Pelvic Girdle Pain, Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome: A Narrative Literature Review
Abstract
1. Introduction
2. Literature Search Method
3. Results
3.1. Epidemiology
3.2. Aetiology and Pathophysiology
3.2.1. Hypermobility-Type Ehlers-Danlos Syndrome and Hypermobility Spectrum Disorder
3.2.2. Pelvic Girdle Pain
3.3. Diagnosis
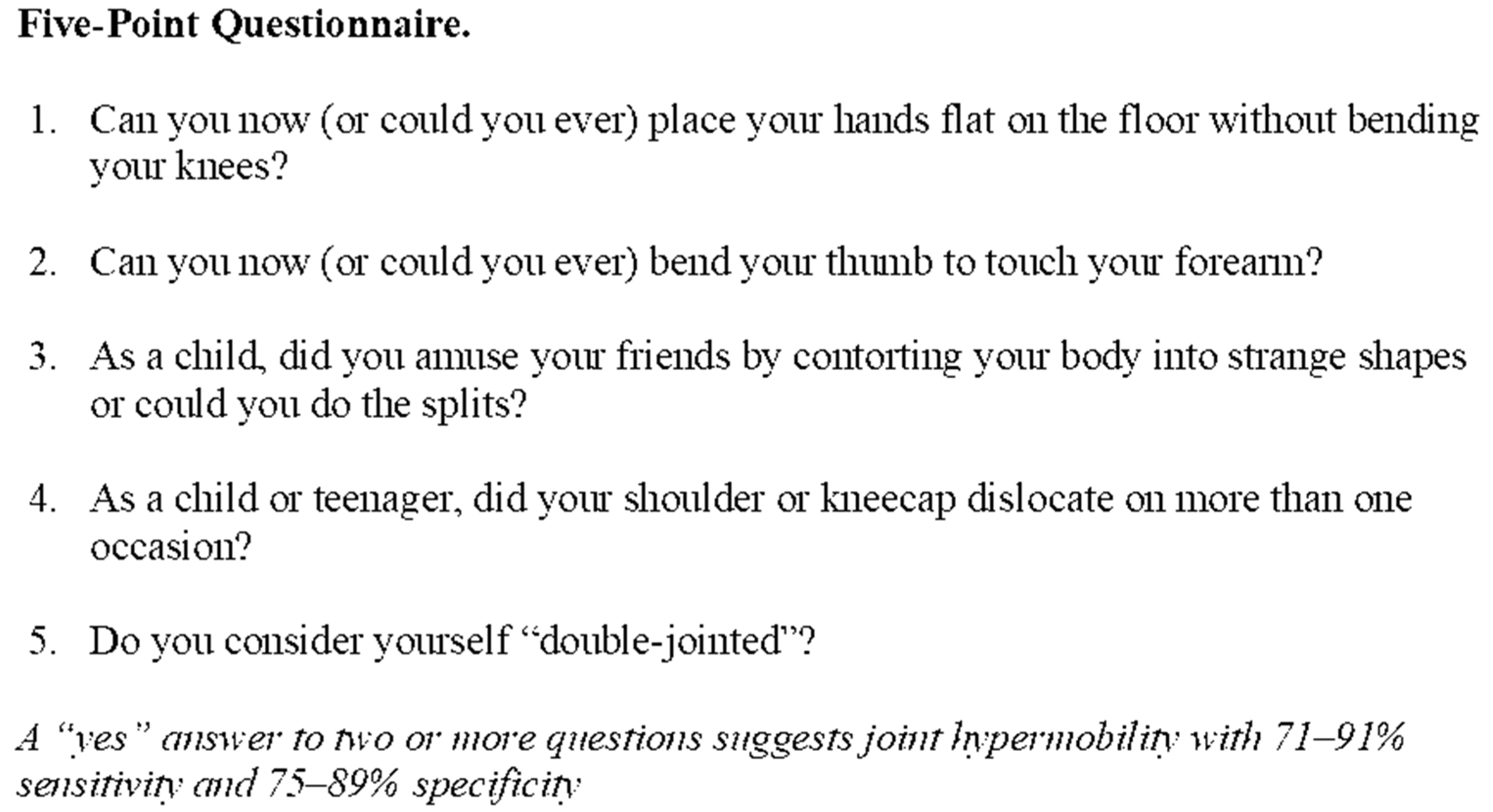
3.3.1. Joint Hypermobility
3.3.2. Hypermobility Spectrum Disorder
3.3.3. Hypermobility-Type Ehlers-Danlos Syndrome
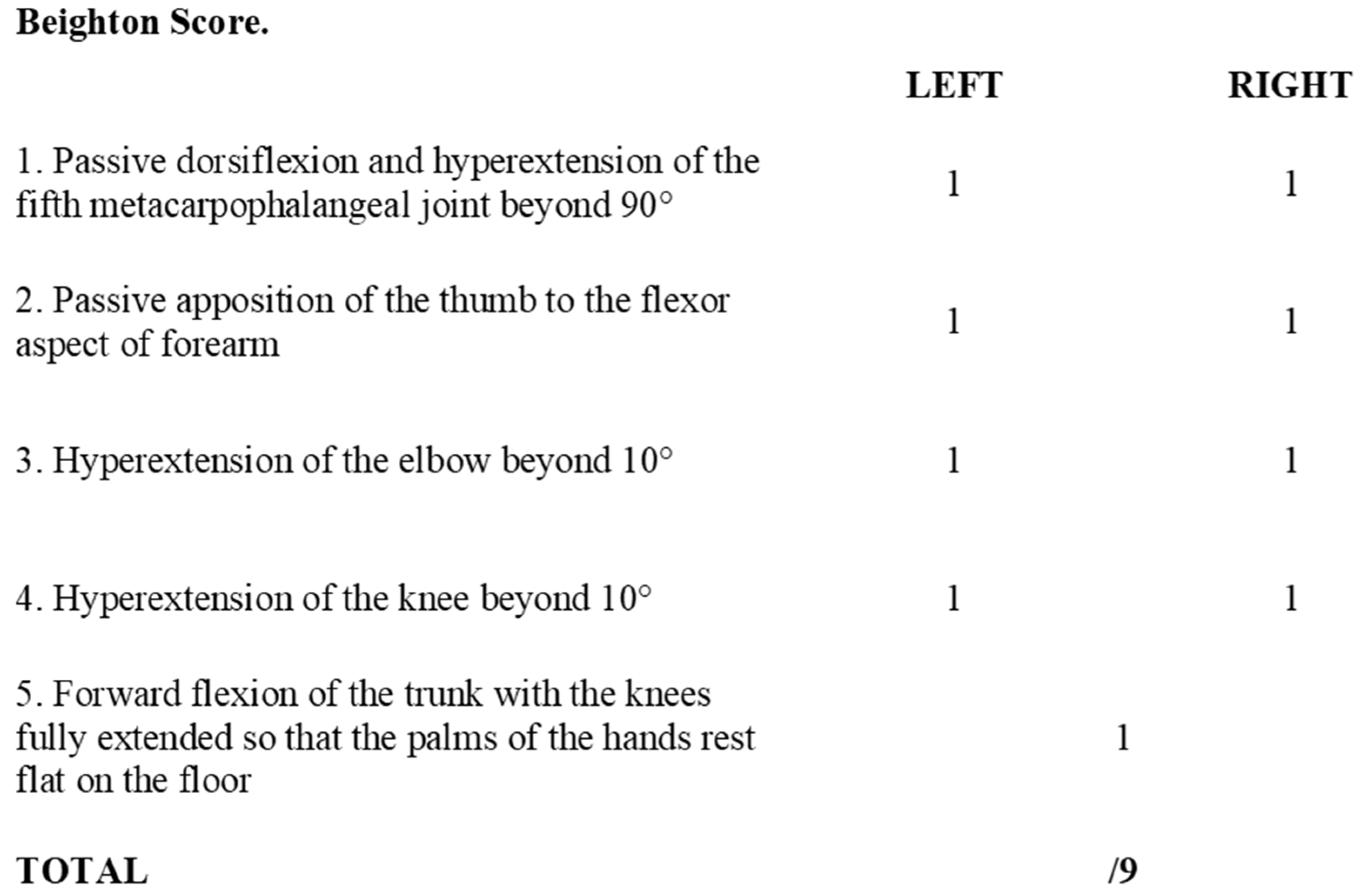
- Generalised joint hypermobility
- Diagnosed by the Beighton score (Figure 1), with cut-off score for diagnosis varying by age
- ≥6 for pre-pubertal children and adolescents
- ≥5 for pubertal men and women up to the age of 50 years
- ≥4 for those >50 years of age
- Associated features—divided into a further three subgroups A, B and C, where two or more of these subgroups are positive
- Systemic manifestations of generalised connective tissue disorder
- Positive family history, with one or more first degree relatives with hEDS
- Musculoskeletal complications associated with hypermobile joints, including pain, instability and dislocations
- Exclusion of other subtypes of EDS and other soft tissue disorders.
