Ventilator-Associated Pneumonia and PaO2/FIO2 Diagnostic Accuracy: Changing the Paradigm?
Abstract
:1. Introduction
2. Methods (Extended Information is Provided in Supplementary Materials)
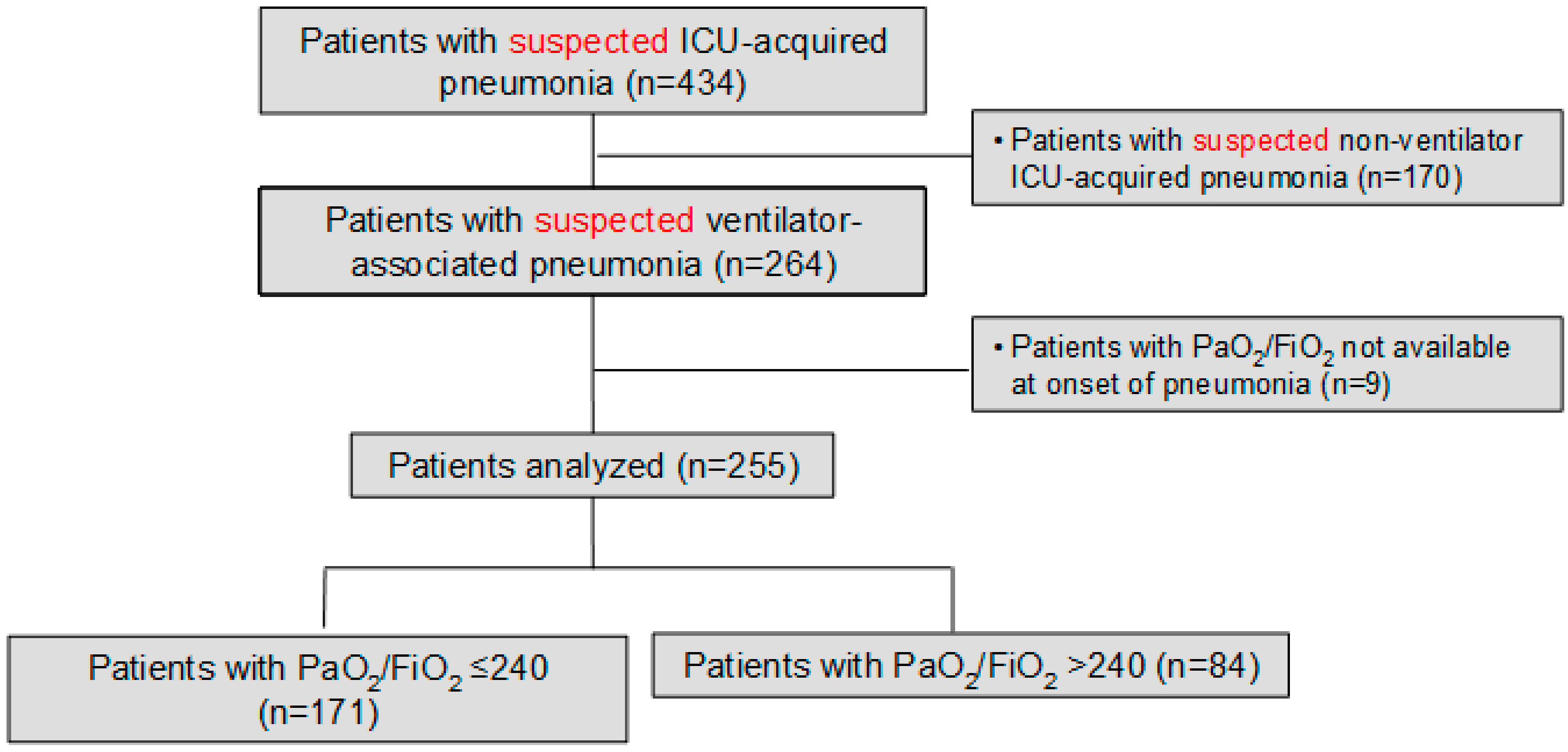
2.1. Study Population
2.2. Definition of Pneumonia, Microbiologic Processing, and Antimicrobial Treatment
2.3. Assessment of the Systemic Inflammatory Response
2.4. Data Collection
2.5. Outcomes Variables
2.6. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Microbiological Aetiology
3.3. Systemic Inflammatory Response
3.4. Empiric Antibiotic Treatment and Outcome Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef] [PubMed]
- Kalanuria, A.A.; Ziai, W.; Zai, W.; Mirski, M. Ventilator-associated pneumonia in the ICU. Crit Care 2014, 18, 208. [Google Scholar] [CrossRef] [PubMed]
- Timsit, J.-F.; Esaied, W.; Neuville, M.; Bouadma, L.; Mourvllier, B. Update on ventilator-associated pneumonia. F1000Res 2017, 6, 2061. [Google Scholar] [CrossRef] [PubMed]
- Van Vught, L.A.; Klein Klouwenberg, P.M.C.; Spitoni, C.; Scicluna, B.P.; Wiewel, M.A.; Horn, J.; Schultz, M.J.; Nürnberg, P.; Bonten, M.J.M.; Cremer, O.L.; et al. Incidence, Risk Factors, and Attributable Mortality of Secondary Infections in the Intensive Care Unit After Admission for Sepsis. JAMA 2016, 315, 1469–1479. [Google Scholar] [CrossRef] [PubMed]
- Metersky, M.L.; Wang, Y.; Klompas, M.; Eckenrode, S.; Bakullari, A.; Eldridge, N. Trend in Ventilator-Associated Pneumonia Rates Between 2005 and 2013. JAMA 2016, 316, 2427–2429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pugin, J.; Auckenthaler, R.; Mili, N.; Janssens, J.P.; Lew, P.D.; Suter, P.M. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am. Rev. Respir. Dis. 1991, 143, 1121–1129. [Google Scholar] [CrossRef]
- Shan, J.; Chen, H.-L.; Zhu, J.-H. Diagnostic accuracy of clinical pulmonary infection score for ventilator-associated pneumonia: A meta-analysis. Respir. Care 2011, 56, 1087–1094. [Google Scholar] [CrossRef]
- Zilberberg, M.D.; Shorr, A.F. Ventilator-associated pneumonia: The clinical pulmonary infection score as a surrogate for diagnostics and outcome. Clin. Infect. Dis. 2010, 51 (Suppl. 1), S131–S135. [Google Scholar] [CrossRef]
