The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases
Abstract
1. Introduction
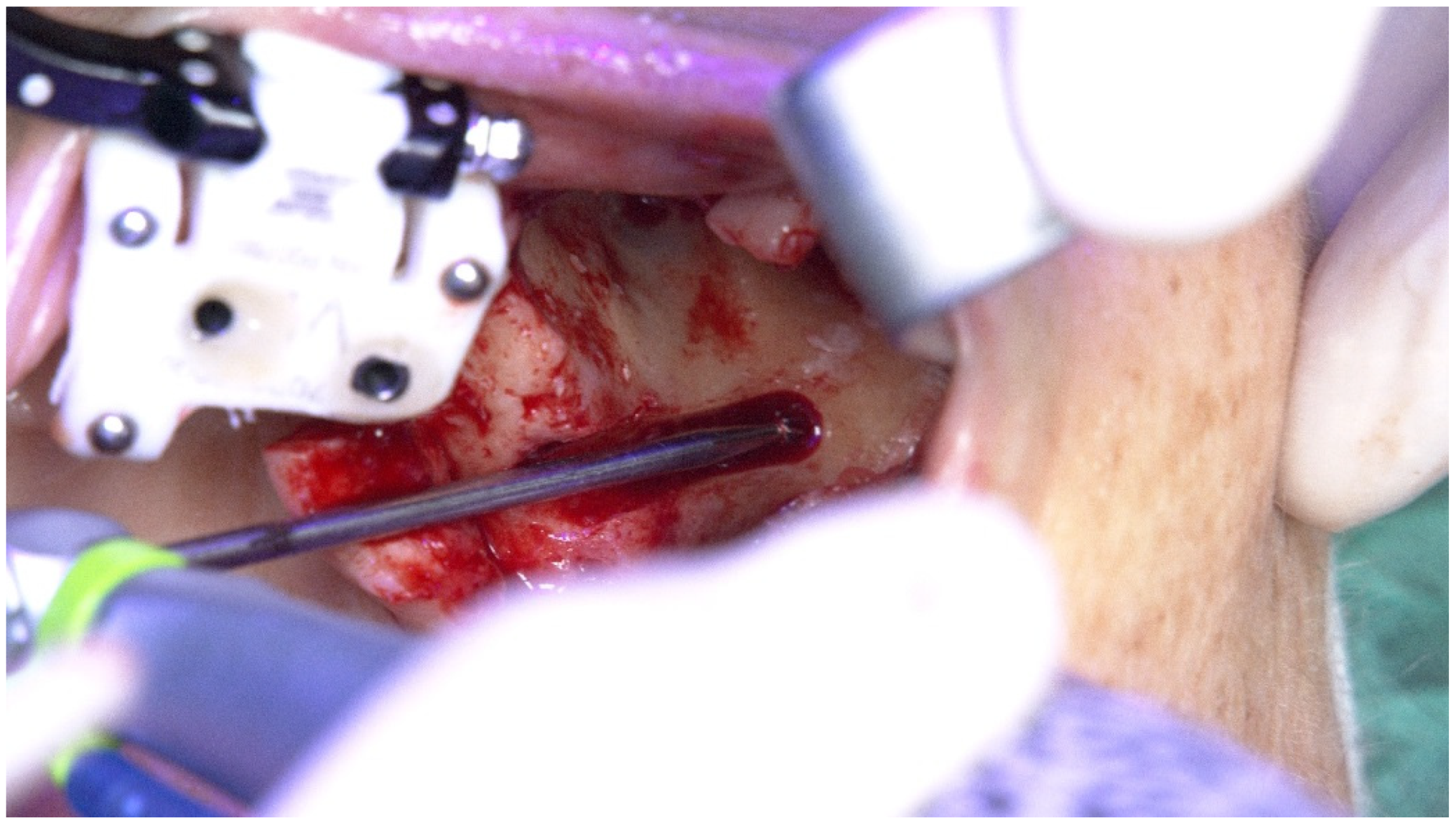
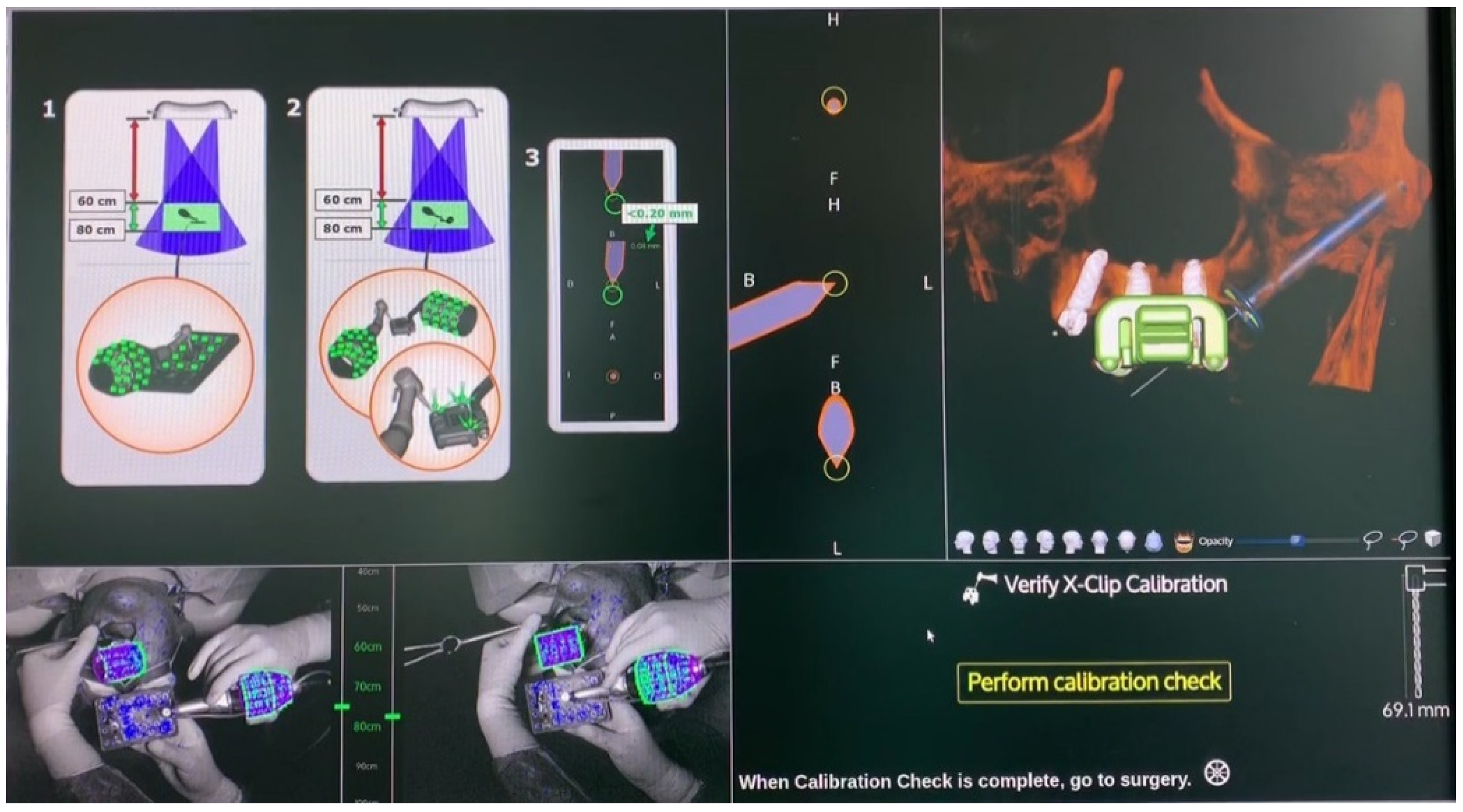
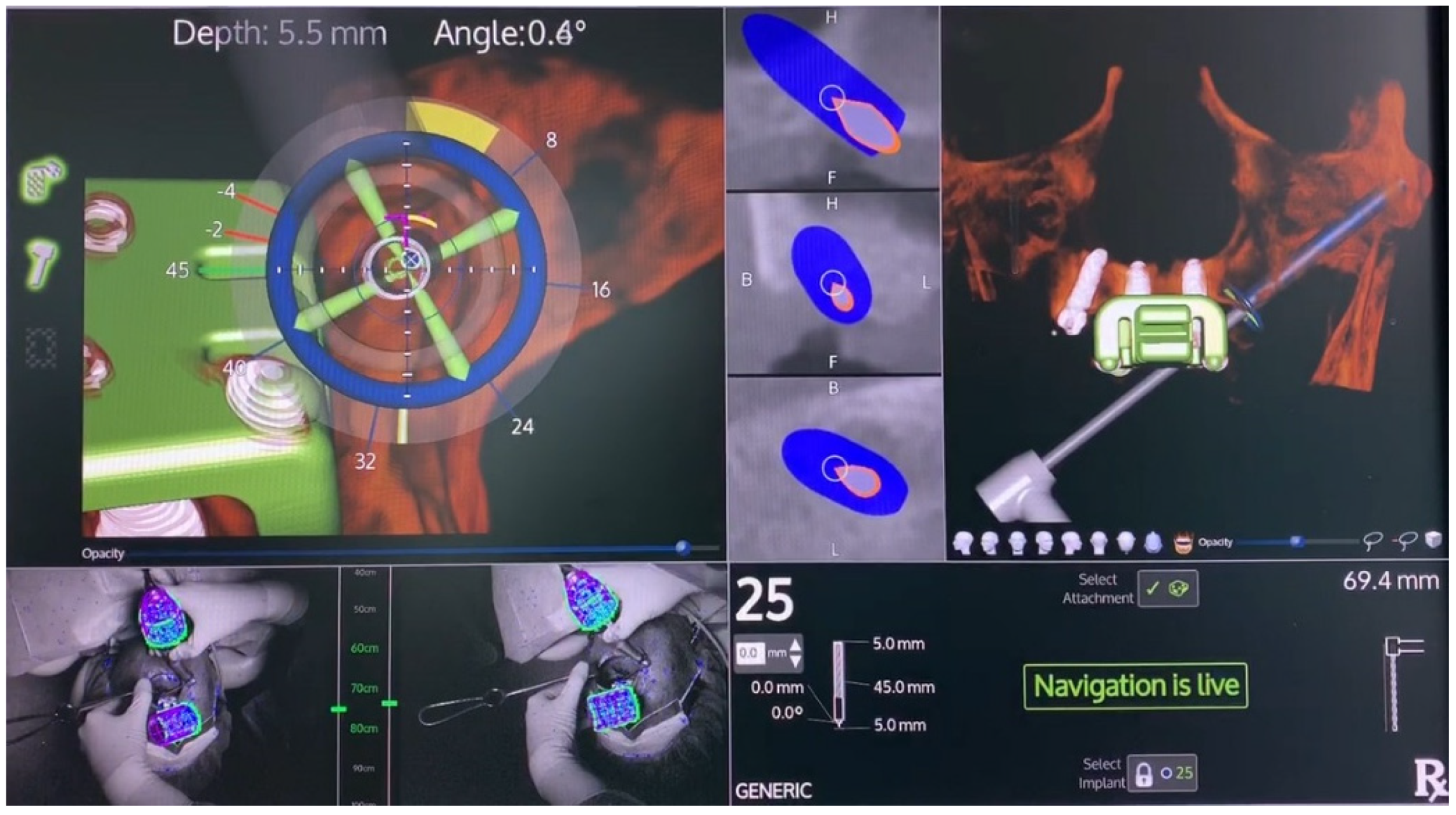
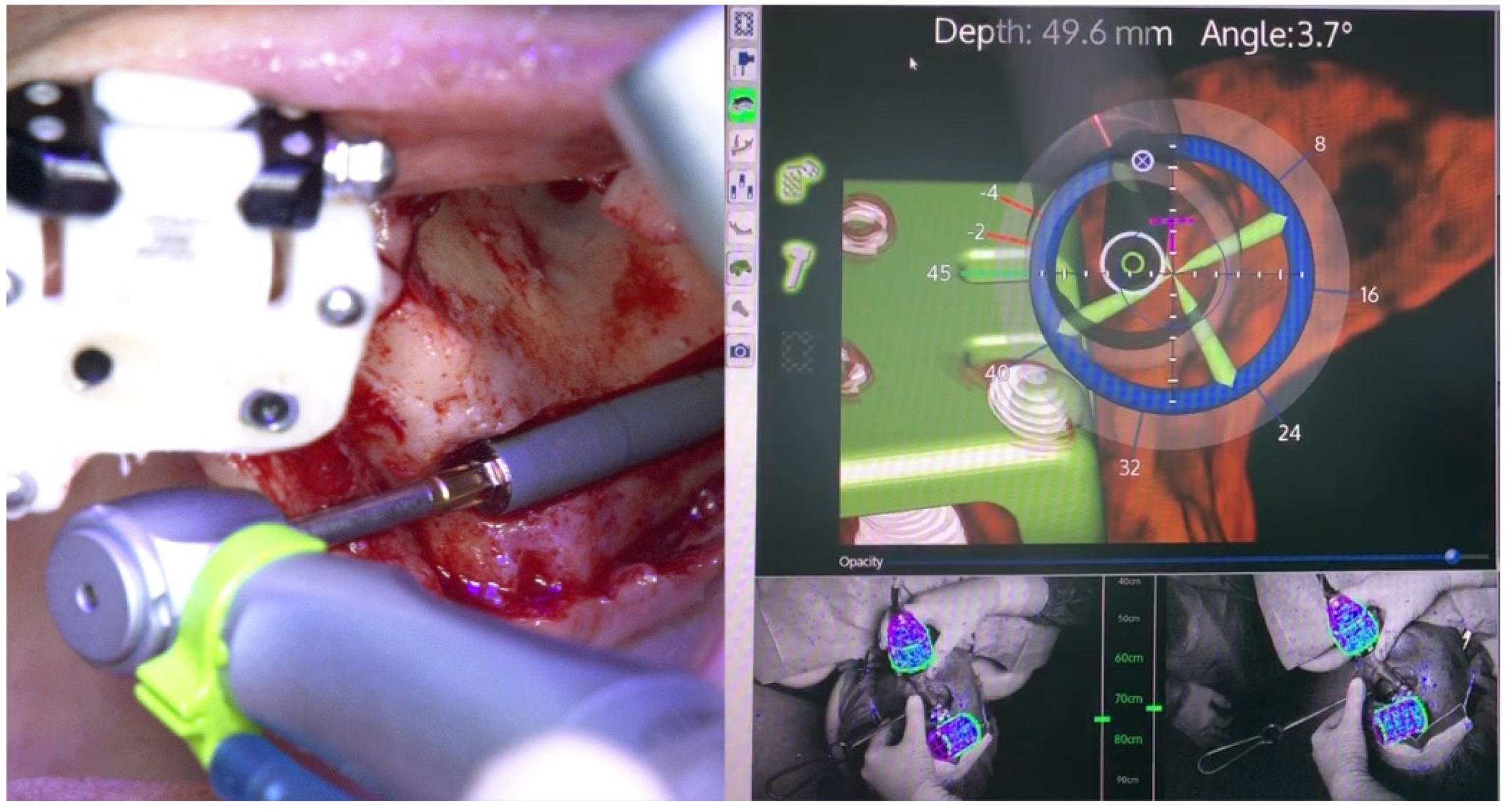
2. Case Reports
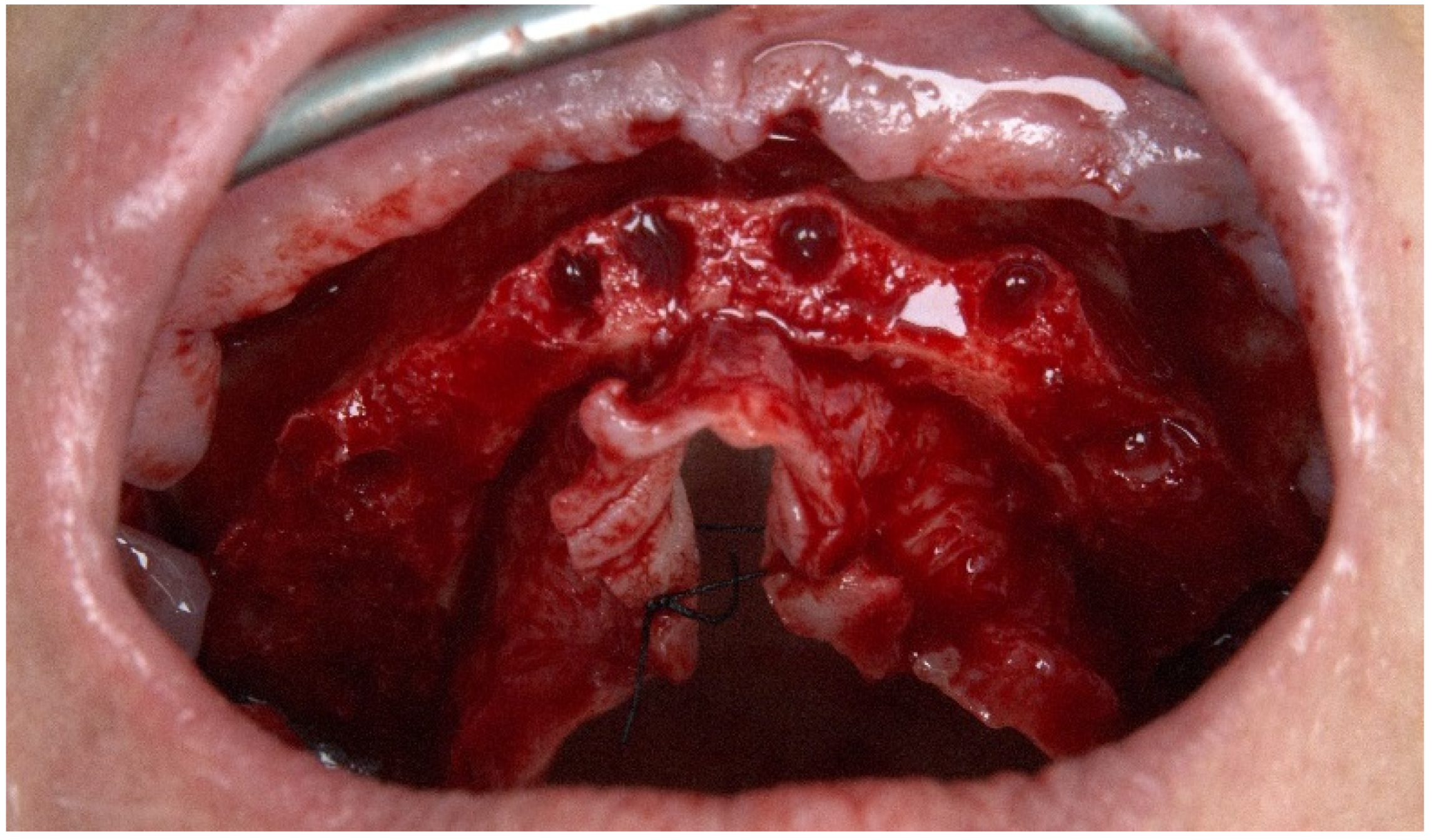
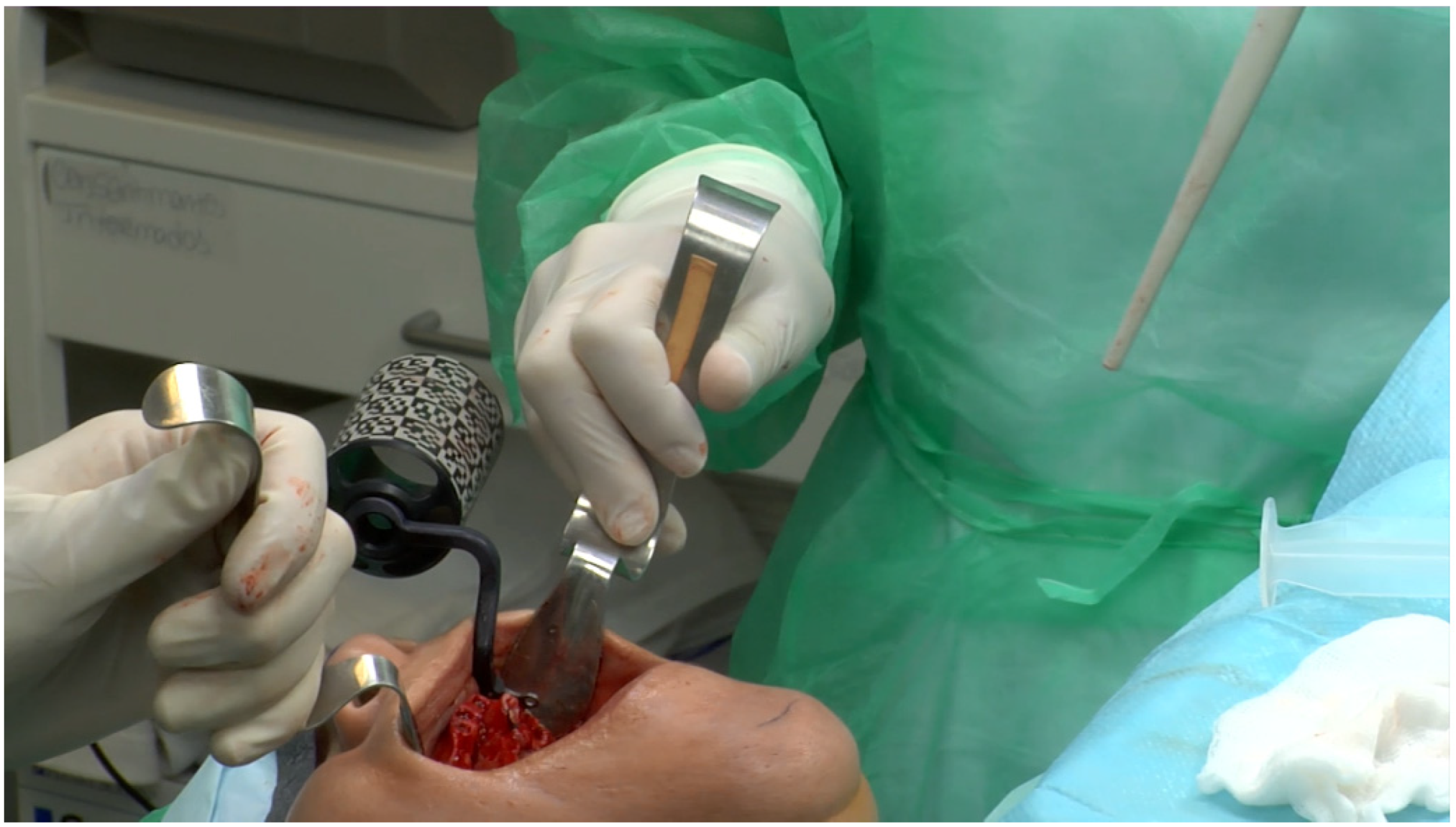
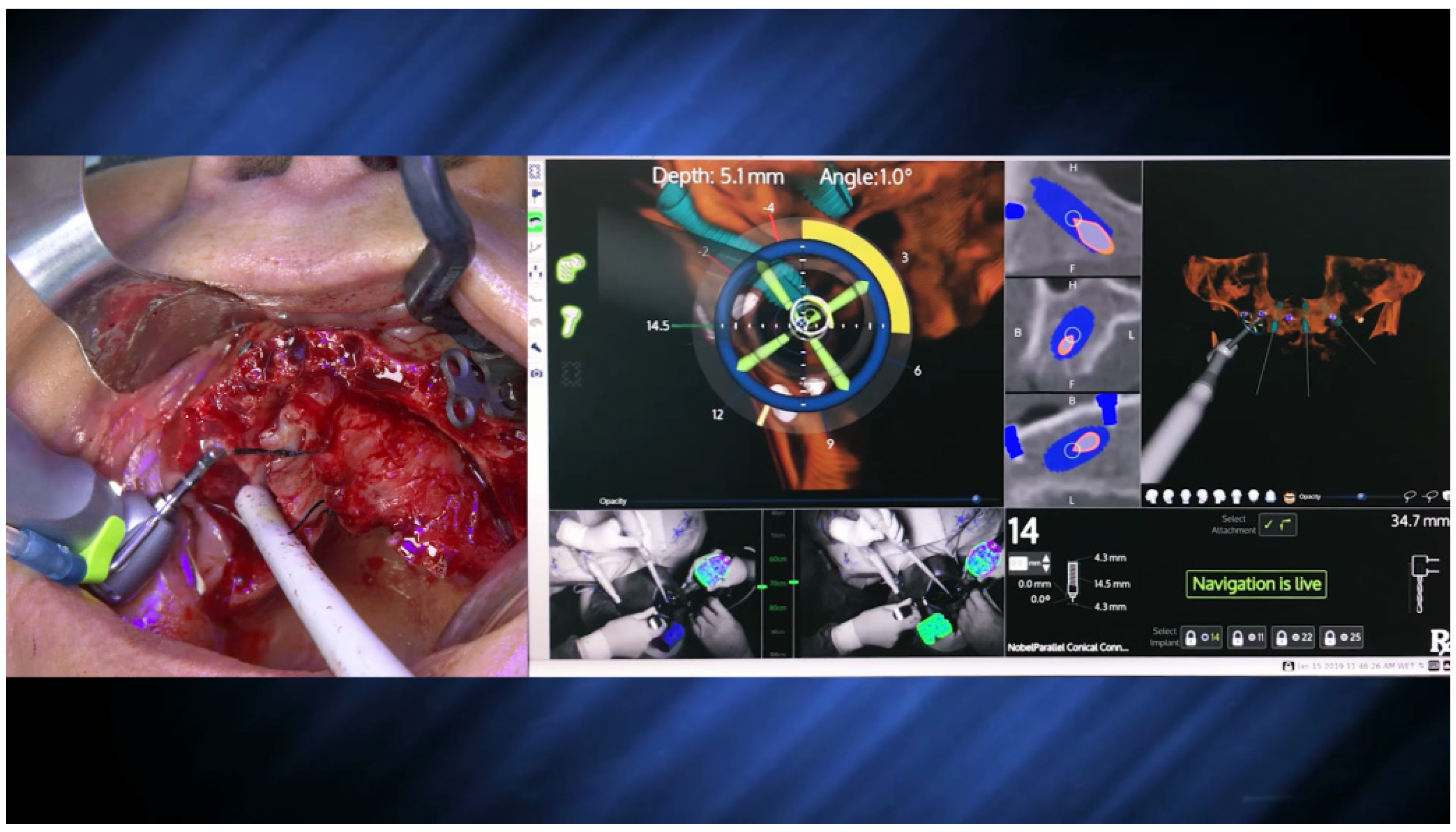
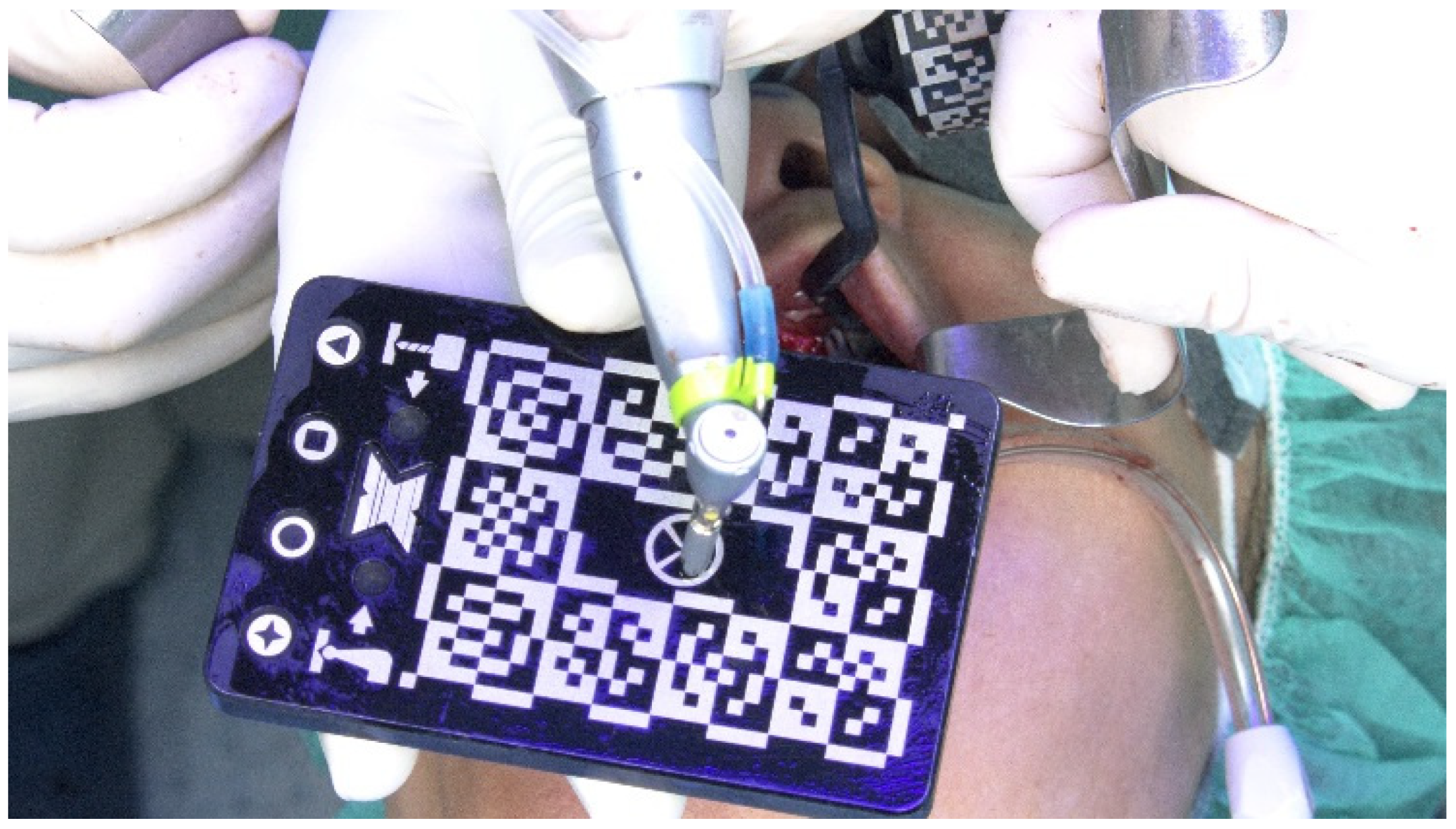
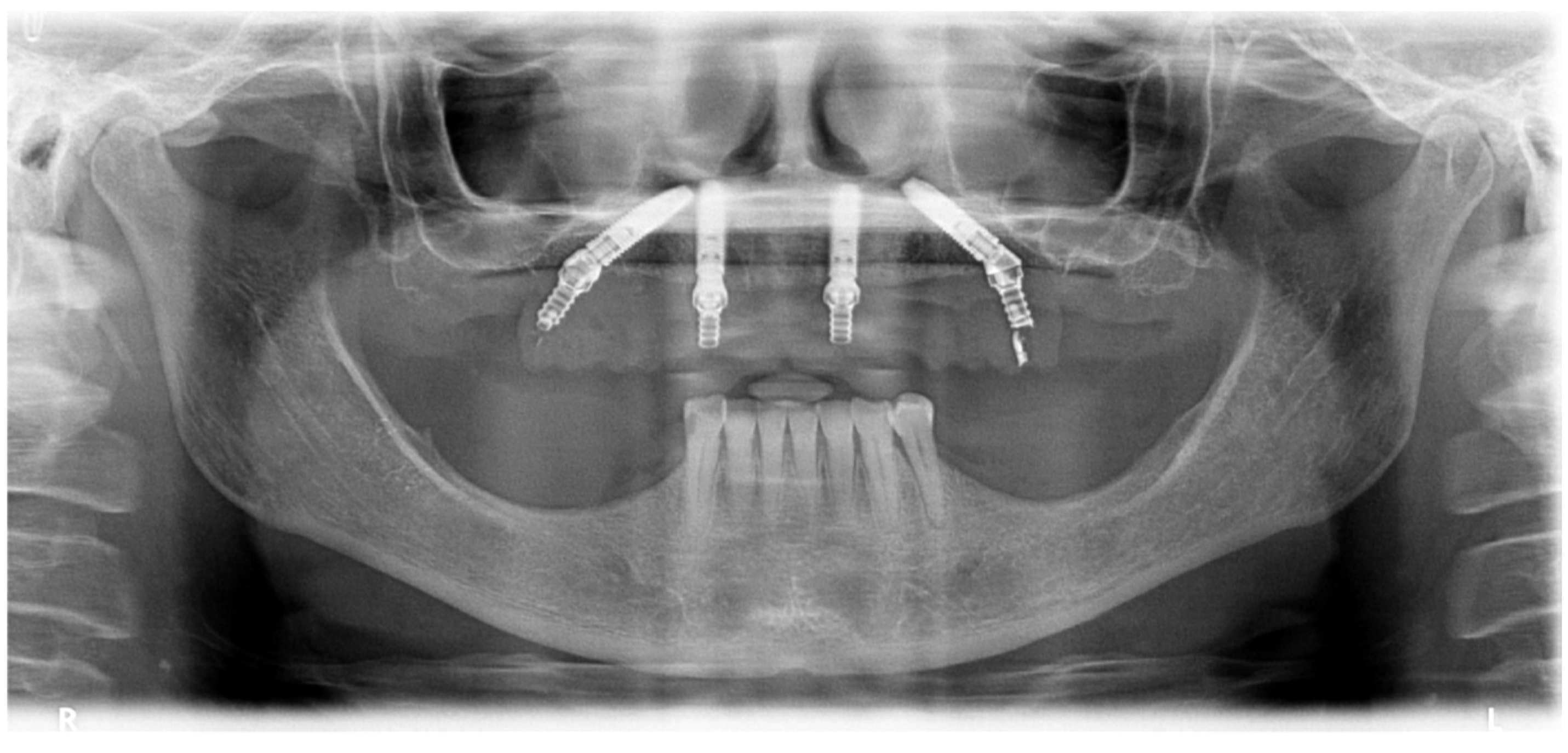
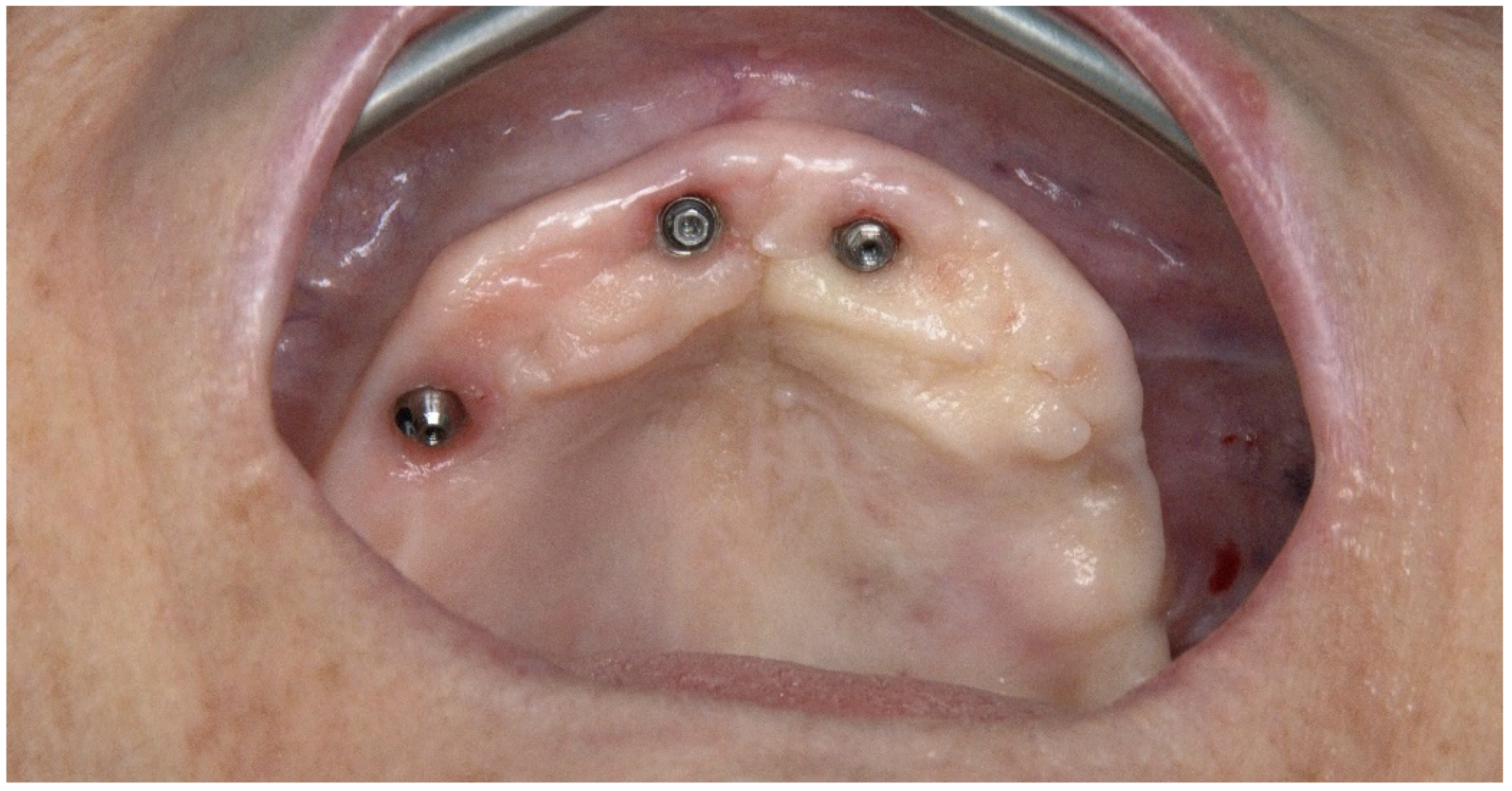
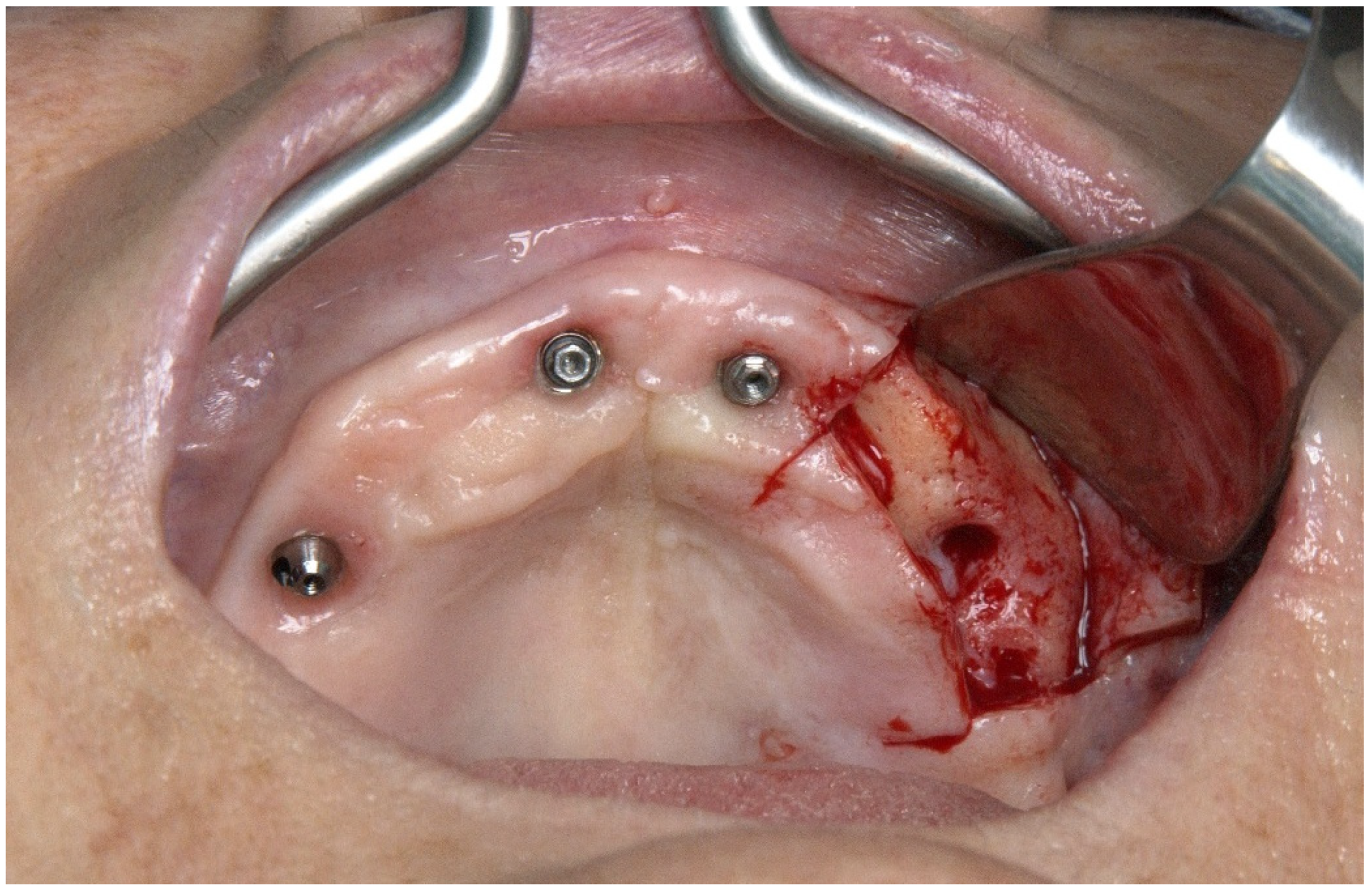
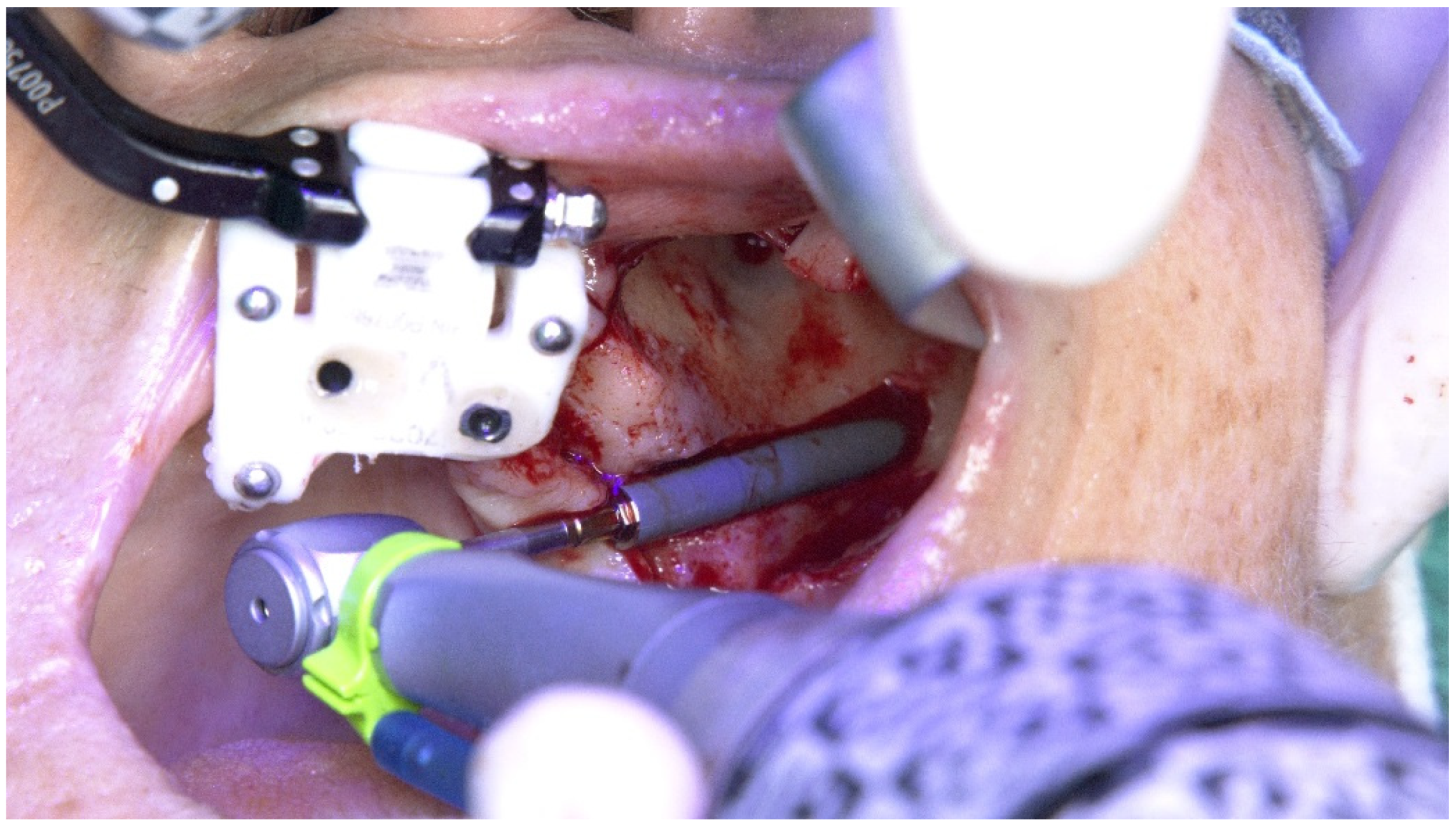
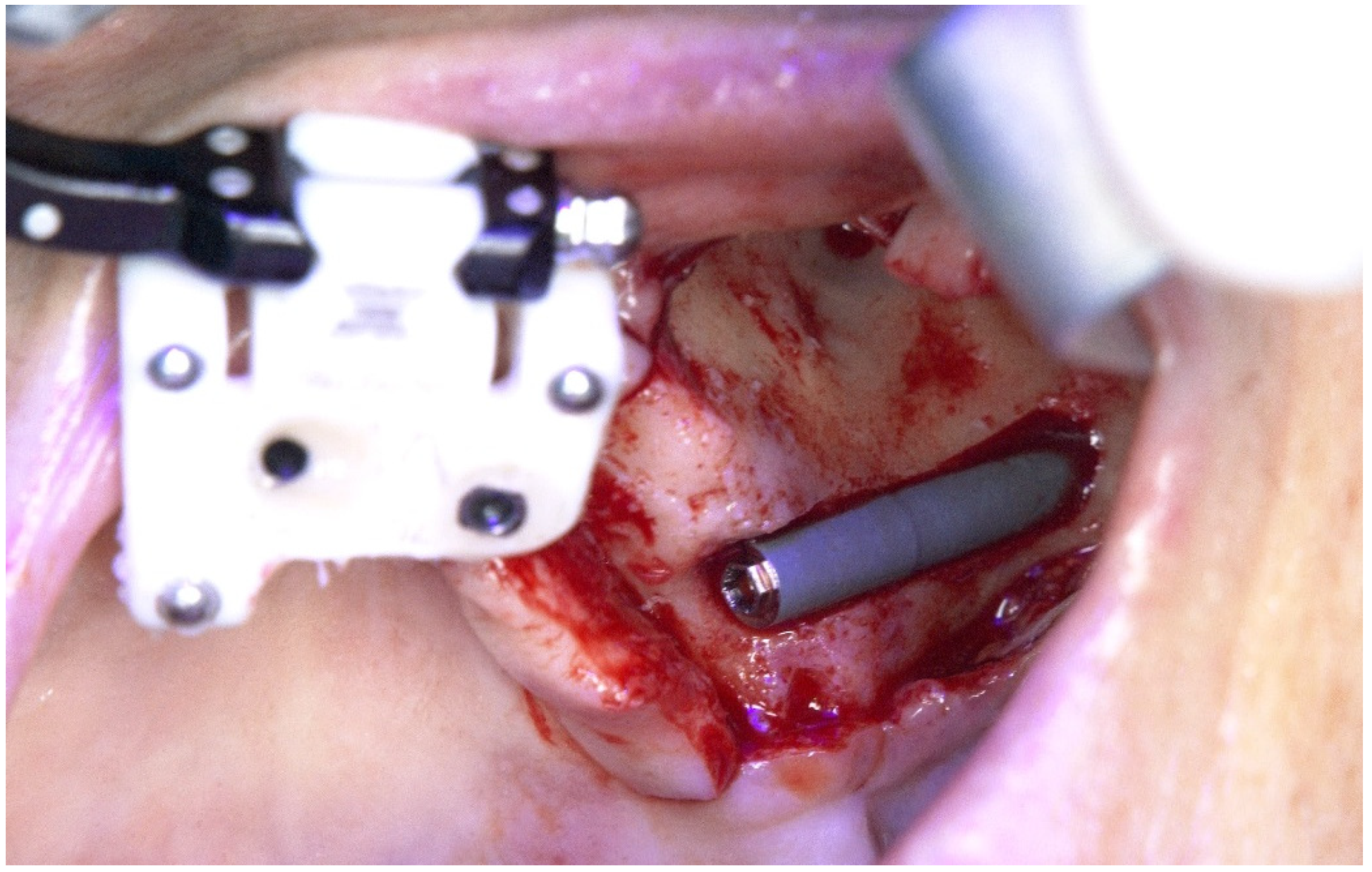
