Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Study Protocol
2.4. Assessment of Symptoms
2.5. Ultrasonographic Assessment of Rectosigmoid Endometriotic Nodules
2.6. Statistical Analysis
2.7. Ethical Approval
3. Results
3.1. Pain and Gastrointestinal Symptoms
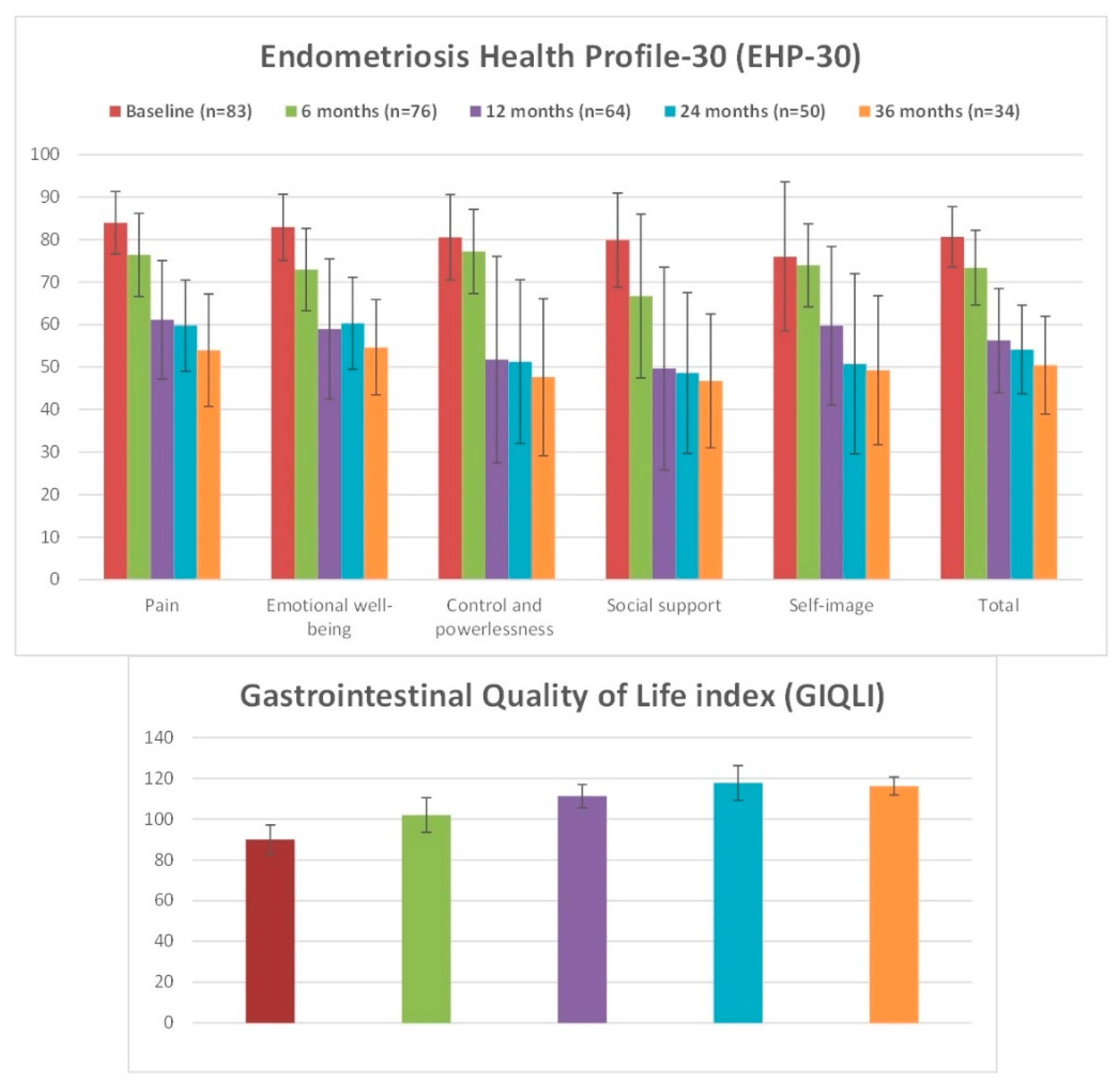
3.2. Patients’ Quality of Life
3.3. Size of Rectosigmoid Endometriotic Nodules
3.4. Tolerability of the Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Nezhat, C.; Li, A.; Falik, R.; Copeland, D.; Razavi, G.; Shakib, A.; Mihailide, C.; Bamford, H.; DiFrancesco, L.; Tazuke, S.; et al. Bowel endometriosis: Diagnosis and management. Am. J. Obstet. Gynecol. 2018, 218, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Remorgida, V.; Ferrero, S.; Fulcheri, E.; Ragni, N.; Martin, D.C. Bowel endometriosis: Presentation, diagnosis, and treatment. Obstet. Gynecol. Surv. 2007, 62, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, S.; Camerini, G.; Ragni, N.; Remorgida, V. Endometriosis and irritable bowel syndrome: Co-morbidity or misdiagnosis? BJOG 2009, 116, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Hudelist, G.; English, J.; Thomas, A.E.; Tinelli, A.; Singer, C.F.; Keckstein, J. Diagnostic accuracy of transvaginal ultrasound for non-invasive diagnosis of bowel endometriosis: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2011, 37, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Condous, G.; van den Bosch, T.; Valentin, L.; Leone, F.P.; Van Schoubroeck, D.; Exacoustos, C.; Installe, A.J.; Martins, W.P.; Abrao, M.S.; et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: A consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet. Gynecol. 2016, 48, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Balla, A.; Quaresima, S.; Subiela, J.D.; Shalaby, M.; Petrella, G.; Sileri, P. Outcomes after rectosigmoid resection for endometriosis: A systematic literature review. Int. J. Colorectal. Dis. 2018, 33, 835–847. [Google Scholar] [CrossRef] [PubMed]
- Donnez, O.; Roman, H. Choosing the right surgical technique for deep endometriosis: Shaving, disc excision, or bowel resection? Fertil. Steril. 2017, 108, 931–942. [Google Scholar] [CrossRef]
- Ferrero, S.; Camerini, G.; Ragni, N.; Venturini, P.L.; Biscaldi, E.; Seracchioli, R.; Remorgida, V. Letrozole and norethisterone acetate in colorectal endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 150, 199–202. [Google Scholar] [CrossRef]
