Impact of Positive Airway Pressure on International Restless Legs Syndrome Score in Sleep Disordered Breathing
Abstract
1. Introduction
2. Methods
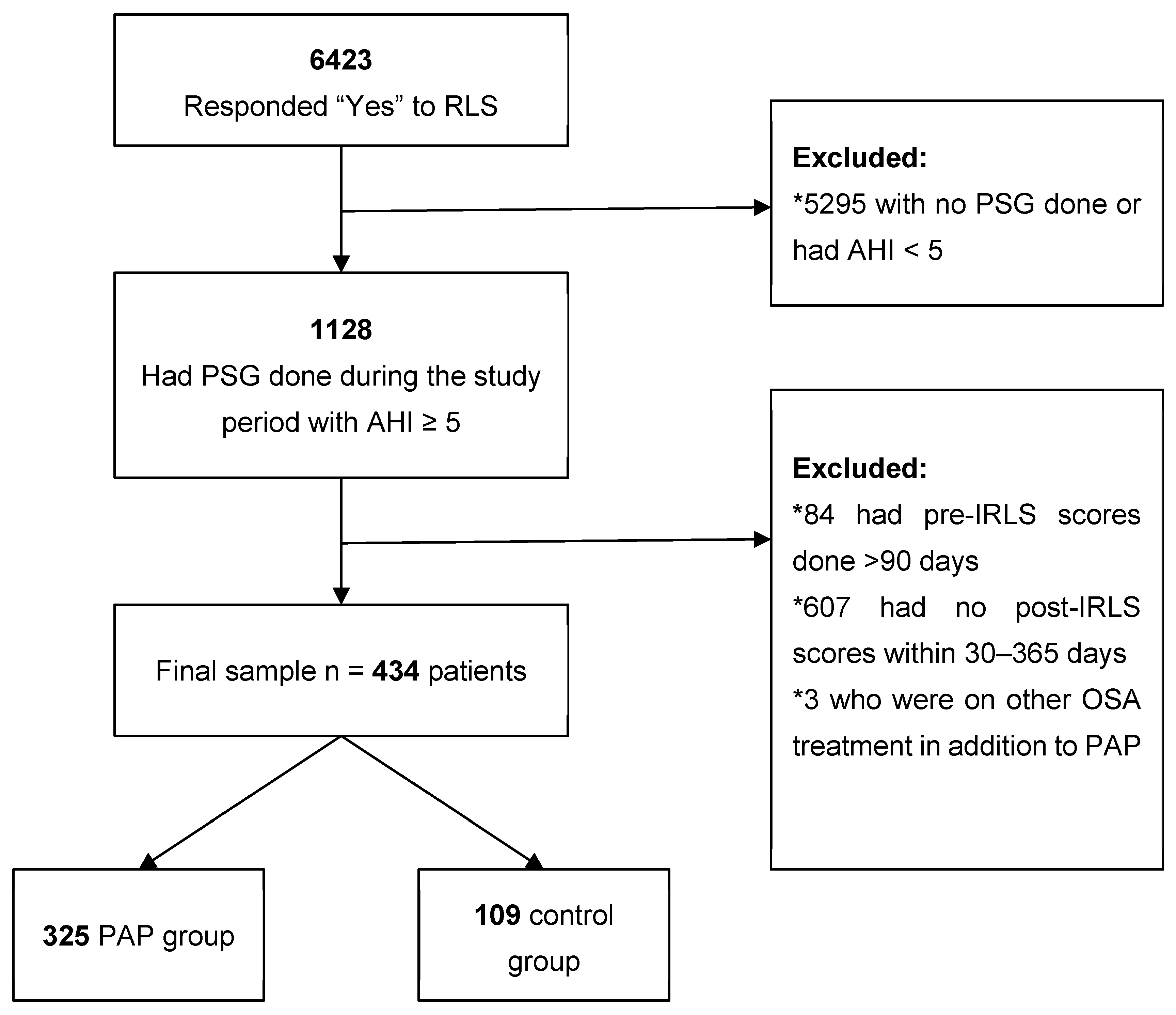
2.1. Patient Population
2.2. Data Collection from the Electronic Health Record
2.3. Data Collection from the Cleveland Clinic Knowledge Program
2.4. Statistical Analyses
3. Results
3.1. Effect of PAP Treatment on IRLS Score Change
3.2. Effect of PAP Self-Report Adherence on IRLS Score Change
3.3. Effect of PAP Objective Adherence on IRLS Score Change
3.4. RLS/Exacerbating Medication Usage
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Clavadetscher, S.C.; Gugger, M.; Bassetti, C.L. Restless legs syndrome: Clinical experience with long-term treatment. Sleep Med. 2004, 5, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.E.; Goodwin, J.L.; Vana, K.D.; Vasquez, M.M.; Wilcox, P.G.; Quan, S.F. Restless legs syndrome, sleep, and quality of life among adolescents and young adults. J. Clin. Sleep Med. 2014, 10, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.; Peralta, A.R.; Bentes, C. The urge to move and breathe—The impact of obstructive sleep apnea syndrome treatment in patients with previously diagnosed, clinically significant restless legs syndrome. Sleep Med. 2017, 38, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Benedikstdottir, B.; Arnardottir, E.S.; Janson, C.; Pack, A.; Juliusson, S.; Gislason, T. Prevalence of restless legs syndrome among patients with obstructive sleep apnea before and after CPAP treatment, compared to the general population-the icelandic sleep apnea cohort (ISAC) study. Eur. Respir. J. 2012, 35, 463. [Google Scholar]
- Lakshminarayanan, S.; Paramasivan, K.D.; Walters, A.S.; Wagner, M.L.; Patel, S.; Passi, V. Clinically significant but unsuspected restless legs syndrome in patients with sleep apnea. Mov. Disord. 2005, 20, 501–503. [Google Scholar] [CrossRef]
- Rodrigues, R.N.D.; Pratesi, R.; Krieger, J. Outcome of restless legs severity after continuous positive air pressure (CPAP) treatment in patients affected by the association of RLS and obstructive sleep apneas. Sleep Med. 2006, 7, 235–239. [Google Scholar] [CrossRef]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L., Jr.; Quan, S.F. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Darien, IL, USA, 2007; Volume 3. [Google Scholar]
