Creating Healthy Change in the Preconception Period for Women with Overweight or Obesity: A Qualitative Study Using the Information–Motivation–Behavioural Skills Model
Abstract
1. Introduction
1.1. Targeting the Preconception Period
1.2. Weight Management Interventions
2. Methods
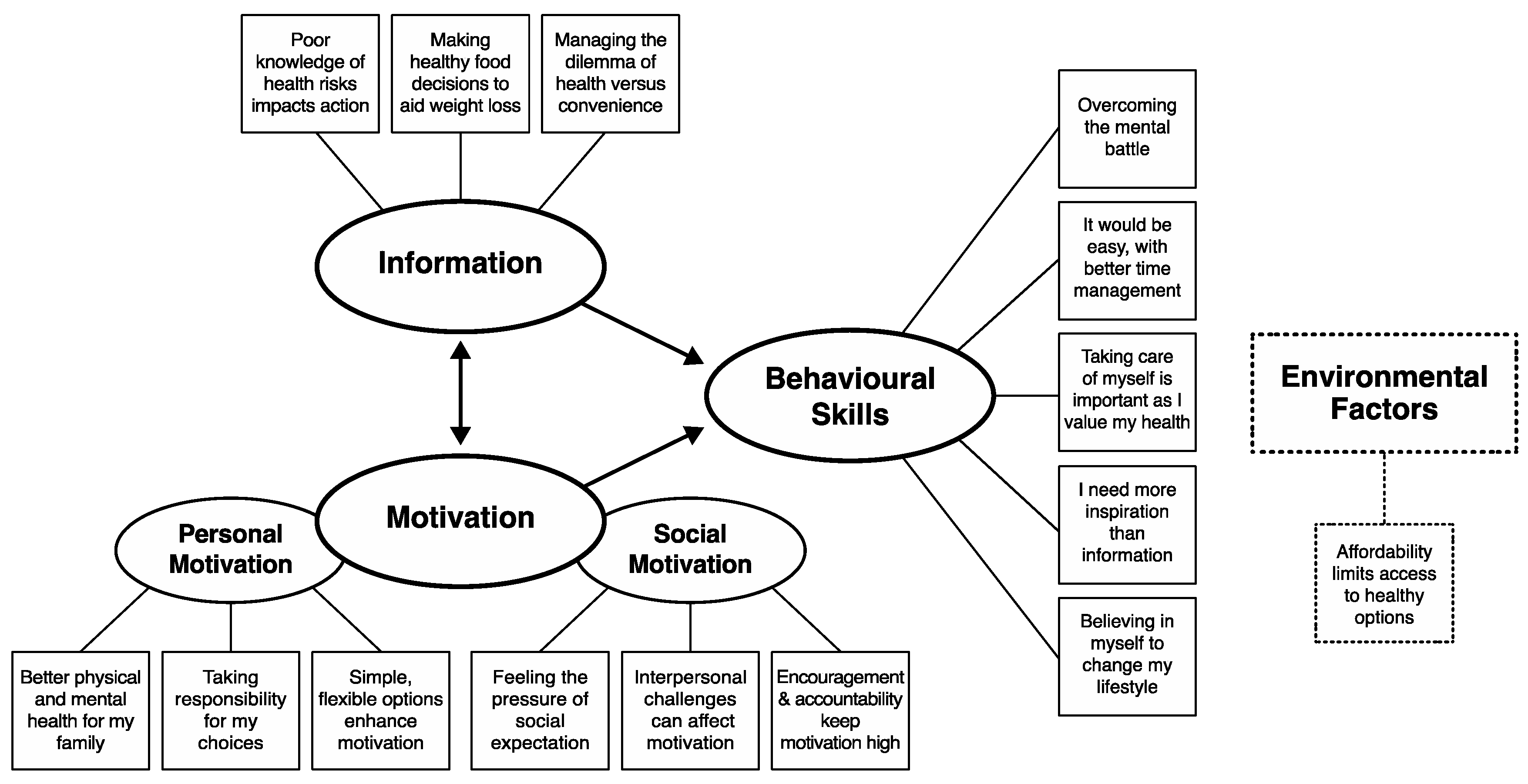
2.1. Theoretical Framework
2.2. Participants
2.3. Procedure
2.4. Analytic Approach
2.5. Ethical Considerations and Quality Criteria
3. Results
3.1. Participant Characteristics
3.2. Overview
3.3. Themes Identified
3.3.1. Theme: Poor Knowledge of Health Risks Impacts Action
“Um, low birthweight, high chance of gestational diabetes, hypertension. And I’ve got it all, so I’m the statistic [laughs].” (Isabel, Overweight)
“Yeah well, stillbirth, um, high birth weight, um, I might be pulling this out of thin air, but I believe it puts your child at higher risk of having diabetes themselves.” (Amber, Obese class II)
“…you want what’s best for your kids, and that starts from the second you see those two pink lines.” (Annie, Obese class III)
3.3.2. Theme: Making Healthy Food Decisions to Aid Weight Loss
“…I suppose an example is when I had gallstones and I wasn’t supposed to be eating fat, I ate kabana [high-fat cured sausage], not realising that it was full of fat, and I ended up in the hospital with a gall bladder attack. It was just a…you know, a lack of information I suppose, I just didn’t know.” (Erin, Overweight)
“Don’t do fad diets, just eat clean. Your food is 80% of it. If you’ve got your food under control, then…other things will fall into place.” (Elizabeth, Overweight)
“There’s a whole confusing world out there when it comes to diet” (Mary, Obese class III)
3.3.3. Theme: Managing the Dilemma of Health Versus Convenience
“…very little time to myself, very little time to prepare food or work out or anything like that. Um, so my lifestyle is very hectic…and very easy… [to choose] what’s easy and convenient, not what is healthy” (Sally, Obese class II)
“So that reliance on convenience foods, you’re bombarded with it when you walk in the supermarket […] everything that ever goes on special is the cheat food […] Why would I, you know, make my own when I can buy a jar on special for $2.” (Annie, Obese class III)
3.3.4. Theme: Better Physical and Mental Health for my Family
“Almost entirely aesthetic. Like I don’t like the way I look in photos. And I understand the health risks, you know, the higher, higher incidence of diabetes, heart disease, all of the fat diseases, but that’s not my main motivator if I’m honest.” (Amber, Obese class II)
“What I make my kids eat is healthy [laughs]. What I eat myself is different, I don’t know why, I don’t know why I do it. […] I really would love my girls to see me um, make healthy choices, and live out what I’m making them live [laughs].” (Mary, Obese class III)
“Just to feel healthier in myself. Also to kick my depression a bit.” (Lucinda, Obese class III)
3.3.5. Theme: Taking Responsibility for My Choices
“… trying to conceive, or have already had children and trying to conceive again, you know, you’ve got another body to look after, like it’s not just you any more” (Sasha, Obese class II)
“I don’t blame my kids or my husband and I don’t think that I don’t have enough time.” (Mary, Obese class III)
“Again, it’s just that overwhelming feeling of, everything’s wrong and I can’t fix any of it, where do I start, you know? […] I’m defeated in my body, I’m defeated in my mind, I’m defeated in my, you know, um, in my home. […] I can’t get on top of anything, and so I will start nowhere [laughs].” (Mary, Obese class III)
