The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms
Abstract
1. Introduction
2. Methods
2.1. Setting, Study Design, and Patients
2.2. Data Collection
2.3. Clinical Data and Definitions
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Schwarz, E.M.; Parvizi, J.; Gehrke, T.; Aiyer, A.; Battenberg, A.; Brown, S.A.; Callaghan, J.J.; Citak, M.; Egol, K.; Garrigues, G.E.; et al. 2018 International Consensus Meeting on Musculoskeletal Infection: Research Priorities from the General Assembly Questions. J. Orthop. Res. 2019, 37, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Peel, T.N. Studying Biofilm and Clinical Issues in Orthopedics. Front. Microbiol. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Saeed, K.; McLaren, A.C.; Schwarz, E.M.; Antoci, V.; Arnold, W.V.; Chen, A.F.; Clauss, M.; Esteban, J.; Gant, V.; Hendershot, E.; et al. 2018 International Consensus Meeting on Musculoskeletal Infection: Summary from the biofilm workgroup and consensus on biofilm related musculoskeletal infections. J. Orthop. Res. 2019, 37, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, W.; Sendi, P. Orthopaedic biofilm infections. APMIS 2017, 125, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Tande, A.J.; Gomez-Urena, E.O.; Berbari, E.F.; Osmon, D.R. Management of prosthetic joint infection. Infect. Dis. Clin. North Am. 2017, 31, 237–252. [Google Scholar] [CrossRef]
- Ariza, J.; Cobo, J.; Baraia-Etxaburu, J.; Benito, N.; Bori, G.; Cabo, J.; Corona, P.; Esteban, J.; Horcajada, J.P.; Lora-Tamayo, J.; et al. Executive summary of management of prosthetic joint infections. Clinical practice guidelines by the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). Enferm. Infecc. Microbiol. Clin. 2017, 35, 189–195. [Google Scholar] [CrossRef]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Infectious Diseases Society of America Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 2013, 56, e1–e25. [Google Scholar] [CrossRef]
- Tande, A.J.; Patel, R. Prosthetic Joint Infection. Clin. Microbiol. Rev. 2014, 27, 302–345. [Google Scholar] [CrossRef]
- Sendi, P.; Zimmerli, W. Antimicrobial treatment concepts for orthopaedic device-related infection. Clin. Microbiol. Infect. 2012, 18, 1176–1184. [Google Scholar] [CrossRef]
- Leekha, S.; Terrell, C.L.; Edson, R.S. General principles of antimicrobial therapy. Mayo Clin. Proc. 2011, 86, 156–167. [Google Scholar] [CrossRef]
