Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective
Abstract
1. Introduction
2. Experimental Section
3. Results
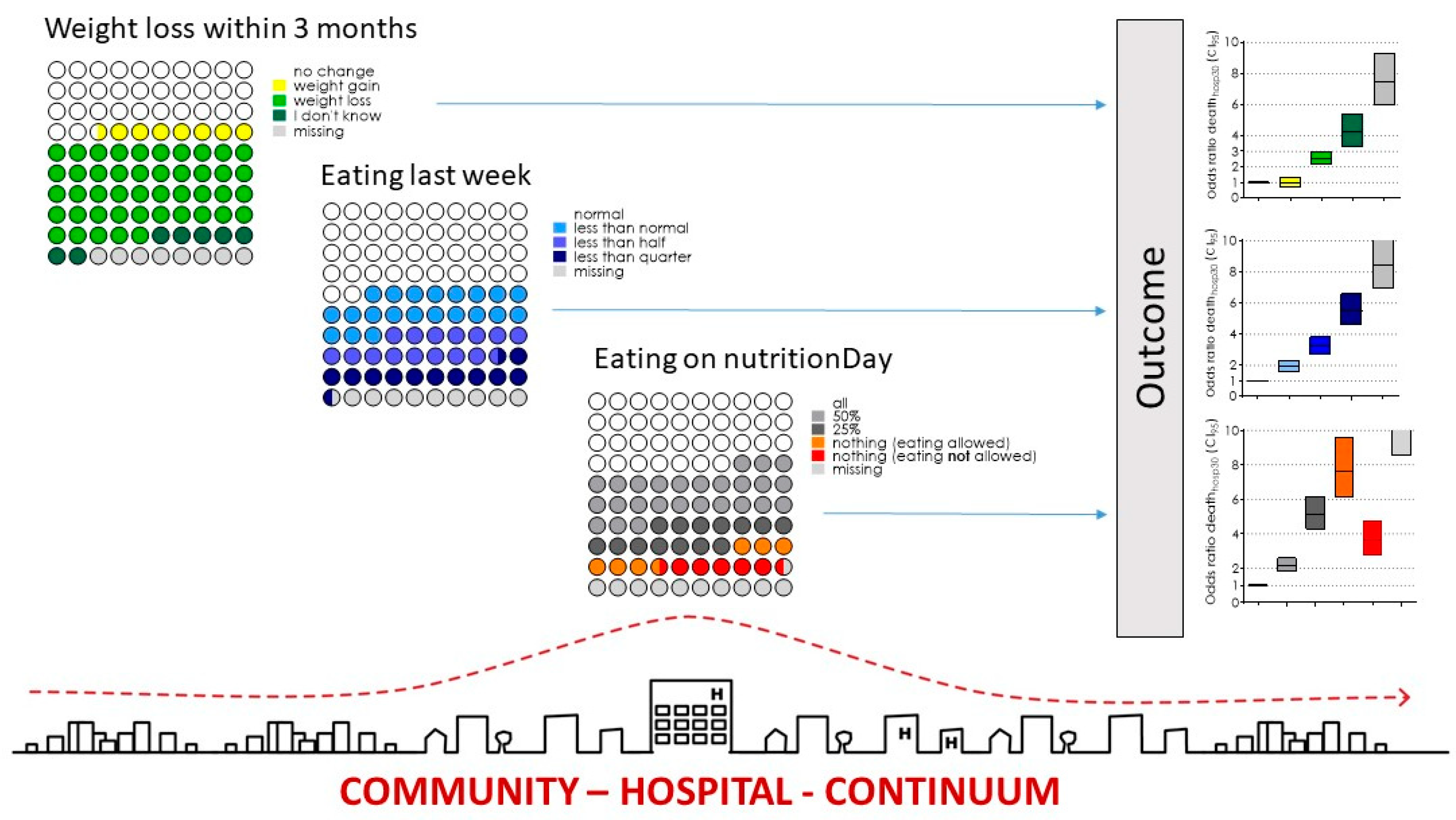
3.1. Prevalence of Nutrition Risk Factors
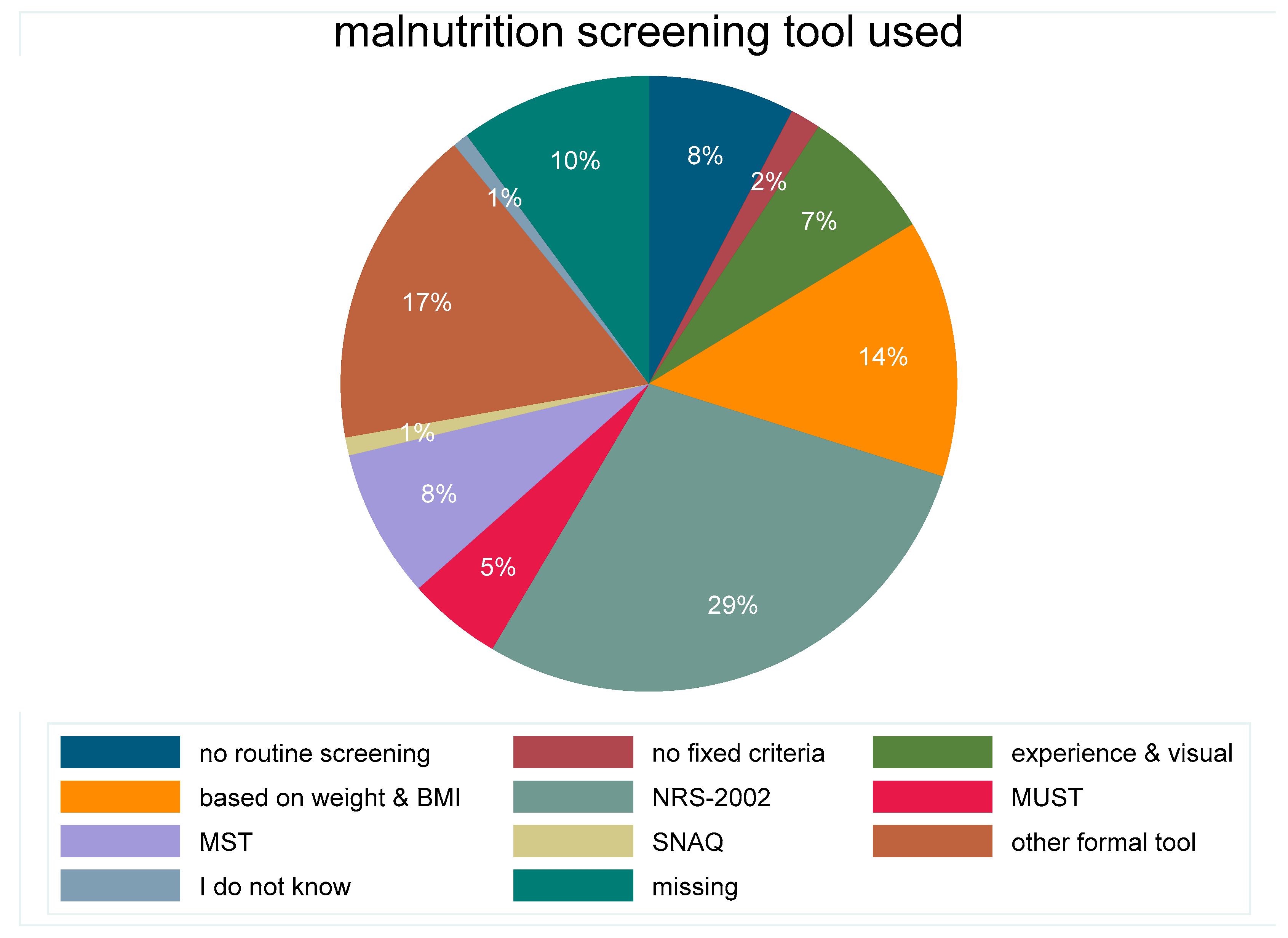
