Concordance between the Clinical Definition of Polypathological Patient versus Automated Detection by Means of Combined Identification through ICD-9-CM Codes
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Population
2.2. Inclusion Criteria
- Administrative discharge in the Andalusian MBDS of the index episode in the services of internal medicine, infectious diseases, digestive, cardiology, pulmonary, neurology, endocrine, hematology, rheumatology, and nephrology specialties.
- Possibility of access to the digital medical history and discharge of the index episode.
- Patients >18 years.
2.3. Exclusion Criteria
- Not meeting the inclusion criteria.
- Discharge encoded by childbirth and/or pregnancy pathology, from pediatric and surgical areas.
2.4. Sample
2.5. Variables
2.6. Statistical Analysis
2.7. Ethical Aspects
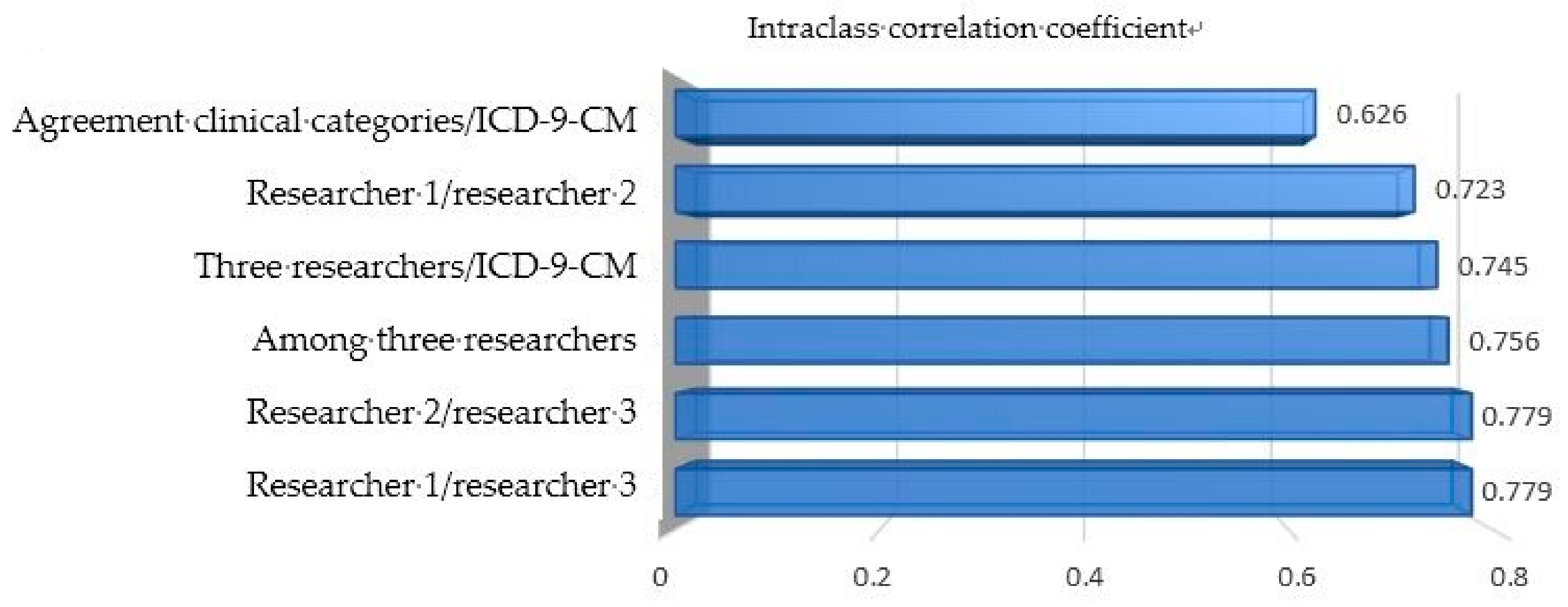
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ollero Baturone, M. Modelos de organización para la atención a pacientes crónicos complejos. Foro de debate. Escuela Andaluza de Salud Pública. Granada. 2009. Available online: http://si.easp.es/gestionclinica/wp-content/uploads/2009/10/Doc-2.-Modelos-de-organizacion-para-la-atencion-a-pacientes-cronicos-complejos-_Ollero-Baturone-M_pdf (accessed on 5 November 2018).