- FAQs: Pneumonia (PNEU) Events | NHSN | CDC. Available online: https://www.cdc.gov/nhsn/faqs/faq-pneu.html (accessed on 8 January 2019).
- Chastre, J.; Fagon, J.-Y. Ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 2002, 165, 867–903. [Google Scholar] [CrossRef]
- Hilbert, G.; Gruson, D.; Vargas, F.; Valentino, R.; Gbikpi-Benissan, G.; Dupon, M.; Reiffers, J.; Cardinaud, J.P. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N. Engl. J. Med. 2001, 344, 481–487. [Google Scholar] [CrossRef]
- Fàbregas, N.; Ewig, S.; Torres, A.; El-Ebiary, M.; Ramirez, J.; de La Bellacasa, J.P.; Bauer, T.; Cabello, H. Clinical diagnosis of ventilator associated pneumonia revisited: Comparative validation using immediate post-mortem lung biopsies. Thorax 1999, 54, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Woodhead, M.; Torres, A. Definition and Classification of Community-Acquired and Nosocomial Pneumonias; European Respiratory Society Journals Ltd.: Lausanne, Switzerland, 1997. [Google Scholar]
- Meduri, G.U.; Chastre, J. The standardization of bronchoscopic techniques for ventilator-associated pneumonia. Chest 1992, 102, 557S–564S. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H.; Bock, K.R.; Richards, R.D.; Hearns, M.L. The safety and diagnostic accuracy of minibronchoalveolar lavage in patients with suspected ventilator-associated pneumonia. Ann. Intern. Med. 1995, 122, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, M.; Torres, A.; Ewig, S.; Marcos, M.A.; Alcón, A.; Lledó, R.; Asenjo, M.A.; Maldonaldo, A. Noninvasive versus invasive microbial investigation in ventilator-associated pneumonia: Evaluation of outcome. Am. J. Respir. Crit. Care Med. 2000, 162, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Van Saene, H.K.F.; Petros, A.J.; Ramsay, G.; Baxby, D. All great truths are iconoclastic: Selective decontamination of the digestive tract moves from heresy to level 1 truth. Intensive Care Med. 2003, 29, 677–690. [Google Scholar] [CrossRef] [PubMed]
- Ioanas, M.; Cavalcanti, M.; Ferrer, M.; Valencia, M.; Agusti, C.; Puig de la Bellacasa, J.; Torres, A. Hospital-acquired pneumonia: Coverage and treatment adequacy of current guidelines. Eur. Respir. J. 2003, 22, 876–882. [Google Scholar] [CrossRef] [PubMed]