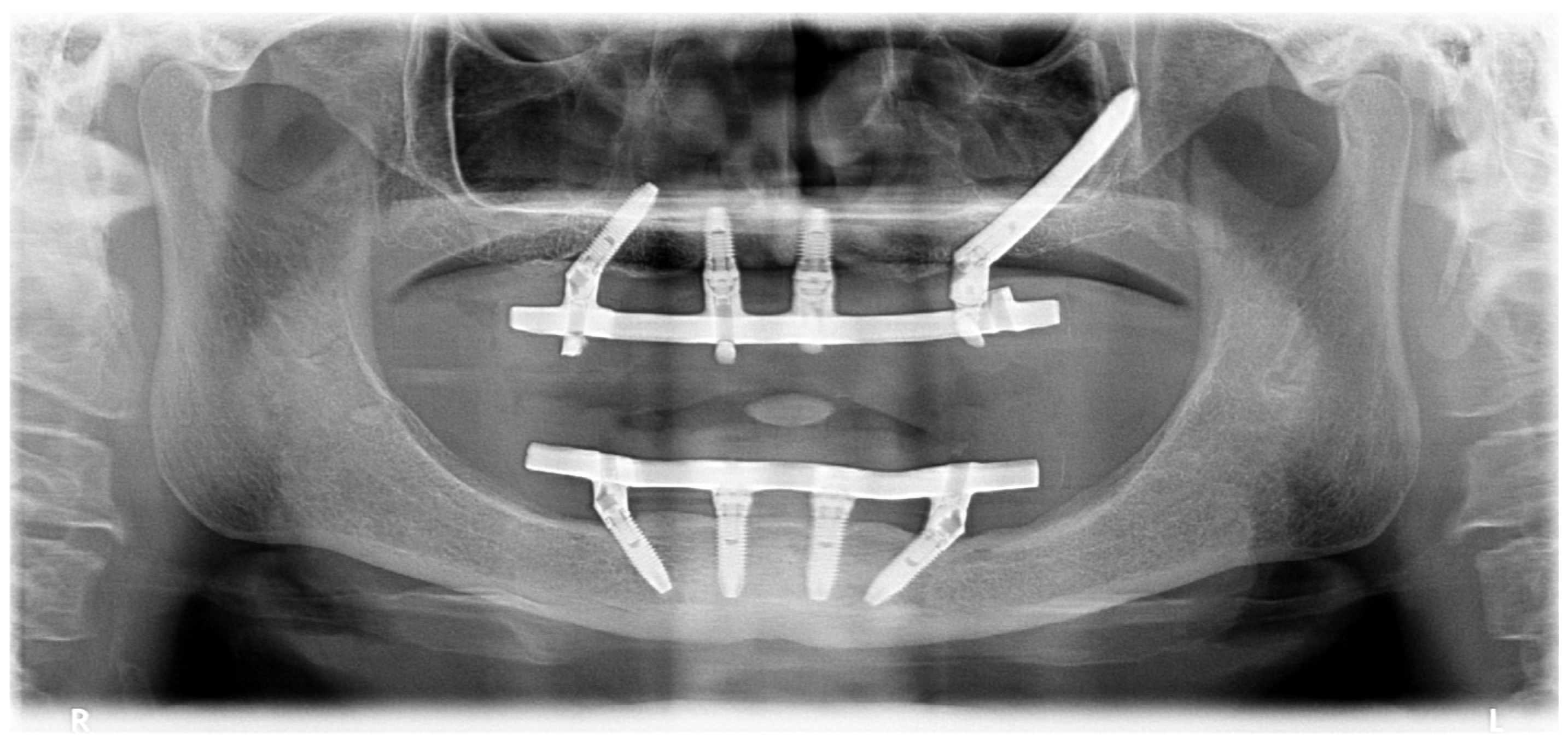
2.1. Patient 1
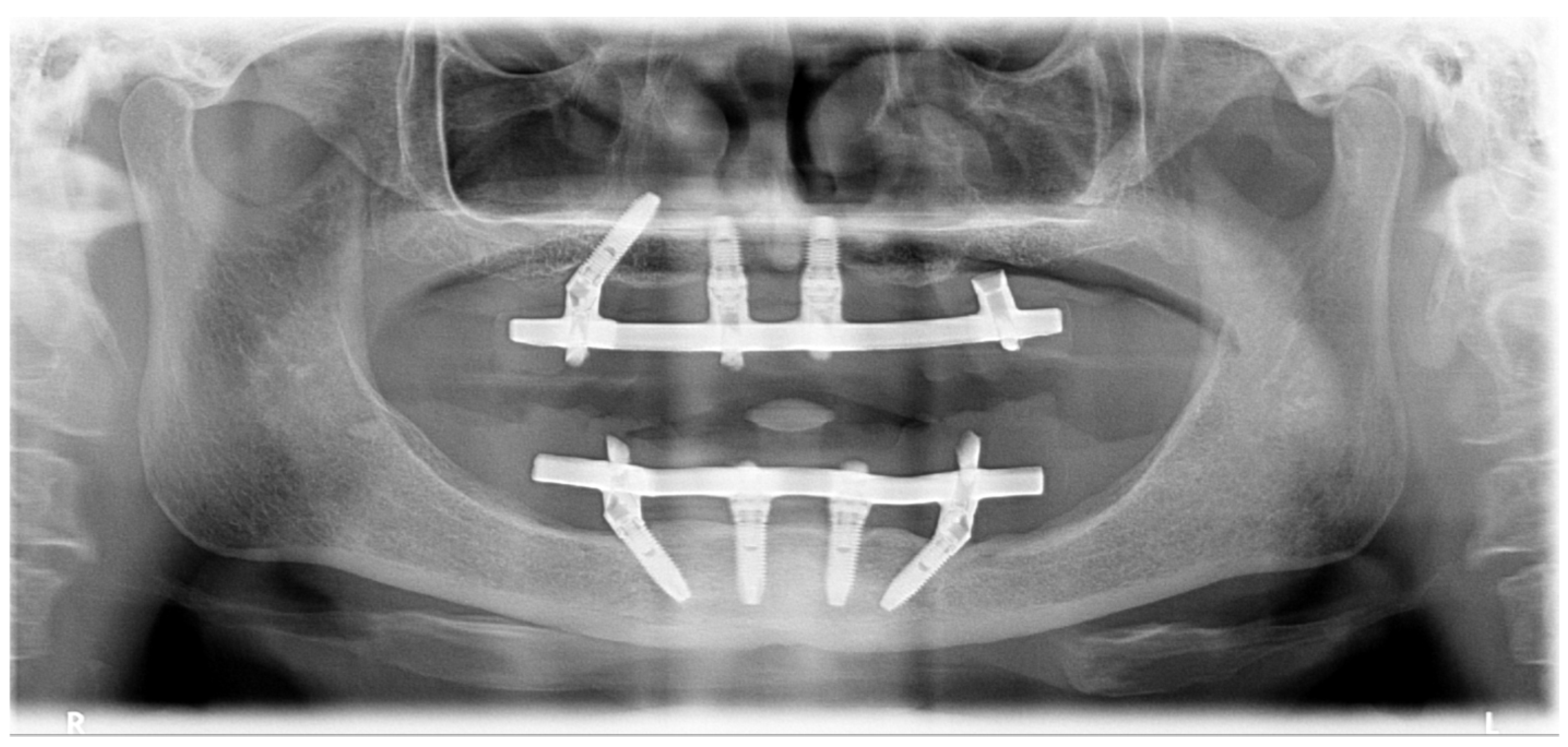
2.2. Patient 2
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Nunes, M. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5–13 years of follow-up. Clin. Implant Dent. Relat. Res. 2019, 21, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant Dent. Relat. Res. 2019, 21, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Moss, S. Extramaxillary surgical technique: Clinical outcome of 352 patients rehabilitated with 747 zygomatic implants with a follow-up between 6 months and 7 years. Clin. Implant Dent. Relat. Res. 2015, 17, e153–e162. [Google Scholar] [CrossRef] [PubMed]
