Is Polymicrobial Bacteremia an Independent Risk Factor for Mortality in Acinetobacter baumannii Bacteremia?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Microbiological Studies
2.4. Statistical Analysis
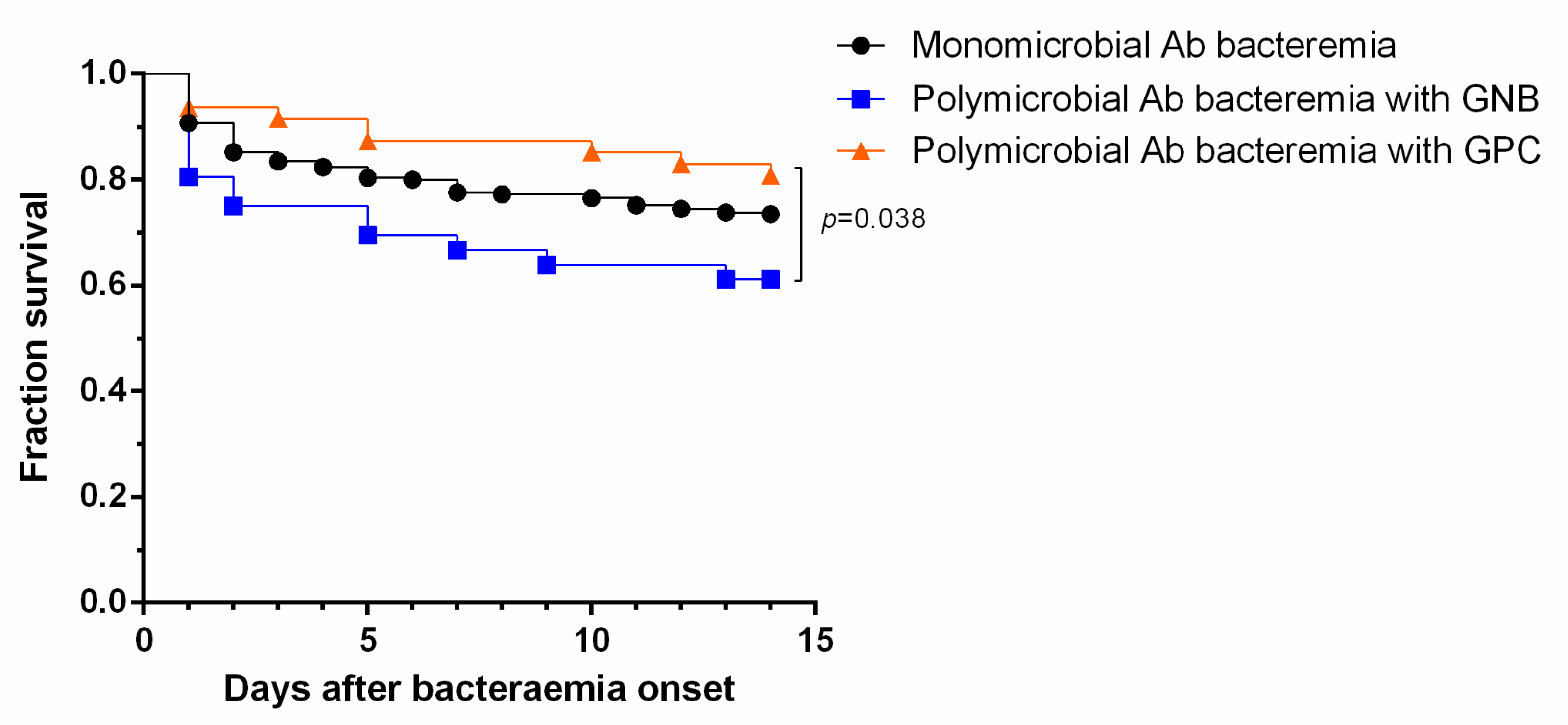
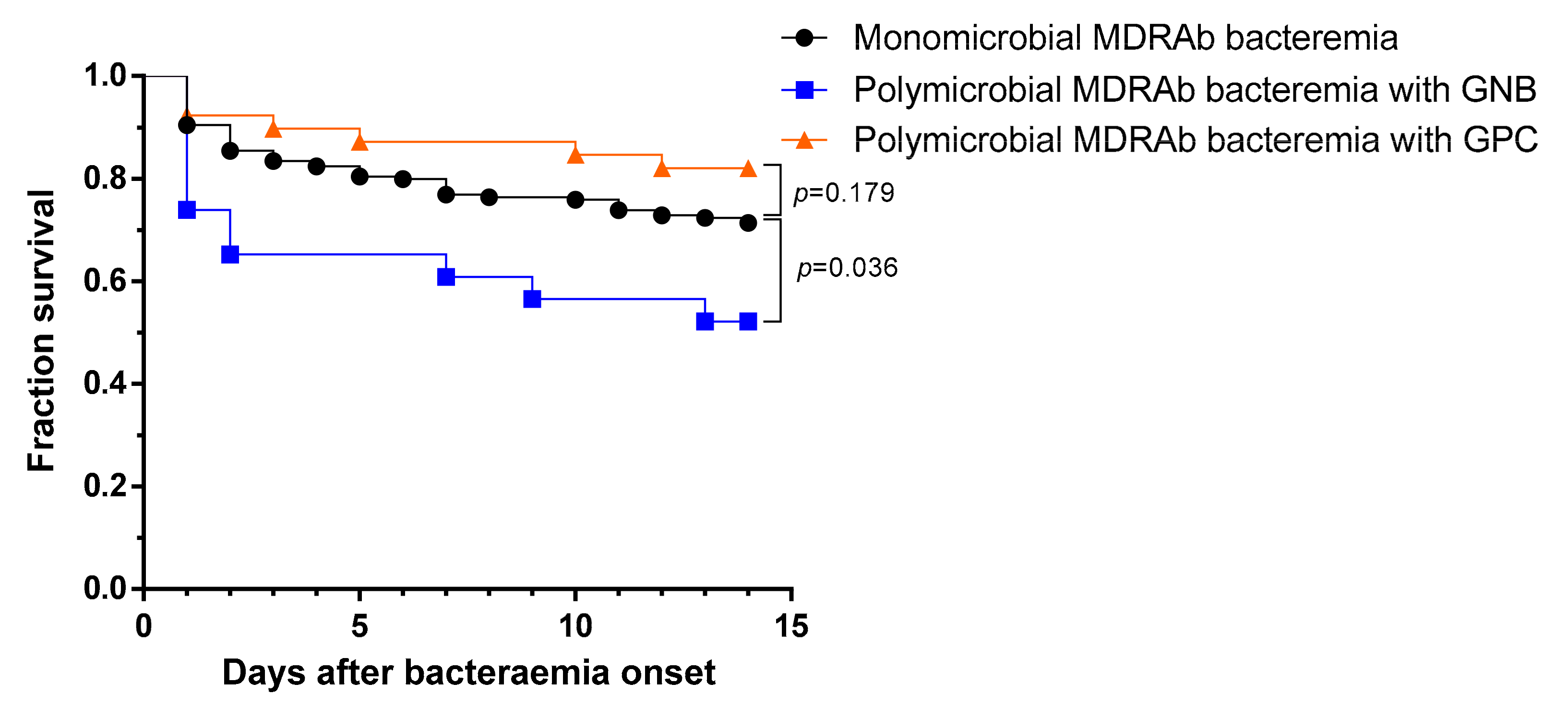
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hermans, P.E.; Washington, J.A., 2nd. Polymicrobial bacteremia. Ann. Intern. Med. 1970, 73, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Roselle, G.A.; Watanakunakorn, C. Polymicrobial bacteremia. JAMA 1979, 242, 2411–2413. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.P.; Murphy, J.R.; Reller, L.B.; Lichtenstein, K.A. The clinical significance of positive blood cultures: A comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. II. Clinical observations, with special reference to factors influencing prognosis. Rev. Infect. Dis. 1983, 5, 54–70. [Google Scholar] [CrossRef] [PubMed]
- Cooper, G.S.; Havlir, D.S.; Shlaes, D.M.; Salata, R.A. Polymicrobial bacteremia in the late 1980s: Predictors of outcome and review of the literature. Medicine 1990, 69, 114–123. [Google Scholar] [CrossRef]
- McKenzie, F.E. Case mortality in polymicrobial bloodstream infections. J. Clin. Epidemiol. 2006, 59, 760–761. [Google Scholar] [CrossRef]
- Pavlaki, M.; Poulakou, G.; Drimousis, P.; Adamis, G.; Apostolidou, E.; Gatselis, N.K.; Kritselis, I.; Mega, A.; Mylona, V.; Papatsoris, A.; et al. Polymicrobial bloodstream infections: Epidemiology and impact on mortality. J Glob Antimicrob Resist 2013, 1, 207–212. [Google Scholar] [CrossRef]