- Ferrero, S.; Camerini, G.; Ragni, N.; Venturini, P.L.; Biscaldi, E.; Remorgida, V. Norethisterone acetate in the treatment of colorectal endometriosis: A pilot study. Hum. Reprod. 2010, 25, 94–100. [Google Scholar] [CrossRef]
- Ferrero, S.; Camerini, G.; Ragni, N.; Menada, M.V.; Venturini, P.L.; Remorgida, V. Triptorelin improves intestinal symptoms among patients with colorectal endometriosis. Int. J. Gynaecol. Obstet. 2010, 108, 250–251. [Google Scholar] [CrossRef]
- Ferrero, S.; Alessandri, F.; Racca, A.; Leone Roberti Maggiore, U. Treatment of pain associated with deep endometriosis: Alternatives and evidence. Fertil. Steril. 2015, 104, 771–792. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, S.; Evangelisti, G.; Barra, F. Current and emerging treatment options for endometriosis. Expert Opin. Pharmacother. 2018, 19, 1109–1125. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, N.; Remorgida, V.; Leone Roberti Maggiore, U.; Scala, C.; Tafi, E.; Ghirardi, V.; Salvatore, S.; Candiani, M.; Venturini, P.L.; Ferrero, S. Dienogest in the treatment of endometriosis. Expert Opin. Pharmacother. 2014, 15, 1889–1902. [Google Scholar] [CrossRef] [PubMed]
- Andres Mde, P.; Lopes, L.A.; Baracat, E.C.; Podgaec, S. Dienogest in the treatment of endometriosis: Systematic review. Arch. Gynecol. Obstet. 2015, 292, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Persico, P.; Di Puppo, F.; Vigano, P.; Tandoi, I.; Garavaglia, E.; Giardina, P.; Mezzi, G.; Candiani, M. Continuous low-dose oral contraceptive in the treatment of colorectal endometriosis evaluated by rectal endoscopic ultrasonography. Acta Obstet. Gynecol. Scand. 2012, 91, 699–703. [Google Scholar] [CrossRef]
- Ferrero, S.; Camerini, G.; Venturini, P.L.; Biscaldi, E.; Remorgida, V. Progression of bowel endometriosis during treatment with the oral contraceptive pill. Gynecol. Surg. 2011, 8, 311–313. [Google Scholar] [CrossRef]
- Ferrero, S.; Leone Roberti Maggiore, U.; Scala, C.; Di Luca, M.; Venturini, P.L.; Remorgida, V. Changes in the size of rectovaginal endometriotic nodules infiltrating the rectum during hormonal therapies. Arch. Gynecol. Obstet. 2013, 287, 447–453. [Google Scholar] [CrossRef]
- Vercellini, P.; Buggio, L.; Borghi, A.; Monti, E.; Gattei, U.; Frattaruolo, M.P. Medical treatment in the management of deep endometriosis infiltrating the proximal rectum and sigmoid colon: A comprehensive literature review. Acta Obstet. Gynecol. Scand. 2018, 7, 942–955. [Google Scholar] [CrossRef]