- Agliardi, E.L.; Romeo, D.; Panigatti, S.; de Araújo Nobre, M.; Maló, P. Immediate full-arch rehabilitation of the severily atrophied maxilla supported by zygomatic implants: A prospective clinical study with minimum follow-up of 6 years. Int. J. Oral Maxillofac. Surg. 2017, 46, 1592–1599. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Emery, R.W. Static or dynamic navigation for implant placement—Choosing the method of guidance. J. Oral Maxillofac. Surg. 2016, 74, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Emery, R.W.; Merritt, S.A.; Lank, K.; Gibbs, J.D. Accuracy of dynamic navigation for dental implant placement-model-based evaluation. J. Oral Implantol. 2016, 42, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Emery, R.W.; Progebin, K.; Knoll, K. Dynamic image navigation—Fmplementation in the esthetic zone using a multidisciplinary approach. Implant Pract. 2016, 9, 32–38. [Google Scholar]
- Cawood, J.I.; Howell, R.A. Reconstructive preprosthetic surgery: I. Anatomical considerations. Int. J. Oral Maxillofac. Implants 1991, 20, 75–82. [Google Scholar] [CrossRef]
- Lopes, A.; Maló, P.; de Araújo Nobre, M.; Sánchez-Fernández, E.; Gravito, I. The Nobelguide® All-on-4® treatment concept for Rehabilitation of edentulous jaws: A retrospective report on the 7-years clinical and 5-years radiographic outcomes. Clin. Implant Dent. Relat. Res. 2017, 19, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Bertossi, D.; Gerosa, R.; Schembri, E.; Zanotti, G.; Rossini, N.; Colleti, G.; Rossetto, A.; Chiarini, L.; Nocini, P.F. Nobelguide™ influence in the perception of postoperative pain. Minerva Stomatol. 2013, 62, 55–63. [Google Scholar] [PubMed]
- Maló, P.; Rigolizzo, M.; de Araújo Nobre, M.; Lopes, A.; Agliardi, E. Clinical outcomes in the presence and absence of