Objective Assessment of Counselling for Fetal Heart Defects: An Interdisciplinary Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Reliability Analyses
3.2. Descriptive Analyses
3.3. Overall Counselling Success as per Definition and in the Five Analytical Dimensions
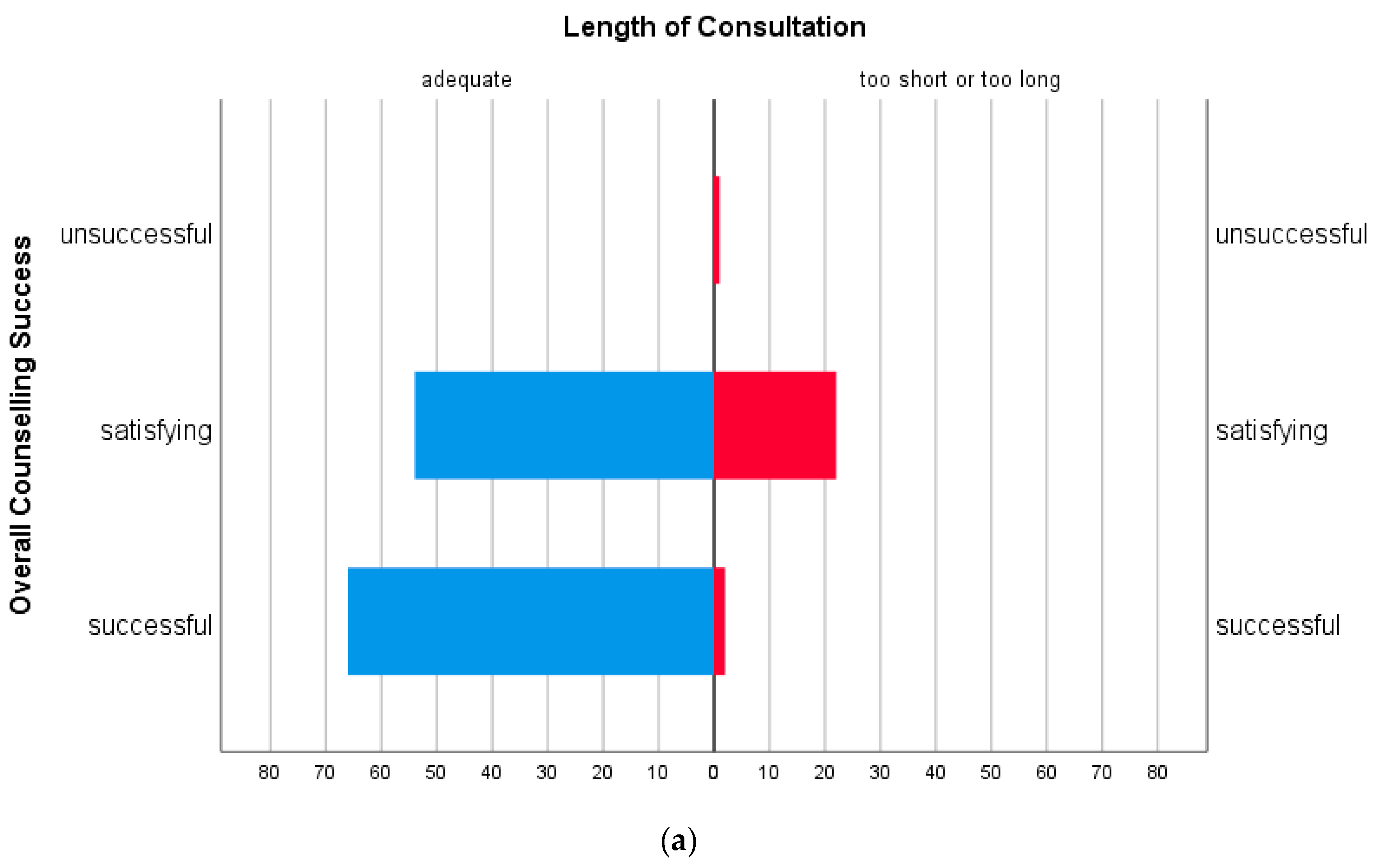
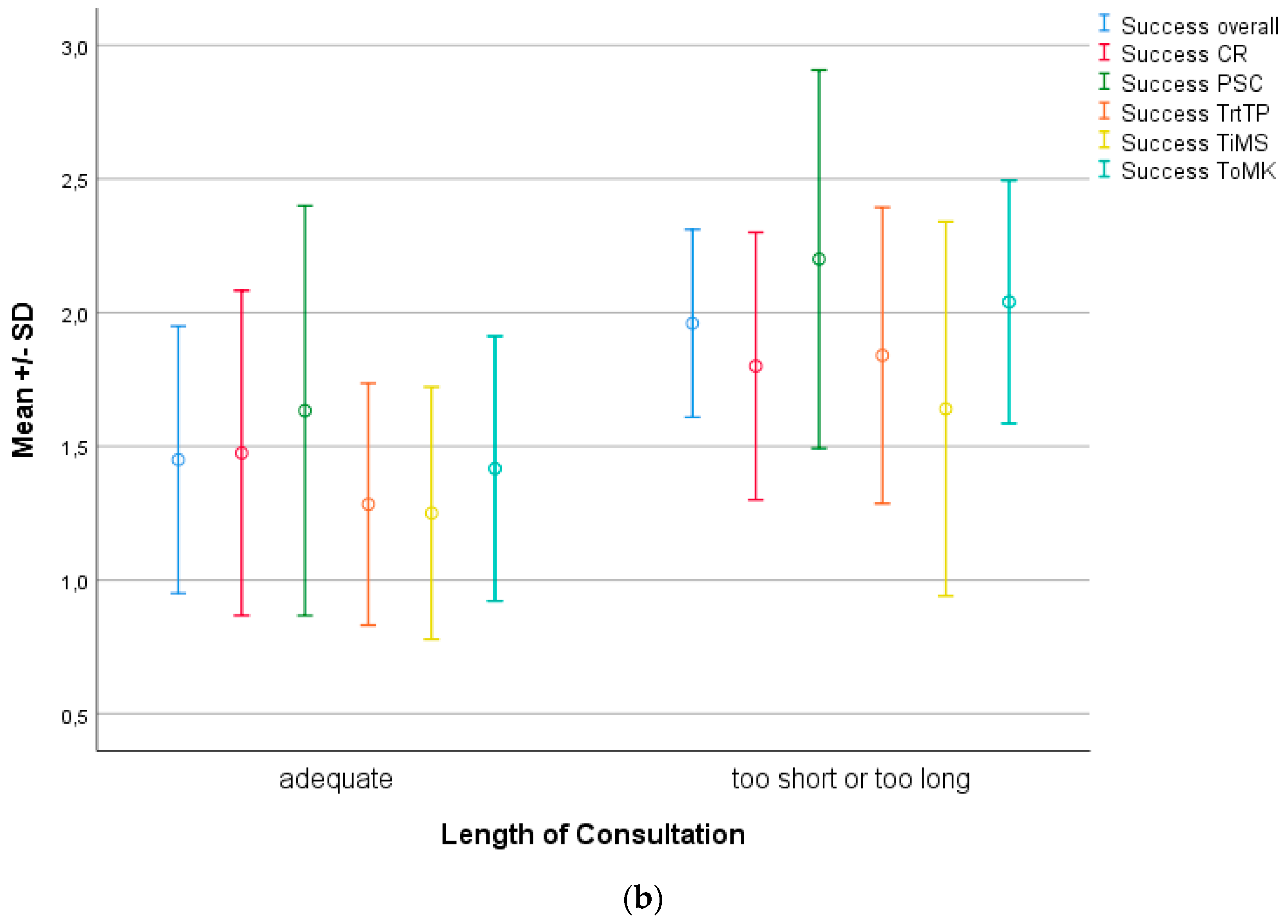
3.4. Effect of Duration and Interruptions of Counselling
3.5. Informational Aspects
3.6. Influence of a Separate Counselling Room
3.7. Counselling Success Depending on Severity of CHD
3.8. Influence of German as Native Language
3.9. Counselling Success Depending on Who Has Counselled and How Often
3.10. Counselling Success Depending on the Institution
4. Discussion
4.1. Literature Review
4.2. Summary
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Van der Linde, D.; Konings, E.E.; Slager, M.A.; Witsenburg, M.; Helbing, W.A.; Takkenberg, J.J.; Roos-Hesselink, J.W. Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2011, 58, 2241–2247. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, D.; Coltri, A.; Butera, G.; Fermont, L.; Le Bidois, J.; Kachaner, J.; Sidi, D. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation 1999, 99, 916–918. [Google Scholar] [CrossRef] [PubMed]
- Franklin, O.; Burch, M.; Manning, N.; Sleeman, K.; Gould, S.; Archer, N. Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbidity. Heart 2002, 87, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Tworetzky, W.; McElhinney, D.B.; Reddy, V.M.; Brook, M.M.; Hanley, F.L.; Silverman, N.H. Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation 2001, 103, 1269–1273. [Google Scholar] [CrossRef]
- Holland, B.J.; Myers, J.A.; Woods, C.R., Jr. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: A meta-analysis. Ultrasound Obstet. Gynecol. 2015, 45, 631–638. [Google Scholar] [CrossRef]
- Allan, L.D.; Huggon, I.C. Counselling following a diagnosis of congenital heart disease. Prenat. Diagn. 2004, 24, 1136–1142. [Google Scholar] [CrossRef]