- Peel, T.N.; Cheng, A.C.; Choong, P.F.M.; Buising, K.L. Early onset prosthetic hip and knee joint infection: treatment and outcomes in Victoria, Australia. J. Hosp. Infect. 2012, 82, 248–253. [Google Scholar] [CrossRef]
- Triffault-Fillit, C.; Ferry, T.; Laurent, F.; Pradat, P.; Dupieux, C.; Conrad, A.; Becker, A.; Lustig, S.; Fessy, M.H.; Chidiac, C.; et al. Microbiologic epidemiology depending on time to occurrence of prosthetic joint infection: a prospective cohort study. Clin. Microbiol. Infect. 2019, 25, 353–358. [Google Scholar] [CrossRef]
- Triffault-Fillit, C.; Valour, F.; Guillo, R.; Tod, M.; Goutelle, S.; Lustig, S.; Fessy, M.-H.; Chidiac, C.; Ferry, T.; Ferry, T.; et al. Prospective cohort study of the tolerability of prosthetic joint infection empirical antimicrobial therapy. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Benito, N.; Franco, M.; Ribera, A.; Soriano, A.; Rodriguez-Pardo, D.; Sorlí, L.; Fresco, G.; Fernández-Sampedro, M.; Dolores Del Toro, M.; Guío, L.; et al. Time trends in the aetiology of prosthetic joint infections: a multicentre cohort study. Clin. Microbiol. Infect. 2016, 22, 732.e1–732.e8. [Google Scholar] [CrossRef] [PubMed]
- Tsukayama, D.T.; Estrada, R.; Gustilo, R.B. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J. Bone Joint Surg. Am. 1996, 78, 512–523. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J. Arthroplasty 2018, 33, 1309–1314.e2. [Google Scholar] [CrossRef] [PubMed]
- Bengtson, S.; Knutson, K. The infected knee arthroplasty. Acta Orthop. Scand. 1991, 62, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Berbari, E.F.; Hanssen, A.D.; Duffy, M.C.; Steckelberg, J.M.; Ilstrup, D.M.; Harmsen, W.S.; Osmon, D.R. Risk factors for prosthetic joint infection: case-control study. Clin. Infect. Dis. 1998, 27, 1247–1254. [Google Scholar] [CrossRef]
- Segawa, H.; Tsukayama, D.T.; Kyle, R.F.; Becker, D.A.; Gustilo, R.B. Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J. Bone Joint Surg. Am. 1999, 81, 1434–1445. [Google Scholar] [CrossRef]
- Steckelberg, J.; Osmon, D.R. Prosthetic Joint Infections. In Infections Associated with Indwelling Medical Devices; Waldvogel, F.A., Bisno, A.L., Eds.; American Society of Microbiology: Washington, DC, USA, 2000; pp. 173–209. [Google Scholar]
- Soriano, A.; Garcia, S.; Bori, G. Treatment of acute post-surgical infection of joint arthroplasty. Clin. Microbiol. Infect. 2006, 12, 930–933. [Google Scholar] [CrossRef]