- Reuben, A.G.; Musher, D.M.; Hamill, R.J.; Broucke, I. Polymicrobial bacteremia: Clinical and microbiologic patterns. Rev. Infect. Dis. 1989, 11, 161–183. [Google Scholar] [CrossRef]
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter baumannii: Emergence of a successful pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef]
- Lee, Y.T.; Kuo, S.C.; Yang, S.P.; Lin, Y.T.; Tseng, F.C.; Chen, T.L.; Fung, C.P. Impact of appropriate antimicrobial therapy on mortality associated with Acinetobacter baumannii bacteremia: Relation to severity of infection. Clin. Infect. Dis. 2012, 55, 209–215. [Google Scholar] [CrossRef]
- Du, X.; Xu, X.; Yao, J.; Deng, K.; Chen, S.; Shen, Z.; Yang, L.; Feng, G. Predictors of mortality in patients infected with carbapenem-resistant Acinetobacter baumannii: A systematic review and meta-analysis. Am J. Infect. Control 2019, 47, 1140–1145. [Google Scholar] [CrossRef]
- Cisneros, J.M.; Reyes, M.J.; Pachon, J.; Becerril, B.; Caballero, F.J.; Garcia-Garmendia, J.L.; Ortiz, C.; Cobacho, A.R. Bacteremia due to Acinetobacter baumannii: Epidemiology, clinical findings, and prognostic features. Clin. Infect. Dis. 1996, 22, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Cisneros, J.M.; Rodriguez-Bano, J. Nosocomial bacteremia due to Acinetobacter baumannii: Epidemiology, clinical features and treatment. Clin. Microbiol. Infect. 