- Donofrio, M.T.; Moon-Grady, A.J.; Hornberger, L.K.; Copel, J.A.; Sklansky, M.S.; Abuhamad, A.; Cuneo, B.F.; Huhta, J.C.; Jonas, R.A.; Krishnan, A.; et al. Diagnosis and treatment of fetal cardiac disease: A scientific statement from the American Heart Association. Circulation 2014, 129, 2183–2242. [Google Scholar] [CrossRef]
- Allan, L.; Dangel, J.; Fesslova, V.; Marek, J.; Mellander, M.; Oberhänsli, I.; Oberhoffer, R.; Sharland, G.; Simpson, J.; Sonesson, S.E. Fetal Cardiology Working Group; Recommendations for the practice of fetal cardiology in Europe. Association for European Paediatric Cardiology. Cardiol. Young 2004, 14, 109–114. [Google Scholar] [CrossRef]
- Arya, B.; Glickstein, J.S.; Levasseur, S.M.; Williams, I.A. Parents of children with congenital heart disease prefer more information than cardiologists provide. Congenit. Heart Dis. 2013, 8, 78–85. [Google Scholar] [CrossRef]
- Kovacevic, A.; Simmelbauer, A.; Starystach, S.; Elsässer, M.; Sohn, C.; Müller, A.; Bär, S.; Gorenflo, M. Assessment of Needs for Counseling After Prenatal Diagnosis of Congenital Heart Disease—A Multidisciplinary Approach. Klin. Padiatr. 2018, 230, 251–256. [Google Scholar] [CrossRef]
- Bertsche, T.; Neininger, M.P.; Kaune, A.; Schumacher, P.M.; Dumeier, H.K.; Bernhard, M.K.; Syrbe, S.; Kiess, W.; Merkenschlager, A.; Bertsche, A. Interdisciplinary Concepts of Paediatrics and Clinical Pharmacy to Optimise Anticonvulsant Treatment. Klin. Padiatr. 2018, 230, 5–12. [Google Scholar] [PubMed]
- Maibach-Nagel, E. Pflegekräftemangel: Ein wirklich großes Thema. Dtsch. Arztebl. 2018, 115, 505. [Google Scholar]
- Carlsson, T.; Bergman, G.; Wadensten, B.; Mattsson, E. Experiences of informational needs and received information following a prenatal diagnosis of congenital heart defect. Prenat. Diagn. 2016, 36, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Bratt, E.L.; Järvholm, S.; Ekman-Joelsson, B.M.; Mattson, L.Å.; Mellander, M. Parent’s experiences of counselling and their need for support following a prenatal diagnosis of congenital heart disease—A qualitative study in a Swedish context. BMC Pregnancy Childbirth. 2015, 15, 171. [Google Scholar] [CrossRef] [PubMed]