- Marculescu, C.E.; Berbari, E.F.; Hanssen, A.D.; Steckelberg, J.M.; Harmsen, S.W.; Mandrekar, J.N.; Osmon, D.R. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin. Infect. Dis. 2006, 42, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Pandey, R.; Berendt, A.R.; Athanasou, N.A. Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. Arch. Orthop. Trauma Surg. 2000, 120, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Pulido, L.; Ghanem, E.; Joshi, A.; Purtill, J.J.; Parvizi, J. Periprosthetic joint infection: The incidence, timing, and predisposing factors. Clin. Orthop. Relat. Res. 2008, 466, 1710–1715. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, P.; Fink, B.; Sandow, D.; Margull, A.; Berger, I.; Frommelt, L. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin. Infect. Dis. 2008, 47, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Douglas, J. Microbiology of infected arthroplasty: implications for empiric peri-operative antibiotics. J. Orthop. Surg. (Hong Kong) 2008, 16, 339–342. [Google Scholar] [CrossRef]
- Lee, J.; Kang, C.-I.; Lee, J.H.; Joung, M.; Moon, S.; Wi, Y.M.; Chung, D.R.; Ha, C.-W.; Song, J.-H.; Peck, K.R. Risk factors for treatment failure in patients with prosthetic joint infections. J. Hosp. Infect. 2010, 75, 273–276. [Google Scholar] [CrossRef]
- Berbari, E.F.; Osmon, D.R.; Carr, A.; Hanssen, A.D.; Baddour, L.M.; Greene, D.; Kupp, L.I.; Baughan, L.W.; Harmsen, W.S.; Mandrekar, J.N.; et al. Dental procedures as risk factors for prosthetic hip or knee infection: a hospital-based prospective case-control study. Clin. Infect. Dis. 2010, 50, 8–16. [Google Scholar] [CrossRef]
- Cobo, J.; Miguel, L.G.S.; Euba, G.; Rodríguez, D.; García-Lechuz, J.M.M.; Riera, M.; Falgueras, L.; Palomino, J.; Benito, N.; del Toro, M.D.D.; et al. Early prosthetic joint infection: outcomes with debridement and implant retention followed by antibiotic therapy. Clin. Microbiol. Infect. 2011, 17, 1632–1637. [Google Scholar] [CrossRef]
- Wang, F.-D.; Wang, Y.-P.; Chen, C.-F.; Chen, H.-P. The incidence rate, trend and microbiological aetiology of prosthetic joint infection after total knee arthroplasty: A 13 years’ experience from a tertiary medical center in Taiwan. J. Microbiol. Immunol. Infect. 2018, 51, 717–722. [Google Scholar] [CrossRef]
- Moran, E.; Masters, S.; Berendt, A.R.; McLardy-Smith, P.; Byren, I.; Atkins, B.L. Guiding empirical antibiotic therapy in orthopaedics: The microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J. Infect. 2007, 55, 1–7. [Google Scholar] [CrossRef]