- Nieveen Van Dijkum, E.J.; Terwee, C.B.; Oosterveld, P.; Van Der Meulen, J.H.; Gouma, D.J.; De Haes, J.C. Validation of the gastrointestinal quality of life index for patients with potentially operable periampullary carcinoma. Br. J. Surg. 2000, 87, 110–115. [Google Scholar] [CrossRef]
- Khong, S.Y.; Lam, A.; Luscombe, G. Is the 30-item Endometriosis Health Profile (EHP-30) suitable as a self-report health status instrument for clinical trials? Fertil. Steril. 2010, 94, 1928–1932. [Google Scholar] [CrossRef]
- Valenzano Menada, M.; Remorgida, V.; Abbamonte, L.H.; Nicoletti, A.; Ragni, N.; Ferrero, S. Does transvaginal ultrasonography combined with water-contrast in the rectum aid in the diagnosis of rectovaginal endometriosis infiltrating the bowel? Hum. Reprod. 2008, 23, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
- Vercellini, P.; Crosignani, P.G.; Somigliana, E.; Berlanda, N.; Barbara, G.; Fedele, L. Medical treatment for rectovaginal endometriosis: What is the evidence? Hum. Reprod. 2009, 24, 2504–2514. [Google Scholar] [CrossRef] [PubMed]
- Noel, J.C.; Chapron, C.; Bucella, D.; Buxant, F.; Peny, M.O.; Fayt, I.; Borghese, B.; Anaf, V. Estrogen and progesterone receptors in smooth muscle component of deep infiltrating endometriosis. Fertil. Steril. 2010, 93, 1774–1777. [Google Scholar] [CrossRef] [PubMed]
- Barra, F.; Scala, C.; Ferrero, S. Current understanding on pharmacokinetics, clinical efficacy and safety of progestins for treating pain associated to endometriosis. Expert Opin. Drug Metab. Toxicol. 2018, 14, 399–415. [Google Scholar] [CrossRef]
- Grandi, G.; Mueller, M.; Bersinger, N.A.; Cagnacci, A.; Volpe, A.; McKinnon, B. Does dienogest influence the inflammatory response of endometriotic cells? A systematic review. Inflamm. Res. 2016, 65, 183–192. [Google Scholar] [CrossRef]
- Vercellini, P.; Bracco, B.; Mosconi, P.; Roberto, A.; Alberico, D.; Dhouha, D.; Somigliana, E. Norethindrone acetate or dienogest for the treatment of symptomatic endometriosis: A before and after study. Fertil. Steril. 2016, 105, 734–743. [Google Scholar] [CrossRef]
- Morotti, M.; Sozzi, F.; Remorgida, V.; Venturini, P.L.; Ferrero, S. Dienogest in women with persistent endometriosis-related pelvic pain during norethisterone acetate treatment. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 183, 188–192. [Google Scholar] [CrossRef]
- Leonardo-Pinto, J.P.; Benetti-Pinto, C.L.; Cursino, K.; Yela, D.A. Dienogest and deep infiltrating endometriosis: The remission of symptoms is not related to endometriosis nodule remission. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 211, 108–111. [Google Scholar] [CrossRef]