- Valencia Arango, M.; Torres Martí, A.; Insausti Ordeñana, J.; Alvarez Lerma, F.; Carrasco Joaquinet, N.; Herranz Casado, M.; Tirapu León, J.P.; Grupo de Estudio de la Neumonía Relacionada con Ventilación Mecánica; Grupo de Trabajo de Enfermedades Infecciosas de la SEMICYUC. Diagnostic value of quantitative cultures of endotracheal aspirate in ventilator-associated pneumonia: A multicenter study. Arch. Bronconeumol. 2003, 39, 394–399. [Google Scholar]
- Murray, P.R.; Baron, E.J.; Joergensen, J.H.; Pfaller, M.A.; Yolken, R.H. Manual of Clinical Microbiology, 8th ed.; American Society for Microbiology: Washington, DC, USA, 2003. [Google Scholar]
- American Thoracic Society; Infectious Diseases Society of America Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [CrossRef]
- Heyland, D.K.; Dodek, P.; Muscedere, J.; Day, A.; Cook, D.; Canadian Critical Care Trials Group. Randomized trial of combination versus monotherapy for the empiric treatment of suspected ventilator-associated pneumonia. Crit. Care Med. 2008, 36, 737–744. [Google Scholar] [CrossRef]
- Ioanas, M.; Ferrer, M.; Cavalcanti, M.; Ferrer, R.; Ewig, S.; Filella, X.; de la Bellacasa, J.P.; Torres, A. Causes and predictors of nonresponse to treatment of intensive care unit-acquired pneumonia. Crit. Care Med. 2004, 32, 938–945. [Google Scholar] [CrossRef]
- Esperatti, M.; Ferrer, M.; Giunta, V.; Ranzani, O.T.; Saucedo, L.M.; Li Bassi, G.; Blasi, F.; Rello, J.; Niederman, M.S.; Torres, A. Validation of predictors of adverse outcomes in hospital-acquired pneumonia in the ICU. Crit. Care Med. 2013, 41, 2151–2161. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, P.; Ferrer, M.; Martí, V.; Reyes, S.; Martínez, R.; Menéndez, R.; Ewig, S.; Torres, A. Inflammatory biomarkers and prediction for intensive care unit admission in severe community-acquired pneumonia. Crit. Care Med. 2011, 39, 2211–2217. [Google Scholar] [CrossRef] [PubMed]
- Bello, S.; Lasierra, A.B.; Mincholé, E.; Fandos, S.; Ruiz, M.A.; Vera, E.; de Pablo, F.; Ferrer, M.; Menendez, R.; Torres, A. Prognostic power of proadrenomedullin in community-acquired pneumonia is independent of aetiology. Eur. Respir. J. 2012, 39, 1144–1155. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- FAQs: Ventilator-Associated (VAE) Events | NHSN | CDC. Available online: https://www.cdc.gov/nhsn/faqs/faq-vae.html (accessed on 8 January 2019).