- Zeller, V.; Kerroumi, Y.; Meyssonnier, V.; Heym, B.; Metten, M.-A.; Desplaces, N.; Marmor, S. Analysis of postoperative and hematogenous prosthetic joint-infection microbiological patterns in a large cohort. J. Infect. 2018, 76, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Peel, T.N.; Cheng, A.C.; Buising, K.L.; Choong, P.F.M. Microbiological aetiology, epidemiology, and clinical profile of prosthetic joint infections: are current antibiotic prophylaxis guidelines effective? Antimicrob. Agents Chemother. 2012, 56, 2386–2391. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, D.; Pigrau, C.; Euba, G.; Cobo, J.; García-Lechuz, J.; Palomino, J.; Riera, M.; del Toro, M.D.; Granados, A.; Ariza, X. Acute haematogenous prosthetic joint infection: prospective evaluation of medical and surgical management. Clin. Microbiol. Infect. 2010, 16, 1789–1795. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pardo, D.; Pigrau, C.; Lora-Tamayo, J.; Soriano, A.; del Toro, M.D.; Cobo, J.; Palomino, J.; Euba, G.; Riera, M.; Sánchez-Somolinos, M.; et al. Gram-negative prosthetic joint infection: outcome of a debridement, antibiotics and implant retention approach. A large multicentre study. Clin. Microbiol. Infect. 2014, 20, O911–O919. [Google Scholar] [CrossRef] [PubMed]
- Lora-Tamayo, J.; Murillo, O.; Iribarren, J.A.; Soriano, A.; Sánchez-Somolinos, M.; Baraia-Etxaburu, J.M.; Rico, A.; Palomino, J.; Rodríguez-Pardo, D.; Horcajada, J.P.; et al. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin. Infect. Dis. 2013, 56, 182–194. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin. Orthop. Relat. Res. 2011, 469, 2992–2994. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Tsukayama, D.T.; Goldberg, V.M.; Kyle, R. Diagnosis and management of infection after total knee arthroplasty. J. Bone Joint Surg. Am. 2003, 85, S75–S80. [Google Scholar] [CrossRef]
- Zimmerli, W.; Trampuz, A.; Ochsner, P.E. Prosthetic-joint infections. N. Engl. J. Med. 2004, 351, 1645–1654. [Google Scholar] [CrossRef]
- Høiby, N.; Bjarnsholt, T.; Moser, C.; Bassi, G.L.L.; Coenye, T.; Donelli, G.; Hall-Stoodley, L.; Holá, V.; Imbert, C.; Kirketerp-Møller, K.; et al. ESCMID guideline for the diagnosis and treatment of biofilm infections 2014. Clin. Microbiol. Infect. 2015, 21, S1–S25. [Google Scholar] [CrossRef]
- Becker, K.; Heilmann, C.; Peters, G. Coagulase-negative staphylococci. Clin. Microbiol. Rev. 2014, 27, 870–926. [Google Scholar] [CrossRef]
- Kahl, B.C.; Becker, K.; Löffler, B. Clinical Significance and Pathogenesis of Staphylococcal Small Colony Variants in Persistent Infections. Clin. Microbiol. Rev. 2016, 29, 401–427. [Google Scholar] [CrossRef]