- Vercellini, P.; Frattaruolo, M.P.; Rosati, R.; Dridi, D.; Roberto, A.; Mosconi, P.; De Giorgi, O.; Cribiu, F.M.; Somigliana, E. Medical treatment or surgery for colorectal endometriosis? Results of a shared decision-making approach. Hum. Reprod. 2018, 33, 202–211. [Google Scholar] [CrossRef]
- Morotti, M.; Venturini, P.L.; Biscaldi, E.; Racca, A.; Calanni, L.; Vellone, V.G.; Stabilini, C.; Ferrero, S. Efficacy and acceptability of long-term norethindrone acetate for the treatment of rectovaginal endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 213, 4–10. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Q.; Guo, S.W. Histological and Immunohistochemical Characterization of the Similarity and Difference between Ovarian Endometriomas and Deep Infiltrating Endometriosis. Reprod. Sci. 2018, 25, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Song, J.Y.; Yi, K.W.; Lee, S.R.; Lee, D.Y.; Shin, J.H.; Cho, S.; Seo, S.K.; Kim, S.H. Effectiveness of Dienogest for Treatment of Recurrent Endometriosis: Multicenter Data. Reprod. Sci. 2018, 25, 1515–1522. [Google Scholar] [CrossRef] [PubMed]
- Techatraisak, K.; Hestiantoro, A.; Ruey, S.; Banal-Silao, M.J.; Kim, M.R.; Seong, S.J.; Thaufik, S.; Ahlers, C.; Shin, S.Y.; Lee, B.S. Effectiveness of dienogest in improving quality of life in Asian women with endometriosis (ENVISIOeN): Interim results from a prospective cohort study under real-life clinical practice. BMC Women’s Health 2019, 19, 68. [Google Scholar] [CrossRef] [PubMed]

| Patients (n = 83) | |
|---|---|
| Age (years; mean ± SD) | 32.8 ± 5.0 |
| BMI (kg/m2; mean ± SD) | 21.0 + 3.0 |
| Smokers (n, %) | 15 (18.1%) |
| Parity (n, %) | 23 (27.7%) |
| Sexually active (n, %) | 66 (81.9%) |
| Other imaging methods confirming the diagnosis of rectosigmoid endometriosis | 63 (80.7%) |
| Magnetic resonance imaging | 56 (83.6%) |
| Computerized tomography colonography | 8 (11.9%) |
| Multidetector computerized tomography enema | 2 (3.1%) |
| Double-contrast barium enema | 1 (1.5%) |
| Previous surgery for endometriosis (n, %) | 30 (36.1%) |
| Ablation of endometriotic implants | 18 (60%) |
| Excision of endometriotic nodules | 12 (43.3%) |
| Removal of endometriotic ovarian cysts | 6 (23.3%) |
| Time to previous surgery for endometriosis (months; median, interval) | 43 (9–87) |
| Previous hormonal therapy for endometriosis (n, %) | 55 (66.3%) |
| Estroprogestins | 22 (73.3%) |
| Other progestins | 11 (36.7%) |
| Danazol | 4 (13.3%) |
| GnRH agonists | 2 (6.7%) |
| Time to previous hormonal therapy for endometriosis (months; median, interval) | 6.7 (4–37) |