2002, 8, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.T.; Kuo, S.C.; Lee, Y.T.; Chen, C.P.; Lin, S.W.; Shen, L.J.; Fung, C.P.; Cho, W.L.; Chen, T.L. Sheltering effect and indirect pathogenesis of carbapenem-resistant Acinetobacter baumannii in polymicrobial infection. Antimicrob. Agents Chemother. 2014, 58, 3983–3990. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Principles and procedures for blood cultures: Approved guideline; M47-A; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2007. [Google Scholar]
- Chen, H.P.; Chen, T.L.; Lai, C.H.; Fung, C.P.; Wong, W.W.; Yu, K.W.; Liu, C.Y. Predictors of mortality in Acinetobacter baumannii bacteremia. J. Microbiol. Immunol. Infect. 2005, 38, 127–136. [Google Scholar] [PubMed]
- Kuo, S.C.; Lee, Y.T.; Yang, S.P.; Chiang, M.C.; Lin, Y.T.; Tseng, F.C.; Chen, T.L.; Fung, C.P. Evaluation of the effect of appropriate antimicrobial therapy on mortality associated with Acinetobacter nosocomialis bacteraemia. Clin. Microbiol. Infect. 2013, 19, 634–639. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmermanm, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control 1988, 16, 128–140. [Google Scholar] [CrossRef]
- Chen, T.L.; Siu, L.K.; Wu, R.C.; Shaio, M.F.; Huang, L.Y.; Fung, C.P.; Lee, C.M.; Cho, W.L. Comparison of one-tube multiplex PCR, automated ribotyping and intergenic spacer (ITS) sequencing for rapid identification of Acinetobacter baumannii. Clin. Microbiol. Infect. 2007, 13, 801–806. [Google Scholar] [CrossRef]
- Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—9th ed. M07-A9; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012.
