An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion
Abstract
1. Introduction
2. Method
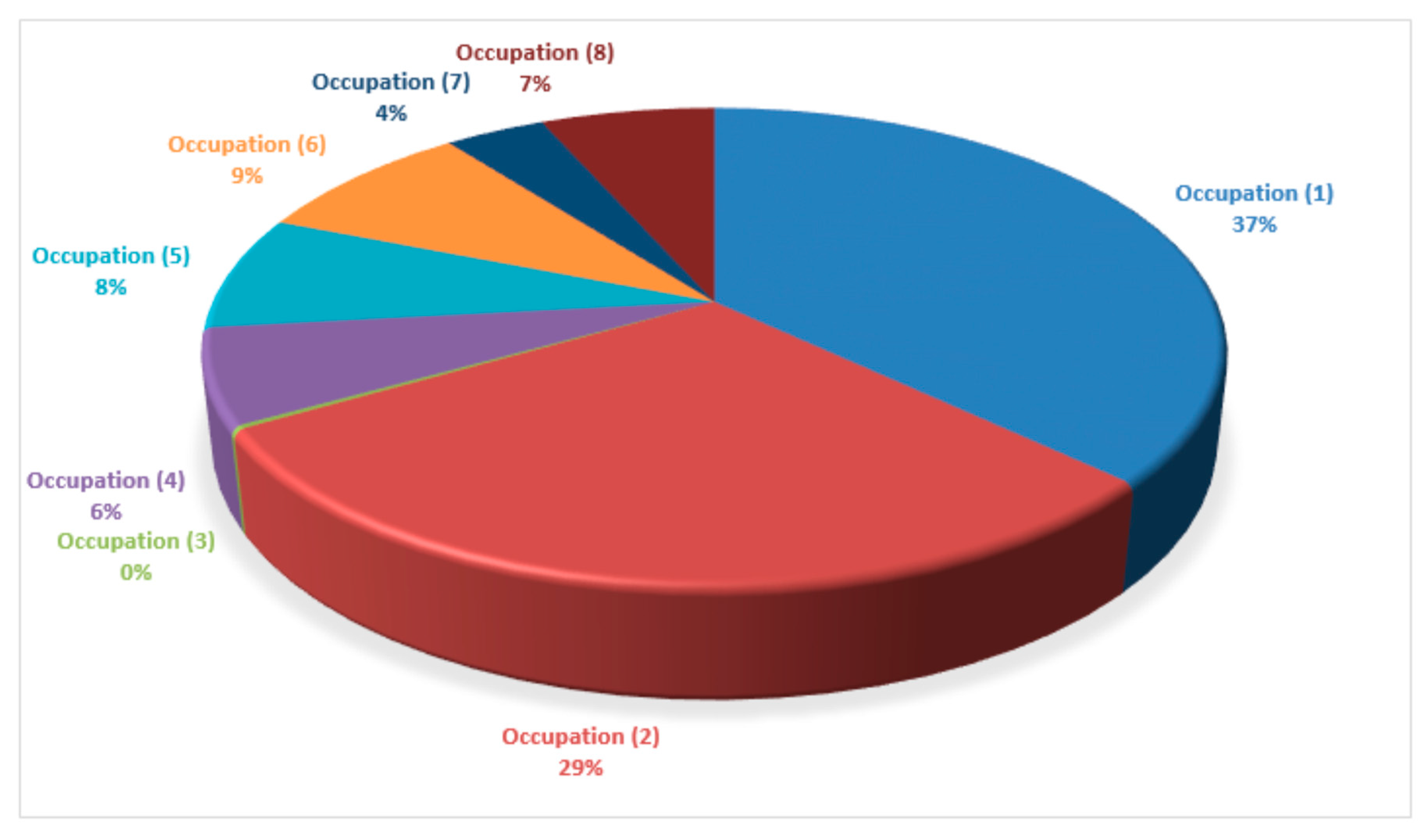
2.1. Participants
2.2. Output Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020; World Health Organization: Geneva, Switzerland, 2020; Volume 10, Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed on 6 August 2020).