- Katzan, I.; Speck, M.; Dopler, C.; Urchek, J.; Bielawski, K.; Dunphy, C.; Jehi, L.; Bae, C.; Parchman, A. The Knowledge Program: An innovative, comprehensive electronic data capture system and warehouse. In AMIA Annual Symposium Proceedings; American Medical Informatics Association: Bethesda, MD, USA, 2011; Volume 2011, pp. 683–692. Available online: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid = PMC3243190 (accessed on 13 December 2019).
- Ferri, R.; Lanuzza, B.; Cosentino, F.I.I.; Iero, I.; Tripodi, M.; Spada, R.S.; Toscano, G.; Marelli, S.; Aricò, D.; Bella, R.; et al. A single question for the rapid screening of restless legs syndrome in the neurological clinical practice. Eur. J. Neurol. 2007, 14, 1016–1021. [Google Scholar] [CrossRef]
- Walters, A.S.; Frauscher, B.; Allen, R.; Benes, H.; Chaudhuri, K.R.; Garcia-Borreguero, D.; Lee, H.B.; Picchietti, D.L.; Trenkwalder, C.; Martinez-Martin, P.; et al. Review of Diagnostic Instruments for the Restless Legs syndrome/Willis-Ekbom Disease (RLS/WED): Critique and Recommendations. J. Clin. Sleep Med. 2014, 10, 1343–1349. [Google Scholar] [CrossRef]
- International Restless Legs Syndrome Study Group. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003, 4, 121–132. [Google Scholar] [CrossRef]
- Trotti, L.M.; Goldstein, C.A.; Harrod, C.G.; Koo, B.B.; Sharon, D.; Zak, R.; Chervin, R.D. Quality measures for the care of adult patients with restless legs syndrome. J. Clin. Sleep Med. 2015, 11, 293–310. [Google Scholar] [CrossRef]
- Wunderlich, G.R.; Evans, K.R.; Sills, T.; Pollentier, S.; Reess, J.; Allen, R.P.; Hening, W.; Waltersf, A.S. The International Restless Legs Syndrome Study Group. An item response analysis of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med. 2005, 6, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Trenkwalder, C.; Kohnen, R.; Allen, R.P.; Beneš, H.; Ferini-Strambi, L.; Garcia-Borreguero, D.; Hadjigeorgiou, G.M.; Happe, S.; Högl, B.; Hornyak, M.; et al. Clinical trials in restless legs syndrome—Recommendations of the European RLS Study Group (EURLSSG). Mov. Disord. 2007, 22, S495–S504. [Google Scholar] [CrossRef]
- Hornyak, M.; Trenkwalder, C.; Kohnen, R.; Scholz, H. Efficacy and safety of dopamine agonists in restless legs syndrome. Sleep Med. 2012, 13, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Centers of Medicare & Medicaid Services. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-0009R2); CMS Gov.: Baltimore, MD, USA, 2008.