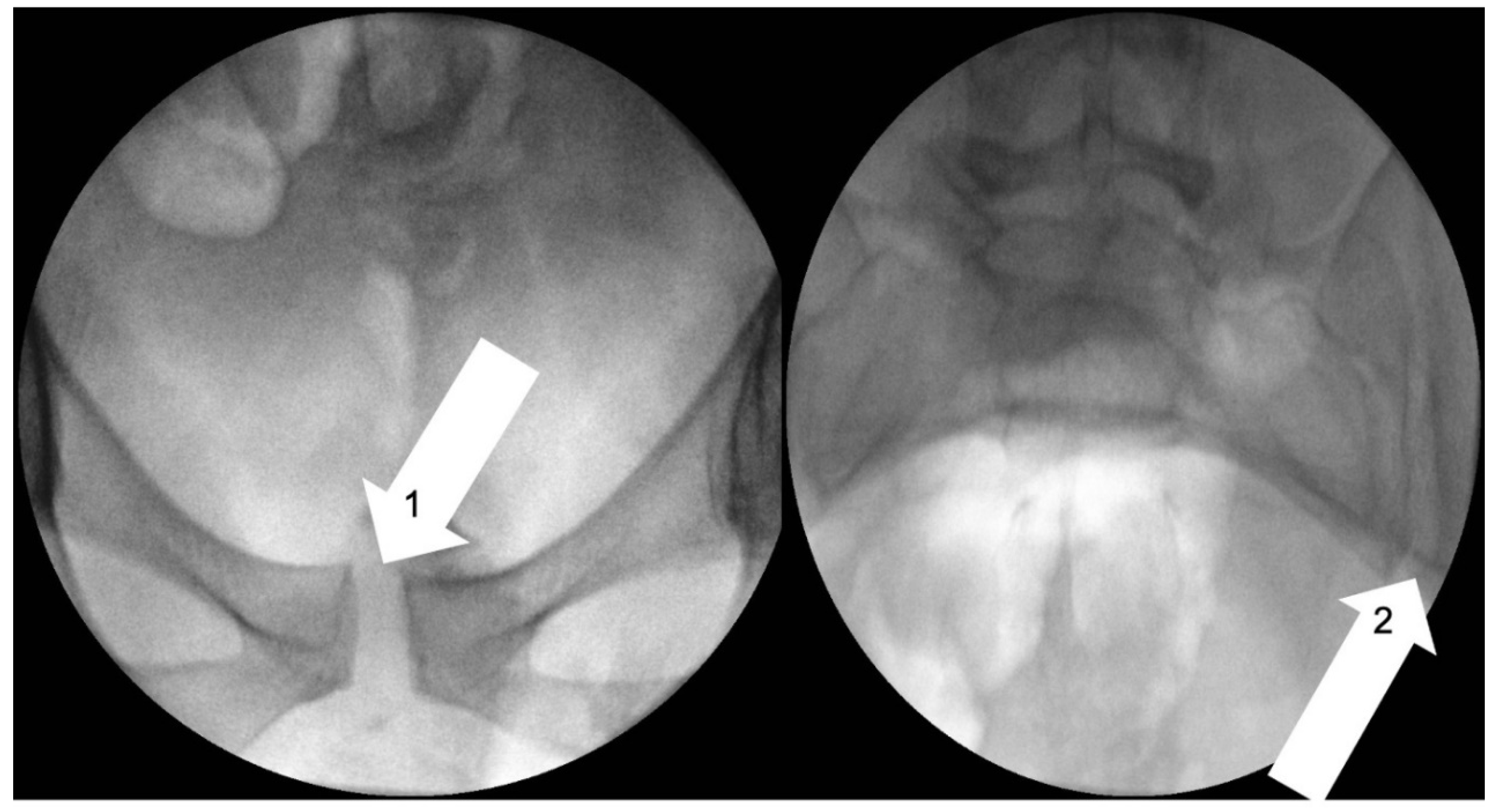
3.3.4. Pelvic Girdle Pain
3.4. Treatment
3.4.1. Analgesia
3.4.2. Mental Health
3.4.3. Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome Specialist Input
3.4.4. Non-Surgical Interventions
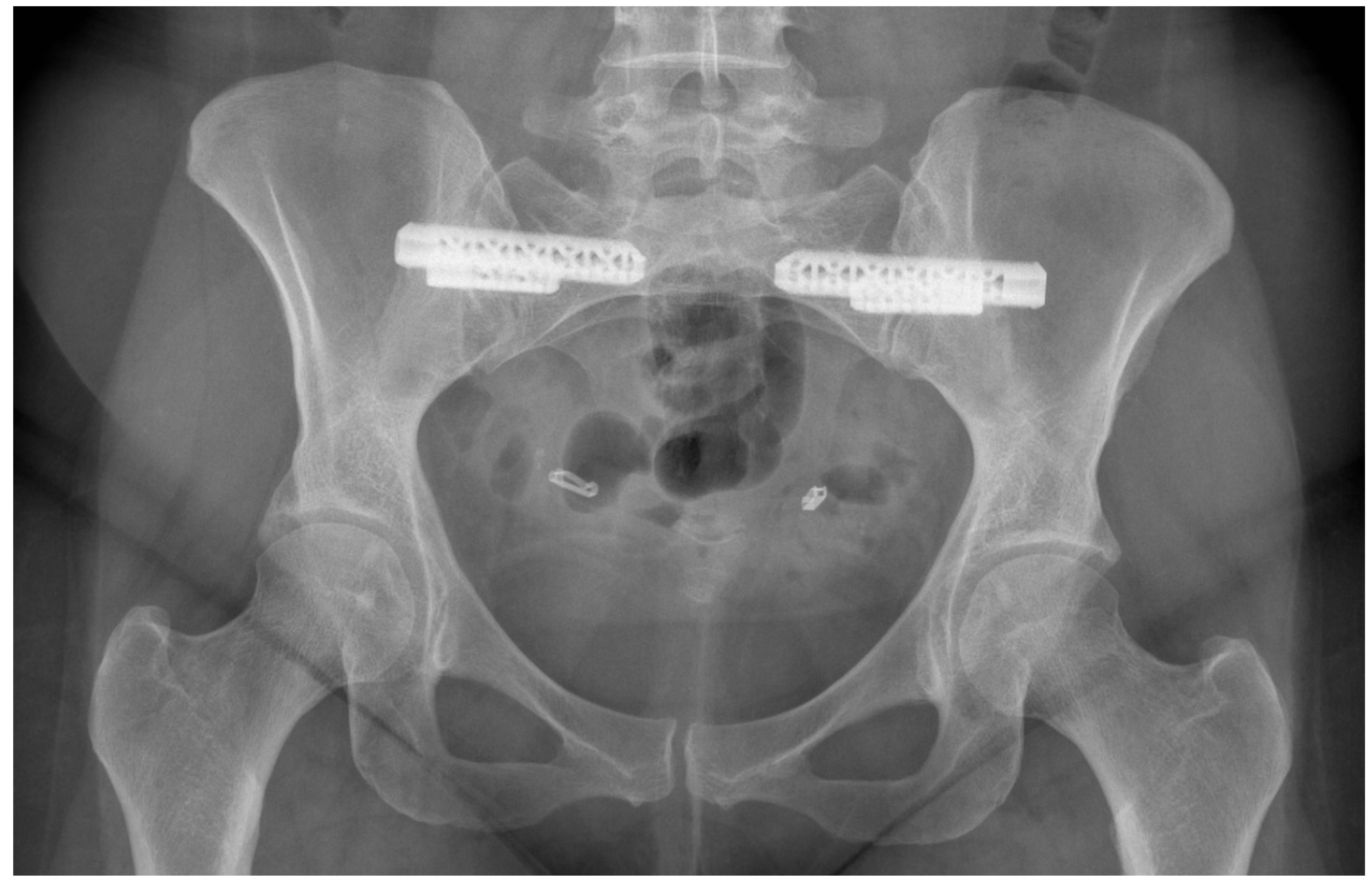
3.4.5. Surgical Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 5-PQ | Five-Point Questionnaire |
| BMI | Body Mass Index |
| CT | Computerised Tomography |
| EDS | Ehlers-Danlos Syndrome |
| EQ-5D | EuroQol 5-Dimension |
| G-HSD | Generalised Hypermobility Spectrum Disorder |
| GJH | Generalised Joint Hypermobility |
| hEDS | Hypermobility-type Ehlers-Danlos Syndrome |
| H-HSD | Historical Hypermobility Spectrum Disorder |
| HSD | Hypermobility Spectrum Disorder |
| JH | Joint Hypermobility |
| L-HSD | Localised Hypermobility Spectrum Disorder |
| LJH | Localised Joint Hypermobility |
| MRI | Magnetic Resonance Imaging |
| NICE | National Institute for Health and Care Excellence |
| ODI | Oswestry Disability Index |
| PGP | Pelvic Girdle Pain |
| P-HSD | Peripheral Hypermobility Spectrum Disorder |
| PJH | Peripheral Joint Hypermobility |
| PROMs | Patient Reported Outcome Measures |
| SF-36 | Short Form-36 |
| SIJ | Sacroiliac Joint |
| VAS | Visual Analogue Scale |
References
- Verstraete, E.; Vanderstraeten, G.; Parewijck, W. Pelvic Girdle Pain during or after Pregnancy: A review of recent evidence and a clinical care path proposal. Facts Views Vis. Obgyn. 2013, 5, 33–43. [Google Scholar]
- Kanakaris, N.K.; Roberts, C.S.; Giannoudis, P.V. Pregnancy-related pelvic girdle pain: An update. BMC Med. 2011, 9, 15. [Google Scholar] [CrossRef]
- Shirley, E.D.; DeMaio, M.; Bodurtha, J. Ehlers-Danlos Syndrome in Orthopaedics: Etiology, Diagnosis, and Treatment Implications. Sports Health 2012, 4, 394–403. [Google Scholar] [CrossRef]
- Gürer, G.; Bozbas, G.T.; Tuncer, T.; Unubol, A.I.; Ucar, U.G.; Memetoglu, O.I. Frequency of joint hypermobility in Turkish patients with knee osteoarthritis: A cross sectional multicenter study. Int. J. Rheum. Dis. 2018, 21. [Google Scholar] [CrossRef] [PubMed]
- Gullo, T.R.; Golightly, Y.M.; Flowers, P.; Jordan, J.M.; Renner, J.B.; Schwartz, T.A.; Kraus, V.B.; Hannan, M.T.; Cleveland, R.J.; Nelson, A.E. Joint hypermobility is not positively associated with prevalent multiple joint osteoarthritis: A cross-sectional study of older adults. BMC Musculoskelet. Disord. 2019, 20. [Google Scholar] [CrossRef]
- Flowers, P.P.E.; Cleveland, R.J.; Schwartz, T.A.; Nelson, A.E.; Kraus, V.B.; Hillstrom, H.J.; Goode, A.P.; Hannan, M.T.; Renner, J.B.; Jordan, J.M.; et al. Association between general joint hypermobility and knee, hip, and lumbar spine osteoarthritis by race: A cross-sectional study. Arthritis Res. Ther. 2018, 20. [Google Scholar] [CrossRef] [PubMed]
- Goode, A.P.; Cleveland, R.J.; Schwartz, T.A.; Nelson, A.E.; Kraus, V.B.; Hillstrom, H.J.; Hannan, M.T.; Flowers, P.; Renner, J.B.; Jordan, J.M.; et al. Relationship of joint hypermobility with low Back pain and lumbar spine osteoarthritis. BMC Musculoskelet. Disord. 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Dolan, A.L.; Hart, D.J.; Doyle, D.V.; Grahame, R.; Spector, T.D. The relationship of joint hypermobility, bone mineral density, and osteoarthritis in the general population: The Chingford Study. J. Rheumatol. 2003, 30, 799–803. [Google Scholar] [PubMed]
- Reinstein, E.; Pariani, M.; Lachman, R.S.; Nemec, S.; Rimoin, D.L. Early-Onset Osteoarthritis in Ehlers-Danlos Syndrome type VIII. Am. J. Med. Genet. A. 2012, 158A, 938–941. [Google Scholar] [CrossRef] [PubMed]
- Briggs, J.; McCormack, M.; Hakim, A.J.; Grahame, R. Injury and joint hypermobility syndrome in ballet dancers--a 5-year follow-up. Rheumatology 2009, 48, 1613–1614. [Google Scholar] [CrossRef] [PubMed]
- Grahame, R.; Jenkins, J.M. Joint hypermobility—Asset or liability? A study of joint mobility in ballet dancers. Ann. Rheum. Dis. 1972, 31, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Bulbena, A.; Duro, J.C.; Mateo, A.; Porta, M.; Vallejo, J. Joint hypermobility syndrome and anxiety disorders. Lancet 1988, 332, 694. [Google Scholar] [CrossRef]
- Nicholas, J.A. Injuries to knee ligaments. Relationship to looseness and tightness in football players. JAMA 1970, 212, 2236–2239. [Google Scholar] [CrossRef] [PubMed]
- Beighton, P.; Solomon, L.; Soskolne, C.L. Articular mobility in an African population. Ann. Rheum. Dis. 1973, 32, 413–418, Epub 01 September 1973. [Google Scholar] [CrossRef] [PubMed]
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A framework for the classification of joint hypermobility and related conditions. Am. J. Med Genet. Part C Semin. Med Genet. 2017, 175. [Google Scholar] [CrossRef] [PubMed]
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 International Classification of the Ehlers-Danlos Syndromes. Am. J. Med. Genet. Part C Semin. Med. Genet. 2017, 175, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Parapia, L.A.; Jackson, C. Ehlers-Danlos syndrome—A historical review. Br. J. Haematol. 2008, 141, 32–35. [Google Scholar] [CrossRef] [PubMed]
- De Wandele, I.; Rombaut, L.; Malfait, F.; De Backer, T.; De Paepe, A.; Calders, P. Clinical heterogeneity in patients with the hypermobility type of Ehlers-Danlos syndrome. Res. Dev. Disabil. 2013, 34, 873–881. [Google Scholar] [CrossRef]
- Tinkle, B.T.; Bird, H.A.; Grahame, R.; Lavallee, M.; Levy, H.P.; Sillence, D. The lack of clinical distinction between the hypermobility type of Ehlers-Danlos syndrome and the joint hypermobility syndrome (a.k.a. hypermobility syndrome). Am. J. Med. Genet. A 2009, 149a, 2368–2370. [Google Scholar] [CrossRef]
- Forghani, I. Updates in Clinical and Genetics Aspects of Hypermobile Ehlers Danlos Syndrome. Balk. Med. J. 2019, 36, 12–16. [Google Scholar] [CrossRef]