| Symptom | Baseline | 6 Months | 12 Months | 24 Months | 36 Months |
|---|---|---|---|---|---|
| Dysmenorrhea | 7.0 ± 1.2 (n = 73) | 5.5 ± 1.4 (n = 27) P < 0.001 * | 4.3 ± 1.8 (n = 18) P < 0.001 * P = 0.046 § | 4.3± 2.1 (n = 13) P < 0.001 * P = 0.044 § P = 0.632 ¥ | 4.4 ± 2.0 (n = 8) P < 0.001 * P = 0.146 § P = 0.546 ¥ P = 0.732 £ |
| Chronic pelvic pain | 6.1 ± 0.9 (n = 60) | 4.0 ± 1.3 (n = 53); P < 0.001 * | 3.3 ± 1.0 (n = 44); P < 0.001 * P = 0.001 § | 3.4 ± 1.6 (n = 35); P < 0.001 * P = 0.548 § P = 0.582 ¥ | 3.3 ± 1.2 (n = 22); P < 0.001 * P = 0.245 § P = 0.763 ¥ P = 0.819 £ |
| Deep dyspareunia | 5.7 ± 1.9 (n = 57) | 4.3 ± 2.2 (n = 53); P < 0.001 * | 3.6 ± 1.8 (n = 45); P < 0.001 * P = 0.045 § | 3.6 ± 1.6 (n = 38); P < 0.001 * P = 0.538 § P = 0.909 ¥ | 3.7 ± 1.1 (n = 26); P < 0.001 * P = 0.563 § P = 0.226 ¥ P = 0.384 £ |
| Dyschezia | 5.2 ± 1.6 (n = 48) | 3.8 ± 2.2 (n = 43); P < 0.001 * | 3.2 ± 2.6 (n = 40); P < 0.001 * P = 0.039 § | 3.0 ± 1.8 (n = 31); P < 0.001 * P = 0.908 § P = 0.131 ¥ | 2.7 ± 1.9 (n = 19); P < 0.001 * P = 0.304 § P = 0.220 ¥ P = 0.398 £ |
| Constipation | 6.7 ± 1.5 (n = 37) | 2.4 ± 2.4 (n = 33); P < 0.001 * | 1.9 ± 2.0 (n = 33); P < 0.001 * P = 0.086 § | 1.9 ± 1.6 (n = 25); P < 0.001 * P = 0.942 § P = 0.192 ¥ | 1.8 ± 1.7 (n = 16); P<0.001 * P = 0.609 § P = 0.300 ¥ P = 0.436 £ |
| Constipation during the menstrual cycle | 4.6 ± 1.5 (n = 19) | 1.9 ± 0.6 (n = 8) P < 0.001 * | 0.8 ± 0.3 (n = 6) P = 0.001 * P = 0.012 § | 1.4 ± 0.4 (n = 5) P = 0.015 * P = 0.012 § P = 0.059 ¥ | 1.1 ± 0.1 (n = 3) P = 0.063* P = 0.272 § P = 0.195 ¥ P = 0.423 £ |
| Diarrhea | 6.9 ± 1.4 (n = 36) | 2.2 ± 2.3 (n = 33) P<0.001 * | 1.9 ± 2.1 (n = 33); P < 0.001 * P = 0.086 § | 1.8 ± 1.5 (n = 25); P < 0.001 * P = 0.878 § P = 0.129 ¥ | 1.6 ± 1.8 (n = 16); P < 0.001 * P = 0.359 § P = 0.108 ¥ P = 0.223 £ |
| Diarrhea during the menstrual cycle | 4.0 ± 1.6 (n = 15) | 1.6 ± 0.8 (n = 7) P = 0.009 * | 1.2 ± 0.4 (n = 6) P = 0.006 * P = 0.434 § | 1.4 ± 1.1 (n = 5); P = 0.040 * P = 0.807 § P = 0.865 ¥ | 1.0 ± 0.0 (n = 3); P = 0.015 * P = 0.020 § P = 0.321 ¥ P = 0.423 £ |
| Intestinal cramping | 5.6 ± 2.0 (n = 40) | 3.5 ± 2.3 (n = 37); P < 0.001 * | 3.2 ± 1.4 (n = 29); P < 0.001 * P = 0.079 § | 3.1 ± 1.6 (n = 24); P < 0.001 * P = 0.036 § P = 0.953 ¥ | 3.1 ± 1.5 (n = 17); P < 0.001 * P = 0.141 § P = 0.725 ¥ P = 0.681 £ |
| Feeling of incomplete evacuation | 5.6 ± 1.7 (n = 44) | 3.6 ± 2.4 (n = 43); P < 0.001 * | 3.2 ± 2.0 (n = 36); P < 0.001 * P = 0.455 § | 3.3 ± 1.9 (n = 31); P < 0.001 * P = 0.588 § P = 0.792 ¥ | 3.2 ± 1.5 (n = 20); P < 0.001 * P = 0.128 § P = 0.609 ¥ P = 0.499 £ |