- Tong, S.Y.C.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [PubMed]
- Tornero, E.; Morata, L.; Martínez-Pastor, J.C.; Bori, G.; Climent, C.; García-Velez, D.M.; García-Ramiro, S.; Bosch, J.; Mensa, J.; Soriano, A. KLIC-score for predicting early failure in prosthetic joint infections treated with debridement, implant retention and antibiotics. Clin. Microbiol. Infect. 2015, 21, 786.e9–786.e17. [Google Scholar] [CrossRef]
- Tornero, E.; Martínez-Pastor, J.C.; Bori, G.; García-Ramiro, S.; Morata, L.; Bosch, J.; Mensa, J.; Soriano, A. Risk factors for failure in early prosthetic joint infection treated with debridement. Influence of etiology and antibiotic treatment. J. Appl. Biomater. Funct. Mater. 2014, 12, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Achermann, Y.; Goldstein, E.J.C.; Coenye, T.; Shirtliffa, M.E. Propionibacterium acnes: From Commensal to opportunistic biofilm-associated implant pathogen. Clin. Microbiol. Rev. 2014, 27, 419–440. [Google Scholar] [CrossRef]
- Aggarwal, V.K.; Bakhshi, H.; Ecker, N.U.; Parvizi, J.; Gehrke, T.; Kendoff, D. Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J. Knee Surg. 2014, 27, 399–406. [Google Scholar] [CrossRef]
- Rodriguez-Merchan, E.C. Preoperative aspiration culture (PAC) for the diagnosis of infection in a prosthetic knee joint. Arch. Bone Jt. Surg. 2018, 6, 342–345. [Google Scholar] [PubMed]
- Lora-Tamayo, J.; Senneville, É.; Ribera, A.; Bernard, L.; Dupon, M.; Zeller, V.; Li, H.K.H.K.; Arvieux, C.; Clauss, M.; Uçkay, I.; et al. The Not-So-Good Prognosis of Streptococcal Periprosthetic Joint Infection Managed by Implant Retention: The Results of a Large Multicenter Study. Clin. Infect. Dis. 2017, 64, 1742–1752. [Google Scholar] [CrossRef]
| Characteristic | No. of Cases (n = 2524) |
|---|---|
| Median age (IQR), years | 74 (13) |
| Female gender | 1508 (59.7) |
| Underlying conditions | |
| 1594 (63.3) |
| 592 (23.5) |
| 506 (20.1) |
| 299 (11.9) |
| 231 (9.2) |
| 221 (8.8) |
| 195 (7.7) |
| 175 (6.9) |
| 168 (6.7) |
| 164 (6.5) |
| 129 (5.1) |
| Charlson score, median (IQR) | 1 (2) |
| Index arthroplasty site | |
| 1244 (49.3) |
| 249 (9.9) |
| 995 (39.5) |
| 1219 (48.3) |
| 46 (1.8) |
| 15 (0.6) |
| ASA score, median (IQR) | 2 (1) |
| Indication for index arthroplasty* | |
| 1938 (77.2) |
| 1264 (52.4) |
| 417 (17.3) |
| 51 (2.1) |
| 32 (1.3) |
| 31 (1.3) |
| 12 (0.5) |
| 43 (1.8) |
| 573 (22.8) |
| 292 (12.1) |
| 158 (6.6) |
| 32 (1.3) |
| 25 (1) |