- Performance standards for antimicrobial susceptibility testing: 27th informational supplement M100-S27; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2017.
- Esterly, J.S.; Griffith, M.; Qi, C.; Malczynski, M.; Postelnick, M.J.; Scheetz, M.H. Impact of carbapenem resistance and receipt of active antimicrobial therapy on clinical outcomes of Acinetobacter baumannii bloodstream infections. Antimicrob. Agents Chemother. 2011, 55, 4844–4849. [Google Scholar] [CrossRef]
- Cheng, A.; Chuang, Y.C.; Sun, H.Y.; Sheng, W.H.; Yang, C.J.; Liao, C.H.; Hsueh, P.R.; Yang, J.L.; Shen, N.J.; Wang, J.T.; et al. Excess mortality associated with colistin-tigecycline compared with colistin-carbapenem combination therapy for extensively drug-resistant Acinetobacter baumannii bacteremia: A multicenter prospective observational study. Crit. Care Med. 2015, 43, 1194–1204. [Google Scholar] [CrossRef]
- Weinstein, M.P.; Towns, M.L.; Quartey, S.M.; Mirrett, S.; Reimer, L.G.; Parmigiani, G.; Reller, L.B. The clinical significance of positive blood cultures in the 1990s: A prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin. Infect. Dis. 1997, 24, 584–602. [Google Scholar] [CrossRef] [PubMed]
- Ilavska, I.; Pichna, P.; Stopkova, K.; Grausova, S.; Krupova, I.; Oravcova, E.; Koren, P.; Lacka, J.; Studena, M.; Spanik, S.; et al. Polymicrobial bacteremia in cancer patients: Analysis of risk factors, etiology and outcome in 214 episodes. Int. J. Antimicrob. Agents 1996, 7, 101–107. [Google Scholar] [CrossRef]
- Roberts, F.J.; Geere, I.W.; Coldman, A. A three-year study of positive blood cultures, with emphasis on prognosis. Rev. Infect. Dis. 1991, 13, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Park, K.H.; Bang, K.M.; Chong, Y.P.; Kim, S.H.; Lee, S.O.; Choi, S.H.; Jeong, J.Y.; Woo, J.H.; Kim, Y.S.; et al. Clinical significance and outcome of polymicrobial Staphylococcus aureus bacteremia. J. Infect. 2012, 65, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Tiseo, G.; Dentali, F.; Foglia, E.; Campanini, M.; Menichetti, F.; Mazzone, A. Early alert from the microbiology laboratory improves the outcome of elderly patients with Enterococcus spp. bloodstream infection: Results from a multicenter prospective study. J. Glob. Antimicrob. Resist. 2019, 18, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Aliaga, L.; Mediavilla, J.D.; Llosa, J.; Miranda, C.; Rosa-Fraile, M. Clinical significance of polymicrobial versus monomicrobial bacteremia involving Pseudomonas aeruginosa. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 871–874. [Google Scholar] [CrossRef]