- Magill, S.S.; Klompas, M.; Balk, R.; Burns, S.M.; Deutschman, C.S.; Diekema, D.; Fridkin, S.; Greene, L.; Guh, A.; Gutterman, D.; et al. Developing a new, national approach to surveillance for ventilator-associated events*. Crit. Care Med. 2013, 41, 2467–2475. [Google Scholar] [CrossRef] [PubMed]
- Ewig, S.; Torres, A.; Angeles Marcos, M.; Angrill, J.; Rañó, A.; de Roux, A.; Mensa, J.; Martínez, J.A.; de la Bellacasa, J.P.; Bauer, T. Factors associated with unknown aetiology in patients with community-acquired pneumonia. Eur. Respir. J. 2002, 20, 1254–1262. [Google Scholar] [CrossRef]
- Giunta, V.; Ferrer, M.; Esperatti, M.; Ranzani, O.T.; Saucedo, L.M.; Li Bassi, G.; Blasi, F.; Torres, A. ICU-acquired pneumonia with or without etiologic diagnosis: A comparison of outcomes. Crit. Care Med. 2013, 41, 2133–2143. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Luna, C.M.; Blanzaco, D.; Niederman, M.S.; Matarucco, W.; Baredes, N.C.; Desmery, P.; Palizas, F.; Menga, G.; Rios, F.; Apezteguia, C. Resolution of ventilator-associated pneumonia: Prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit. Care Med. 2003, 31, 676–682. [Google Scholar] [CrossRef]
- Torres, A.; Niederman, M.S.; Chastre, J.; Ewig, S.; Fernandez-Vandellos, P.; Hanberger, H.; Kollef, M.; Bassi, G.L.; Luna, C.M.; Martin-Loeches, I.; et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). Eur. Respir. J. 2017, 50, 1700582. [Google Scholar] [PubMed]
- Martin-Loeches, I.; Deja, M.; Koulenti, D.; Dimopoulos, G.; Marsh, B.; Torres, A.; Niederman, M.S.; Rello, J. EU-VAP Study Investigators Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: The interaction of ecology, shock and risk factors. Intensive Care Med. 2013, 39, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Martin-Loeches, I.; Povoa, P.; Rodríguez, A.; Curcio, D.; Suarez, D.; Mira, J.-P.; Cordero, M.L.; Lepecq, R.; Girault, C.; Candeias, C.; et al. Incidence and prognosis of ventilator-associated tracheobronchitis (TAVeM): A multicentre, prospective, observational study. Lancet Respir. Med. 2015, 3, 859–868. [Google Scholar] [CrossRef]