| 13 (0.5) |
| 29 (1.2) |
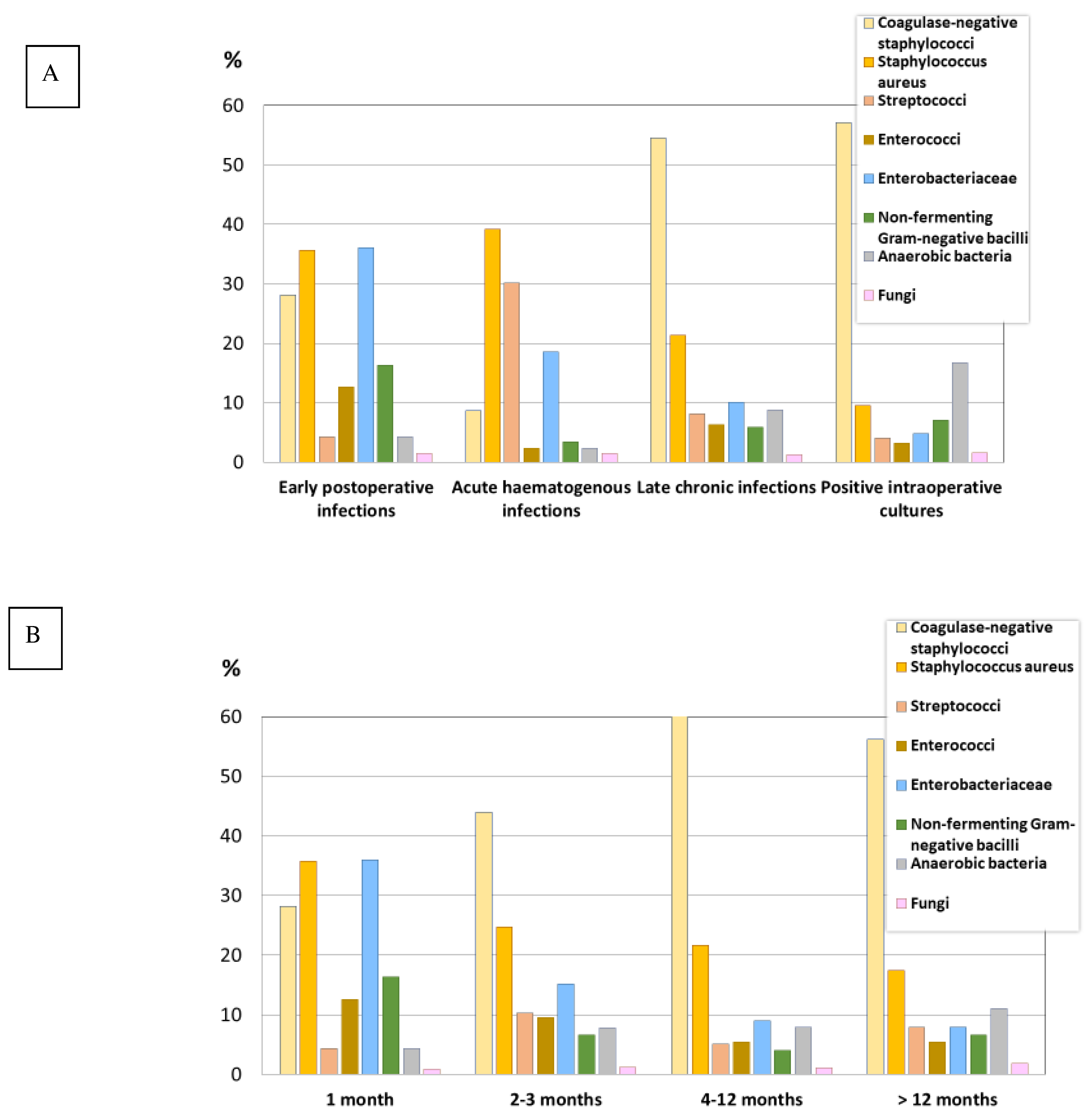
| Microorganism or Microorganism Group | Early Postoperative Infections n = 839 | Acute Hematogenous Infections n = 265 | Late Chronic Infections n = 1052 | Positive Intraoperative Cultures n = 126 | p-Value |
|---|---|---|---|---|---|
| Total no. (%)* | |||||
| Staphylococcus species | 505 (60.2) | 122 (46) | 776 (73.8) | 84 (66.7) | <0.001 |
| 236 (28.1) | 23 (8.7) | 573 (54.5) | 72 (57.1) | <0.001 |
| 130 (15.5) | 11 (4.2) | 355 (33.7) | 36 (28.6) | <0.001 |
| 2 (0.2) | 6 (2.3) | 31 (2.9) | 4 (3.2) | <0.001 |
| 8 (1) | 0 (0) | 25 (2) | 2 (1.6) | 0.014 |
| 8 (1) | 0 (0) | 22 (2.1) | 0 (0) | 0.014 |
| 5 (0.6) | 0 (0) | 11 (1) | 3 (2.4) | 0.065 |
| 2 (0.2) | 0 (0) | 12 (1.1) | 1 (0.8) | 0.048 |
| 89 (10.6) | 6 (2.3) | 168 (16) | 23 (23) | <0.001 |
| 299 (35.6) | 104 (39.2) | 224 (21.3) | 12 (9.5) | <0.001 |
| Streptococcus species | 36 (4.3) | 80 (30.2) | 85 (8.1) | 5 (4) | <0.001 |
| 8 (1) | 28 (10.9) | 28 (2.7) | 0 (0) | <0.001 |
| 6 (0.7) | 12 (4.5) | 25 (2.4) | 2 (1.6) | 0.002 |
| 8 (1) | 5 (1.9) | 16 (1.5) | 2 (1.6) | 0.632 |
| 3 (0.4) | 8 (3) | 12 (1.1) | 1 (0.8) | 0.005 |
| 10 (1.2) | 5 (1.9) | 1 (0.1) | 0 (0) | 0.003 |
| 0 (0) | 10 (3.8) | 2 (0.2) | 0 (0) | <0.001 |
| 2 (0.2) | 7 (2.6) | 1 (0.1) | 0 (0) | <0.001 |
| Enterococcus species | 106 (12.6) | 6 (2.3) | 66 (6.3) | 4 (3.2) | <0.001 |
| 95 (11.3) | 5 (1.9) | 55 (5.2) | 3 (2.4) | <0.001 |
| 7 (0.8) | 1 (0.4) | 5 (0.5) | 0 (0.0) | 0.584 |
| Microorganism or Microorganism Group | Early Postoperative Infections n = 839 | Acute Hematogenous Infections n = 265 | Late Chronic Infections n = 1052 | Positive Intraoperative Cultures n = 126 | p-Value |
|---|---|---|---|---|---|
| Total no. (%)* | |||||
| Aerobic Gram-negative bacilli | 395 (47.1) | 60 (22.6) | 161 (15.3) | 14 (11.1) | <0.001 |
| 303 (36.1) | 49 (18.5) | 106 (10.1) | 6 (4.8) | <0.001 |
| 129 (15.4) | 33 (12.5) | 41 (3.9) | 3 (2.4) | <0.001 |
| 75 (8.9) | 4 (1.5) | 27 (2.6) | 2 (1.6) | <0.001 |
| 73 (8.7) | 5 (1.9) | 19 (1.8) | 0 (0) | <0.001 |
| 48 (5.7) | 1 (0.4) | 1 (0.4) | 9 (0.9) | <0.001 |
| 26 (3.1) | 4 (1.5) | 11 (1) | 1 (0.8) | =0.009 |
| 13 (1.5) | 0 (0) | 6 (0.6) | 0 (0) | =0.028 |
| 137 (16.3) | 9 (3.4) | 62 (5.9) | 9 (7.1) | <0.001 |
| 128 (15.3) | 8 (3) | 59 (5.6) | 6 (4.8) | <0.001 |
| 10 (1.2) | 0 (0) | 2 (0.2) | 1 (0.8) | 0.021 |
| Aerobic Gram-positive bacilli | 16 (1.9) | 5 (1.9) | 29 (2.8) | 4 (3.2) | 0.555 |
| 16 (1.9) | 1 (0.4) | 29 (2.8) | 4 (3.2) | 0.087 |