- Liu, Q.; Wu, J.; Wang, Z.; Wu, X.; Wang, G.; Ren, J. Polymicrobial bacteremia involving Klebsiella pneumoniae in patients with complicated intra-abdominal infections: Frequency, co-pathogens, risk factors, and clinical outcomes. Surg. Infect. (Larchmt) 2019, 20, 317–325. [Google Scholar] [CrossRef]
- Peters, B.M.; Jabra-Rizk, M.A.; O’May, G.A.; Costerton, J.W.; Shirtliff, M.E. Polymicrobial interactions: Impact on pathogenesis and human disease. Clin. Microbiol. Rev. 2012, 25, 193–213. [Google Scholar] [CrossRef]
- Wang, Y.C.; Huang, T.W.; Yang, Y.S.; Kuo, S.C.; Chen, C.T.; Liu, C.P.; Liu, Y.M.; Chen, T.L.; Chang, F.Y.; Wu, S.H.; et al. Biofilm formation is not associated with worse outcome in Acinetobacter baumannii bacteremic pneumonia. Sci. Rep. 2018, 8, 7289. [Google Scholar] [CrossRef]
| Characteristic | All (n = 379) | Polymicrobial (n = 89) | Monomicrobial (n = 290) | p |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, years | 74 (60–81) | 78 (64–82.5) | 73 (59–81) | 0.012 |
| Male sex | 280 (73.9) | 66 (74.2) | 214 (73.8) | 1.000 |
| Community-onset | 20 (5.3) | 2 (2.2) | 18 (6.2) | 0.181 |
| Acquired in ICU | 189 (49.9) | 47 (52.8) | 142 (49.0) | 0.608 |
| Days of hospitalization before bacteremia | 18 (5–34) | 21 (4.5–48) | 16 (5.8–32) | 0.161 |
| Comorbidity | ||||
| Alcoholism | 30 (7.9) | 9 (10.1) | 21 (7.2) | 0.514 |
| Liver cirrhosis | 23 (6.1) | 5 (5.6) | 18 (6.2) | 1.000 |
| Chronic kidney disease | 90 (23.7) | 28 (31.5) | 62 (21.4) | 0.070 |
| Type 2 diabetes mellitus | 99 (26.1) | 20 (22.5) | 79 (27.2) | 0.448 |
| Chronic obstructive pulmonary disease | 68 (17.9) | 17 (19.1) | 51 (17.6) | 0.867 |
| Hypertension | 127 (33.5) | 31 (34.8) | 96 (33.1) | 0.862 |
| Coronary artery disease | 56 (14.8) | 22 (24.7) | 34 (11.7) | 0.004 |
| Congestive heart failure | 43 (11.3) | 13 (14.6) | 30 (10.3) | 0.359 |
| Cerebral vascular accident | 71 (18.7) | 17 (19.1) | 58 (20.0) | 0.973 |
| Collagen vascular disease | 18 (4.7) | 5 (5.6) | 13 (4.5) | 0.775 |
| Malignancy | 128 (33.8) | 28 (31.5) | 100 (34.5) | 0.690 |
| Neutropenia | 18 (4.7) | 4 (4.5) | 14 (4.8) | 1.000 |
| Chemotherapy | 39 (10.3) | 6 (6.7) | 33 (11.4) | 0.289 |
| Immunosuppressive therapy | 19 (5.0) | 4 (4.5) | 15 (5.2) | 1.000 |
| Recent surgery (within 4 weeks) | 126 (33.2) | 26 (29.2) | 100 (34.5) | 0.427 |
| Trauma | 11 (2.9) | 1 (1.1) | 10 (3.4) | 0.470 |
| Shock within 3 days | 15 (4.0) | 0 (0.0) | 15 (5.2) | 0.027 |
| APACHE II score within 24 h before bacteremia onset | 24 (18–31) | 24 (18.3–31) | 24 (27–31) | 0.820 |
| Invasive procedures a | ||||
| Abdominal drainage | 33 (8.7) | 3 (3.4) | 30 (10.3) | 0.068 |
| Arterial catheter | 76 (20.1) | 15 (16.9) | 61 (21.0) | 0.478 |
| Central venous catheter | 196 (51.7) | 51 (57.3) | 145 (50.2) | 0.291 |