- Paladini, D.; Alfirevic, Z.; Carvalho, J.S.; Khalil, A.; Malinger, G.; Martinez, J.M.; Rychik, J.; Gardiner, H. Prenatal counseling for neurodevelopmental delay in congenital heart disease: Results of a worldwide survey of experts’ attitudes advise caution. Ultrasound Obstet. Gynecol. 2016, 47, 667–671. [Google Scholar] [CrossRef]
- Paladini, D.; Alfirevic, Z.; Carvalho, J.S.; Khalil, A.; Malinger, G.; Martinez, J.M.; Rychik, J.; Ville, Y.; Gardiner, H.; ISUOG Clinical Standards Committee. ISUOG consensus statement on current understanding of the association of neurodevelopmental delay and congenital heart disease: Impact on prenatal counseling. Ultrasound Obstet. Gynecol. 2017, 49, 287–288. [Google Scholar] [CrossRef]
- Kovacevic, A.; Öhman, A.; Tulzer, G.; Herberg, U.; Dangel, J.; Carvalho, J.S.; Fesslova, V.; Jicinska, H.; Sarkola, T.; Pedroza, C.; et al. Fetal hemodynamic response to aortic valvuloplasty and postnatal outcome: A European multicenter study. Ultrasound Obstet. Gynecol. 2018, 52, 221–229. [Google Scholar] [CrossRef]
- Friedman, K.G.; Sleeper, L.A.; Freud, L.R.; Marshall, A.C.; Godfrey, M.E.; Drogosz, M.; Lafranchi, T.; Benson, C.B.; Wilkins-Haug, L.E.; Tworetzky, W. Improved technical success, postnatal outcome and refined predictors of outcome for fetal aortic valvuloplasty. Ultrasound Obstet. Gynecol. 2018, 52, 212–220. [Google Scholar] [CrossRef]
- Tulzer, A.; Arzt, W.; Gitter, R.; Prandstetter, C.; Grohmann, E.; Mair, R.; Tulzer, G. Immediate effects and outcome of in-utero pulmonary valvuloplasty in fetuses with pulmonary atresia with intact ventricular septum or critical pulmonary stenosis. Ultrasound Obstet. Gynecol. 2018, 52, 230–237. [Google Scholar] [CrossRef]
- Malhotra, A.; Menahem, S.; Gillam, L. Ethical issues in fetal management: A cardiac perspective. Int. J. Pediatr. 2010, 2010, 857460. [Google Scholar] [CrossRef]