| 9 (1.1) | 0 (0) | 7 (0.7) | 1 (0.8) | 0.321 |
| 3 (0.4) | 1 (0.4) | 14 (1.3) | 2 (1.6) | 0.081 |
| Anaerobic Gram-positive bacilli | 19 (2.3) | 3 (1.1) | 73 (6.9)** | 22 (17.3)** | <0.001 |
| 17 (2) | 3 (1.1) | 64 (6.1)** | 19 (15.1)** | <0.001 |
| Anaerobic Gram-positive cocci† | 8 (1) | 2 (0.8) | 23 (2.2) | 0 (0) | 0.042 |
| Anaerobic Gram-negative bacilli | 12 (1.4) | 1 (0.4) | 8 (0.8) | 0 (0) | 0.182 |
| 10 (1.1) | 1 (0.3) | 5 (0.4) | 0 (0) | 0.145 |
| Mycobacterium species | 2 (0.2) | 0 (0) | 8 (0.8) | 0 (0) | 0.183 |
| Fungi | 8 (1.5) | 4 (1.5) | 16 (1.5) | 2 (1.6) | 0.723 |
| 8 (1) | 3 (1.1) | 14 (1.3) | 2 (1.6) | 0.854 |
| Multidrug-resistant organisms | 201 (24) | 29 (10.9) | 82 (7.8) | 6 (4.8) | <0.001 |
| 92 (11) | 22 (8.3) | 58 (5.5) | 5 (4) | <0.001 |
| 112 (13.3) | 7 (2.6) | 25 (2.4) | 1 (0.8) | <0.001 |
| 36 (4.3) | 2 (0.8) | 4 (0.4) | 0 (0.0) | <0.001 |
| Ciprofloxacin-resistant Gram-negative bacilli | 63 (7.5) | 7 (2.6) | 20 (1.9) | 3 (2.4) | <0.001 |
| Polymicrobial infections | 230 (27.4)** | 17 (6.3) | 143 (13.1)** | 7 (5.6) | <0.001 |
| Microorganism or Microorganism Group | PJI within 1 Month after Surgery n = 844 | PJI 2-3 Months after Surgery n = 243 | PJI 4-12 Months after Surgery n = 277 | PJI > 12 Months after Surgery n = 619 | p-Value |
|---|---|---|---|---|---|
| Total no. (%)* | |||||
| Staphylococcus species | |||||
| 236 (28.2) ** | 107 (44) ** † | 167 (60.3) † | 348 (56.2) | <0.001 |
| 132 (15.6) ** | 68 (28) ** † | 106 (38.3) † | 203 (32.8) | <0.001 |
| 2 (0.2) ** | 3 (1.3) ** | 10 (3.6) | 22 (3.6) | <0.001 |
| 301 (35.7) | 60 (24.7) | 60 (21.7) | 108 (17.4) | <0.001 |
| Streptococcus species | 36 (4.3) ** | 25 (10.3) ** | 14 (5.1) | 49 (7.9) | <0.001 |
| 8 (0.9) ** | 11 (4.5) ** | 6 (2.2) | 10 (1.6) | 0.003 |
| 6 (0.7) ** | 7 (2.9) ** | 2 (0.7) † | 18 (2.9) † | 0.003 |
| Enterococcus species | 106 (12.6) | 23 (9.5) | 15 (5.4) | 32 (5.4) | <0.001 |
| Aerobic Gram-negative bacilli | 396 (46.9) ** | 50 (20.6) ** † | 37 (13.4) † | 37 (13.4) | <0.001 |
| 303 (35.9) ** | 37 (15.2) ** † | 25 (9) † | 48 (7.8) | <0.001 |
| 129 (15.3) | 12 (4.9) | 10 (3.6) | 21 (3.4) | <0.001 |
| 75 (8.9) | 7 (2.9) | 7 (2.5) | 14 (2.3) | <0.001 |
| 73 (8.6) ** | 11 (4.5) ** † | 2 (0.7) † | 6 (1) | <0.001 |
| 48 (5.7) | 2 (0.8) | 4 (1.4) | 3 (0.5 | <0.001 |
| 138 (16.4) ** | 16 (6.6) ** | 11 (4) | 41 (6.6) | <0.001 |
| 128 (15.2) ** | 17 (7) ** | 11 (4) | 35 (5.7) | <0.001 |
| Aerobic Gram-positive bacilli | 16 (1.9) | 3 (1.2) | 7 (2.5) | 23 (3.7) | 0.083 |