| Foley catheter | 221 (58.3) | 53 (59.6) | 168 (57.9) | 0.882 |
| Hemodialysis | 27 (7.1) | 8 (9.0) | 19 (6.6) | 0.585 |
| Nasogastric tube | 255 (67.3) | 63 (70.8) | 192 (66.2) | 0.499 |
| Pulmonary artery catheter | 41 (10.8) | 7 (7.9) | 34 (11.7) | 0.406 |
| Total parental nutrition | 27 (7.1) | 2 (2.2) | 25 (8.6) | 0.070 |
| Tracheotomy | 46 (12.1) | 16 (18.0) | 30 (10.3) | 0.081 |
| Ventilator | 192 (50.7) | 51 (57.3) | 141 (48.6) | 0.190 |
| Infection source b | ||||
| Respiratory tract | 213 (56.2) | 54 (60.7) | 159 (54.8) | 0.395 |
| Urinary tract | 31 (8.2) | 4 (4.5) | 27 (9.3) | 0.219 |
| Catheter-related | 35 (9.2) | 11 (12.4) | 24 (8.3) | 0.340 |
| Intra-abdomen | 26 (6.9) | 3 (3.4) | 23 (7.9) | 0.212 |
| Soft tissue or wound | 12 (3.2) | 4 (4.5) | 8 (2.8) | 0.487 |
| Primary bacteremia | 71 (18.7) | 16 (18.0) | 55 (19.0) | 0.957 |
| Resistance profiles of the bloodstream isolate | ||||
| Multidrug resistance | 265 (69.9) | 66 (74.2) | 199 (68.6) | 0.387 |
| Carbapenem resistance | 91 (24.0) | 19 (21.3) | 72 (24.8) | 0.596 |
| Appropriate antimicrobial therapy | 124 (32.7) | 12 (13.5) | 112 (38.6) | <0.001 |
| 14-day mortality | 104 (27.4) | 26 (29.2) | 78 (26.9) | 0.770 |
| 30-day mortality | 135 (35.6) | 34 (38.2) | 101 (34.8) | 0.561 |
| Demographic or Characteristic | Univariable Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| Chronic kidney disease | 1.617 (0.946–2.765) | 0.079 | ||
| Coronary artery disease | 1.735 (0.956–3.148) | 0.070 | ||
| Malignancy | 1.667 (1.046–2.657) | 0.032 | 2.554 (1.373–4.753) | 0.003 |
| Neutropenia | 3.551 (1.361–9.263) | 0.010 | ||
| Recent surgery (within 4 weeks) | 0.410 (0.239–0.701) | 0.001 | ||
| Shock within 3 days | 4.081 (2.386–6.981) | <0.001 | 2.430 (1.220–4.843) | 0.012 |
| APACHE II score | 1.169 (1.129–1.210) | <0.001 | 1.173 (1.130–1.216) | <0.001 |
| Arterial catheter | 2.170 (1.280–3.680) | 0.004 | ||
| Central venous catheter | 1.682 (1.060–2.668) | 0.027 | ||
| Foley catheter | 2.285 (1.400–3.729) | 0.001 | ||
| Nasogastric tube | 2.198 (1.293–3.735) | 0.004 | ||
| Ventilator | 2.054 (1.291–3.267) | 0.002 | ||
| Respiratory tract infection | 2.015 (1.252–3.243) | 0.004 | ||
| Urinary tract infection | 0.262 (0.078–0.881) | 0.030 | ||
| Appropriate antimicrobial therapy | 0.525 (0.313–0.881) | 0.015 | 0.317 (0.162–0.621) | 0.001 |
| Polymicrobial bacteremia | 1.122 (0.663–1.897) | 0.668 | ||
| Concomitantly Isolated Bacterial Species | No. (%) of Patients | APACHE II Score, Mean (Interquartile Range) | No. (%) of Patients | ||
|---|---|---|---|---|---|
| Appropriate Antimicrobial Therapy | Concomitant MDR/CR A. baumannii | 14-Day Non-Survival | |||