3.3.6. Theme: Simple, Flexible Options Enhance Motivation
“I like taking the ideas from it, but I need the flexibility, with the family…for what’s best to eat for us.” (Chloe, Overweight)
“I don’t want a diet that I can’t have for the rest of my life.” (Mary, Obese class III)
3.3.7. Theme: Feeling the Pressure of Social Expectation
“You’re bombarded with Weight Watchers, Michelle Bridges, the Biggest Loser, um…all of that, social media bombards you every day. […] Yeah, and that societal norm. […] there’s always going to be that voice in the back of your head that there is someone judging you, that doesn’t even know you.” (Annie, Obese class III)
3.3.8. Theme: Interpersonal Challenges Can Affect Motivation
“I struggle every day to eat well [laughs]. […] My partner is 60 kilos wringing wet and can sit there and eat whatever he likes. And it’s like trying to give up smoking in a house…where people smoke. […] he’s never been overweight so he doesn’t understand.” (Erin, Overweight)
“I’ve got two kids that are fussy eaters, to try and provide foods that are easy and carb-loaded for them […] So that’s where I‘ve had issues with putting on weight, because trying to motivate the kids to eat and put on a bit of weight, you have to eat what they’re eating. So, it’s just trying to get that balance.” (Ella, Obese class II)
3.3.9. Theme: Encouragement and Accountability Keep Motivation High
“Just nice words of encouragement, like you know ‘you’re doing a good job, and well done on you know, getting through the day, and you know, reaching your goal of however many steps’ or ‘it’s ok you didn’t get there today, but, you know, you’re still doing good’.” (Olivia, Overweight)
“I can fool myself pretty easily and make excuses for why I haven’t done what I’ve done. It’s different when you’ve got to explain to someone else your pathetic reasons for not having done something.” (Amber, Obese class II)
3.3.10. Theme: Overcoming the Mental Battle
“…mental health is a huge thing when you’re trying to lose weight. […] [it] can be really demoralising, especially if you’re not achieving those goals. Or if people around you are achieving them, and you’re not.” (Elizabeth, Overweight)
“You’ve really got to sort of train yourself mentally as well, to…um, eat better and to exercise more. It’s kind of a mental battle as well.” (Olivia, Overweight)
3.3.11. Theme: It Would Be Easy, with Better Time Management
“I feel like it’s just managing my time better isn’t it? Just getting up, even like a little bit earlier, I can do it in the morning…” (Alex, Obese class II)
“I think if someone can help you plan your whole day, so you can fit it in.” (Mary, Obese class III)
3.3.12. Theme: Taking Care of Myself Is Important as I Value My Health
“When I eat well, I feel well if that makes sense.” (Erin, Overweight)
“For me it’s got the stress relief component, it’s my ‘me’ time, it feels good, I feel good afterwards, I tend to be…I find the flow on effects, so when I exercise that’s when I do tend to be less likely to go to straight the cupboard because I’m still feeling motivated.” (Chloe, Overweight)
3.3.13. Theme: I Need More Inspiration Than Information
“…knowing how to make foods interesting so you’re not eating the same old things continuously […] how to make vegetables more interesting […] without adding massive amounts of calories to them.” (Lucinda, Obese class III)
“…oh gosh, I need more inspiration than information” (Amber, Obese class II)
3.3.14. Theme: Believing in Myself to Change My Lifestyle