- Ministerio de Sanidad Servicios Sociales e Igualdad, Sanidad. Estrategia para el Abordaje de la Cronicidad en el Sistema Nacional de Salud; Ministerio de Sanidad Servicios Sociales e Igualdad, Sanidad: Madrid, Spain, 2012. [Google Scholar]
- Valderas, J.M.; Starfield, B.; Sibbald, B.; Salisbury, C.; Roland, M. Defining comorbidity: Implications for understanding health and health services. Ann. Fam. Med. 2009, 7, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Action Plan for Implementation of the European Strategy for the Prevention and Control of Noncommunicable Diseases 2012–2016. World Health Organization. 2012. Available online: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/cancer/publications/2012/action-plan-for-implementation-of-the-european-strategy-for-the-prevention-and-control-of-noncommunicable-diseases-20122016 (accessed on 5 November 2018).
- Jadad, A.R.; Cabrera, A.; Martos, F.; Smith, R.; Lyons, R.F. When people live with multiple chronic diseases: A collaborative approach to an emerging global challenge. Granada: Andalusian School of Public Health; 2010. Available online: http://www.opimec.org/equipos/when-people-live-with-multiple-chronic-diseases/ (accessed on 10 November 2018).
- Unidad de pacientes pluripatológicos. Estándares y Recomendaciones. Informes, Estudios e Investigación 2009. Ministerio de Sanidad y Política Social. Available online: http://www.msc.es/organizacion/sns/planCalidadSNS/docs/EyR_UPP.pdf (accessed on 5 November 2018).
- Montes, J.; Casariego, E.; De Toro, M.; Mosquera, E. La asistencia a pacientes crónicos y pluripatológicos. Magnitud e iniciativas para su manejo: La Declaración de Sevilla. Situación y propuestas en Galicia. Galicia Clínica 2012, 73, 7–14. [Google Scholar] [CrossRef]
- Bernabeu-Wittel, M.; Alonso-Coello, P.; Rico-Blázquez, M.; Rotaeche-del-Campo, R.; Sánchez-Gómez, S.; Casariego-Vales, E. Desarrollo de guías de práctica clínica en pacientes con comorbilidad y pluripatología. Rev. Clin. Esp. 2014, 214, 328–335. [Google Scholar] [CrossRef]
- García-Morillo, J.S.; Bernabéu-Wittel, M.; Ollero-Baturone, M.; Aguilar-Guisado, M.; Ramirez-Duque, N.; González-de-la-Puente, M.A.; Limpo, P.; Romero-Carmona, S.; Cuello-Contreras, J.A. Incidencia y características clínicas de los pacientes pluripatológicos ingresados en una unidad de medicina Interna. Med. Clin. 2005, 125, 5–9. [Google Scholar] [CrossRef]
- Vogeli, C.; Shields, A.E.; Lee, T.A.; Gibson, T.B.; Marder, W.D.; Weiss, K.B.; Blumenthal, D. Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. J. Gen. Intern. Med. 2007, 22, 391–395. [Google Scholar] [PubMed]
- Bernabeu-Wittel, M.; Jadad, A.; Moreno-Gaviño, L.; Hernández-Quiles, C.; Toscano, F.; Cassani, M.; Ramírez, N.; Ollero-Baturone, M. Peeking through the cracks: An assessment of the prevalence, clinical characteristics and health-related quality life (HRQoL) of people with polypathology in a hospital setting. Arch. Gerontol. Geriatr. 2010, 51, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Ocaña, J.; Bernabeu-Wittel, M.; Gil-Navarro, M.V.; García-Morillo, J.S.; Ortiz Camuñez, M.A.; Ollero-Baturone, M. La discapacidad como barrera a la adherencia terapéutica en pacientes pluripatológicos: Papel del cuidador principal. Rev. Clin. Esp. 2010, 210, 221–226. [Google Scholar] [CrossRef]
- Galindo-Ocaña, J.; Bernabeu-Wittel, M.; Gil-Navarro, M.V.; García-Morillo, J.S.; Ortiz-Camuñez, M.A.; Ollero-Baturone, M. Interacciones medicamentosas en pacientes pluripatológicos. Rev. Clin. Esp. 2010, 210, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Camúñez, M.A.; Bohórquez-Colombo, P.; Garrido-Porras, E.; Codina-Lanaspa, A.; Yerro-Páez, V.; Bernabéu-Wittel, M. Deterioro funcional, cognitivo y vulnerabilidad clínica en pacientes pluripatológicos. XXVI Congreso de la Sociedad Española de Medicina Familiar y Comunitaria. Atención Primaria 2006. [Google Scholar]