| Gram-positive cocci (GPC) | 47 (52.8) | 23 (18–28) | 5 (10.6) | 39/8 (83.0/17.0) | 9 (19.1) |
| Coagulase-negative staphylococci (CNS) | 20 (22.5) | 18.5 (11.25–25.75) | 1 (5.0) | 15/3 (78.0/15.0) | 2 (10.0) |
| Enterococcus spp. | 12 (13.5) | 24.5 (18.5–37.75) | 2 (16.7) | 10/0 (83.3/0) | 3 (25.0) |
| Staphylococcus aureus | 4 (4.5) | 24.5 (22–35.25) | 1 (25.0) | 4/2 (100.0/50.0) | 1 (25.0) |
| Enterococcus spp. + S. aureus | 4 (4.5) | 26.5 (9.25–28.75) | 0 (0) | 3/1 (75.0/25.0) | 0 (0) |
| CNS + S. aureus | 2 (2.3) | 19, 24 | 0 (0) | 1/1 (50.0/50.0) | 0 (0) |
| Other GPCa | 5 (5.6) | 25 (22.5–30.5) | 1 (20.0) | 5/1 (100.0/20.0) | 3 (60.0) |
| Gram-negative bacilli (GNB) | 36 (40.5) | 24 (19–35) | 6 (16.7) | 23/10 (63.9/27.8) | 14 (38.9) |
| Pseudomonas aeruginosa | 8 (9.0) | 33.5 (18.25–38.75) | 2 (25.0) | 6/2 (75.0/25.0) | 4 (50.0) |
| Enterobacter spp. | 8 (9.0) | 26 (22.25–40) | 1 (12.5) | 5/2 (62.5/25.0) | 3 (37.5) |
| Escherichia coli | 7 (7.9) | 31 (24–39) | 1 (14.3) | 6/2 (85.7/28.6) | 5 (71.4) |
| Klebsiella pneumoniae | 6 (6.7) | 20 (17.5–31.5) | 0 (0) | 3/1 (50.0/16.7) | 1 (16.7) |
| Other GNBb | 7 (7.9) | 18 (10–27) | 2 (28.6) | 4/4 (42.9/42.9) | 1 (14.3) |
| Yeastc | 3 (3.4) | 18, 23, 33 | 1 (33.3) | 2/1 (66.7/33.3) | 1 (33.3) |
| Mixed GNB and GPC | 3 (3.4) | 19, 24, 47 | 0 (0) | 2/0 (66.7/0) | 2 (66.7) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.-C.; Ku, W.-W.; Yang, Y.-S.; Kao, C.-C.; Kang, F.-Y.; Kuo, S.-C.; Chiu, C.-H.; Chen, T.-L.; Wang, F.-D.; Lee, Y.-T. Is Polymicrobial Bacteremia an Independent Risk Factor for Mortality in Acinetobacter baumannii Bacteremia? J. Clin. Med. 2020, 9, 153. https://doi.org/10.3390/jcm9010153
Wang Y-C, Ku W-W, Yang Y-S, Kao C-C, Kang F-Y, Kuo S-C, Chiu C-H, Chen T-L, Wang F-D, Lee Y-T. Is Polymicrobial Bacteremia an Independent Risk Factor for Mortality in Acinetobacter baumannii Bacteremia? Journal of Clinical Medicine. 2020; 9(1):153. https://doi.org/10.3390/jcm9010153
Chicago/Turabian StyleWang, Yung-Chih, Wen-Wei Ku, Ya-Sung Yang, Chih-Chun Kao, Fang-Yu Kang, Shu-Chen Kuo, Chun-Hsiang Chiu, Te-Li Chen, Fu-Der Wang, and Yi-Tzu Lee. 2020. "Is Polymicrobial Bacteremia an Independent Risk Factor for Mortality in Acinetobacter baumannii Bacteremia?" Journal of Clinical Medicine 9, no. 1: 153. https://doi.org/10.3390/jcm9010153
APA StyleWang, Y.-C., Ku, W.-W., Yang, Y.-S., Kao, C.-C., Kang, F.-Y., Kuo, S.-C., Chiu, C.-H., Chen, T.-L., Wang, F.-D., & Lee, Y.-T. (2020). Is Polymicrobial Bacteremia an Independent Risk Factor for Mortality in Acinetobacter baumannii Bacteremia? Journal of Clinical Medicine, 9(1), 153. https://doi.org/10.3390/jcm9010153





