A Nationwide Cross-Sectional Study of Self-Reported Adherence and Factors Associated with Analgesic Treatment in People with Chronic Pain
Abstract
1. Introduction
2. Materials and Methods
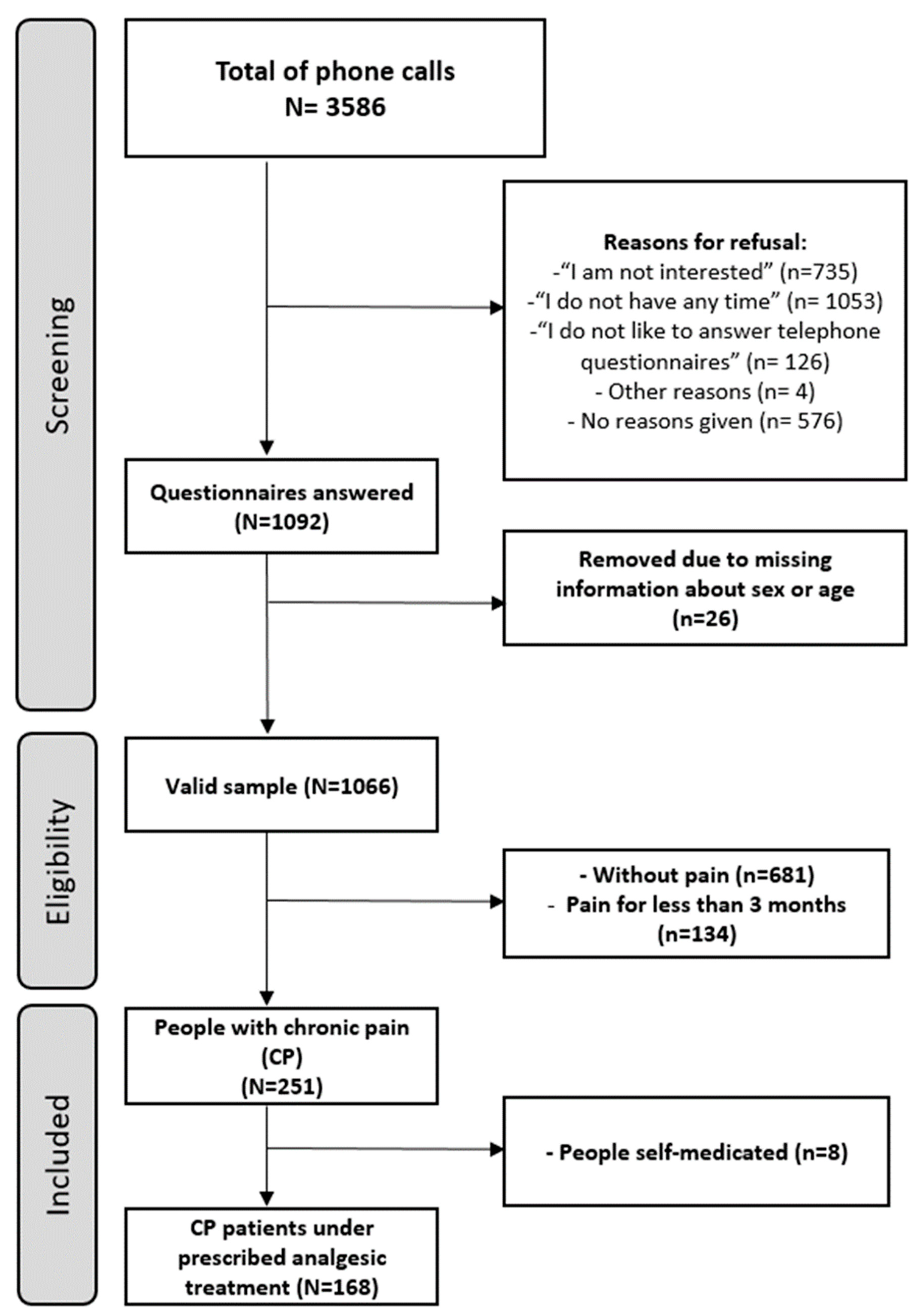
2.1. Participants and Recruitment
2.2. Sampling Methods
2.3. Sample Size
2.4. Procedure and Instruments
2.5. Ethical Statement
2.6. Survey Structure
2.7. Statistical Analysis
3. Results
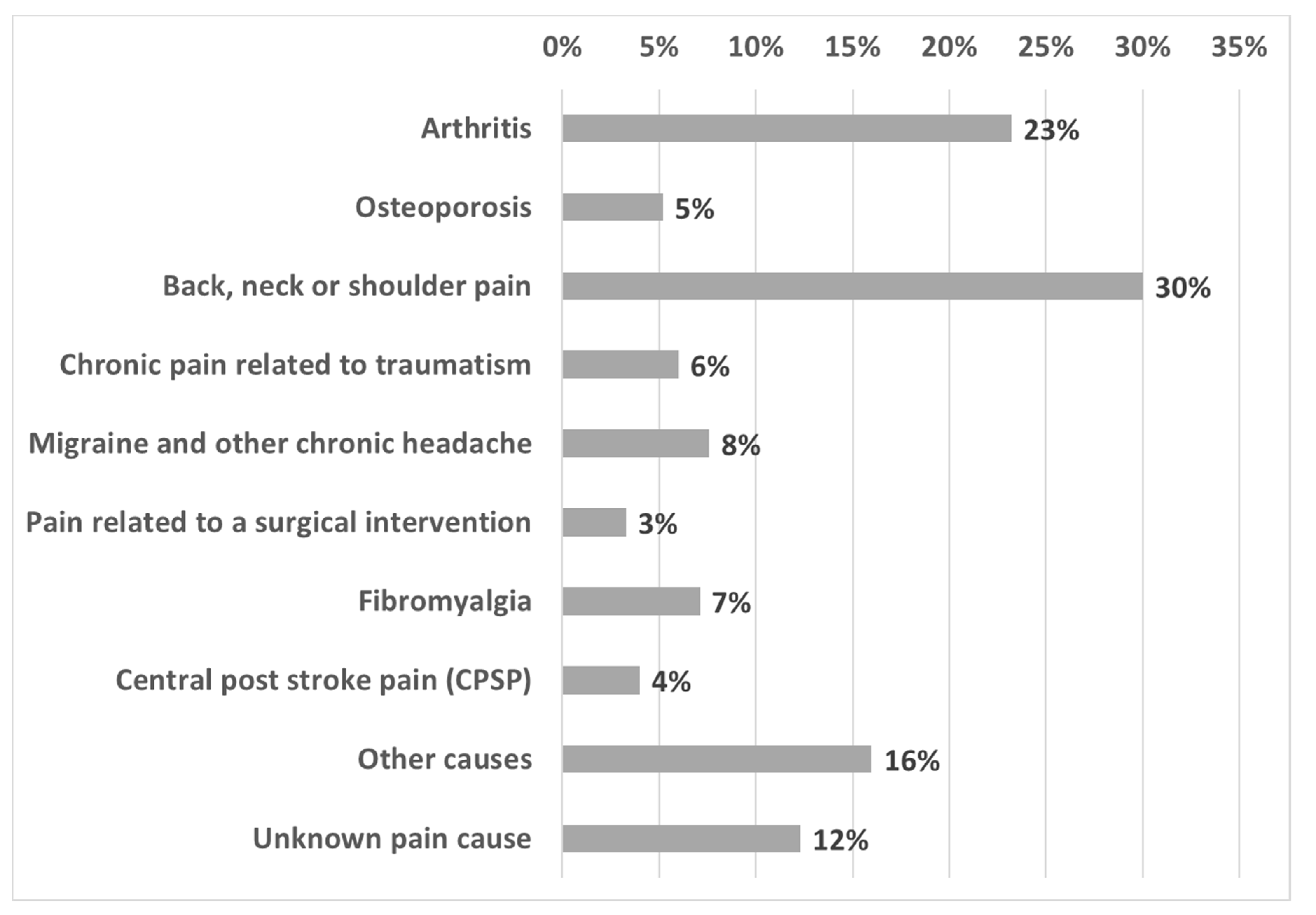
3.1. Characteristics of the Sample
3.2. Comparison of the Factors Related to Self-Reported Adherence among People with CP Taking Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pagé, M.G.; Fortier, M.; Ware, M.; Choinière, M. As if one pain problem was not enough: Prevalence and patterns of coexisting chronic pain conditions and their impact on treatment outcomes. J. Pain Res. 2018, 11, 237–254. [Google Scholar] [CrossRef]
- Langley, P.C.; Ruiz-Iban, M.A.; Molina, J.T.; De Andres, J.; Castellón, J.R.G.-E.; Castellon, J.R. The prevalence, correlates and treatment of pain in Spain. J. Med. Econ. 2011, 14, 367–380. [Google Scholar] [CrossRef] [PubMed]
- Fayaz, A.; Croft, P.; Langford, R.M.; Donaldson, L.J.; Jones, G.T. Prevalence of chronic pain in the UK: A systematic review and meta-analysis of population studies. BMJ Open 2016, 6, e010364. [Google Scholar] [CrossRef] [PubMed]
- Dueñas, M.; Salazar, A.; Ojeda, B.; Fernández-Palacín, F.; Micó, J.A.; Torres, L.M.; Failde, I. A nationwide study of chronic pain prevalence in the general spanish population: Identifying clinical subgroups through cluster analysis. Pain Med. 2015, 16, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Ojeda, B.; Salazar, A.; Dueñas, M.; Torres, L.M.; Mico, J.A.; Failde, I. The