- Ferrer, M.; Travierso, C.; Cilloniz, C.; Gabarrus, A.; Ranzani, O.T.; Polverino, E.; Liapikou, A.; Blasi, F.; Torres, A. Severe community-acquired pneumonia: Characteristics and prognostic factors in ventilated and non-ventilated patients. PLoS ONE 2018, 13, e0191721. [Google Scholar] [CrossRef] [PubMed]
- Martin-Loeches, I.; Levy, M.M.; Artigas, A. Management of severe sepsis: Advances, challenges, and current status. Drug Des. Devel. Ther. 2015, 9, 2079–2088. [Google Scholar] [CrossRef] [PubMed]
- Esperatti, M.; Ferrer, M.; Theessen, A.; Liapikou, A.; Valencia, M.; Saucedo, L.M.; Zavala, E.; Welte, T.; Torres, A. Nosocomial pneumonia in the intensive care unit acquired by mechanically ventilated versus nonventilated patients. Am. J. Respir. Crit. Care Med. 2010, 182, 1533–1539. [Google Scholar] [CrossRef] [PubMed]
| PaO2/FIO2 ≤ 240 n = 171 | PaO2/FIO2 > 240 n = 84 | p Value | |
|---|---|---|---|
| Age, year | 62 ± 16 | 61 ± 15 | 0.57 |
| Sex, male/female, n | 116/55 | 60/24 | 0.56 |
| Alcohol abuse (current or former), n (%) | 41 (24) | 18 (21) | 0.63 |
| Smoking habit (current or former), n (%) | 90 (53) | 40 (48) | 0.45 |
| APACHE-II score | 17 ± 6 | 19 ± 8 | 0.044 |
| SAPS score | 42 ± 15 | 45 ± 16 | 0.24 |
| SOFA score | 8 ± 3 | 8 ± 3 | 0.71 |
| Co-morbidities, n (%) | |||
| Diabetes mellitus | 41 (24) | 19 (23) | 0.81 |
| Chronic renal failure | 15 (9) | 5 (6) | 0.43 |
| Solid cancer | 19 (11) | 10 (12) | 0.85 |
| Chronic heart disorders | 54 (32) | 28 (33) | 0.78 |
| Chronic lung disease | 58 (34) | 30 (24) | 0.10 |
| Chronic liver disease | 27 (16) | 9 (11) | 0.27 |
| Recent surgery, n (%) | 81 (47) | 43 (51) | 0.57 |
| Tracheotomy at admission, n (%) | 16 (9) | 11 (13) | 0.37 |
| Causes of ICU admission, n (%) | 0.051 | ||
| Post-operative | 40 (23) | 13 (16) | |
| Hypoxemic respiratory failure | 20 (12) | 5 (6) | |
| Decreased consciousness | 31 (18) | 17 (20) | |
| Hypercapnic respiratory failure | 16 (9) | 5 (6) | |
| Septic shock | 12 (7) | 10 (12) | |