“Very [confident]. As long as it’s cost-effective and easy to fit it in with the schedule. Like it’s not a 2 h prep. […] It’s gotta be a…let’s just chop it up and get it happening. But I like things from scratch.” (April, Overweight)
“Reasonably confident. I know I can do it. I know I can, because I’ve done that with little things, like the soft drink as I said. So I know I could do it.” (Erin, Overweight)
3.3.15. Theme: Affordability Limits Access to Healthy Options
“So it’s more about finding the alternate to those expensive things […] because it’s very expensive starting a diet and that can sometimes put a lot of people off, because budget-wise you just can’t fit it in. And I find that’s why people go for the easy foods, because it is cheaper.” (April, Overweight)
“…that makes it a bit harder sometimes, especially if we’re like, tight on money and the only thing that we can whip up is like sausages and packet pasta and stuff like that.” (Carla, Obese class III)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The International Weight Management in Pregnancy [i-WIP] Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar]
- Marchi, J.; Berg, M.; Dencker, A.; Olander, E.K.; Begley, C. Risks associated with obesity in pregnancy, for the mother and baby: A systematic review of reviews. Obes. Rev. 2015, 16, 621–638. [Google Scholar] [CrossRef]
- Salihu, H.; de la Cruz, C.; Rahman, S.; August, E. Does maternal obesity cause preeclampsia? A systematic review of the evidence. Minerva Ginecol. 2012, 64, 259–280. [Google Scholar] [PubMed]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalán, C.; Uauy, R.; Herring, S.; Gillman, M. Preconceptional and maternal obesity: Epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016, 4, 1025–1036. [Google Scholar] [CrossRef]
- Turcksin, R.; Bel, S.; Galjaard, S.; Devlieger, R. Maternal obesity and breastfeeding intention, initiation, intensity and duration: A systematic review. Matern. Child Nutr. 2014, 10, 166–183. [Google Scholar] [CrossRef] [PubMed]
- Araujo Junior, E.; Peixoto, A.; Zamarian, A.; Elito Junior, J.; Tonni, G. Macrosomia. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 38, 83–96. [Google Scholar] [CrossRef]
- Davey, M.A.; Flood, M.; Pollock, W.; Cullinane, F.; McDonald, S. Risk factors for severe postpartum haemorrhage: A population-based retrospective cohort study. Aust. N. Z. J. Obstet. Gynaecol. 2020, 60, 522–532. [Google Scholar] [CrossRef]
- Rooney, B.L.; Mathiason, M.A.; Schauberger, C.W. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern. Child Health J. 2011, 15, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.; Beall, M.; Ross, M.G. Developmental origins of obesity: Programmed adipogenesis. Curr. Diabetes Rep. 2013, 13, 27–33. [Google Scholar] [CrossRef]
- Contu, L.; Hawkes, C.A. A Review of the Impact of Maternal Obesity on the Cognitive Function and Mental Health of the Offspring. Int. J. Mol. Sci. 2017, 18, 1093. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J. Pregnancy: Managing obesity during pregnancy-what are the options? Nat. Rev. Endocrinol. 2015, 11, 691–692. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.; Barker, M.; Dodd, J.M.; Kumanyika, S.; Norris, S.; Steegers, E.; Stephenson, J.; Thangaratinam, S.; Yang, H. Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2017, 5, 65–76. [Google Scholar] [CrossRef]
- Price, S.; Nankervis, A.; Permezel, M.; Prendergast, L.; Sumithran, P.; Proietto, J. Health consequences for mother and baby of substantial pre-conception weight loss in obese women: Study protocol for a randomized controlled trial. Trials 2018, 19, 248. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.; deMouzon, S. Maternal obesity and metabolic risk to the offspring: Why lifestyle interventions may have not achieved the desired outcomes. Int. J. Obes. 2015, 39, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.; Robker, R.L.; Robertson, S.A. Parenting from before conception. Science 2014, 345, 756–760. [Google Scholar] [CrossRef]