Impact of Chronic Pain: The Perspective of Patients, Relatives, and Caregivers. Fam. Syst. Health 2014, 32, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Dueñas, M.; Ojeda, B.; Salazar, A.; Fernández-Palacín, F.; Mico, J.; Torres, L.; Failde, I. Use and satisfaction with the Healthcare System of the chronic pain patients in Spain. Result from a nationwide study. Curr. Med. Res. Opin. 2016, 32, 1813–1820. [Google Scholar] [CrossRef]
- de Sola, H.; Salazar, A.; Dueñas, M.; Ojeda, B.; Failde, I. Nationwide cross-sectional study of the impact of chronic pain on an individual´s employment. Relationship with the family and the social support. BMJ Open 2016, 6, e012246. [Google Scholar] [CrossRef]
- Dueñas, M.; Salazar, A.; Sánchez, M.; De Sola, H.; Ojeda, B.; Failde, I. Relationship Between Using Clinical Practice Guidelines for Pain Treatment and Physicians’ Training and Attitudes Toward Patients and the Effects on Patient Care. Pain Pract. 2017, 18, 38–47. [Google Scholar] [CrossRef]
- Azevedo, L.F.; Costa-Pereira, A.; Mendonça, L.; Dias, C.C.; Castro-Lopes, J.M. Epidemiology of Chronic Pain: A Population-Based Nationwide Study on Its Prevalence, Characteristics and Associated Disability in Portugal. J. Pain 2012, 13, 773–783. [Google Scholar] [CrossRef]
- Breivik, H.; Eisenberg, E.; O’Brien, T. The individual and societal burden of chronic pain in Europe: The case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health 2013, 13. [Google Scholar] [CrossRef]