| Multiple trauma | 12 (7) | 16 (19) | |
| Non-surgical abdominal disease | 5 (3) | 3 (4) | |
| Acute coronary syndrome | 10 (6) | 2 (2) | |
| Cardiac arrest | 12 (7) | 9 (11) | |
| Other | 6 (4) | 4 (5) |
| PaO2/FIO2 ≤ 240 n = 171 | PaO2/FIO2 > 240 n = 84 | p Value | |
|---|---|---|---|
| Previous antibiotics, n (%) | 139 (81) | 66 (79) | 0.61 |
| Most frequent groups, n (%): | |||
| Penicillins | 78 (46) | 26 (31) | |
| Cephalosporins | 50 (29) | 26 (31) | |
| Quinolones | 48 (28) | 20 (24) | |
| Carbapenems | 23 (13) | 14 (17) | |
| Glycopeptides | 28 (16) | 9 (11) | |
| Aminoglycosides | 15 (9) | 11 (13) | |
| Clindamycin | 14 (8) | 11 (13) | |
| Antifungals | 6 (4) | 2 (2) | |
| Hospital stay before pneumonia, days * | 7 (4–13) | 7 (5–15) | 0.34 |
| ICU stay before pneumonia, days * | 5 (3–9) | 6 (4–10) | 0.12 |
| SOFA score | 8 ± 3 | 7 ± 3 | 0.004 |
| Bilateral pulmonary infiltrates, n (%) | 55 (32) | 19 (23) | 0.11 |
| ARDS criteria, n (%) | 32 (19) | 1 (1) | <0.001 |
| Pleural effusion, n (%) | 56 (33) | 18 (22) | 0.10 |
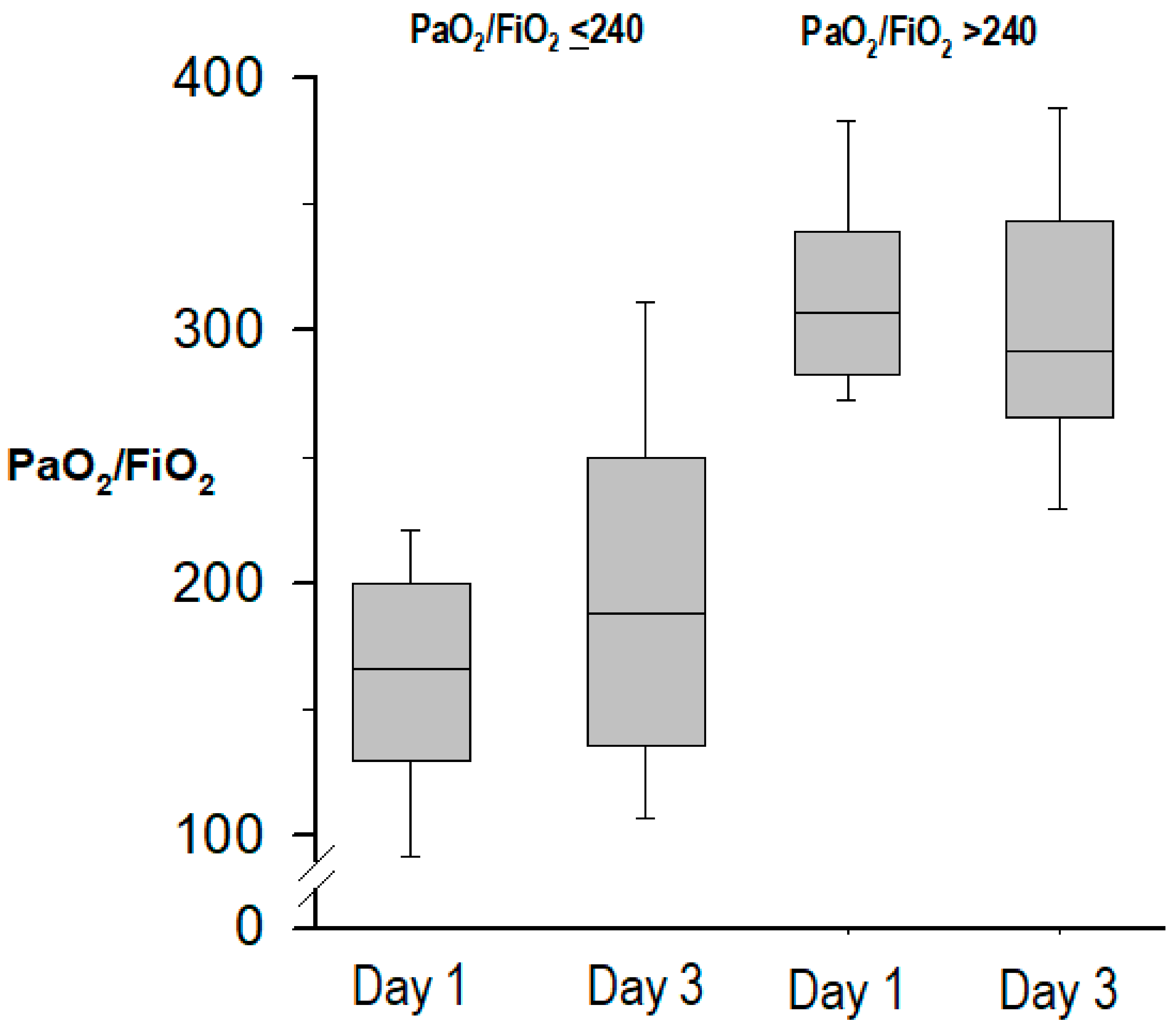
| PaO2/FiO2 | 161 ± 47 | 301 ± 49 | <0.001 |
| FiO2 | 0.55 ± 0.18 | 0.41 ± 11 | <0.001 |
| PEEP, cmH2O | 7.4 ±3.4 | 7.8 ± 3.0 | 0.36 |
| PaCO2, mmHg | 41 ± 9 | 39 ± 7 | 0.066 |
| pHa | 7.40 ± 0.09 | 7.41 ± 0.07 | 0.33 |
| Shock at onset of pneumonia, n (%) | 96 (56) | 32 (38) | 0.007 |
| Temperature | 36.9 ± 1.4 | 37.0 ± 1.3 | 0.37 |
| Serum creatinine, mg/dL | 1.3 ± 1.0 | 1.2 ± 1.2 | 0.85 |
| Blood haemoglobin, g/L | 11 ± 2 | 10 ± 2 | 0.67 |
| White blood cell count, L−9 | 14 ± 7 | 13 ± 6 | 0.11 |
| Sodium, mEq/L | 139 ± 6 | 141 ± 8 | 0.042 |
| Potassium, mEq/L | 4.0 ± 0.7 | 4.1 ± 0.5 | 0.75 |
| CPIS day 1 | 7 ± 1 | 5 ± 1 | <0.001 |
| CPIS day 3 | 6 ± 2 | 5 ± 2 | <0.001 |
| Pathogen | PaO2/FIO2 ≤ 240 n = 171 | PaO2/FIO2 > 240 n = 84 | p Value |
|---|---|---|---|
| Sample processed for microbiology, n (%) | |||
| Endotracheal aspirates | 157 (92) | 79 (94) | 0.52 |
| Bonchoalveolar lavage | 38 (23) | 21 (25) | 0.62 |
| Blood | 126 (74) | 58 (69) | 0.44 |