- Moreno-Gaviño, L.; Bernabéu-Wittel, M.; Álvarez Tello, M.; Rincón Gómez, M.; García-Morillo, S.; Cassani Garza, M.; Ollero Baturone, M. Sobrecarga sentida por la figura del cuidador principal en una cohorte de pacientes pluripatológicos. Atención Primaria 2008, 40, 193–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-Morillo, S.; Bernabéu-Wittel, M.; Cassani Garza, M.; Rincón Gómez, M.; Yerro Páez, V.; Ollero Baturone, M. Influencia de los factores biopsicosociales en el grado de empatía en la relación médico-enfermo en una cohorte de pacientes pluripatológicos. Rev. Clin. Esp. 2007, 207, 379–382. [Google Scholar] [CrossRef]
- Melguizo Jiménez, M. From the chronic disease to the patient in a chronic condition. Atención Primaria 2011, 43, 67–68. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Linn, B.S.; Linn, M.W.; Gurel, L. Cumulative illness rating scale. J. Am. Geriatr. Soc. 1968, 16, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, S.; Apolone, G.; McNeil, B.J.; Cleary, P.D. The importance of co-existing disease in the occurrence of postoperative complications and one-year recovery in patients undergoing total hip replacement. Med. Care 1993, 31, 141–154. [Google Scholar] [CrossRef]
- Kaplan, M.H.; Feinstein, A.R. The importance of classifying initial co-morbidity in evaluating the outcome of diabetes mellitus. J. Chron. Dis. 1974, 27, 387–404. [Google Scholar] [CrossRef]
- Wang, H.E.; Donnelly, J.P.; Yende, S.; Levitan, E.B.; Shapiro, N.I.; Dai, Y.; Zhao, H.; Heiss, G.; Odden, M.; Newman, A.; Safford, M. Validation of the REGARDS severe sepsis risk score. J. Clin. Med. 2018, 7, 536. [Google Scholar] [CrossRef] [PubMed]
- MSC (Ministerio de Sanidad y Consumo). CIE-9-MC (Clasificación Internacional de Enfermedades 9ª. Revisión Modificación Clínica), 9th ed.; Ministerio de Sanidad y Consumo: Madrid, Spain, 2014. [Google Scholar]
- Harnod, T.; Chen, W.; Wang, J.H.; Lin, S.Z.; Ding, D.C. Hysterectomies are associated with an increased risk of depression: A population-based cohort study. J. Clin. Med. 2018, 7, 366. [Google Scholar] [CrossRef] [PubMed]
- Orueta, J.F.; Mateos Del Pino, M.; Barrio Beraza, I.; Solinis, R.N.; Zubizarreta, M.C.; Sarabia, C.S. Estratificación de la población en el País Vasco: Resultados en el primer año de implantación. Atención Primaria 2013, 45, 54–60. [Google Scholar] [CrossRef]
- Ollero Baturone, M.; et al. Proceso asistencial integrado. In Atención al Paciente Pluripatológico, 2nd ed.; Consejería de Salud, Junta de Andalucía: Sevilla, Spain, 2007. [Google Scholar]
- Martínez Reina, A. Clasificación mediante grupos relacionados con el diagnóstico de pacientes diagnosticados de Pancreatitis. Med. Intensiv. 2003, 27, 75–77. [Google Scholar] [CrossRef]
- Barba, R.; Losa, J.E.; Guijarro, C.; Zapatero, A. Fiabilidad del conjunto mínimo básico de datos (CMBD) en el diagnóstico de la enfermedad tromboembólica. Med. Clin. 2006, 127, 255–257. [Google Scholar] [CrossRef]
- Gimeno Benítez, A.; Suero Villa, P.; Suero Villa, S.; Guerrero Porras, M.; Sánchez Veja, J.; Luengo Pérez, L.M. El conjunto mínimo básico de datos como herramienta de vigilancia epidemiológica de la incidencia diabetes mellitus 1: Experiencia en extremadura. Enferm. Glob. 2013, 32, 164–170. [Google Scholar] [CrossRef]
- Redondo González, O. Validez y fiabilidad del conjunto mínimo básico de datos en la estimación de la gastroenteritis aguda nosocomial por rotavirus. Rev. Esp. Enferm. Dig. 2015, 107, 152–161. [Google Scholar]
- Vicente-Fatela, L.; Acedo-Gutiérrez, M.S.; Rodríguez-Sánchez, S.; González-García, E.; Martínez-Salio, A.; Sanz-Ayan, M.P. Codificación del dolor crónico con la clasificación internacional de enfermedades—9ª revisión modificación clínica (CIE-9-MC). Rev. Soc. Esp. Dolor 2007, 2, 95–103. [Google Scholar]