- Zoppi, N.; Chiarelli, N.; Binetti, S.; Ritelli, M.; Colombi, M. Dermal fibroblast-to-myofibroblast transition sustained by αvß3 integrin-ILK-Snail1/Slug signaling is a common feature for hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864, 1010–1023. [Google Scholar] [CrossRef] [PubMed]
- Mulvey, M.R.; Macfarlane, G.J.; Beasley, M.; Symmons, D.P.M.; Lovell, K.; Keeley, P.; Woby, S.; McBeth, J. Modest association of joint hypermobility with disabling and limiting musculoskeletal pain: Results from a large-scale general population-based survey. Arthritis Care Res. 2013, 65, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Larsson, L.G.; Baum, J.; Mudholkar, G.S. Hypermobility: Features and differential incidence between the sexes. Arthritis Rheum. 1987, 30, 1426–1430. [Google Scholar] [CrossRef] [PubMed]
- Demmler, J.C.; Atkinson, M.D.; Reinhold, E.J.; Choy, E.; Lyons, R.A.; Brophy, S.T. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: A national electronic cohort study and case–control comparison. BMJ Open 2019, 9. [Google Scholar] [CrossRef] [PubMed]
- Al-Rawi, Z.S.; Al-Aszawi, A.J.; Al-Chalabi, T. Joint mobility among university students in Iraq. Br. J. Rheumatol. 1985, 24, 326–331. [Google Scholar] [CrossRef]
- Gedalia, A.; Person, D.A.; Brewer, E.J., Jr.; Giannini, E.H. Hypermobility of the joints in juvenile episodic arthritis/arthralgia. J Pediatr. 1985, 107, 873–876. [Google Scholar] [CrossRef]
- Decoster, L.C.; Vailas, J.C.; Lindsay, R.H.; Williams, G.R. Prevalence and features of joint hypermobility among adolescent athletes. Arch. Pediatr. Adolesc. Med. 1997, 151, 989–992. [Google Scholar] [CrossRef]
- Ahlqvist, K.; Bjelland, E.K.; Pingel, R.; Schlager, A.; Nilsson-Wikmar, L.; Kristiansson, P. The Association of Self-Reported Generalized Joint Hypermobility with pelvic girdle pain during pregnancy: A retrospective cohort study. BMC Musculoskelet. Disord. 2020, 21, 474. [Google Scholar] [CrossRef]
- Lind, J.; Wallenburg, H.C. Pregnancy and the Ehlers-Danlos syndrome: A retrospective study in a Dutch population. Acta Obstet. Gynecol. Scand. 2002, 81, 293–300. [Google Scholar] [CrossRef]
- Karthikeyan, A.; Venkat-Raman, N. Hypermobile Ehlers-Danlos syndrome and pregnancy. Obstet. Med. 2018, 11, 104–109. [Google Scholar] [CrossRef]
- Van Dongen, P.W.; De Boer, M.; Lemmens, W.A.; Theron, G.B. Hypermobility and peripartum pelvic pain syndrome in pregnant South African women. Eur. J. Obstet. Gynecol. Reprod. Biol. 1999, 84, 77–82. [Google Scholar] [CrossRef]
- Mogren, I.M.; Pohjanen, A.I. Low back pain and pelvic pain during pregnancy: Prevalence and risk factors. Spine 2005, 30, 983–991. [Google Scholar] [CrossRef] [PubMed]
- Mogren, I.M. BMI, pain and hyper-mobility are determinants of long-term outcome for women with low back pain and pelvic pain during pregnancy. Eur. Spine J. 2006, 15, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Castori, M.; Morlino, S.; Celletti, C.; Celli, M.; Morrone, A.; Colombi, M.; Camerota, F.; Grammatico, P. Management of pain and fatigue in the joint hypermobility syndrome (a.k.a. Ehlers-Danlos syndrome, hypermobility type): Principles and proposal for a multidisciplinary approach. Am. J. Med. Genet. A 2012, 158a, 2055–2070. [Google Scholar] [CrossRef] [PubMed]
- Gazit, Y.; Jacob, G.; Grahame, R. Ehlers-Danlos Syndrome-Hypermobility Type: A Much Neglected Multisystemic Disorder. Rambam Maimonides Med. J. 2016, 7. [Google Scholar] [CrossRef]
- Enix, D.E.; Mayer, J.M. Sacroiliac Joint Hypermobility Biomechanics and What it Means for Health Care Providers and Patients. PM&R 2019, 11 (Suppl. 1), S32–S39. [Google Scholar] [CrossRef]
- Kiapour, A.; Joukar, A.; Elgafy, H.; Erbulut, D.U.; Agarwal, A.K.; Goel, V.K. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int. J. Spine Surg. 2020, 14 (Suppl. 1), 3–13. [Google Scholar] [CrossRef]
- Dydyk, A.M.; Forro, S.D.; Hanna, A. Sacroiliac Joint Injury. In Treasure Island (FL); StatPearls Publishing LLC: St. Petersburg, FL, USA, 2020. [Google Scholar]
- Hastings, J.; Forster, J.E.; Witzeman, K. Joint Hypermobility among Female Patients Presenting with Chronic Myofascial Pelvic Pain. PM&R 2019, 11, 1193–1199. [Google Scholar] [CrossRef]
- Joukar, A.; Shah, A.; Kiapour, A.; Vosoughi, A.S.; Duhon, B.; Agarwal, A.K.; Elgafy, H.; Ebraheim, N.; Goel, V.K. Sex Specific Sacroiliac Joint Biomechanics During Standing Upright: A Finite Element Study. Spine 2018, 43, E1053–E1060. [Google Scholar] [CrossRef]
- Pyeritz, R. Ehlers-Danlos syndromes. In Cecil Textbook of Medicine, 21st ed.; Goldman, L., Bennett, J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2000; Volume 1. [Google Scholar]
- Tinkle, B.; Castori, M.; Berglund, B.; Cohen, H.; Grahame, R.; Kazkaz, H.; Levy, H. Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome Type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 48–69. [Google Scholar] [CrossRef]
- Remvig, L.; Jensen, D.V.; Ward, R.C. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: Review of the literature. J. Rheumatol. 2007, 34, 804–809. [Google Scholar] [PubMed]
- Russek, L.N.; Errico, D.M. Prevalence, injury rate and, symptom frequency in generalized joint laxity and joint hypermobility syndrome in a “healthy” college population. Clin. Rheumatol. 2016, 35, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Seçkin, U.; Tur, B.S.; Yilmaz, O.; Yağci, I.; Bodur, H.; Arasil, T. The prevalence of joint hypermobility among high school students. Rheumatol. Int. 2005, 25, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Van der Giessen, L.J.; Liekens, D.; Rutgers, K.J.; Hartman, A.; Mulder, P.G.; Oranje, A.P. Validation of beighton score and prevalence of connective tissue signs in 773 Dutch children. J. Rheumatol. 2001, 28, 2726–2730. [Google Scholar] [PubMed]
- Kovacs, F.M.; Garcia, E.; Royuela, A.; González, L.; Abraira, V. Prevalence and factors associated with low back pain and pelvic girdle pain during pregnancy: A multicenter study conducted in the Spanish National Health Service. Spine 2012, 37. [Google Scholar] [CrossRef] [PubMed]