- Fleming, T.P.; Watkins, A.J.; Velazquez, M.A.; Mathers, J.C.; Prentice, A.M.; Stephenson, J.; Barker, M.; Saffery, R.; Yajnik, C.S.; Eckert, J.J.; et al. Origins of lifetime health around the time of conception: Causes and consequences. Lancet 2018, 391, 1842–1852. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Clinical Practice Guidelines: Pregnancy Care; Department of Health: Canberra, Australia, 2019; pp. 113–119.
- McPhie, S.; Skouteris, H.; Millar, L.; Olsson, C.; Campbell, K.; van der Pligt, P.; Dodd, J.; Hill, B. Preconception weight management: An untapped area of women’s health. Aust. J. Prim. Health 2017, 23, 61–65. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Report of the Commission on Ending Childhood Obesity; World Health Organization (WHO): Geneva, Switzerland, 2016.
- Bull, F.; Willumsen, J. Evidence to prevent childhood obesity: The continuum of preconception, pregnancy, and postnatal interventions. Obes. Rev. 2019, 20, 3–4. [Google Scholar] [CrossRef]
- Dodd, J.; Thangaratinam, S.; i–WIP Collaborative Network. Researchers’ position statement on tackling obesity in pregnancy: The International Weight Management in Pregnancy (i-WIP) collaboration pleads for public health intervention. BJOG 2016, 123, 163–164. [Google Scholar] [CrossRef]
- Godfrey, K.M.; Reynolds, R.M.; Prescott, S.L.; Nyirenda, M.; Jaddoe, V.; Eriksson, J.G.; Broekman, B. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 2017, 5, 53–64. [Google Scholar] [CrossRef]
- Kretowicz, H.; Hundley, V.; Tsofliou, F. Exploring the Perceived Barriers to Following a Mediterranean Style Diet in Childbearing Age: A Qualitative Study. Nutrients 2018, 10, 1694. [Google Scholar] [CrossRef]
- Agha, M.; Agha, R.A.; Sandall, J. Interventions to reduce and prevent obesity in pre-conceptual and pregnant women: A systematic review and meta-analysis. PLoS ONE 2014, 9, e95132. [Google Scholar] [CrossRef] [PubMed]
- van Elten, T.M.; Karsten, M.D.A.; Geelen, A.; van Oers, A.M.; van Poppel, M.N.M.; Groen, H.; Gemke, R.; Mol, B.W.; Mutsaerts, M.A.Q.; Roseboom, T.J.; et al. Effects of a preconception lifestyle intervention in obese infertile women on diet and physical activity; A secondary analysis of a randomized controlled trial. PLoS ONE 2018, 13, e0206888. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Steptoe, A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J. Epidemiol. Community Health 2003, 57, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.N.; Boyle, J.A.; Lang, A.Y.; Harrison, C.L. Preconception Health Attitudes and Behaviours of Women: A Qualitative Investigation. Nutrients 2019, 11, 1490. [Google Scholar] [CrossRef]
- Lillis, J.; Kendra, K.E. Acceptance and Commitment Therapy for weight control: Model, evidence, and future directions. J. Context. Behav. Sci. 2014, 3, 1–7. [Google Scholar] [CrossRef]
- Lang, A.; Harrison, C.; Boyle, J. Preconception lifestyle and weight-related behaviors by maternal body mass index: A cross-sectional study of pregnant women. Nutrients 2019, 11, 759. [Google Scholar] [CrossRef]
- Green, J.; Thorogood, N. Qualitative Methods for Health Research, 2nd ed.; Sage Publications Ltd.: London, UK, 2009. [Google Scholar]
- Fisher, J.; Fisher, W. Changing AIDS-risk behavior. Psychol. Bull. 1992, 111, 455–474. [Google Scholar] [CrossRef]