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Novel Coronavirus(2019-nCoV), Situation Report-12; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Coronavirus Disease (COVID-19): Situation Report, 199; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- European Commission. Coronavirus: EU Mobilises €10 Million for Research; European Commission: Brussels, Belgium, 2020. [Google Scholar]
- BBC. Coronavirus: UK Donates £20m to Speed up Vaccine; BBC: London, UK, 2020. [Google Scholar]
- The Regulatory Affairs Professionals Society (RAPS)-COVID-19 Vaccine Tracker. Available online: https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker (accessed on 6 August 2020).
- £75 Million Boost for Scottish University Research. One-off Government Payment to Help Mitigate Financial Effects of COVID-19. 2020. Available online: https://www.gov.scot/news/minister-announces-gbp-75m-boost-for-university-research/ (accessed on 6 August 2020).
- Kumar, M.S.; Raut, R.D.; Narwane, V.S.; Narkhede, B.E. Applications of industry 4.0 to overcome the COVID-19 operational challenges. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1283–1289. [Google Scholar] [CrossRef] [PubMed]
- Brun, D.; Curti, C.; Mekideche, T.; Benech, A.; Hounliasso, I.; Lamy, E.; Castera, C.; Rathelot, P.; Vanelle, P. Stockpiled N95 respirator/surgical mask release beyond manufacturer-designated shelf-life: A French experience. J. Hosp. Infect. 2020, 106, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Plana, D.; Tian, E.; Cramer, A.K.; Yang, H.; Carmack, M.M.; Sinha, M.S.; Bourgeois, F.T.; Yu, S.H.; Masse, P.; Boyer, J. Assessing the quality of nontraditional N95 filtering face-piece respirators available during the COVID-19 pandemic. medRxiv 2020. [Google Scholar] [CrossRef]
- Tarfaoui, M.; Nachtane, M.; Goda, I.; Qureshi, Y.; Benyahia, H. 3D Printing to Support the Shortage in Personal Protective Equipment Caused by COVID-19 Pandemic. Materials 2020, 13, 3339. [Google Scholar] [CrossRef]
- Hyoju, S.K.; Zaborina, O.; van Goor, H. SARS-CoV-2 and the sympathetic immune response: Dampening inflammation with antihypertensive drugs (Clonidine and Propranolol). Med. Hypotheses 2020, 144, 110039. [Google Scholar] [CrossRef]
- Wiese, O.; Zemlin, A.E.; Pillay, T.S. Molecules in pathogenesis: Angiotensin converting enzyme 2 (ACE2). J. Clin. Pathol. 2020. [Google Scholar] [CrossRef]
- Malayala, S.V.; Raza, A. A Case of COVID-19-Induced Vestibular Neuritis. Cureus 2020, 12, e8918. [Google Scholar] [CrossRef]
- Assenza, G.; Lanzone, J.; Brigo, F.; Coppola, A.; Di Gennaro, G.; Di Lazzaro, V.; Ricci, L.; Romigi, A.; Tombini, M.; Mecarelli, O. Epilepsy Care in the Time of COVID-19 Pandemic in Italy: Risk Factors for Seizure Worsening. Front. Neurol. 2020, 11, 737. [Google Scholar] [CrossRef]
- Grippo, A.; Assenza, G.; Scarpino, M.; Broglia, L.; Cilea, R.; Galimberti, C.A.; Lanzo, G.; Michelucci, R.; Tassi, L.; Vergari, M. Electroencephalography during SARS-CoV-2 outbreak: Practical recommendations from the task force of the Italian Society of Neurophysiology (SINC), the Italian League Against Epilepsy (LICE), and the Italian Association of Neurophysiology Technologists (AITN). Neurol. Sci. 2020, 41, 2345–2351. [Google Scholar]