- Albert, H.B.; Godskesen, M.; Westergaard, J.G. Incidence of four syndromes of pregnancy-related pelvic joint pain. Spine 2002, 27, 2831–2834. [Google Scholar] [CrossRef] [PubMed]
- Albert, H.; Godskesen, M.; Westergaard, J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet. Gynecol. Scand. 2001, 80, 505–510. [Google Scholar]
- Elden, H.; Gutke, A.; Kjellby-Wendt, G.; Fagevik-Olsen, M.; Ostgaard, H.C. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: A longitudinal follow-up study. BMC Musculoskelet. Disord. 2016, 17, 276. [Google Scholar] [CrossRef]
- Zweers, M.C.; Bristow, J.; Steijlen, P.M.; Dean, W.B.; Hamel, B.C.; Otero, M.; Kucharekova, M.; Boezeman, J.B.; Schalkwijk, J. Haploinsufficiency of TNXB is associated with hypermobility type of Ehlers-Danlos syndrome. Am. J. Hum. Genet. 2003, 73, 214–217. [Google Scholar] [CrossRef]
- Morissette, R.; Chen, W.; Perritt, A.F.; Dreiling, J.L.; Arai, A.E.; Sachdev, V.; Hannoush, H.; Mallappa, A.; Xu, Z.; McDonnell, N.B.; et al. Broadening the Spectrum of Ehlers Danlos Syndrome in Patients with Congenital Adrenal Hyperplasia. J. Clin. Endocrinol. Metab. 2015, 100, E1143–E1152. [Google Scholar] [CrossRef]
- Syx, D.; Symoens, S.; Steyaert, W.; De Paepe, A.; Coucke, P.J.; Malfait, F. Ehlers-Danlos Syndrome, Hypermobility Type, Is Linked to Chromosome 8p22-8p21.1 in an Extended Belgian Family. Dis. Markers 2015, 2015, 828970. [Google Scholar] [CrossRef] [PubMed]
- Russek, L.N. Hypermobility syndrome. Phys. Ther. 1999, 79, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Hakim, A.J.; Cherkas, L.F.; Grahame, R.; Spector, T.D.; MacGregor, A.J. The genetic epidemiology of joint hypermobility: A population study of female twins. Arthritis Rheum. 2004, 50, 2640–2644. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, A.; Milosavljevic, S.; Woodley, S.; Sole, G. Effects of external pelvic compression on form closure, force closure, and neuromotor control of the lumbopelvic spine—A systematic review. Man. Ther. 2012, 17, 275–284. [Google Scholar] [CrossRef]
- Beales, D.J.; O’Sullivan, P.B.; Briffa, N.K. The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pelvic girdle pain subjects. Man. Ther. 2010, 15, 190–199. [Google Scholar] [CrossRef]
- Garras, D.N.; Carothers, J.T.; Olson, S.A. Single-leg-stance (flamingo) radiographs to assess pelvic instability: How much motion is normal? J. Bone Joint Surg. Am. 2008, 90, 2114–2118. [Google Scholar] [CrossRef] [PubMed]
- Kumar, B.; Lenert, P. Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. Am. J. Med. 2017, 130. [Google Scholar] [CrossRef]
- Sahin, N.; Baskent, A.; Ugurlu, H.; Berker, E. Isokinetic evaluation of knee extensor/flexor muscle strength in patients with hypermobility syndrome. Rheumatol. Int. 2008, 28, 643–648. [Google Scholar] [CrossRef]
- Wolf, J.M.; Cameron, K.L.; Owens, B.D. Impact of joint laxity and hypermobility on the musculoskeletal system. J. Am. Acad. Orthop. Surg. 2011, 19, 463–471. [Google Scholar] [CrossRef]
- Toprak Celenay, S.; Ozer Kaya, D. Effects of spinal stabilization exercises in women with benign joint hypermobility syndrome: A randomized controlled trial. Rheumatol. Int. 2017, 37, 1461–1468. [Google Scholar] [CrossRef]
- Jain, S.; Jamjute, P.; Eedarapalli, P.; Sawdy, R. Symphysis pubis dysfunction: A practical approach to management. Obstet. Gynaecol. 2006, 8. [Google Scholar] [CrossRef]
- Björklund, K.; Bergström, S.; Nordström, M.-L.; Ulmsten, U. Symphyseal distention in relation to serum relaxin levels and pelvic pain in pregnancy. Acta Obstet. Gynecol. Scand. 2000, 79, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Hakim, A.J.; Grahame, R. A simple questionnaire to detect hypermobility: An adjunct to the assessment of patients with diffuse musculoskeletal pain. Int. J. Clin. Pract. 2003, 57, 163–166. [Google Scholar] [PubMed]
- Glans, M.; Humble, M.B.; Elwin, M.; Bejerot, S. Self-rated joint hypermobility: The five-part questionnaire evaluated in a Swedish non-clinical adult population. BMC Musculoskelet. Disord. 2020, 21, 174. [Google Scholar] [CrossRef] [PubMed]
- Moraes, D.A.; Baptista, C.A.; Crippa, J.A.; Louzada-Junior, P. Translation into Brazilian Portuguese and validation of the five-part questionnaire for identifying hypermobility. Rev. Bras. Reumatol. 2011, 51, 53–69, Epub 18 March 2011. [Google Scholar] [CrossRef]
- Vleeming, A.; Albert, H.B.; Östgaard, H.C.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef]
- Ando, F.; Ohashi, K. Using the posterior pelvic pain provocation test in pregnant Japanese women. Nurs. Health Sci. 2009, 11, 3–9. [Google Scholar] [CrossRef]
- Mens, J.M.; Vleeming, A.; Snijders, C.J.; Ronchetti, I.; Stam, H.J. Reliability and validity of hip adduction strength to measure disease severity in posterior pelvic pain since pregnancy. Spine 2002, 27, 1674–1679. [Google Scholar] [CrossRef]
- Ostgaard, H.C.; Zetherström, G.; Roos-Hansson, E. The posterior pelvic pain provocation test in pregnant women. Eur. Spine J. 1994, 3, 258–260. [Google Scholar] [CrossRef]
- Puhakka, K.B.; Jurik, A.G.; Egund, N.; Schiottzchristensen, B.; Stengaardpedersen, K.; Hansen, G.V.O.; Christiansen, J.V. Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol. 2003, 44, 218–229. [Google Scholar] [CrossRef]
- Udoji, M.A.; Ness, T.J. New directions in the treatment of pelvic pain. Pain Manag. 2013, 3, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Siqueira-Campos, V.M.E.; Da Luz, R.A.; De Deus, J.M.; Martinez, E.Z.; Conde, D.M. Anxiety and depression in women with and without chronic pelvic pain: Prevalence and associated factors. J. Pain Res. 2019, 12, 1223–1233. [Google Scholar] [CrossRef] [PubMed]