| Passage of mucus | 5.6 ± 1.9 (n = 43) | 5.5 ± 2.2 (n = 41); P = 0.206 * | 2.9 ± 1.8 (n = 34); P < 0.001 * P < 0.001 § | 3.0 ± 2.3 (n = 29); P < 0.001 * P = 0.001 § P = 0.977 ¥ | 2.9 ± 1.1 (n = 19); P<0.001 * P = 0.001 § P = 0.861 ¥ P = 0.954 £ |
| Cyclical rectal bleeding | 4.1 ± 2.3 (n = 11) | 1.3 ± 0.9 (n = 6) P = 0.047 * | 1.3 ± 0.5 (n = 4) P = 0.057 * P = 0.330 § | 0.8 ± 0.3 (n = 3); P = 0.004 * P = 0.188 § P = 0.177 ¥ | 1.2 ± 0.8 (n = 3); P = 0.053 * P = 0.873 § P = 0.635 ¥ P = 0.275 £ |
| Largest Diameter of Endometriotic Nodules (mm ± SD) | ||||
|---|---|---|---|---|
| Baseline | 6-month treatment | 12-month treatment | 24-month treatment | 36-month treatment |
| 2.7 ± 0.5 | 2.6 ± 0.5 P = 0.075 * | 2.4 ± 0.5 P = 0.003 * P = 0.046 § | 2.3 ± 0.6 P = 0.026 * P = 0.073 § P = 0.421 ¥ | 2.3 ± 0.5 P = 0.038 * P = 0.234 § P = 0.421 ¥ P = 0.856 £ |
| Volume of Endometriotic Nodules (cm3 ± SD) | ||||
| Baseline | 6-month treatment | 12-month treatment | 24-month treatment | 36-month treatment |
| 4.0 ± 2.1 | 3.7 ± 1.4 P = 0.033 * | 3.1 ± 1.2 P < 0.001 * P < 0.001 § | 3.2 ± 1.3 P = 0.006 * P = 0.017 § P = 0.153 ¥ | 3.0 ± 1.5 P = 0.011 * P = 0.010 § P = 0.677 ¥ P = 0.560 £ |
| Adverse Events (n = 52) | Number of Adverse Effects (%) | Prevalence of Adverse Effects in the Study Population (n = 83) (%) |
|---|---|---|
| Weight gain | 21 (30.1) | 25.3 |
| Abnormal uterine bleeding * | 14 (26.9) | 16.9 |
| Headache | 11 (21.2) | 13.3 |
| Depression | 5 (9.6) | 6.0 |
| Decrease libido | 2 (3.8) | 2.4 |
| Acne | 1 (1.9) | 1.2 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barra, F.; Scala, C.; Leone Roberti Maggiore, U.; Ferrero, S. Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis. J. Clin. Med. 2020, 9, 154. https://doi.org/10.3390/jcm9010154
Barra F, Scala C, Leone Roberti Maggiore U, Ferrero S. Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis. Journal of Clinical Medicine. 2020; 9(1):154. https://doi.org/10.3390/jcm9010154
Chicago/Turabian StyleBarra, Fabio, Carolina Scala, Umberto Leone Roberti Maggiore, and Simone Ferrero. 2020. "Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis" Journal of Clinical Medicine 9, no. 1: 154. https://doi.org/10.3390/jcm9010154
APA StyleBarra, F., Scala, C., Leone Roberti Maggiore, U., & Ferrero, S. (2020). Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis. Journal of Clinical Medicine, 9(1), 154. https://doi.org/10.3390/jcm9010154