- Comín-Colet, J.; Verdú-Rotellar, J.M.; Vela, E.; Clèries, M.; Bustins, M.; Mendoza, L.; Badosa, N.; Cladellas, M.; Ferré, S.; Bruguera, J. Eficacia de un programa integrado hospital-atención primaria para la insuficiencia cardiaca: Análisis poblacional sobre 56.742 pacientes. Rev. Esp. Cardiol. 2014, 67, 283–293. [Google Scholar] [CrossRef]
- Yetano Laguna, J.; López Arbeloa, G.; Guajardo Remacha, J.; Barriola Lerchundi, M.T.; Aguirre Larracoechea, U. Calidad de la codificación de los procedimientos quirúrgicos y su influencia en los grupos relacionados con el diagnóstico. Papeles Médicos 2005, 1, 10–16. [Google Scholar]
- Allepuz, A.; Serra-Sutton, V.; Espallargues, M.; Salvador, X.; Pons, J.M.V. Artroplastias de cadera y rodilla en Cataluña desde 1994 a 2005. Gac. Sanit. 2008, 22, 534–540. [Google Scholar] [CrossRef] [Green Version]
- Acedo, M.S.; Rodríguez, S.; González, E.; Sanz, M.P.; Martínez, A.; Vicente, L. La codificación como instrumento en la gestión clínica de las unidades del dolor. Rev. Soc. Esp. Dolor 2015, 22, 145–158. [Google Scholar] [CrossRef] [Green Version]
- Kern, E.F.; Maney, M.; Miller, D.R.; Tseng, C.L.; Tiwari, A.; Rajan, M.; Aron, D.C.; Pogach, L. Failure of ICD-9-MC codes to identify patients with comorbid chronic kidney disease in diabetes. Health Serv. Res. 2006, 41, 564–580. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, G.S.; Wu, C.; Senthilselvan, A.; McMurtry, M.S. The validity of ICD codes coupled with imaging procedure codes for identifying acute venous thromboembolism using administrative data. Vasc. Med. 2015, 20, 364–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garvin, J.H.; Redd, A.; Bolton, D.; Graham, P.; Roche, D.; Groeneveld, P.; Leecaster, M.; Shen, S.; Weiner, M.G. Exploration of ICD-9-CM coding of chronic disease within the elixhauser comorbidity measure in patients with chronic heart failure. Perspect. Health Inf. Manag. 2013, 10, 1b. [Google Scholar]
- De Achaval, S.; Feudtner, C.; Palla, S.; Suarez-Almazor, M.E. Validation of ICD-9-CM codes for identification of acetaminophen-related emergency department visits in a large pediatric hospital. BMC Health Serv. Res. 2013, 13, 72. [Google Scholar] [CrossRef] [PubMed]
- Ginde, A.A.; Blanc, P.G.; Lieberman, R.M.; Camargo, C.A. Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr. Disord. 2008, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Fincke, B.G.; Miller, D.R.; Turpin, R. A classification of diabetic foot infections using ICD-9-CM codes: Application to a large computerized medical database. BMC Health Serv. Res. 2010, 10, 192. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, E.A.; Ellis, J.L.; Shoup, J.A.; Zeng, C.; McQuillan, D.B.; Steiner, J.F. Association of patient-centered outcomes with patient-reported and ICD-9–based morbidity measures. Ann. Family Med. 2012, 10, 126–133. [Google Scholar] [CrossRef]
- Orueta, J.F.; Urraca, J.; Berraondo, I.; Darpón, J. ¿Es factible que los médicos de primaria utilicen CIE-9-MC? Calidad de la codificación de diagnósticos en las historias clínicas informatizadas. Gac. Sanit. 2006, 20, 194–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández Miera, M. El paciente pluripatológico en el ámbito hospitalario. Gac. Sanit. 2008, 22, 137–143. [Google Scholar] [CrossRef]
- Cortés-Reyes, E.; Rubio-Romero, J.A.; Gaitan-Duarte, H. Métodos estadísticos de evaluación de la concordancia y la reproducibilidad de pruebas diagnósticas. Revista Colombiana de Obstetricia y Ginecología 2010, 3, 247–255. [Google Scholar]
- López de Ullibarri Galparsoro, I.; Pita Fernández, S. Medidas de concordancia: El índice de Kappa. Atención Primaria en la Red. Available online: https://www.fisterra.com/mbe/investiga/kappa/kappa2.pdf (accessed on 10 November 2018).