- Ayorinde, A.A.; Bhattacharya, S.; Druce, K.L.; Jones, G.T.; Macfarlane, G.J. Chronic pelvic pain in women of reproductive and post-reproductive age: A population-based study. Eur. J. Pain. 2017, 21, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Miller-Matero, L.R.; Saulino, C.; Clark, S.; Bugenski, M.; Eshelman, A.; Eisenstein, D. When treating the pain is not enough: A multidisciplinary approach for chronic pelvic pain. Arch. Womens Ment. Health 2016, 19, 349–354. [Google Scholar] [CrossRef]
- Bryant, C.; Cockburn, R.; Plante, A.F.; Chia, A. The psychological profile of women presenting to a multidisciplinary clinic for chronic pelvic pain: High levels of psychological dysfunction and implications for practice. J. Pain Res. 2016, 9, 1049–1056. [Google Scholar] [CrossRef] [PubMed]
- Alappattu, M.J.; Bishop, M.D. Psychological factors in chronic pelvic pain in women: Relevance and application of the fear-avoidance model of pain. Phys. Ther. 2011, 91, 1542–1550, Epub 13 August 2011. [Google Scholar] [CrossRef] [PubMed]
- Rashidi Fakari, F.; Simbar, M.; Saei Ghare Naz, M. The Relationship between Fear-Avoidance Beliefs and Pain in Pregnant Women with Pelvic Girdle Pain: A Cross-Sectional Study. Int. J. Community Based Nurs. Midwifery 2018, 6, 305–313. [Google Scholar]
- Mackenzie, J.; Murray, E.; Lusher, J. Women’s experiences of pregnancy related pelvic girdle pain: A systematic review. Midwifery 2018, 56, 102–111. [Google Scholar] [CrossRef]
- Bjelland, E.K.; Stuge, B.; Engdahl, B.; Eberhard-Gran, M. The effect of emotional distress on persistent pelvic girdle pain after delivery: A longitudinal population study. BJOG 2013, 120, 32–40. [Google Scholar] [CrossRef]
- Gutke, A.; Josefsson, A.; Oberg, B. Pelvic girdle pain and lumbar pain in relation to postpartum depressive symptoms. Spine 2007, 32, 1430–1436. [Google Scholar] [CrossRef]
- Sobey, G. Ehlers-Danlos syndrome: How to diagnose and when to perform genetic tests. Arch. Dis. Child. 2015, 100, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Rewari, A.; Shanthanna, H. Management of chronic pain in Ehlers-Danlos syndrome: Two case reports and a review of literature. Medicine 2018, 97, e13115. [Google Scholar] [CrossRef] [PubMed]
- Bathen, T.; Hångmann, A.B.; Hoff, M.; Andersen, L.; Rand-Hendriksen, S. Multidisciplinary treatment of disability in ehlers-danlos syndrome hypermobility type/hypermobility syndrome: A pilot study using a combination of physical and cognitive-behavioral therapy on 12 women. Am. J. Med. Genet. A 2013, 161a, 3005–3011. [Google Scholar] [CrossRef] [PubMed]
- Castori, M. Ehlers-danlos syndrome, hypermobility type: An underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol. 2012, 2012, 751768. [Google Scholar] [CrossRef] [PubMed]
- Gausel, A.M.; Malmqvist, S.; Andersen, K.; Kjærmann, I.; Larsen, J.P.; Dalen, I.; Økland, I. Subjective recovery from pregnancy-related pelvic girdle pain the first 6 weeks after delivery: A prospective longitudinal cohort study. Eur. Spine J. 2020, 29, 556–563. [Google Scholar] [CrossRef]
- Vural, M. Pelvic pain rehabilitation. Turk. J. Phys. Med. Rehabil. 2018, 64, 291–299. [Google Scholar] [CrossRef]
- Al-Subahi, M.; Alayat, M.S.M.; AlShehri, M.A.; Helal, O.; Alhasan, H.; Alalawi, A.; Takrouni, A.; Alfaqeh, A. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: A systematic review. J. Phys. Ther. Sci. 2017, 29, 1689–1694. [Google Scholar] [CrossRef]
- Marreiros, S.S.P.; Riskowski, J.L.; Steultjens, M.P. 287° Proprioception and Laxity in Patients with Joint Hypermobility Syndrome with and without Knee Instability. Rheumatology 2016, 55 (Suppl. 1), i178–i179. [Google Scholar] [CrossRef][Green Version]
- Scholten, P.M.; Patel, S.I.; Christos, P.J.; Singh, J.R. Short-term efficacy of sacroiliac joint corticosteroid injection based on arthrographic contrast patterns. PM&R 2015, 7, 385–391. [Google Scholar] [CrossRef]
- Via, A.G.; Frizziero, A.; Finotti, P.; Oliva, F.; Randelli, F.; Maffulli, N. Management of osteitis pubis in athletes: Rehabilitation and return to training—A review of the most recent literature. Open Access J. Sports Med. 2019, 10, 1–10. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Psarakis, S.; Kanakaris, N.K.; Pape, H.C. Biological enhancement of bone healing with Bone Morphogenetic Protein-7 at the clinical setting of pelvic girdle non-unions. Injury 2007, 38 (Suppl. 4), S43–S48. [Google Scholar] [CrossRef]
- Belanger, T.A.; Dall, B.E. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: A new technique. J. Spinal Disord. 2001, 14, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Van Zwienen, C.M.; Van den Bosch, E.W.; Snijders, C.J.; Van Vugt, A.B. Triple pelvic ring fixation in patients with severe pregnancy-related low back and pelvic pain. Spine 2004, 29, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Kibsgård, T.J.; Røise, O.; Sudmann, E.; Stuge, B. Pelvic joint fusions in patients with chronic pelvic girdle pain: A 23-year follow-up. Eur. Spine J. 2013, 22, 871–877. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kibsgård, T.J.; Røise, O.; Stuge, B. Pelvic joint fusion in patients with severe pelvic girdle pain—A prospective single-subject research design study. BMC Musculoskelet. Disord. 2014, 15, 85. [Google Scholar] [CrossRef] [PubMed]
- Giannikas, K.A.; Khan, A.M.; Karski, M.T.; Maxwell, H.A. Sacroiliac joint fusion for chronic pain: A simple technique avoiding the use of metalwork. Eur. Spine J. 2004, 13, 253–256. [Google Scholar] [CrossRef]
- Dale, M.; Evans, J.; Carter, K.; O’Connell, S.; Morgan, H.; Carolan-Rees, G. iFuse Implant System for Treating Chronic Sacroiliac Joint Pain: A NICE Medical Technology Guidance. Appl. Health Econ. Health Policy 2020, 18, 363–373. [Google Scholar] [CrossRef]
- Mehin, R.; Meek, R.; O’Brien, P.; Blachut, P. Surgery for osteitis pubis. Can. J. Surg. 2006, 49, 170–176. [Google Scholar]