- Fisher, W.; Fisher, J.; Shuper, P. Social Psychology and the Fight Against AIDS: An Information–Motivation–Behavioral Skills Model for the Prediction and Promotion of Health Behavior Change. In Advances in Experimental Social Psychology; Academic Press: New York, NY, USA, 2014; pp. 105–193. [Google Scholar]
- Fisher, W.; Fisher, J.; Harman, J. The Information–Motivation–Behavioral Skills Model: A generalsocial psychological approach to understanding and promoting health behavior. In Social Psychological Foundations of Health and Illness; Suls, J., Wallston, K.A., Eds.; Blackwell Publishing: Malden, MA, USA, 2003; pp. 82–106. [Google Scholar]
- Goodell, L.; Pierce, M.; Amico, K.; Ferris, A. Parental information, motivation, and behavioral skills correlate with child sweetened beverage consumption. J. Nutr. Educ. Behav. 2012, 44, 240–245. [Google Scholar] [CrossRef]
- Bartholmae, M.M. The Information-Motivation-Behavioral Skills Model: An Examination of Obesity Prevention Behavioral Change in Children Who Participated In The Afterschool Program Virginia Beach Let’s Move. Old Dom. Univ. 2016, 82–88. [Google Scholar] [CrossRef]
- Sinley, R.; Albrecht, J. Application of the IMB Model to the Reported Intake of Fruits and Vegetables of Native American Children. J. Health Disparities Res. Pract. 2018, 11, 2. [Google Scholar]
- Kelly, S.; Melnyk, B.M.; Belyea, M. Predicting physical activity and fruit and vegetable intake in adolescents: A test of the information, motivation, behavioral skills model. Res. Nurs. Health 2012, 35, 146–163. [Google Scholar] [CrossRef] [PubMed]
- Osborn, C.Y.; Rivet Amico, K.; Fisher, W.A.; Egede, L.E.; Fisher, J.D. An information-motivation-behavioral skills analysis of diet and exercise behavior in Puerto Ricans with diabetes. J. Health Psychol. 2010, 15, 1201–1213. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V.; Hayfield, N.; Terry, G. Thematic Analysis. In Handbook of Research Methods in Health and Social Sciences; Liamputtong, P., Ed.; Springer: Singapore, 2019; pp. 843–860. [Google Scholar]
- O’Cathain, A.; Croot, L.; Duncan, E.; Rousseau, N.; Sworn, K.; Turner, K.M.; Yardley, L.; Hoddinott, P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019, 9, e029954. [Google Scholar] [CrossRef]
- Tracy, S.J. Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qual. Inq. 2010, 16, 837–851. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; Sage Publications Ltd.: London, UK, 2013. [Google Scholar]
- Roberts, J.P.; Fisher, T.R.; Trowbridge, M.J.; Bent, C. A design thinking framework for healthcare management and innovation. Healthcare (Amst) 2016, 4, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Scholten, H.; Granic, I. Use of the Principles of Design Thinking to Address Limitations of Digital Mental Health Interventions for Youth: Viewpoint. J. Med. Internet Res. 2019, 21, e11528. [Google Scholar] [CrossRef]
- Dodd, J.; Turnbull, D.; McPhee, A.; Deussen, A.; Grivell, R.; Yelland, L.; Crowther, C.; Wittert, G.; Owens, J.; Robinson, J.; et al. Antenatal lifestyle advice for women who are overweight or obese: LIMIT randomised trial. BMJ 2014, 348, g1285. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.; Louise, J.; Deussen, A.; Grivell, R.; Dekker, G.; McPhee, A.; Hague, W. Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: The GRoW randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019, 7, 15–24. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Reproductive Health Indicators: Guidelines for Their Generation, Interpretation and Analysis for Global Monitoring; World Health Organization (WHO): Geneva, Switzerland, 2006.