- Menahem, S.; Grimwade, J. Counselling strategies in the prenatal diagnosis of major heart abnormality. Heart Lung Circ. 2004, 13, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Flaig, F.; Lotz, J.D.; Knochel, K.; Borasio, G.D.; Führer, M.; Hein, K. Perinatal Palliative Care: A qualitative study evaluating the perspectives of pregnancy counselors. Palliat. Med. 2019, 33, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Nell, S.; Wijngaarde, C.A.; Pistorius, L.R.; Slieker, M.; ter Heide, H.; Manten, G.T.; Freund, M.W. Fetal heart disease: Severity, associated anomalies and parental decision. Fetal Diagn. Ther. 2013, 33, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.J.; Verghese, G.R.; Ferguson, M.E.; Fino, N.F.; Goldberg, D.J.; Owens, S.T.; Pinto, N.; Zyblewski, S.C.; Quartermain, M.D. Counseling Practices for Fetal Hypoplastic Left Heart Syndrome. Pediatr. Cardiol. 2017, 38, 946–958. [Google Scholar] [CrossRef]
| Counselling Success | |
|---|---|
| overall | 0.905 |
| Transfer of Medical Knowledge | 0.792 |
| Trust in Medical Staff | 0.792 |
| Transparency regarding Treatment Process | 0.809 |
| Coping resources | 0.770 |
| Sorrows | 0.815 |
| Counselling Success in % | |||
|---|---|---|---|
| Successful | Satisfying | Unsuccessful | |
| Overall | 47.3 | 52.1 | 0.7 |
| Transfer of Medical Knowledge | 47.6 | 50.6 | 1.8 |
| Trust in Medical Staff | 70.6 | 26.3 | 3.1 |
| Transparency regarding the Treatment Process | 63.4 | 35.4 | 1.2 |
| Coping resources | 50.3 | 44.7 | 5.0 |
| Perceived Situational Control | 43.9 | 33.5 | 22.6 |
| Written or Online Information: | ||
|---|---|---|
| Provided | Not Provided | |
| Overall Counselling Success | 57.7% | 41.5% |
| Transfer of Medical Knowledge | 65.5% | 38.5% |
| Trust in Medical Staff | 78.2% | 66.7% |
| Transparency regarding Treatment Process | 76.8% | 59.3% |
| Coping resources | 59.3% | 45.8% |
| Perceived situational control | 61.8% | 34.9% |
| Degree of CHD Severity | |||
|---|---|---|---|
| 1 | 2 | 3 | |
| overall | 71.4 % | 47.5 % | 42.7 % |
| Transfer of Medical Knowledge | 61.1 % | 43.5 % | 45.4 % |
| Trust in Medical Staff | 88.2 % | 66.7 % | 69.5 % |