- McNemar, Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 1947, 12, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 1987. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–68. [Google Scholar] [CrossRef]
- Stehlik, R.; Ulfberg, J.; Zou, D.; Hedner, J.; Grote, L. Perceived sleep deficit is a strong predictor of RLS in multisite pain—A population based study in middle aged females. Scand. J. Pain 2017, 17, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Myc, L.A.; Churnin, I.T.; Jameson, M.J.; Davis, E.M. Treatment of Comorbid Obstructive Sleep Apnea by Upper Airway Stimulation Results in Resolution of Debilitating Symptoms of Restless Legs Syndrome. J. Clin. Sleep Med. 2018, 14, 1797–1800. [Google Scholar] [CrossRef]
- Patton, S.M.; Ponnuru, P.; Snyder, A.M.; Podskalny, G.D.; Connor, J.R. Hypoxia-inducible factor pathway activation in restless legs syndrome patients. Eur. J. Neurol. 2011, 18, 1329–1335. [Google Scholar] [CrossRef]
- Ding, Z.; Stehlik, R.; Hedner, J.; Ulfberg, J.; Grote, L. Chronic pulmonary disease is associated with pain spreading and restless legs syndrome in middle-aged women—A population-based study. Sleep Breath. 2019, 23, 135–142. [Google Scholar] [CrossRef]
- Earley, C.J.; Connor, J.; Garcia-Borreguero, D.; Jenner, P.; Winkelman, J.; Zee, P.C.; Allen, R. Altered Brain iron homeostasis and dopaminergic function in Restless Legs Syndrome (Willis-Ekbom Disease). Sleep Med. 2014, 15, 1288–1301. [Google Scholar] [CrossRef]
- Lo Coco, D.; Mattaliano, A.; Coco, A.L.; Randisi, B. Increased frequency of restless legs syndrome in chronic obstructive pulmonary disease patients. Sleep Med. 2009, 10, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Salminen, A.V.; Rimpilä, V.; Polo, O. Peripheral hypoxia in restless legs syndrome (Willis-Ekbom disease). Neurology 2014, 82, 1856–1861. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.; O’Connor, R.C.; Grubb, N.; O’Carroll, R. Type D personality predicts poor medication adherence in myocardial infarction patients. Psychol Health 2011, 26, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Broström, A.; Strömberg, A.; Mårtensson, J.; Ulander, M.; Harder, L.; Svanborg, E. Association of Type D personality to perceived side effects and adherence in CPAP-treated patients with OSAS. J. Sleep Res. 2007, 16, 439–447. [Google Scholar] [CrossRef] [PubMed]
| All Patients N = 434 | PAP N = 325 | Control N = 109 | p-Value | |
|---|---|---|---|---|
| Age, years | 51.9 ± 13.4 | 53.0 ± 13.0 | 48.9 ± 14.0 | 0.008 |
| Female | 219 (50.5%) | 154 (47.4%) | 65 (59.6%) | 0.035 |
| Caucasian | 337 (77.6%) | 258 (79.4%) | 79 (72.5%) | 0.087 |
| Married | 242 (55.8%) | 190 (58.5%) | 52 (47.7%) | 0.170 |