- Bhaskar, S.; Bradley, S.; Israeli-Korn, S.; Menon, B.; Chattu, V.K.; Thomas, P.; Chawla, J.; Kumar, R.; Prandi, P.; Ray, D. Chronic neurology in COVID-19 era: Clinical considerations and recommendations from the REPROGRAM Consortium. Front. Neurol. 2020, 11, 664. [Google Scholar] [CrossRef] [PubMed]
- Manganotti, P.; Bellavita, G.; D’Acunto, L.; Tommasini, V.; Fabris, M.; Sartori, A.; Bonzi, L.; Buoite Stella, A.; Pesavento, V. Clinical neurophysiology and cerebrospinal liquor analysis to detect Guillain Barré syndrome and polyneuritis cranialis in COVID-19 patients: A case series. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Polvoy, I.; Flavell, R.R.; Ohliger, M.; Rosenberg, O.; Wilson, D.M. Nuclear imaging of bacterial infection-state of the art and future directions. J. Nucl. Med. 2020, 61, jnumed-120. [Google Scholar] [CrossRef]
- Jiang, M.D.; Zu, Z.Y.; Schoepf, U.J.; Savage, R.H.; Zhang, X.L.; Lu, G.M.; Zhang, L.J. Current Status of Etiology, Epidemiology, Clinical Manifestations and Imagings for COVID-19. Korean J. Radiol. 2020, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.I. Radiologists’ Solutions for COVID-19 in Korea. Korean J. Radiol. 2020, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Park, J.; Lim, J.-K.; Shin, K.M.; Lee, J.; Seo, H.; Lee, Y.H.; Heo, J.; Lee, W.K.; Kim, J.Y. Prognostic Implication of Volumetric Quantitative CT Analysis in Patients with COVID-19: A Multicenter Study in Daegu, Korea. Korean J. Radiol. 2020, 21, 1256. [Google Scholar] [CrossRef]
- Wang, L.-Q.; Zhang, M.; Liu, G.-M.; Nan, S.-Y.; Li, T.; Xu, L.; Xue, Y.; Zhang, M.; Wang, L.; Qu, Y.-D. Psychological impact of Coronavirus Disease 2019 (COVID-19) epidemic on medical staff in different posts in China: A multicenter study. J. Psychiatr. Res. 2020, 129, 198–205. [Google Scholar] [CrossRef]
- Huang, L.; Lei, W.; Xu, F.; Liu, H.; Yu, L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS ONE 2020, 15, e0237303. [Google Scholar] [CrossRef]
- Fox-Lewis, S.; Muttaiyah, S.; Rahnama, F.; McAuliffe, G.; Roberts, S. An understanding of discordant SARS-CoV-2 test results: An examination of the data from a central Auckland laboratory. N. Z. Med. J. 2020, 133, 81–88. [Google Scholar] [PubMed]
- Campioli, C.C.; Cevallos, E.C.; Assi, M.; Patel, R.; Binnicker, M.J.; O’Horo, J.C. Clinical predictors and timing of cessation of viral RNA shedding in patients with COVID-19. J. Clin. Virol. 2020, 130, 104577. [Google Scholar] [CrossRef] [PubMed]
- Mahendiratta, S.; Batra, G.; Sarma, P.; Kumar, H.; Bansal, S.; Kumar, S.; Prakash, A.; Sehgal, R.; Medhi, B. Molecular diagnosis of COVID-19 in different biologic matrix, their diagnostic validity and clinical relevance: A systematic review. Life Sci. 2020, 258, 118207. [Google Scholar] [CrossRef] [PubMed]
- Perkmann, T.; Perkmann-Nagele, N.; Breyer, M.-K.; Breyer-Kohansal, R.; Burghuber, O.C.; Hartl, S.; Aletaha, D.; Sieghart, D.; Quehenberger, P.; Marculescu, R. Side by side comparison of three fully automated SARS-CoV-2 antibody assays with a focus on specificity. medRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- De Smet, K.; De Smet, D.; Ryckaert, T.; Laridon, E.; Heremans, B.; Vandenbulcke, R.; Demedts, I.; Bouckaert, B.; Gryspeerdt, S.; Martens, G.A. Diagnostic Performance of Chest CT for SARS-CoV-2 Infection in Individuals with or without COVID-19 Symptoms. Radiology 2020, 202708. [Google Scholar] [CrossRef] [PubMed]