- Bravo-Grau, S.; Cruz, J.P.Q. Estudios de exactitud diagnóstica: Herramientas para su Interpretación. Revista Chilena de Radiología 2015, 4, 158–164. [Google Scholar] [CrossRef]
| Clinical Categories | ICD-9 Codes | |
|---|---|---|
| A | ||
| A.1. Heart failure | Heart failure | 428 |
| Long-term effect following cardiac surgery | 429.4 | |
| Hypertensive heart disease | 402.91–402.01–402.11–404 | |
| A.2. Ischemic heart disease | Rheumatic heart failure (congestive) | 398.91 |
| Ischemic heart disease | 410 to 414 | |
| B | ||
| B.1.Vasculitis and systemic autoimmune diseases | Diffuse diseases of connective tissue (systemic lupus erythematosus, RA (rheumatoid arthritis), Scleroderma, diffuse fasciitis, polymyositis, Sjogren, MCTD (mixed connective tissue disease)). | 710 |
| B.2. Chronic kidney disease | Polyarteritis nodosa and allied conditions | 446 |
| Rheumatoid arthritis | 714 | |
| Polymyalgia rheumatica | 725 | |
| Chronic kidney disease | 585 | |
| Hypertensive chronic kidney disease | 403 | |
| Atherosclerosis of the renal artery | 440.1 | |
| C | ||
| Chronic airway obstruction, bronchial asthma or alveolar hypoventilation with functional limitation. | Chronic obstructive pulmonary disease | 491 to 496–518.0 |
| Chronic pulmonary heart disease | Acute and chronic respiratory failure | 518.1 |
| Chronic pulmonary heart disease (unspecified) | 518.83–518.84 | |
| 416.9 | ||
| D | ||
| D.1. Chronic inflammatory bowel disease | Inflammatory bowel disease | 555–556 |
| D.2. Syntomatic chronic liver disease or in activity | Chronic liver disease and cirrhosis (except for fatty liver and acute alcoholic) | 571 (except for 571.0 and 571.1) |
| E | ||
| E.1. Cerebrovascular disease | Cerebrovascular disease | 430 to 438 |
| Other cerebral degenerations | 331 | |
| E.2. Neurological disease with motor deficiency generating disability | Parkinson’s disease | 332 |
| Other degenerative diseases of the basal ganglia | 333 | |
| Huntington chorea | 333.4 | |
| Torsion dystonia | 333.6–333.7 | |
| E.3. Neurological disease with permanent cognitive impairment, at least moderate | Spinocerebellar disease | 334 |
| Anterior horn cell disease | 335 | |
| Syringomyelia | 336 | |
| Multiple sclerosis | 340 | |
| Other demyelinating diseases | 341 | |
| Hemiplegia and hemiparesis | 342 | |
| Cerebral palsy | 343 | |
| Other paralytic syndromes | 344 | |
| Muscular dystrophies and other myopathies | 359 | |
| Senile dementia | 290 | |
| Other alcoholic dementia | 291.2 | |
| Dementia in conditions classified elsewhere | 294.1 | |
| F | ||
| F.1. Symptomatic peripheral vascular disease | Symptomatic peripheral vascular disease | 443 (except for 443.81) |
| Atherosclerosis of native arteries of the extremities | 440.2 | |
| F.2. Diabetes mellitus with proliferative retinopathy or symptomatic neuropathy | Generalized atherosclerosis | 440.9 |
| Diabetes mellitus | 250.6– 250.5–352.5–362.01–362.07 | |
| −2117.7 | ||
| G | ||