| Median income (×$1000) | 53.3 ± 17.5 | 53.9 ± 17.6 | 51.6 ± 17.3 | 0.244 |
| Smoking status | ||||
| Current | 48 (11.1%) | 34 (10.5%) | 14 (12.8%) | 0.473 |
| Former | 142 (32.7%) | 111 (34.2%) | 31 (28.4%) | |
| Never | 193 (44.5%) | 142 (43.7%) | 51 (46.8%) | |
| Missing | 51 (11.8%) | 38 (11.7%) | 13 (11.9%) | |
| Coronary artery disease | 32 (7.4%) | 24 (7.4%) | 8 (7.3%) | 1.000 |
| Cancer | 76 (17.5%) | 55 (16.9%) | 21 (19.3%) | 0.563 |
| Chronic renal failure | 15 (3.5%) | 10 (3.1%) | 5 (4.6%) | 0.544 |
| Depression | 116 (26.7%) | 81 (24.9%) | 35 (32.1%) | 0.169 |
| Diabetes | 98 (22.6%) | 68 (20.9%) | 30 (27.5%) | 0.185 |
| Hypertension | 168 (38.7%) | 124 (38.2%) | 44 (40.4%) | 0.733 |
| Stroke | 15 (3.5%) | 8 (2.5%) | 7 (6.4%) | 0.067 |
| AHI | 20 (9,44) | 22 (11,49) | 13 (8,32) | <0.001 |
| BMI, kg/m2 | 33 (28,38) | 33 (29,38) | 33 (27,39) | 0.389 |
| Neck circumference, cm | 40 (37, 43.25) | 40 (38, 43.5) | 39.5 (36,43) | 0.101 |
| Family history of RLS | 48 (11.1%) | 35 (10.8%) | 13 (11.9%) | 0.726 |
| RLS medications | 202 (46.5%) | 146 (44.9%) | 56 (51.4%) | 0.268 |
| Exacerbating medications | 198 (45.6%) | 146 (44.9%) | 52 (47.7%) | 0.657 |
| Any caffeine consumption | 325 (74.9%) | 252 (77.5%) | 73 (67.0%) | 0.054 |
| Days from baseline to PSG | 23.5 (6,41) | 23 (7,38) | 25 (5,44) | 0.879 |
| Days from PSG to follow-up | 113 (75,169) | 125 (86,172) | 71 (42,131) | <0.001 |
| Baseline IRLS Score | 16.2 ± 8.3 | 16.3 ± 8.3 | 15.9 ± 8.2 | 0.596 |
| Baseline average sleep time | ||||
| <7 h | 286 (65.9%) | 216 (66.5%) | 70 (64.2%) | 0.615 |
| 7–9 h | 112 (25.8%) | 83 (25.5%) | 29 (26.6%) | |
| >9 h | 27 (6.2%) | 19 (5.8%) | 8 (7.3%) |
| PAP N = 325 | Control N = 109 | Estimated Difference | p-Value | Estimated Difference, Adjusted † | p-Value | |
|---|---|---|---|---|---|---|
| Baseline | 16.3 ± 8.3 | 15.9 ± 8.2 | ||||
| Follow-up | 11.5 ± 8.9 | 13.2 ± 8.4 | ||||
| Change | −4.8 ± 7.5 | −2.7 ± 7.6 | −2.1 (−3.7, −0.4) | 0.014 | −1.8 (−3.6, 0.00) | 0.050 |
| Effect Size | −0.57 | −0.33 |
| PAP Adherent N = 237 | PAP Non-Adherent N = 76 | Control N = 109 | PAP Adherent vs. Control Estimated Difference | PAP Non-Adherent vs. Control Estimated Difference | PAP Adherent vs. PAP Non-Adherent Estimated Difference | |
|---|---|---|---|---|---|---|
| Baseline | 16.4 ± 8.3 | 15.4 ± 8.4 | 15.9 ± 8.2 | |||
| Follow-up | 11.1 ± 8.3 | 12.4 ± 9.9 | 13.2 ± 8.4 | |||
| Change, unadjusted | −5.3 ± 7.4 | −3.0 ± 7.0 | −2.7 ± 7.6 | −2.6 (−4.4, −0.7) p = 0.010 | −0.3 (−2.7, 2.1) p > 0.999 | −2.3 (−4.4, −0.2) p = 0.065 |
| Change, adjusted † | −2.3 (−4.3, −0.3) p = 0.045 | −0.1 (−2.6, 2.5) p > 0.999 | −2.2 (−4.9, 0.0) p = 0.091 | |||