| Pleural fluid | 18 (11) | 5 (6) | 0.23 |
| Positive microbiology, n (%) | 117 (69) | 71 (85) | 0.007 |
| Gram-positive bacteria, n (%) | 37 (32) | 23 (32) | 0.96 |
| MS Staphylococcus aureus | 18 (15) | 17 (24) | 0.20 |
| MR Staphylococcus aureus | 12 (10) | 4 (6) | 0.41 |
| Streptococcus pneumoniae | 8 (7) | 2 (3) | 0.39 |
| Gram-negative enteric bacteria, n (%) | 39 (33) | 16 (23) | 0.16 |
| Enterobacter spp | 7 (6) | 2 (3) | 0.53 |
| Klebsiella spp | 11 (9) | 6 (9) | 0.78 |
| Escherichia coli | 9 (8) | 2 (3) | 0.62 |
| Proteus spp | 2 (2) | 2 (3) | 0.99 |
| Citrobacter spp | 3 (3) | 3 (4) | 0.84 |
| Serratia spp | 8 (7) | 4 (6) | 0.97 |
| Morganella morganii | 1 (1) | 0 (0) | 0.80 |
| Non-fermentating gram-negative bacilli | 38 (32) | 29 (41) | 0.32 |
| Stenotrophomonas maltophilia | 7 (6) | 3 (4) | 0.85 |
| Pseudomonas aeruginosa | 31 (27) | 26 (37) | 0.19 |
| Other gram-negative bacteria | |||
| Moraxella catarrhalis | 2 (2) | 0 (0) | 0.71 |
| Haemophilus influenzae | 3 (3) | 4 (6) | 0.50 |
| Fungi, n (%) | 2 (2) | 1 (1) | 0.66 |
| Aspergillus spp | 2 (2) | 1 (1) | 0.66 |
| Others, n (%) | 0 (0) | 1 (5) | - |
| Polymicrobial aetiology * | 19 (11) | 9 (11) | 0.91 |
| n† | PaO2/FIO2 ≤ 240 n = 171 | n† | PaO2/FIO2 > 240 n = 84 | p Value | |
|---|---|---|---|---|---|
| C-reactive protein day 1, mg/dL | 164 | 13 (6–21) | 81 | 11 (4–19) | 0.13 |
| C-reactive protein day 3, mg/dL | 149 | 11 (4–19) | 78 | 9 (5–15) | 0.078 |
| IL-6 day 1, pg/mL | 89 | 168 (72–431) | 36 | 109 (41–229) | 0.077 |
| IL-6 day 3, pg/mL | 75 | 91 (19–204) | 32 | 78 (33–183) | 0.98 |
| IL-8 day 1, pg/mL | 89 | 108 (64–214) | 36 | 94 (57–137) | 0.17 |
| IL-8 day 3, pg/mL | 75 | 76 (41–145) | 32 | 99 (63–170) | 0.15 |
| TNF-alpha day 1, pg/mL | 89 | 8 (5–17) | 36 | 7 (5–14) | 0.73 |
| TNF-alpha day 3, pg/mL | 75 | 7 (4–14) | 32 | 8 (5–15) | 0.61 |
| Procalcitonin day 1, ng/mL | 90 | 0.45 (0.14–1.37) | 37 | 0.19 (0.07–0.59) | 0.037 |
| Procalcitonin day 3, ng/mL | 78 | 0.30 (0.10–1.06) | 34 | 0.20 (0.08–0.74) | 0.57 |