- Landmark, T.; Romundstad, P.; Dale, O.; Borchgrevink, P.C.; Vatten, L.; Kaasa, S. Chronic pain: One year prevalence and associated characteristics (the HUNT pain study). Scand. J. Pain 2013, 4, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Andersson, H.I.; Ejlertsson, G.; Leden, I.; Scherstén, B. Impact of chronic pain on health care seeking, self care, and medication. Results from a population-based Swedish study. J. Epidemiol. Community Health 1999, 53, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, L.; Stronks, D.L.; Groeneweg, J.G.; Huygen, F.J. Prevalence and determinants of medication non-adherence in chronic pain patients: A systematic review. Acta Anaesthesiol. Scand. 2016, 60, 416–431. [Google Scholar] [CrossRef] [PubMed]
- Vrijens, B.; De Geest, S.; Hughes, D.A.; Przemyslaw, K.; Demonceau, J.; Ruppar, T.; Dobbels, F.; Fargher, E.; Morrison, V.; Lewek, P.; et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 2012, 73, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Kardas, P.; Lewek, P.; Matyjaszczyk, M. Determinants of patient adherence: A review of systematic reviews. Front. Pharmacol. 2013, 4, 1–16. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Adherence to Long-Term Therapies; Evidence for Action; WHO: Geneva, Switzerland, 2003; pp. 1–194. [Google Scholar]
- Timmerman, L.; Stronks, D.L.; Huygen, F.J. The relation between patients’ beliefs about pain medication, medication adherence and treatment outcome in chronic pain patients. Clin. J. Pain 2019, 35, 941–947. [Google Scholar] [CrossRef]
- Stern, A.; Sánchez-Magro, I.; Rull, M. Chronic noncancer pain intensity is inversely related to analgesic adherence in pain clinics. J. Med. Econ. 2011, 14, 568–575. [Google Scholar] [CrossRef]
- Colección Cuadernos de Población. La Población en España: 1900–2009; Fundación BBVA: Bilbao, Spain, 2010. [Google Scholar]