| Transparency regarding Treatment Process | 88.9 % | 55.3 % | 62.5 % |
| Coping resources | 76.5 % | 47.7 % | 46.4 % |
| Perceived situational control | 36.8 % | 37.8 % | 47.4 % |
| Native Language | ||
|---|---|---|
| German | Not German | |
| overall | 48.8 % | 40.9 % |
| Transfer of Medical Knowledge | 50.0 % | 37.0 % |
| Trust in Medical Staff | 74.6 % | 48.1 % |
| Transparency regarding Treatment Process | 64.7 % | 52.0 % |
| Coping resources | 50.7 % | 50.0 % |
| Perceived situational control | 44.4 % | 38.5 % |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovacevic, A.; Bär, S.; Starystach, S.; Simmelbauer, A.; Elsässer, M.; Müller, A.; Mohammadi Motlagh, A.; Oberhoffer-Fritz, R.; Ostermayer, E.; Ewert, P.; et al. Objective Assessment of Counselling for Fetal Heart Defects: An Interdisciplinary Multicenter Study. J. Clin. Med. 2020, 9, 467. https://doi.org/10.3390/jcm9020467
Kovacevic A, Bär S, Starystach S, Simmelbauer A, Elsässer M, Müller A, Mohammadi Motlagh A, Oberhoffer-Fritz R, Ostermayer E, Ewert P, et al. Objective Assessment of Counselling for Fetal Heart Defects: An Interdisciplinary Multicenter Study. Journal of Clinical Medicine. 2020; 9(2):467. https://doi.org/10.3390/jcm9020467
Chicago/Turabian StyleKovacevic, Alexander, Stefan Bär, Sebastian Starystach, Andreas Simmelbauer, Michael Elsässer, Andreas Müller, Aida Mohammadi Motlagh, Renate Oberhoffer-Fritz, Eva Ostermayer, Peter Ewert, and et al. 2020. "Objective Assessment of Counselling for Fetal Heart Defects: An Interdisciplinary Multicenter Study" Journal of Clinical Medicine 9, no. 2: 467. https://doi.org/10.3390/jcm9020467
APA StyleKovacevic, A., Bär, S., Starystach, S., Simmelbauer, A., Elsässer, M., Müller, A., Mohammadi Motlagh, A., Oberhoffer-Fritz, R., Ostermayer, E., Ewert, P., Gorenflo, M., & Wacker-Gussmann, A. (2020). Objective Assessment of Counselling for Fetal Heart Defects: An Interdisciplinary Multicenter Study. Journal of Clinical Medicine, 9(2), 467. https://doi.org/10.3390/jcm9020467