| Anaerobic Gram-positive bacilli | 19 (2.3) ** | 14 (5.7) ** | 16 (5.8) | 61 (9.7) | <0.001 |
| 17 (2) ** | 12 (4.9) ** | 16 (5.8) | 51 (8.2) | <0.001 |
| Anaerobic Gram-positive cocci | 8 (0.9) | 4 (1.6) | 5 (1.8) | 13 (2.1) | 0.330 |
| Anaerobic Gram-negative bacilli | 12 (1.4) | 2 (0.8) | 1 (0.4) | 5 (0.8) | 0.409 |
| Mycobacterium species | 2 (0.2) | 1 (0.9) | 4 (1.4) | 2 (0.3) | 0.068 |
| Fungi | 8 (0.9) | 3 (1.2) | 3 (1.1) | 12 (1.9) | 0.418 |
| Multidrug-resistant organisms | 202 (23.9) | 20 (8.2) | 20 (7.2) | 43 (6.9) | <0.001 |
| 93 (11) | 14 (5.8) | 14 (5.1) | 30 (4.8) | <0.001 |
| 112 (13.3) | 7 (2.5) | 5 (1.8) | 14 (2.3) | <0.001 |
| 36 (4.3) | 1 (0.4) | 2 (0.7) | 1 (0.3) | <0.001 |
| Ciprofloxacin-resistant Gram-negative bacilli | 84 (10) | 5 (2.1) | 4 (1.4) | 11 (1.8) | <0.001 |
| Polymicrobial infections | 230 (27.2) | 36 (14.7) | 32 (11.1) | 77 (11.1) | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benito, N.; Mur, I.; Ribera, A.; Soriano, A.; Rodríguez-Pardo, D.; Sorlí, L.; Cobo, J.; Fernández-Sampedro, M.; del Toro, M.D.; Guío, L.; et al. The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms. J. Clin. Med. 2019, 8, 673. https://doi.org/10.3390/jcm8050673
Benito N, Mur I, Ribera A, Soriano A, Rodríguez-Pardo D, Sorlí L, Cobo J, Fernández-Sampedro M, del Toro MD, Guío L, et al. The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms. Journal of Clinical Medicine. 2019; 8(5):673. https://doi.org/10.3390/jcm8050673
Chicago/Turabian StyleBenito, Natividad, Isabel Mur, Alba Ribera, Alex Soriano, Dolors Rodríguez-Pardo, Luisa Sorlí, Javier Cobo, Marta Fernández-Sampedro, María Dolores del Toro, Laura Guío, and et al. 2019. "The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms" Journal of Clinical Medicine 8, no. 5: 673. https://doi.org/10.3390/jcm8050673
APA StyleBenito, N., Mur, I., Ribera, A., Soriano, A., Rodríguez-Pardo, D., Sorlí, L., Cobo, J., Fernández-Sampedro, M., del Toro, M. D., Guío, L., Praena, J., Bahamonde, A., Riera, M., Esteban, J., Baraia-Etxaburu, J. M., Martínez-Alvarez, J., Jover-Sáenz, A., Dueñas, C., Ramos, A., ... REIPI (Spanish Network for Research in Infectious Disease) Group for the Study of Prosthetic Joint Infections/GEIO (Group for the Study of Osteoarticular Infections), SEIMC (Spanish Society of Infectious Diseases and Clinical Microbiolo, o. b. o. t. (2019). The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms. Journal of Clinical Medicine, 8(5), 673. https://doi.org/10.3390/jcm8050673