- Herr, K.A.; Mobily, P.R.; Smith, C. Depression and the experience of chronic back pain: A study of related variables and age differences. Clin. J. Pain 1993, 9, 104–114. [Google Scholar] [CrossRef]
- Turk, D.C.; Okifuji, A.; Scharff, L. Chronic pain and depression: Role of perceived impact and perceived control in different age cohorts. Pain 1995, 4, 93–101. [Google Scholar] [CrossRef]
- Riley, J.L.; Gilbert, G.H. Orofacial pain symptoms: An interaction between age and sex. Pain 2001, 90, 245–256. [Google Scholar] [CrossRef]
- Hermsen, L.A.; Leone, S.S.; van der Windt, D.A.; Smalbrugge, M.; Dekker, J.; van der Horst, H.E. Functional outcome in older adults with joint pain and comorbidity: Design of a prospective cohort study. BMC Musculoskelet. Disord. 2011, 12, 241. [Google Scholar] [CrossRef] [PubMed]
- Miró, J.; Paredes, S.; Rull, M.; Queral, R.; Miralles, R.; Nieto, R.; Huguet, A.; Baos, J. Pain in older adults: A prevalence study in the Mediterranean region of Catalonia. Eur. J. Pain 2007, 11, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Sitio Web de Infobel España. Available online: http://eshop.infobel.com/es/productdetails.aspx?ProductID=199. (accessed on 15 January 2011).
- Instituto Nacional de Estadística. Encuesta sobre Equipamiento y Uso de Tecnologías de la Información y Comunicación en los Hogares; Instituto Nacional de Estadística: Madrid, Spain, 2011. [Google Scholar]
- Instituto Nacional de Estadística (INE). Patrón Municipal de 2009; Instituto Nacional de Estadística: Madrid, Spain, 2009. [Google Scholar]
- Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain. Suppl. 1986, 3, S1–S226.