| Effect Size | −0.64 | −0.35 | −0.32 |
| PAP Adherent N = 80 | PAP Non-Adherent N = 50 | Control N = 109 | PAP Adherent vs. Control | PAP Non-Adherent vs. Control | PAP Adherent vs. PAP Non-Adherent | |
|---|---|---|---|---|---|---|
| Estimated Difference | Estimated Difference | Estimated Difference | ||||
| Baseline | 15.4 (7.1) | 16.4 (8.7) | 15.9 (8.2) | |||
| Follow-up Imp | 10.1 (7.5) | 12.1 (9.4) | 13.2 (8.4) | |||
| Change, unadjusted | −5.2 (7.8) | −4.4 (6.1) | −2.7 (7.6) | −2.5 (−4.8, −0.2) p = 0.066 | −1.7 (−4.4, 0.9) p = 0.481 | −0.8 (−3.5, 2.0) p > 0.999 |
| Change, adjusted † | −2.0 (−4.6, 0.6) p = 0.292 | −1.2 (−4.2, 1.7) p > 0.999 | −0.8 (−3.7, 2.2) p > 0.999 | |||
| Effect Size | −0.73 | −0.51 | −0.33 |
| Follow-Up | ||||||||
|---|---|---|---|---|---|---|---|---|
| All Patients | PAP Group | Control Group | ||||||
| No | Yes | No | Yes | No | Yes | |||
| Baseline | RLS Medication Use | No | 174 (40.1%) | 58 (13.4%) | 129 (39.7%) | 50 (15.4%) | 45 (41.3%) | 8 (7.3%) |
| Yes | 17 (3.9%) | 185 (42.6%) | 11 (3.4%) | 135 (41.5%) | 6 (5.5%) | 50 (45.9%) | ||
| p-Value | <0.001 | <0.001 | 0.791 † | |||||
| Exacerbating Medication Use | No | 197 (45.4%) | 39 (9.0%) | 150 (46.2%) | 29 (8.9%) | 47 (43.1%) | 10 (9.2%) | |
| Yes | 19 (4.4%) | 179 (41.2%) | 16 (4.9%) | 130 (40.0%) | 3 (2.8%) | 49 (45.0%) | ||
| p-Value | 0.013 | 0.074 | 0.092 † | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lakshmanan, S.; Thompson, N.R.; Pascoe, M.; Mehra, R.; Foldvary-Schaefer, N.; Katzan, I.L.; Walia, H.K. Impact of Positive Airway Pressure on International Restless Legs Syndrome Score in Sleep Disordered Breathing. J. Clin. Med. 2019, 8, 2212. https://doi.org/10.3390/jcm8122212
Lakshmanan S, Thompson NR, Pascoe M, Mehra R, Foldvary-Schaefer N, Katzan IL, Walia HK. Impact of Positive Airway Pressure on International Restless Legs Syndrome Score in Sleep Disordered Breathing. Journal of Clinical Medicine. 2019; 8(12):2212. https://doi.org/10.3390/jcm8122212
Chicago/Turabian StyleLakshmanan, Seetha, Nicolas R. Thompson, Maeve Pascoe, Reena Mehra, Nancy Foldvary-Schaefer, Irene L. Katzan, and Harneet K. Walia. 2019. "Impact of Positive Airway Pressure on International Restless Legs Syndrome Score in Sleep Disordered Breathing" Journal of Clinical Medicine 8, no. 12: 2212. https://doi.org/10.3390/jcm8122212
APA StyleLakshmanan, S., Thompson, N. R., Pascoe, M., Mehra, R., Foldvary-Schaefer, N., Katzan, I. L., & Walia, H. K. (2019). Impact of Positive Airway Pressure on International Restless Legs Syndrome Score in Sleep Disordered Breathing. Journal of Clinical Medicine, 8(12), 2212. https://doi.org/10.3390/jcm8122212