- Patton, M.Q. Qualitative Evaluation and Research Methods; Sage: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- QSR International Pty Ltd. NVivo Qualitative Data Analysis Software 12; QSR International Pty Ltd.: Melbourne, Australia, 2018. [Google Scholar]
- Hennink, M.; Kaiser, B.; Marconi, V. Code saturation versus meaning saturation: How many interviews are enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 2018, 18, 148. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Wick, D. Deviant Case Analysis. In Encyclopedia of Case Study Research; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2010; pp. 289–291. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Sui, Z.; Turnbull, D.A.; Dodd, J.M. Overweight and obese women’s perceptions about making healthy change during pregnancy: A mixed method study. Matern. Child Health J. 2013, 17, 1879–1887. [Google Scholar] [CrossRef] [PubMed]
- Opray, N.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M. Directed preconception health programs and interventions for improving pregnancy outcomes for women who are overweight or obese. Cochrane Database Syst. Rev. 2015, 2015, CD010932. [Google Scholar] [CrossRef] [PubMed]
- Campbell, F.; Johnson, M.; Messina, J.; Guillaume, L.; Goyder, E. Behavioural interventions for weight management in pregnancy: A systematic review of quantitative and qualitative data. BMC Public Health 2011, 11, 491. [Google Scholar] [CrossRef]
- Phelan, S. Pregnancy: A “teachable moment” for weight control and obesity prevention. Am. J. Obstet. Gynecol. 2010, 202, 135.e1–135.e8. [Google Scholar] [CrossRef]
- Barker, M.; Dombrowski, S.U.; Colbourn, T.; Fall, C.H.D.; Kriznik, N.M.; Lawrence, W.T.; Norris, S.A.; Ngaiza, G.; Patel, D.; Skordis-Worrall, J.; et al. Intervention strategies to improve nutrition and health behaviours before conception. Lancet 2018, 391, 1853–1864. [Google Scholar] [CrossRef]
- Bearak, J.; Popinchalk, A.; Alkema, L.; Sedgh, G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: Estimates from a Bayesian hierarchical model. Lancet Global Health 2018, 6, e380–e389. [Google Scholar] [CrossRef]
- Cheney, K.; Sim, K.A.; D’Souza, M.; Pelosi, M.; Black, K.I. Unintended pregnancy amongst an early pregnancy clinic cohort: Identifying opportunities for preventative health interventions. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 426–431. [Google Scholar] [CrossRef]
- Blakely, T.; Cleghorn, C.; Mizdrak, A.; Waterlander, W.; Nghiem, N.; Swinburn, B.; Wilson, N.; Ni Mhurchu, C. The effect of food taxes and subsidies on population health and health costs: A modelling study. Lancet Public Health 2020, 5, e404–e413. [Google Scholar] [CrossRef]
- Lal, A.; Mantilla-Herrera, A.M.; Veerman, L.; Backholer, K.; Sacks, G.; Moodie, M.; Siahpush, M.; Carter, R.; Peeters, A. Modelled health benefits of a sugar-sweetened beverage tax across different socioeconomic groups in Australia: A cost-effectiveness and equity analysis. PLoS Med. 2017, 14, e1002326. [Google Scholar] [CrossRef]
- Swinburn, B.; Sacks, G.; Hall, K.; McPherson, K.; Finegood, D.; Moodie, M.; Gortmaker, S. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Cohen, D.A.; Babey, S.H. Contextual influences on eating behaviours: Heuristic processing and dietary choices. Obes. Rev. 2012, 13, 766–779. [Google Scholar] [CrossRef] [PubMed]