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. Rheum. Dis. 1978, 37, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Serrano, M.S.; Caballero, J.; Cañas, A.; García-Saura, P.L.; Serrano-Álvarez, C.; Prieto, J. Valoración del dolor (I). Rev. Soc. Esp. Dolor. 2002, 9, 94–108. [Google Scholar]
- da Costa, F.A.; Pedro, A.R.; Teixeira, I.; Bragança, F.; da Silva, J.A.; Cabrita, J. Primary non-adherence in Portugal: Findings and implications. Int. J. Clin. Pharm. 2015, 37, 626–635. [Google Scholar] [CrossRef]
- Broekmans, S.; Dobbels, F.; Milisen, K. Pharmacologic Pain Treatment in a Multidisciplinary Pain Center. Clin. J. Pain 2010, 26, 81–86. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Health literacy The solid facts. In The Solid Facts; WHO: Copenhagen, Denmark, 2013; pp. 1–68. ISBN 978 92 890 00154. [Google Scholar]
- Atkinson, T.M.; Rodríguez, V.M.; Gordon, M.; Avildsen, I.K.; Emanu, J.C.; Jewell, S.T.; Anselmi, K.A.; Ginex, P.K. The association between patient-reported and objective oral anticancer medication adherence measures: A systematic review. Oncol. Nurs. Forum 2016, 43, 576–582. [Google Scholar] [CrossRef]
- Bruxvoort, K.; Festo, C.; Cairns, M.; Kalolella, A.; Mayaya, F.; Kachur, S.P.; Schellenberg, D.; Goodman, C. Measuring patient adherence to malaria treatment: A comparison of results from self-report and a customised electronic monitoring device. PLoS ONE 2015, 10, 1–18. [Google Scholar] [CrossRef]
- Sampaio, R.; Azevedo, L.F.; Dias, C.C.; Lopes, J.M.C. Non-adherence to pharmacotherapy: A prospective multicentre study about its incidence and its causes perceived by chronic pain patients. Patient Prefer. Adherence 2020, 14, 321–332. [Google Scholar] [CrossRef]
- Blanchard, K.A.; Morgenstern, J.; Morgan, T.J.; Labouvie, E.; Bux, D.A. Motivational subtypes and continuous measures of readiness for change: Concurrent and predictive validity. Psychol. Addict. Behav. 2003, 17, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.R.; Williams, S.L.; Haskard, K.B.; Dimatteo, M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005, 1, 189–199. [Google Scholar] [PubMed]
- Markotic, F.; Cerni Obrdalj, E.; Zalihic, A.; Pehar, R.; Hadziosmanovic, Z.; Pivic, G.; Durasovic, S.; Grgic, V.; Banozic, A.; Sapunar, D.; et al. Adherence to Pharmacological Treatment of Chronic Nonmalignant Pain in Individuals Aged 65 and Older. Pain Med. 2013, 14, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Mcdonald, H.P.; Garg, A.X.; Haynes, R.B. Interventions to Enhance Patient Adherence Scientific Review. JAMA 2002, 288, 2868–2879. [Google Scholar] [CrossRef] [PubMed]