| MR-proADM day 1, nmol/L | 98 | 1.27 (0.33–2.22) | 40 | 1.16 (0.65–2.23) | 0.84 |
| MR-proADM day 3, nmol/L | 87 | 1.36 (0.38–2.37) | 37 | 1.08 (0.61–2.04) | 0.92 |
| PaO2/FIO2 ≤ 240 n = 171 | PaO2/FIO2 > 240 n = 84 | p Value | |
|---|---|---|---|
| ICU stay, days * | 19 (12–29) | 18 (13–32) | 0.75 |
| Hospital stay, days * | 34 (19–56) | 43 (21–56) | 0.34 |
| Non-response to treatment, n (%) | 94 (55) | 48 (57) | 0.74 |
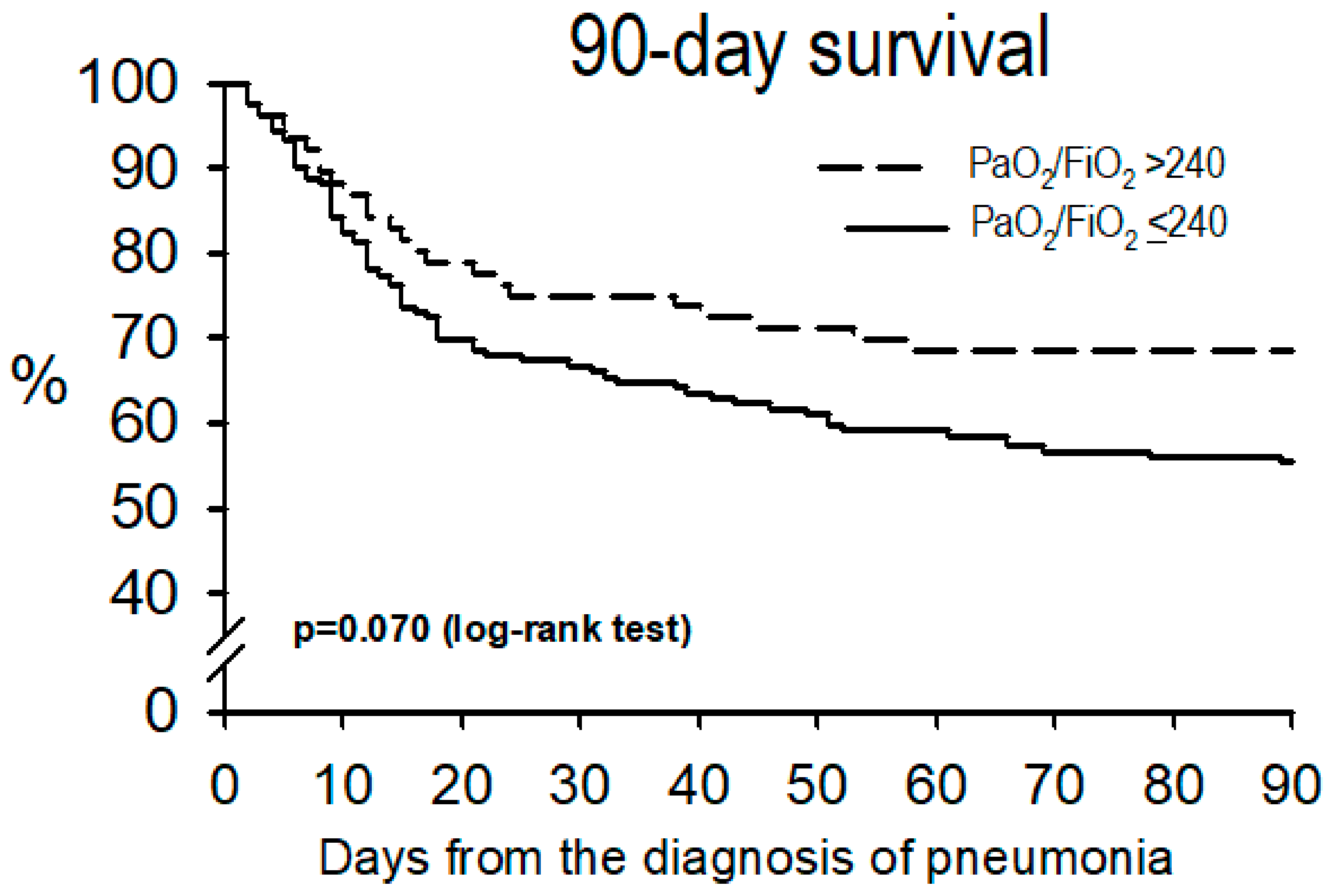
| ICU mortality, n (%) | 53 (31) | 18 (24) | 0.11 |
| Hospital mortality, n (%) | 71 (42) | 24 (29) | 0.044 |
| Ventilator-free days at day 28 * | 3 (0–21) | 17 (0–24) | 0.022 |
| Causes of death within 90 days: | 0.28 | ||
| Shock, n (%) | 52 (74) | 14 (58) | |
| Refractory hypoxemia, n (%) | 4 (6) | 2 (8) | |
| Order do-not-resuscitate, n (%) | 1 (1) | 2 (8) | |
| Brain anoxia, n (%) | 11 (16) | 6 (25) | |
| Others, n (%) | 2 (3) | 0 (0) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrer, M.; Sequeira, T.; Cilloniz, C.; Dominedo, C.; Li Bassi, G.; Martin-Loeches, I.; Torres, A. Ventilator-Associated Pneumonia and PaO2/FIO2 Diagnostic Accuracy: Changing the Paradigm? J. Clin. Med. 2019, 8, 1217. https://doi.org/10.3390/jcm8081217
Ferrer M, Sequeira T, Cilloniz C, Dominedo C, Li Bassi G, Martin-Loeches I, Torres A. Ventilator-Associated Pneumonia and PaO2/FIO2 Diagnostic Accuracy: Changing the Paradigm? Journal of Clinical Medicine. 2019; 8(8):1217. https://doi.org/10.3390/jcm8081217
Chicago/Turabian StyleFerrer, Miquel, Telma Sequeira, Catia Cilloniz, Cristina Dominedo, Gianluigi Li Bassi, Ignacio Martin-Loeches, and Antoni Torres. 2019. "Ventilator-Associated Pneumonia and PaO2/FIO2 Diagnostic Accuracy: Changing the Paradigm?" Journal of Clinical Medicine 8, no. 8: 1217. https://doi.org/10.3390/jcm8081217
APA StyleFerrer, M., Sequeira, T., Cilloniz, C., Dominedo, C., Li Bassi, G., Martin-Loeches, I., & Torres, A. (2019). Ventilator-Associated Pneumonia and PaO2/FIO2 Diagnostic Accuracy: Changing the Paradigm? Journal of Clinical Medicine, 8(8), 1217. https://doi.org/10.3390/jcm8081217