| G.1. Chronic anaemia through digestive blood losing or acquired hematologic disease unsuitable for treatment with curative intent | Iron deficiency anaemia secondary to blood loss (chronic)—Myelodysplastic syndrome | 280.0–280.9–238.72–238.73–238.74–238.75 |
| Primary malignant neoplasm | 140 to 195 | |
| Secondary malignant neoplasms and metastatic | 196 to 198 | |
| G.2. Solid neoplasia or active hematologic neoplasia unsuitable for treatment with curative intent | Malignant neoplasm without specification of site | 199 |
| Malignant neoplasm of lymphatic and hematopoietic tissue | 200 to 208 | |
| Neoplasms of uncertain behaviour | 235 to 238 | |
| Neoplasms of unspecified nature | 239 | |
| Except for chemotherapy and radiotherapy admission | V58 | |
| H | ||
| Chronic osteoarticular disease with functional limitation | Arthropathy associated with Reiter’s disease | 711.1 |
| Arthropathy in Behcet’s syndrome | 711.2 | |
| Arthropathy, gastrointestinal conditions | 713.1 | |
| Crystal arthropathies | 712 | |
| Psoriatic arthropathy | 696 | |
| Arthropathy associated with hypersensitivity reaction | 713.6 | |
| Schönlein | 713.5 | |
| Arthropathy associated with neurological disorders | 713.7 | |
| Other general diseases with articular involvement | 715 | |
| Osteoarthrosis generalized | 720 | |
| Ankylosing spondylitis | ||
| Categories | Kappa | CI | Global Agreement Proportion | CI |
|---|---|---|---|---|
| A1 Heart failure | 0.620 * | 0.554–0.688 | 0.813 | 0.777–0.845 |
| A2 Ischemic heart disease | 0.794 * | 0.741–0.846 | 0.902 | 0.873–0.925 |
| A | 0.655 * | 0.587–0.723 | 0.845 | 0.811–0.873 |
| B1 Vasculitis and systemic autoimmune diseases | 0.751 * | 0.617–0.884 | 0.976 | 0.958–0.986 |
| B2 Chronic kidney disease | 0.834 * | 0.784–0.884 | 0.928 | 0.902–0.947 |
| B | 0.807 * | 0.755–0.859 | 0.911 | 0.883–0.933 |
| C Chronic airway obstruction, bronchial asthma, or alveolar hypoventilation with functional limitationChronic pulmonary heart disease | 0.814 * | 0.765–0.864 | 0.909 | 0.881–0.931 |
| D1 Chronic inflammatory bowel disease | 0.664 * | 0.201–1.00 | 0.996 | 0.985–0.999 |
| D2 Symptomatic chronic liver disease or in activity | 0.798 * | 0.706–0.889 | 0.966 | 0.947–0.979 |
| D | 0.805 | 0.716–0.893 | 0.966 | 0.947–0.979 |
| E1 Cerebrovascular disease | 0.525 * | 0.443–0.608 | 0.811 | 0.775–0.843 |
| E2 Neurological disease with motor deficiency generating disability | 0.144 * | 0.00–0.410 | 0.931 | 0.906–0.950 |
| E3 Neurological disease with permanent cognitive impairment, at least moderate | 0.568 * | 0.44–0.691 | 0.918 | 0.891–0.939 |
| E | 0.568 * | 0.503–0.647 | 0.802 | 0.766–0.834 |
| F1 Symptomatic peripheral vascular disease | 0.692 * | 0.580–0.803 | 0.948 | 0.925–0.964 |
| F2 Diabetes mellitus with proliferative retinopathy or symptomatic neuropathy | 0.754 * | 0.632–0.877 | 0.972 | 0.953–0.983 |
| F | 0.740 * | 0.665–0.824 | 0.937 | 0.912–0.955 |
| G1 Chronic anemia through digestive blood losing or acquired hematologic disease unsuitable for treatment with curative intent | 0.490 * | 0.321–0.658 | 0.939 | 0.914–0.957 |
| G2 Solid neoplasia or active hematologic neoplasia unsuitable for treatment with curative intent | 0.725 * | 0.634–0.816 | 0.913 | 0.897–0.926 |