- Assadeck, H.; Toudou, M.; Hassane, F.; Douma, D.; Adehossi, E. Prevalence and characteristics of chronic pain: Experience of Niger. Scand. J. Pain 2017, 17, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.W.; Choi, S.W.; Wong, S.S.C.; Lee, Y.; Irwin, M.G. Changes in Prevalence, Outcomes, and Help-seeking Behavior of Chronic Pain in an Aging Population Over the Last Decade. Pain Pract. 2017, 17, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Shaw, W.S.; Besen, E.; Pransky, G.; Boot, C.R.L.; Nicholas, M.K.; McLellan, R.K.; Tveito, T.H. Manage at work: A randomized, controlled trial of a self-management group intervention to overcome workplace challenges associated with chronic physical health conditions. BMC Public Health 2014, 14, 515. [Google Scholar] [CrossRef]
- Broekmans, S.; Dobbels, F.; Milisen, K.; Morlion, B.; Vanderschueren, S. Determinants of medication underuse and medication overuse in patients with chronic non-malignant pain: A multicenter study. Int. J. Nurs. Stud. 2010, 47, 1408–1417. [Google Scholar] [CrossRef]
| Variables | Categories | Whole Sample (n = 1066) n (%) | People with Chronic Pain (CP) (n = 251) n (%) | People with CP Taking Analgesic Treatment (n = 168) n (%) |
|---|---|---|---|---|
| SOCIODEMOGRAPHIC DATA | ||||
| Age | 18–44 45–64 65 or more | 424 (39.8) 385 (36.1) 257 (24.1) | 72 (28.7) 105 (41.8) 74 (29.5) | 45 (26.8) 68 (40.5) 55 (32.7) |
| Age | Mean (SD) | 51.6(16.5) | 55.9 (15.5) | 57.1 (15.6) |
| Sex | Men Women | 456 (42.8) 610 (57.2) | 78 (31.1) 173 (68.9) | 40 (23.8) 128 (76.2) |
| Education level | No education received Primary school Secondary school Vocational training University degree | 83 (7.8) 215 (20.3) 252 (23.8) 162 (15.3) 348 (32.8) | 31 (12.4) 73 (29.1) 54 (21.5) 42 (16.7) 51 (20.3) | 21 (12.5) 49 (29.2) 37 (22) 29 (17.3) 32 (19) |
| Employment status | Unemployed Student Housewife/househusband Working Retired Partial disability Total disability | 147 (13.8) 54 (5.1) 125 (11.8) 484 (45.6) 240 (22.6) 6 (0.6) 6 (0.6) | 41 (16.4) 4 (1.6) 43 (17.2) 92 (36.8) 60 (24) 5 (2) 5 (2) | 29 (17.4) 3 (1.8) 34 (20.4) 57 (34.1) 39 (23.4) 2 (1.2) 3 (1.8) |
| Financial difficulties | With great difficulty With difficulty With some difficulty With some ease With ease With great ease | 65 (6.2) 137 (13) 201 (19.1) 272 (25.9) 339 (32.3) 37 (3.5) | 30 (12) 45 (18.1) 60 (24.1) 59 (23.7) 53 (21.3) 2 (0.8) | 20 (12) 29 (17.4) 40 (24) 45 (26.9) 32 (19.2) 1 (0.6) |
| Variables | Categories | Do you Take your Prescription as Indicated by the Doctor? | p | ||
|---|---|---|---|---|---|
| NO (n = 32; 19%) | YES (n = 136; 81%) | ||||
| Social and economic factors | |||||
| Age | 18–44 45–64 65 or more | 8 (25%) 16 (50%) 8 (25%) | 37 (27.2%) 52 (38.2%) 47 (34.6%) | 0.44 a | |
| Sex | Men Women | 8 (25 %) 24 (75%) | 32 (23.5%) 104 (76.5%) | 0.86 a | |
| Level of education | No education received Primary school Secondary school or vocational training University studies | 1 (3.1%) 10 (31.1%) 14 (43.8%) 7 (21.9%) | 20 (14.7%) 39 (28.7%) 52 (38.2%) 25 (18.4%) | 0.36 a | |
| Employment status | Inactive Active Housewife/househusband Retired | 6 (18.8%) 17 (53.1%) 4 (12.5%) 5 (15.6%) | 28 (20.7%) 43 (31.9%) 30 (22.2%) 34 (25.2%) | 0.14 a | |
| How difficult is it for you to make ends meet? | With great difficulty With some difficulty With ease | 9 (29%) 7 (22.6%) 15(48.4%) | 40 (29.4%) 33 (24.3%) 63 (46.3%) | 0.97 a | |