- Buckton, C.; Lean, M.; Combet, E. Language is the source of misunderstandings—Impact of terminology on public perceptions of health promotion messages. BMC Public Health 2015, 15, 579. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Williams, S.; Bradbury, K.; Garip, G.; Renouf, S.; Ware, L.; Dorling, H.; Smith, E.; Little, P. Integrating user perspectives into the development of a web-based weight management intervention. Clin. Obes. 2013, 2, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Ufholz, K. Peer Support Groups for Weight Loss. Curr. Cardiovasc. Risk Rep. 2020, 14, 1–11. [Google Scholar] [CrossRef]
- Shingleton, R.M.; Palfai, T.P. Technology-delivered adaptations of motivational interviewing for health-related behaviors: A systematic review of the current research. Patient Educ. Couns. 2016, 99, 17–35. [Google Scholar] [CrossRef]
- Rogers, J.M.; Ferrari, M.; Mosely, K.; Lang, C.P.; Brennan, L. Mindfulness-based interventions for adults who are overweight or obese: A meta-analysis of physical and psychological health outcomes. Obes. Rev. 2017, 18, 51–67. [Google Scholar] [CrossRef]
- Ogata, K.; Koyama, K.I.; Amitani, M.; Amitani, H.; Asakawa, A.; Inui, A. The Effectiveness of Cognitive Behavioral Therapy With Mindfulness and an Internet Intervention for Obesity: A Case Series. Front. Nutr. 2018, 5, 56. [Google Scholar] [CrossRef]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef] [PubMed]
|
| n | |
|---|---|
| Age (years) | |
| 20–29 | 7 |
| 30–39 | 9 |
| 40–49 | 7 |
| Number of children | |
| 1 | 4 |
| 2 | 8 |
| 3 | 6 |
| 4 | 5 |
| Intending pregnancy in next 12 months | |
| Yes | 2 |
| No | 18 |
| Unsure | 3 |
| Body Mass Index (BMI) a | |
| Overweight (25.0–29.9) b | 9 |
| Obese class I (30.0–34.9) b | 4 |
| Obese class II (35.0–39.9) b | 5 |
| Obese class III (≥40.0) b | 5 |
| Amount of weight desire to lose (kg) | |
| 5–9 | 5 |
| 10–19 | 6 |
| 20–29 | 2 |
| 30–39 | 4 |
| 40–49 | 2 |
| 50+ | 3 |
| Unsure | 1 |
| Education | |
| High School | 4 |
| Trade or Diploma | 16 |
| Degree | 2 |
| Postgraduate Degree | 1 |
| Employment Status | |
| Full time | 6 |
| Part time | 6 |
| Student | 2 |
| Home duties | 9 |
| Family situation | |
| Single parent family | 1 |
| Two-parent family | 21 |
| Undisclosed | 1 |
| Difficulty meeting basic living costs | |
| Weekly | 4 |
| Monthly | 8 |
| Never | 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scott, J.; Oxlad, M.; Dodd, J.; Szabo, C.; Deussen, A.; Turnbull, D. Creating Healthy Change in the Preconception Period for Women with Overweight or Obesity: A Qualitative Study Using the Information–Motivation–Behavioural Skills Model. J. Clin. Med. 2020, 9, 3351. https://doi.org/10.3390/jcm9103351
Scott J, Oxlad M, Dodd J, Szabo C, Deussen A, Turnbull D. Creating Healthy Change in the Preconception Period for Women with Overweight or Obesity: A Qualitative Study Using the Information–Motivation–Behavioural Skills Model. Journal of Clinical Medicine. 2020; 9(10):3351. https://doi.org/10.3390/jcm9103351
Chicago/Turabian StyleScott, Jodie, Melissa Oxlad, Jodie Dodd, Claudia Szabo, Andrea Deussen, and Deborah Turnbull. 2020. "Creating Healthy Change in the Preconception Period for Women with Overweight or Obesity: A Qualitative Study Using the Information–Motivation–Behavioural Skills Model" Journal of Clinical Medicine 9, no. 10: 3351. https://doi.org/10.3390/jcm9103351
APA StyleScott, J., Oxlad, M., Dodd, J., Szabo, C., Deussen, A., & Turnbull, D. (2020). Creating Healthy Change in the Preconception Period for Women with Overweight or Obesity: A Qualitative Study Using the Information–Motivation–Behavioural Skills Model. Journal of Clinical Medicine, 9(10), 3351. https://doi.org/10.3390/jcm9103351