- Giannoudis, P.V.; Kanakaris, N.K. Pubic Symphysis Fusion. In Practical Procedures in Elective Orthopaedic Surgery: Pelvis and Lower Extremity; Giannoudis, P.V., Ed.; Springer: London, UK, 2012; pp. 23–28. [Google Scholar]
- Smith-Petersen, M.N. Arthrodesis of the Sacroiliac Joint. A New Method of Approach. JBJS 1921, 3, 400–405. [Google Scholar]
- Engle, C.P.; Gruen, G.S. Anterior fixation of the sacroiliac joint. Oper. Tech. Orthop. 1993, 3, 26–34. [Google Scholar] [CrossRef]
- Smith, A.G.; Capobianco, R.; Cher, D.; Rudolf, L.; Sachs, D.; Gundanna, M.; Kleiner, J.; Mody, M.G.; Shamie, A.N. Open versus minimally invasive sacroiliac joint fusion: A multi-center comparison of perioperative measures and clinical outcomes. Ann. Surg. Innov. Res. 2013, 7, 14. [Google Scholar] [CrossRef]
- Rudolf, L. Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: Report of the First 50 Patients and Outcomes. Open Orthop. J. 2012, 6, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.T.; Haase, L.; Lender, P.A.; Polly, D.W. Minimally Invasive Sacroiliac Joint Fusion: The Current Evidence. Int. J. Spine Surg. 2020, 14 (Suppl. 1), 20–29. [Google Scholar] [CrossRef] [PubMed]
- Dengler, J.; Kools, D.; Pflugmacher, R.; Gasbarrini, A.; Prestamburgo, D.; Gaetani, P.; Cher, D.; Van Eeckhoven, E.; Annertz, M.; Sturesson, B. Randomized Trial of Sacroiliac Joint Arthrodesis Compared with Conservative Management for Chronic Low Back Pain Attributed to the Sacroiliac Joint. J. Bone Joint Surg. Am. 2019, 101, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Lorio, M.P.; Polly, D.W., Jr.; Ninkovic, I.; Ledonio, C.G.; Hallas, K.; Andersson, G. Utilization of Minimally Invasive Surgical Approach for Sacroiliac Joint Fusion in Surgeon Population of ISASS and SMISS Membership. Open Orthop. J. 2014, 8, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Hechtman, K.S.; Zvijac, J.E.; Popkin, C.A.; Zych, G.A.; Botto-van Bemden, A. A minimally disruptive surgical technique for the treatment of osteitis pubis in athletes. Sports Health 2010, 2, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Kanakaris, N.K.; Mallina, R.; Calori, G.M.; Kontakis, G.; Giannoudis, P.V. Use of bone morphogenetic proteins in arthrodesis: Clinical results. Injury 2009, 40 (Suppl. 3), S62–S66. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Tzioupis, C. Clinical applications of BMP-7: The UK perspective. Injury 2005, 36 (Suppl. 3), S47–S50. [Google Scholar] [CrossRef]
- Jaya Sanapati, M.D.; Laxmaiah Manchikanti, M.D.; Sairam Atluri, M.D.; Sheldon Jordan, M.D. Do Regenerative Medicine Therapies Provide Long-Term Relief in Chronic Low Back Pain: A Systematic Review and Metaanalysis. Pain Physician 2018, 21, 515–540. [Google Scholar]
- Wuytack, F.; O’Donovan, M. Outcomes and outcomes measurements used in intervention studies of pelvic girdle pain and lumbopelvic pain: A systematic review. Chiropr. Man. Ther. 2019, 27, 62. [Google Scholar] [CrossRef]
- Banierink, H.; Ten Duis, K.; Wendt, K.; Heineman, E.; Ijpma, F.; Reininga, I. Patient-reported physical functioning and quality of life after pelvic ring injury: A systematic review of the literature. PLoS ONE 2020, 15, e0233226. [Google Scholar] [CrossRef] [PubMed]
- Stuge, B.; Garratt, A.; Krogstad Jenssen, H.; Grotle, M. The pelvic girdle questionnaire: A condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. Phys. Ther. 2011, 91, 1096–1108. [Google Scholar] [CrossRef] [PubMed]
- Majeed, S.A. Grading the outcome of pelvic fractures. J. Bone Joint Surg. Br. 1989, 71, 304–306. [Google Scholar] [CrossRef] [PubMed]
- Nepola, J.V.; Trenhaile, S.W.; Miranda, M.A.; Butterfield, S.L.; Fredericks, D.C.; Riemer, B.L. Vertical shear injuries: Is there a relationship between residual displacement and functional outcome? J. Trauma 1999, 46, 1024–1029; discussion 9–30. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.D.; Blum, D.A.; Ansel, L.J. Outcome after fixation of unstable posterior pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 160–179. [Google Scholar] [CrossRef] [PubMed]
- Lefaivre, K.A.; Slobogean, G.P.; Ngai, J.T.; Broekhuyse, H.M.; O’Brien, P.J. What outcomes are important for patients after pelvic trauma? Subjective responses and psychometric analysis of three published pelvic-specific outcome instruments. J. Orthop. Trauma 2014, 28, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Bajada, S.; Mohanty, K. Psychometric properties including reliability, validity and responsiveness of the Majeed pelvic score in patients with chronic sacroiliac joint pain. Eur. Spine J. 2016, 25, 1939–1944. [Google Scholar] [CrossRef] [PubMed]
- Rejano-Campo, M.; Ferrer-Peña, R.; Urraca-Gesto, M.A.; Gallego-Izquierdo, T.; Pecos-Martín, D.; Stuge, B.; Plaza-Manzano, G. Transcultural adaptation and psychometric validation of a Spanish-language version of the “Pelvic Girdle Questionnaire”. Health Qual Life Outcomes 2017, 15, 30. [Google Scholar] [CrossRef]
- Grotle, M.; Garratt, A.M.; Krogstad Jenssen, H.; Stuge, B. Reliability and construct validity of self-report questionnaires for patients with pelvic girdle pain. Phys. Ther. 2012, 92, 111–123, Epub 22 October 2011. [Google Scholar] [CrossRef]
- Rashidi Fakari, F.; Kariman, N.; Ozgoli, G.; Ghare Naz, M.S.; Ghasemi, V.; Ebadi, A. Iranian version of Pelvic Girdle Questionnaire: Psychometric properties and cultural adaptation. J. Res. Med. Sci. 2019, 24, 43. [Google Scholar] [CrossRef]