| Condition-related factors | |||||
| How long have you been suffering from this pain? (months) | Mean (SD) | 95.97 (98.21) (n = 31) | 118.14 (131.73) (n = 135) | 0.89 c | |
| Have you been diagnosed with depression during the previous 12 months? | No Yes | 28 (87.5%) 4 (12.5%) | 109 (80.1%) 27 (19.9%) | 0.33 a | |
| Have you been diagnosed with anxiety during the previous 12 months? | No Yes | 24 (75%) 8 (25%) | 99 (72.8%) 37 (27.2%) | 0.80 a | |
| On a scale of 0 to 10, how would you rate the intensity of your chronic pain during the last week? | Mean (SD) | 6.47 (1.525) (n = 30) | 7.29 (1.67) (n = 127) | 0.015 c | |
| Osteoporosis is the main diagnosed cause of the pain | No Yes | 32 (100%) 0 | 126 (93.3%) 9 (6.7%) | 0.047 b | |
| Migraine is the main diagnosed cause of the pain | No Yes | 32 (100) 0 | 125 (92.6%) 10 (7.4%) | 0.036 b | |
| Therapy-related factors | |||||
| How long have you been taking the pain medication? (months) | Mean (SD) | 79.52 (93.75) (n = 29) | 89.91(117) (n = 124) | 0.874 c | |
| Could you tell me which medication you have been prescribed for the pain? | NSAIDs (M01A) | No Yes | 10 (37.0%) 17 (63.0%) | 58 (48.3%) 62 (51.7%) | 0.287 a |
| Antipyretic analgesics (N02B) | No Yes | 14 (51.9%) 13 (48.1%) | 72 (60.0%) 48 (40.0%) | 0.44 a | |
| Opioids (N02A) | No Yes | 24 (88.9%) 3 (11.1%) | 89 (74.2%) 31 (25.8%) | 0.10 a | |
| Antidepressant (N06A) | No Yes | 26 (96.3%) 1 (3.7%) | 114 (95.0%) 6 (5.0%) | 0.77 b | |
| Antiepileptic (N03A) | No Yes | 26 (96.3%) 1 (3.7%) | 111 (92.5%) 9 (7.5%) | 0.45 b | |
| Others (benzodiazepines, cortisone, etc.) | No Yes | 27 (100%) 0 (0%) | 98 (81.7%) 22 (18.3%) | 0.002 b | |
| How many medications are you taking in total at the moment (not just for the pain)? | One Two or three Four or five More than five | 13 (43.3%) 12 (40%) 4 (13.3%) 1 (3.3%) | 26 (19.3%) 59 (43.7%) 23 (17%) 27 (20%) | 0.016 a | |
| How do you take the pain medication? | Orally | No Yes | 0 (0%) 30 (100%) | 6 (4.4%) 130 (95.6%) | 0.118 b |
| Injections | No Yes | 29 (96.7%) 1 (3.3%) | 112 (82.4%) 24 (17.6%) | 0.023 b | |
| Patches | No Yes | 30 (100%) 0 (0%) | 125 (91.9%) 11 (8.1%) | 0.033 b | |
| Has your pain improved as you expected with the treatment? | Less than expected As expected More than expected | 15 (48.4%) 12 (38.7%) 4 (12.9%) | 58 (42.6%) 55 (40.4%) 23 (16.9%) | 0.79 a | |
| Patients that take medication for pain can easily become addicted to it | Disagree Somewhat agree Agree | 10 (32.3%) 4 (13.9%) 17 (54.8%) | 44 (33.3%) 39 (29.5%) 49 (37.1%) | 0.101 a | |
| Medication used to treat pain leads to side effects | Disagree Somewhat agree Agree | 5 (16.1%) 6 (19.4%) 20 (64.5%) | 32 (23.7%) 36 (26.7%) 67 (49.6%) | 0.32 a | |
| Patient-related factors | |||||
| Do you ever forget to take your pain medicine? | No Yes | 21 (65.6%) 11 (34.4%) | 112 (82.4%) 24 (17.6%) | 0.036 a | |
| Do you ever forget to take medications at the hours indicated? | No Yes | 20 (62.5%) 12 (37.5%) | 101 (74.3%) 35 (25.7%) | 0.18 a | |