| G | 0.624 * | 0.536–0.713 | 0.887 | 0.857–0.912 |
| H Chronic osteoarticular disease with functional limitation | 0.340 * | 0.040–0.639 | 0.966 | 0.947–0.979 |
| Factors | Odds Ratio (β Exp) | CI 95% | p |
|---|---|---|---|
| Number of diagnoses grouped ICD-9-CM | 0.928 | 0.889–0.969 | 0.001 |
| Number of PP categories according to clinical criteria | 0.590 | 0.445–0.782 | 0.000 |
| C category according to clinical identification | 1.807 | 1.158–2.820 | 0.009 |
| E category according to clinical identification | 1.752 | 1.199–2.559 | 0.004 |
| E3 subcategory according to clinical identification | 2.981 | 1.517–5.857 | 0.002 |
| A1 subcategory according to clinical identification | 2.042 | 1.000–4.167 | 0.05 |
| A2 subcategory according to clinical identification | 2.924 | 1.448–5.904 | 0.003 |
| B2 subcategory according to clinical identification | 2.208 | 1.311–3.718 | 0.003 |
| F2 subcategory according to clinical identification | 3.136 | 1.038–9.474 | 0.043 |
| ICD-9-CM (CI 95%) | ICD-9-CM without Category H (CI 95%) | |
|---|---|---|
| Sensitivity | 78.4% (74.8%–81.7%) | 78.2% (74.5%–81.5%) |
| Specificity | 87.8% (85.6%–89.7%) | 88.2% (86.1%–90.1%) |
| PPV | 78.1% (74.5%–81.4%) | 78.6% (75.0%–81.9%) |
| NPV | 88.0% (85.8%–89.9%) | 88.0% (85.8%–89.8%) |
| Accuracy | 84.5% (82.5%–86.2%) | 84.7% (82.8%–86.4%) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Salgado, J.; Bernabeu-Wittel, M.; Aguilera-González, C.; Goicoechea-Salazar, J.A.; Larrocha, D.; Nieto-Martín, M.D.; Moreno-Gaviño, L.; Ollero-Baturone, M. Concordance between the Clinical Definition of Polypathological Patient versus Automated Detection by Means of Combined Identification through ICD-9-CM Codes. J. Clin. Med. 2019, 8, 613. https://doi.org/10.3390/jcm8050613
Gómez-Salgado J, Bernabeu-Wittel M, Aguilera-González C, Goicoechea-Salazar JA, Larrocha D, Nieto-Martín MD, Moreno-Gaviño L, Ollero-Baturone M. Concordance between the Clinical Definition of Polypathological Patient versus Automated Detection by Means of Combined Identification through ICD-9-CM Codes. Journal of Clinical Medicine. 2019; 8(5):613. https://doi.org/10.3390/jcm8050613
Chicago/Turabian StyleGómez-Salgado, Juan, Máximo Bernabeu-Wittel, Carmen Aguilera-González, Juan Antonio Goicoechea-Salazar, Daniel Larrocha, María Dolores Nieto-Martín, Lourdes Moreno-Gaviño, and Manuel Ollero-Baturone. 2019. "Concordance between the Clinical Definition of Polypathological Patient versus Automated Detection by Means of Combined Identification through ICD-9-CM Codes" Journal of Clinical Medicine 8, no. 5: 613. https://doi.org/10.3390/jcm8050613
APA StyleGómez-Salgado, J., Bernabeu-Wittel, M., Aguilera-González, C., Goicoechea-Salazar, J. A., Larrocha, D., Nieto-Martín, M. D., Moreno-Gaviño, L., & Ollero-Baturone, M. (2019). Concordance between the Clinical Definition of Polypathological Patient versus Automated Detection by Means of Combined Identification through ICD-9-CM Codes. Journal of Clinical Medicine, 8(5), 613. https://doi.org/10.3390/jcm8050613






