | DV: Depression | |||
|---|---|---|---|---|
| Predictor Variables | B | SE | B | SE |
| Socio-Demographics | ||||
| Age, years | 0.00 | 0.02 | 0.05 * | 0.02 * |
| Gender | 0.69 | 0.47 | −0.76 | 0.43 |
| Marital Status | 0.99 | 0.55 | −0.09 | 0.51 |
| BMI | 0.05 | 0.06 | 0.07 | 0.05 |
| Financial standing | −0.20 | 0.37 | −0.48 | 0.34 |
| School education | −0.04 | 0.23 | 0.16 | 0.21 |
| Professional education | 0.36 | 0.35 | −0.44 | 0.32 |
| Clinical Classification | ||||
| Warnes | 0.21 | 0.34 | 0.23 | 0.31 |
| Functional class (Perloff) | −0.40 | 0.45 | 0.81 | 0.41 |
| Heart surgery | −1.35 * | 0.58 * | −0.22 | 0.53 |
| Cyanosis | −2.33 * | 1.13 * | 0.17 | 1.04 |
| Illness Identity | ||||
| Engulfment | 2.45 ** | 0.28 ** | 2.39 ** | 0.26 ** |
| Rejection | 0.69 * | 0.27 * | −0.06 | 0.25 |
| Acceptance | 0.01 | 0.28 | −0.16 | 0.25 |
| Enrichment | −0.44 | 0.23 | −0.97 ** | 0.21 ** |
| R2 | 0.50 | 0.59 | ||
| R2-adjusted | 0.46 | 0.56 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andonian, C.; Beckmann, J.; Ewert, P.; Freilinger, S.; Kaemmerer, H.; Oberhoffer-Fritz, R.; Sack, M.; Neidenbach, R. Assessment of the Psychological Situation in Adults with Congenital Heart Disease. J. Clin. Med. 2020, 9, 779. https://doi.org/10.3390/jcm9030779
Andonian C, Beckmann J, Ewert P, Freilinger S, Kaemmerer H, Oberhoffer-Fritz R, Sack M, Neidenbach R. Assessment of the Psychological Situation in Adults with Congenital Heart Disease. Journal of Clinical Medicine. 2020; 9(3):779. https://doi.org/10.3390/jcm9030779
Chicago/Turabian StyleAndonian, Caroline, Jürgen Beckmann, Peter Ewert, Sebastian Freilinger, Harald Kaemmerer, Renate Oberhoffer-Fritz, Martin Sack, and Rhoia Neidenbach. 2020. "Assessment of the Psychological Situation in Adults with Congenital Heart Disease" Journal of Clinical Medicine 9, no. 3: 779. https://doi.org/10.3390/jcm9030779
APA StyleAndonian, C., Beckmann, J., Ewert, P., Freilinger, S., Kaemmerer, H., Oberhoffer-Fritz, R., Sack, M., & Neidenbach, R. (2020). Assessment of the Psychological Situation in Adults with Congenital Heart Disease. Journal of Clinical Medicine, 9(3), 779. https://doi.org/10.3390/jcm9030779