- Fagundes, F.M.L.; Cabral, C.M.N. Cross-cultural adaptation of the Pelvic Girdle Questionnaire (PGQ) into Brazilian Portuguese and clinimetric testing of the PGQ and Roland Morris questionnaire in pregnancy pelvic pain. Braz. J. Phys. Ther. 2019, 23, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Starzec, M.; Truszczyńska-Baszak, A.; Stuge, B.; Tarnowski, A.; Rongies, W. Cross-cultural Adaptation of the Pelvic Girdle Questionnaire for the Polish Population. J. Manip. Physiol. Ther. 2018, 41, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Gutke, A.; Stuge, B.; Elden, H.; Sandell, C.; Asplin, G.; Fagevik Olsén, M. The Swedish version of the pelvic girdle questionnaire, cross-cultural adaptation and validation. Disabil. Rehabil. 2020, 42, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Acharya, R.; Tveter, A.T.; Grotle, M.; Khadgi, B.; Koju, R.; Eberhard-Gran, M.; Stuge, B. Cross-Cultural Adaptation and Validation of the Nepali Version of the Pelvic Girdle Questionnaire. J. Manip. Physiol. Ther. 2020. [Google Scholar] [CrossRef]
- Lefaivre, K.A.; Slobogean, G.P.; Valeriote, J.; O’Brien, P.J.; Macadam, S.A. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: A systematic review. J. Bone Joint Surg. Br. 2012, 94, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Copay, A.G.; Cher, D.J. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual. Life Res. 2016, 25, 283–292. [Google Scholar] [CrossRef] [PubMed]



| Asymptomatic Generalised Joint Hypermobility (Asymptomatic GJH) |
| Asymptomatic Peripheral Joint Hypermobility (Asymptomatic PJH) |
| Asymptomatic Localised Joint Hypermobility (Asymptomatic LJH) |
| Generalised Hypermobility Spectrum Disorder (G-HSD) |
| Peripheral Hypermobility Spectrum Disorder (P-HSD) |
| Localised Hypermobility Spectrum Disorder (L-HSD) |
| Historical Hypermobility Spectrum Disorder (H-HSD) |
| Hypermobility-Type Ehlers-Danlos Syndrome (hEDS) |
| EDS Subtype | Inheritance Pattern | Genetic Basis | Protein Affected | Common Clinical Signs (Not Extensive) |
|---|---|---|---|---|
| Classical EDS | Autosomal dominant | COL5A1 | Type V collagen | Skin: hyperextensible, fragile, soft, atrophic scarring |
| COL1A1 | Type I collagen | Other: generalised-JH, hernias | ||
| Classical-like EDS | Autosomal recessive | TNXB | Tenascin XB | Skin: hyperextensible, velvety, absence of atrophic scarring, easy bruising skin |
| Other: generalised-JH, foot deformities, oedema, pelvic organ prolapse | ||||
| Cardiac-Valvular EDS | Autosomal recessive | COL1A2 | Type I collagen | Progressive cardiac valve disease |
| Skin: hyperextensible, atrophic scars, easy bruising | ||||
| Other: Joint hypermobility, hernia, foot deformity | ||||
| Vascular EDS | Autosomal dominant | COL3A1 | Type III collagen | Arterial rupture at young age, spontaneous sigmoid colon perforation, uterine rupture, peripartum perineal tears, carotid-cavernous sinus fistula, thin skin, varicose vein |
| COL1A1 | Type I collagen | |||
| Hypermobile EDS | Autosomal dominant | Unknown | Unknown | Generalised-JH, absence of skin fragility, mild skin hyperextensibility, unexplained striae, pelvic organ prolapse, dental crowding, hernias |
| Article Title | Publication Year | First Author | Journal | Article Type | Relevance |
|---|---|---|---|---|---|
| Hypermobility and peripartum pelvic pain syndrome in pregnant South African women [31] | 1999 | Van Dongen, PW | International Journal of Gynecology & Obstetrics | Cross-Sectional Study | This study included 509 South African pregnant women, of which only 4.9% suffered from hypermobility (Beighton score ≥5/9). No significant correlation was determined between peripartum pelvic pain and hypermobility. Only 20 cases of peripartum pelvic pain were recorded in the entire study population. There is no mention of JH prevalence in these 20 patients with pelvic pain. |
| Low back pain and pelvic pain during pregnancy: prevalence and risk factors [32] | 2005 | Mogren, IM | Spine | Cross-Sectional Study | Identified that women with diagnosed hypermobility were at 1.79 times the odds (95% confidence interval 1.14–2.80) of developing low back and pelvic pain during pregnancy compared to those with normal joints (p = 0.012). Did not differentiate between low back pain and pelvic pain. |
| Body mass index (BMI), pain and hyper-mobility are determinants of long-term outcome for women with low back pain and pelvic pain during pregnancy [33] | 2006 | Mogren, IM | European Spine Journal | Cross-Sectional Study | Identified that women with diagnosed hypermobility were not at increased risk of low back and pelvic pain 6-months postpartum (p = 0.123). Grouping of women with diagnosed hypermobility and whose who perceived themselves to be hypermobile found statistical significance in increased risk of low back and pelvic pain 6-month postpartum (p = 0.042), odds ratio 1.56 (95% confidence interval 1.01–2.40). |
| Management of pain and fatigue in the joint hypermobility syndrome (a.k.a. Ehlers-Danlos syndrome, hypermobility type): principles and proposal for a multidisciplinary approach [34] | 2012 | Castori, M | American Journal of Medical Genetics Part A | Literature Review | Mentions pelvic ring instability are likely more common in hypermobility spectrum disorder (HSD). Also states trunk stabilisation as treatment but is usually ineffective due to high risk of instability recurrence. |
| Ehlers-Danlos Syndrome-Hypermobility Type: A Much Neglected Multisystemic Disorder [35] | 2016 | Gazit, Y | Rambam Maimonides Medical Journal | Literature Review | Discusses increase in joint laxity and pain during pregnancy. Pelvic pain management is discussed in the form of pelvic belts, crutches and bed rest. Mentions women with Ehlers-Danlos Syndrome, mainly hypermobility subtype, are more likely to suffer from pelvic pain and instability (26%) compared to those without the condition (7%), p < 0.05 [29]. |
| Joint Hypermobility among Female Patients Presenting with Chronic Myofascial Pelvic Pain [39] | 2019 | Hastings, J | PM&R | Retrospective Case-Control Study | This study included 318 women who were diagnosed with chronic myofascial pelvic pain during a 1-year period. Prevalence of generalised-HSD was 24% in this sample. Secondary outcomes found women with generalised-HSD were at 7.46 times the odds of low back pain compared to those with normal joints (p = 0.02). |