- Valle, C.; Martin, B.; Touret, F.; Shannon, A.; Canard, B.; Guillemot, J.C.; Coutard, B.; Decroly, E. Drugs against SARS-CoV-2: What do we know about their mode of action? Rev. Med. Virol. 2020, e2143. [Google Scholar] [CrossRef]
- Weisberg, E.; Parent, A.; Yang, P.L.; Sattler, M.; Liu, Q.; Liu, Q.; Wang, J.; Meng, C.; Buhrlage, S.J.; Gray, N. Repurposing of Kinase Inhibitors for Treatment of COVID-19. Pharm. Res. 2020, 37, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Shamim, S.; Khan, M.; Kharaba, Z.J.; Ijaz, M.; Murtaza, G. Potential strategies for combating COVID-19. Arch. Virol. 2020, 1–20. [Google Scholar] [CrossRef]
- Dutheil, F.; Trousselard, M.; Perrier, C.; Lac, G.; Chamoux, A.; Duclos, M.; Naughton, G.; Mnatzaganian, G.; Schmidt, J. Urinary interleukin-8 is a biomarker of stress in emergency physicians, especially with advancing age—The JOBSTRESS* randomized trial. PLoS ONE 2013, 8, e71658. [Google Scholar] [CrossRef]
- Dutheil, F.; Pereira, B.; Moustafa, F.; Naughton, G.; Lesage, F.-X.; Lambert, C. At-risk and intervention thresholds of occupational stress using a visual analogue scale. PLoS ONE 2017, 12, e0178948. [Google Scholar] [CrossRef]
- Dutheil, F.; Boudet, G.; Perrier, C.; Lac, G.; Ouchchane, L.; Chamoux, A.; Duclos, M.; Schmidt, J. JOBSTRESS study: Comparison of heart rate variability in emergency physicians working a 24-hour shift or a 14-hour night shift—A randomized trial. Int. J. Cardiol. 2012, 158, 322–325. [Google Scholar] [CrossRef] [PubMed]
- Woods, J.; Hutchinson, N.T.; Powers, S.K.; Roberts, W.O.; Gomez-Cabrera, M.C.; Radak, Z.; Berkes, I.; Boros, A.; Boldogh, I.; Leeuwenburgh, C. The COVID-19 pandemic and physical activity. Sports Med. Health Sci. 2020, 2, 55–64. [Google Scholar] [CrossRef]
- Smith, B.J.; Lim, M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020, 30, e3022008. [Google Scholar] [CrossRef]
- Seeman, T.E. Health promoting effects of friends and family on health outcomes in older adults. Am. J. Health Promot. 2000, 14, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef]
- Shankar, A.; McMunn, A.; Banks, J.; Steptoe, A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011, 30, 377. [Google Scholar] [CrossRef]
- Luo, Y.; Hawkley, L.C.; Waite, L.J.; Cacioppo, J.T. Loneliness, health, and mortality in old age: A national longitudinal study. Soc. Sci. Med. 2012, 74, 907–914. [Google Scholar] [CrossRef]
- World Health Organisation-Physical Activity. Available online: https://www.who.int/health-topics/physical-activity#tab=tab_1 (accessed on 6 August 2020).
- WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents, Adults and Older Adults (DRAFT-for Consultation). 2020. Available online: https://www.who.int/docs/default-source/physical-activity/call-for-consultation/draft-guideline-on-physical-activity-and-sedentray-behaviour.pdf?sfvrsn=ddf523d5_4#:~:text=For%20adults%2C%20sedentary%20behaviour%20is,and%20community%20settings%20and%20transportation (accessed on 6 August 2020).