keratinized mucosa in mandibular guided implant surgeries: A pilot study with a proposal for the modification of the technique. Quintessence Int. 2013, 44, 149–157. [Google Scholar] [PubMed]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery—A review. Int. J. Oral Maxillofac. Implants 2006, 21, 305–313. [Google Scholar] [PubMed]
- Stefanelli, L.V.; de Groot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a dynamic dental implant navigation system in a private practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of implant placement with a navigation system, a laboratory guide, and freehand drilling. Int. J. Oral Maxillofac. Implants 2018, 33, 1213–1218. [Google Scholar] [CrossRef] [PubMed]
- Mediavilla Guzmán, A.; Riad Deglow, E.; Zubizarreta-Macho, A.; Agustin-Panadero, R.; Hernández-Montero, S. Accuracy of computer-aided dynamic navigation compared to computer-aided static navigation for dental implant placement: An in vitro study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef] [PubMed]
















© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes, A.; de Araújo Nobre, M.; Santos, D. The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases. J. Clin. Med. 2020, 9, 421. https://doi.org/10.3390/jcm9020421
Lopes A, de Araújo Nobre M, Santos D. The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases. Journal of Clinical Medicine. 2020; 9(2):421. https://doi.org/10.3390/jcm9020421
Chicago/Turabian StyleLopes, Armando, Miguel de Araújo Nobre, and Diogo Santos. 2020. "The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases" Journal of Clinical Medicine 9, no. 2: 421. https://doi.org/10.3390/jcm9020421
APA StyleLopes, A., de Araújo Nobre, M., & Santos, D. (2020). The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases. Journal of Clinical Medicine, 9(2), 421. https://doi.org/10.3390/jcm9020421