| Sacroiliac Joint Hypermobility Biomechanics and What it Means for Health Care Providers and Patients [36] | 2019 | Enix, DE | PM&R | Literature Review | Discusses biomechanical causes of pelvic pain, and approaches to physiotherapy treatment. Advise that manual manipulation therapy may be useful as an initial treatment, but not suitable long-term. A care plan including active and passive strategies that engage patients are likely to improve compliance and outcomes. |
| Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain [37] | 2020 | Kiapour, A | International Journal of Spine Surgery | Literature Review | States hypermobility is a potential cause for pain at the sacroiliac joint (SIJ), mentioning that female SIJs have greater mobility when compared to males, resulting in greater stresses, loads and pelvic ligament strains [40]. |
| Sacroiliac Joint Injury [38] | 2020 | Dydyk, AM | StatPearls | Book | States fusion surgery or pregnancy can lead to either hypermobility or hypomobility of the SIJ, which can cause pain. Also highlights several causes of SIJ injury such as trauma, leg-length discrepancy, obesity, pregnancy, and hypermobility. |
| The Association of Self-Reported Generalized Joint Hypermobility with pelvic girdle pain during pregnancy: a retrospective cohort study [28] | 2020 | Ahlqvist, K | BMC Musculoskeletal Disorders | Cohort Study | A 5-point questionnaire was used to determine self-reported generalised joint hypermobility (GJH). 2455 women from 144 antenatal clinics in Sweden were included. Prevalence of overall self-reported GJH was 28.7%. Women with GJH had higher odds of developing pelvic girdle pain during pregnancy than those without GJH, p = 0.001 (odds-ratio 1.27, 95% confidence interval 1.11–1.47). |
| Hypermobility Spectrum Disorder (HSD) Subtype | Beighton Score | Notes |
|---|---|---|
| Generalised-HSD | Positive | High suspicion of potential hypermobility-type Ehlers-Danlos Syndrome (hEDS), requiring thorough assessment. Mainly consists of individuals with generalised joint hypermobility (GJH) and secondary musculoskeletal manifestations, but do not meet full criteria for hEDS. |
| Peripheral-HSD | Usually negative | Joint hypermobility (JH) limited to hands and feet with one or more secondary musculoskeletal manifestations. |
| Localised-HSD | Negative | JH at single or small group of joints with secondary musculoskeletal manifestations. |
| Historical-HSD | Negative | Self-reported GJH using the five-point questionnaire, with a negative Beighton score, plus musculoskeletal manifestations. |
| Dermatological | Skin hyperextensibility—to a lesser extent than seen in Classical Ehlers-Danlos Syndrome |
| Velvety, soft skin texture | |
| Absence of skin fragility | |
| Striae formation | |
| Herniation of bowel or muscle | |
| Capillary fragility and wound healing defects such as atrophic scars | |
| Orthopaedic | Congenital capsule-ligamentous laxity |
| Joint hypermobility | |
| Joint instability | |
| Joint dislocations | |
| Soft tissue injuries | |
| Spine: hyperkyphosis, hyperlordosis, scoliosis | |
| Fixed subluxations of: costochondral, sternoclavicular, distal radioulnar, first carpometacarpal joints | |
| Cubitus valgus | |
| Genuum valgum | |
| Hallux valgus | |
| Femur anteversion | |
| Flexible flatfoot | |
| Gynaecological | Irregular menses |
| Menorrhagia | |
| Metorrhagia | |
| Dysmenorrhea | |
| Uterine prolapse | |
| Urinary stress incontinence | |
| Neurological | Altered myopathic electrophysiology |
| Reduced sensation | |
| Muscle weakness | |
| Myalgia and cramps | |
| Neuropathy | |
| Chronic/recurrent pain—musculoskeletal, neuropathic and visceral | |
| Sleep disturbance | |
| Migraines and headaches | |
| Impaired joint proprioception | |
| Mucosal & Oral | Dryness of eyes, mouth and vagina |
| Mucosal fragility causing spontaneous epistaxis and gingival bleeding | |
| Agenesis or absence of lingual frenulum | |
| Temporomandibular joint dysfunction | |
| Cardiac | Cardiac valve disease |
| Aortic root dilatation | |
| Autonomic cardiac dysfunction—orthostatic intolerance, postural tachycardia syndrome | |
| Pulmonary | Asthmatic and atopic symptoms |
| Increased lung volumes | |
| Impaired gas exchange | |
| Upper and lower airway collapse | |
| Ocular | Blue sclera |
| Blepharochalasis | |
| Antimongoloid palpebral slant | |
| Myopia | |
| Xerophthalmia | |
| Gastrointestinal | Constipation (slow transit)/diarrhoea |
| Gastroesophageal reflux | |
| Gastritis | |
| Hiatus hernia | |
| Crohn’s disease | |
| Abdominal pain | |
| Faecal incontinence | |
| Psychiatric | Anxiety |
| Depression | |
| Panic disorder | |
| Personality disorder |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, A.; Andrzejowski, P.; Kanakaris, N.K.; Giannoudis, P.V. Pelvic Girdle Pain, Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome: A Narrative Literature Review. J. Clin. Med. 2020, 9, 3992. https://doi.org/10.3390/jcm9123992
Ali A, Andrzejowski P, Kanakaris NK, Giannoudis PV. Pelvic Girdle Pain, Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome: A Narrative Literature Review. Journal of Clinical Medicine. 2020; 9(12):3992. https://doi.org/10.3390/jcm9123992
Chicago/Turabian StyleAli, Ahmed, Paul Andrzejowski, Nikolaos K. Kanakaris, and Peter V. Giannoudis. 2020. "Pelvic Girdle Pain, Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome: A Narrative Literature Review" Journal of Clinical Medicine 9, no. 12: 3992. https://doi.org/10.3390/jcm9123992
APA StyleAli, A., Andrzejowski, P., Kanakaris, N. K., & Giannoudis, P. V. (2020). Pelvic Girdle Pain, Hypermobility Spectrum Disorder and Hypermobility-Type Ehlers-Danlos Syndrome: A Narrative Literature Review. Journal of Clinical Medicine, 9(12), 3992. https://doi.org/10.3390/jcm9123992