| If you ever feel better, do you stop taking the treatment? | No Yes | 5 (16.1%) 26 (83.9%) | 73 (53.7%) 63 (46.3%) | 0.000 a | |
| If you ever feel bad, do you stop taking the treatment? | No Yes | 17 (54.8%) 14 (45.2) | 90 (66.7%) 45 (33.3%) | 0.21 a | |
| If you ever feel more pain, do you take more medicine than prescribed? | No Yes | 26 (81.3%) 6 (18.8%) | 121 (89.0%) 15 (11.0%) | 0.26 b | |
| Have you stopped taking the medication due to its price? | No Yes | 31 (96.9%) 1 (3.1%) | 126 (92.6%) 10 (7.4%) | 0.35 b | |
| Have you skipped a dose so that the medication lasts longer? | No Yes | 29 (90.6%) 3 (9.4%) | 129 (94.9%) 7 (5.1%) | 0.39 b | |
| In general, you would say your health is… | Excellent or very good Good Normal Bad | 0 (0 %) 17 (53.1%) 12 (37.5%) 3 (9.4%) | 8 (5.9%) 58 (42.6%) 51 (37.5%) 19 (14.0%) | 0.22 b | |
| Healthcare professional- and family-related factors | |||||
| The information that your doctor has given you about your treatment for pain was… | Very good or good Acceptable Bad or very bad | 16 (50%) 12 (37.5%) 4 (12.5%) | 84 (61.8%) 43 (31.6%) 9 (6.6%) | 0.36 a | |
| The attention provided by your doctor regarding your pain was… | Very good or good Acceptable Bad or very bad | 16 (50%) 10 (31.3%) 6 (18.8%) | 103 (75.7%) 21 (15.4%) 12 (8.8%) | 0.016 a | |
| Are you satisfied with the help received from your family for your pain? | Unsatisfied Satisfied Very satisfied | 8 (25%) 15 (46.9%) 9 (28.1%) | 41 (30.1%) 66 (48.5%) 29 (21.3%) | 0.68 a | |
| Do you have a relative that reminds you to take your medication? | No Yes | 25 (78.1%) 7 (21.9%) | 103 (75.7%) 33 (24.3%) | 0.77 a | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortega-Jiménez, P.; De Sola, H.; Salazar, A.; Dueñas, M.; Del Reguero, L.; Failde, I. A Nationwide Cross-Sectional Study of Self-Reported Adherence and Factors Associated with Analgesic Treatment in People with Chronic Pain. J. Clin. Med. 2020, 9, 3666. https://doi.org/10.3390/jcm9113666
Ortega-Jiménez P, De Sola H, Salazar A, Dueñas M, Del Reguero L, Failde I. A Nationwide Cross-Sectional Study of Self-Reported Adherence and Factors Associated with Analgesic Treatment in People with Chronic Pain. Journal of Clinical Medicine. 2020; 9(11):3666. https://doi.org/10.3390/jcm9113666
Chicago/Turabian StyleOrtega-Jiménez, Patricia, Helena De Sola, Alejandro Salazar, María Dueñas, Leticia Del Reguero, and Inmaculada Failde. 2020. "A Nationwide Cross-Sectional Study of Self-Reported Adherence and Factors Associated with Analgesic Treatment in People with Chronic Pain" Journal of Clinical Medicine 9, no. 11: 3666. https://doi.org/10.3390/jcm9113666
APA StyleOrtega-Jiménez, P., De Sola, H., Salazar, A., Dueñas, M., Del Reguero, L., & Failde, I. (2020). A Nationwide Cross-Sectional Study of Self-Reported Adherence and Factors Associated with Analgesic Treatment in People with Chronic Pain. Journal of Clinical Medicine, 9(11), 3666. https://doi.org/10.3390/jcm9113666