- Lesage, F.; Berjot, S. Validity of occupational stress assessment using a visual analogue scale. Occup. Med. 2011, 61, 434–436. [Google Scholar] [CrossRef]
- Lesage, F.-X.; Berjot, S.; Deschamps, F. Clinical stress assessment using a visual analogue scale. Occup. Med. 2012, 62, 600–605. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Chan, Y.H. Biostatistics 104: Correlational analysis. Singap. Med. J. 2003, 44, 614–619. [Google Scholar]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- Ozamiz-Etxebarria, N.; Dosil-Santamaria, M.; Picaza-Gorrochategui, M.; Idoiaga-Mondragon, N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos de Saúde Pública 2020, 36, e00054020. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact of COVID-19 in Spain: Early data report. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Kochhar, A.S.; Bhasin, R.; Kochhar, G.K.; Dadlani, H.; Mehta, V.V.; Kaur, R.; Bhasin, C.K. Lockdown of 1.3 billion people in India during Covid-19 pandemic: A survey of its impact on mental health. Asian J. Psychiatry 2020, 54, 102213. [Google Scholar] [CrossRef]
- Rehman, U.; Shahnawaz, M.G.; Khan, N.H.; Kharshiing, K.D.; Khursheed, M.; Gupta, K.; Kashyap, D.; Uniyal, R. Depression, Anxiety and Stress Among Indians in Times of Covid-19 Lockdown. Community Ment. Health J. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Álvarez, N.Y.; Piñeiro-Lamas, R.; Vuelvas-Olmos, C.R. Psychological Effects and Associated Factors of COVID-19 in a Mexican Sample. Disaster Med. Public Health Prep. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Smith, L.; Jacob, L.; Yakkundi, A.; McDermott, D.; Armstrong, N.C.; Barnett, Y.; López-Sánchez, G.F.; Martin, S.; Butler, L.; Tully, M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Res. 2020, 291, 113138. [Google Scholar] [CrossRef]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Cerami, C.; Santi, G.C.; Galandra, C.; Dodich, A.; Cappa, S.F.; Vecchi, T.; Crespi, C. Covid-19 Outbreak in Italy: Are We Ready for the Psychosocial and the Economic Crisis? Baseline Findings From the PsyCovid Study. Front. Psychiatry 2020, 11, 556. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Mishra, A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int. J. Soc. Psychiatry 2020, 66, 756–762. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Rushing, W.A. Marital status and mental disorder: Evidence in favor of a behavioral model. Soc. Forces 1979, 58, 540–556. [Google Scholar] [CrossRef]
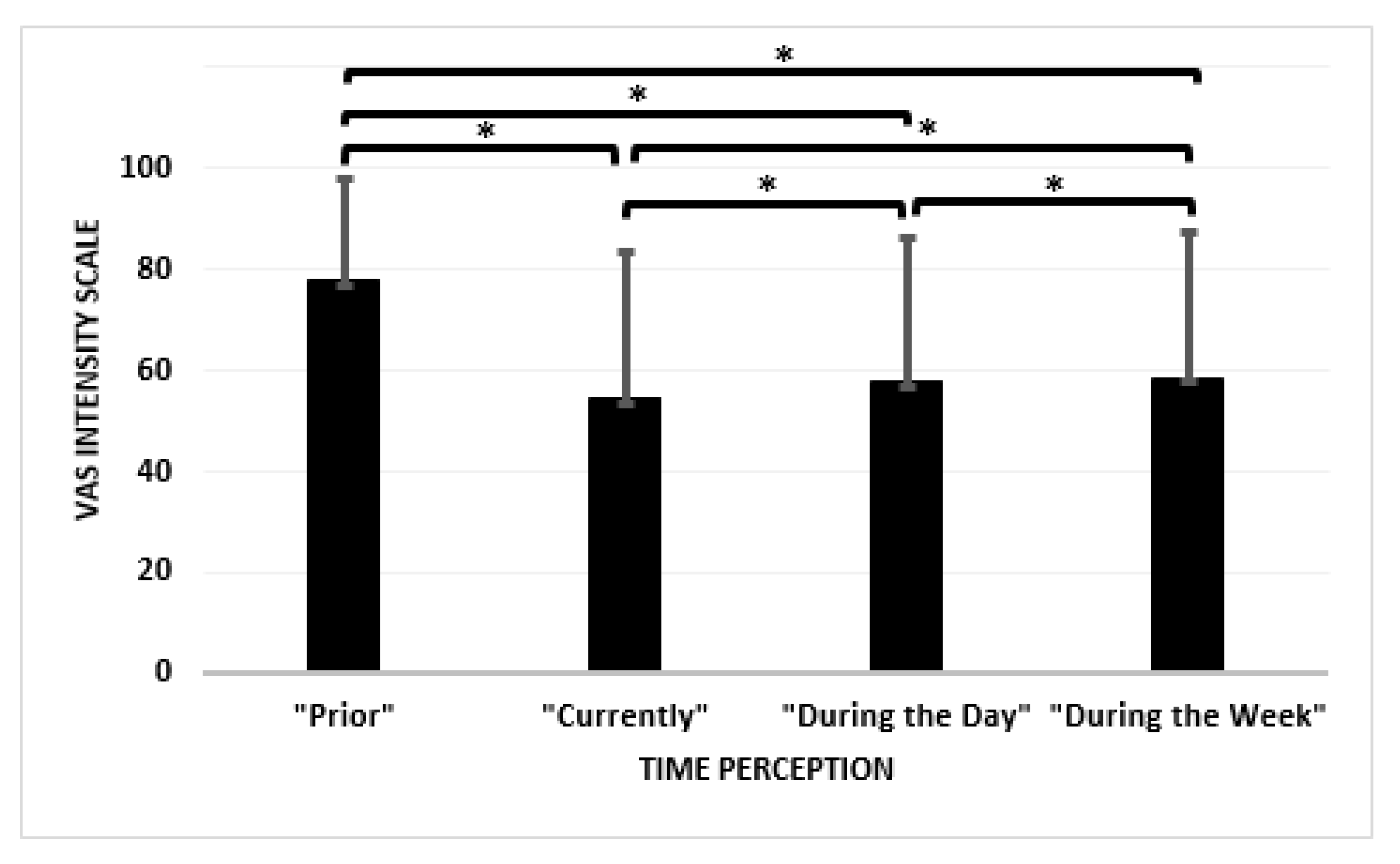
| Output Measures | Assessment “Prior” COVID-19 (Mean ± SD) | Assessment “Currently” during COVID-19 (Mean ± SD) | Mean Difference between “Prior” and “Currently” | Correlation (r) between “Prior” and “Currently” | Statistical Significance |
|---|---|---|---|---|---|
| Number of hours seated per day | 12.45 ± 6.11 | 15.43 ± 7.60 | 2.98 | 0.656 | <0.001 |
| Number of hours of leisure physical activity per week | 8.97 ± 7.79 | 6.55 ± 6.65 | −2.42 | 0.503 | <0.001 |
| a Soothed/Anger | 38.13 ± 22.90 | 54.84 ± 25.60 | 16.71 | 0.190 | <0.001 |
| b Sadness/Joy | 68.56 ± 21.14 | 46.94 ± 24.91 | −21.62 | 0.191 | <0.001 |
| Peaceful/Excited | 43.86 ± 25.19 | 46.93 ± 25.06 | 3.07 | 0.252 | <0.001 |
| c Busy/Bored | 19.27 ± 19.46 | 41.07 ± 30.77 | 21.8 | 0.253 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ugbolue, U.C.; Duclos, M.; Urzeala, C.; Berthon, M.; Kulik, K.; Bota, A.; Thivel, D.; Bagheri, R.; Gu, Y.; Baker, J.S.; et al. An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion. J. Clin. Med. 2020, 9, 3352. https://doi.org/10.3390/jcm9103352
Ugbolue UC, Duclos M, Urzeala C, Berthon M, Kulik K, Bota A, Thivel D, Bagheri R, Gu Y, Baker JS, et al. An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion. Journal of Clinical Medicine. 2020; 9(10):3352. https://doi.org/10.3390/jcm9103352
Chicago/Turabian StyleUgbolue, Ukadike Chris, Martine Duclos, Constanta Urzeala, Mickael Berthon, Keri Kulik, Aura Bota, David Thivel, Reza Bagheri, Yaodong Gu, Julien S. Baker, and et al. 2020. "An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion" Journal of Clinical Medicine 9, no. 10: 3352. https://doi.org/10.3390/jcm9103352
APA StyleUgbolue, U. C., Duclos, M., Urzeala, C., Berthon, M., Kulik, K., Bota, A., Thivel, D., Bagheri, R., Gu, Y., Baker, J. S., Andant, N., Pereira, B., Rouffiac, K., Clinchamps, M., Dutheil, F., & on behalf of the COVISTRESS Network. (2020). An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion. Journal of Clinical Medicine, 9(10), 3352. https://doi.org/10.3390/jcm9103352