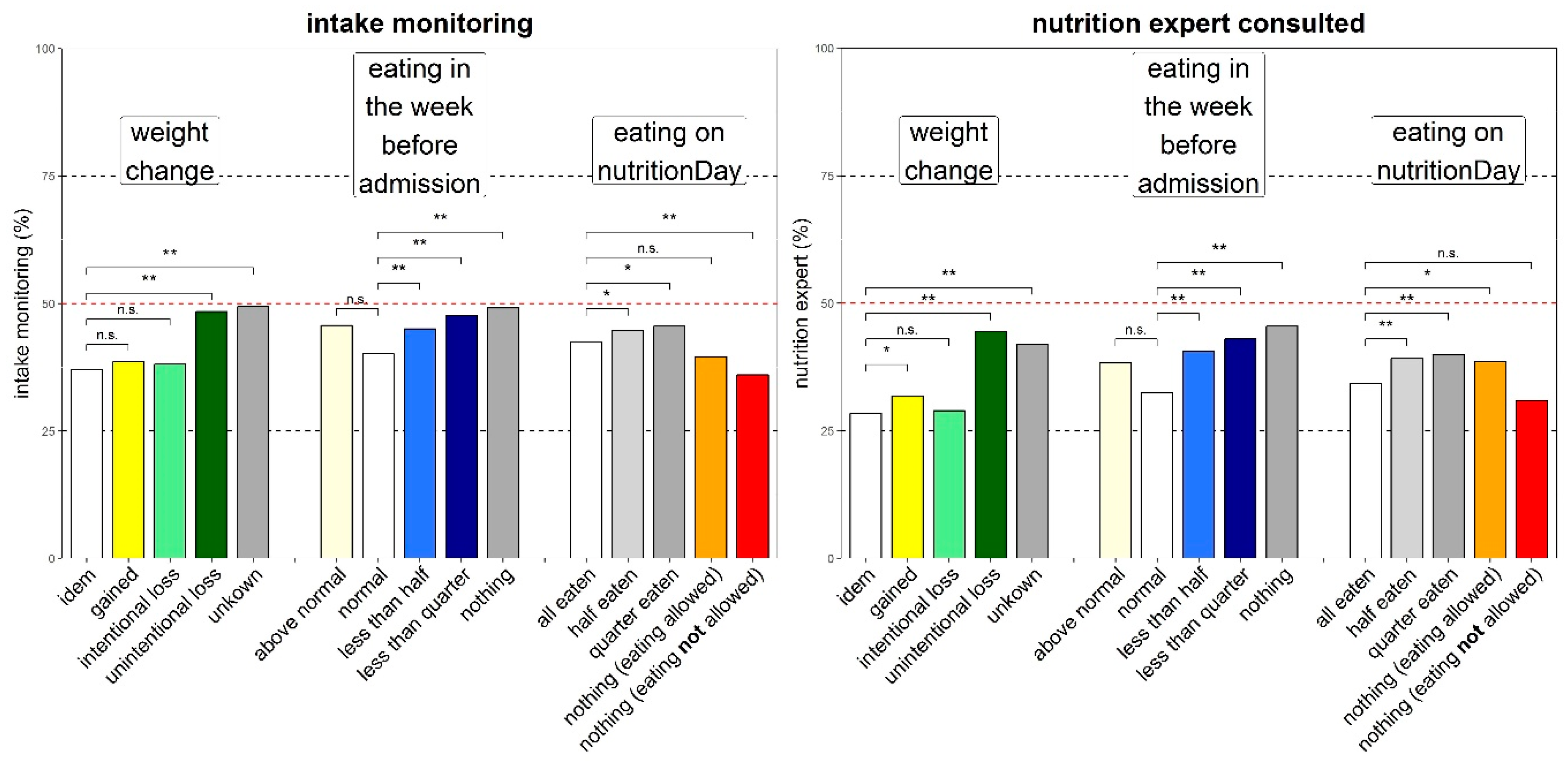
3.2. Nutrition Care
3.2.1. Food provision
3.2.2. Process indicators
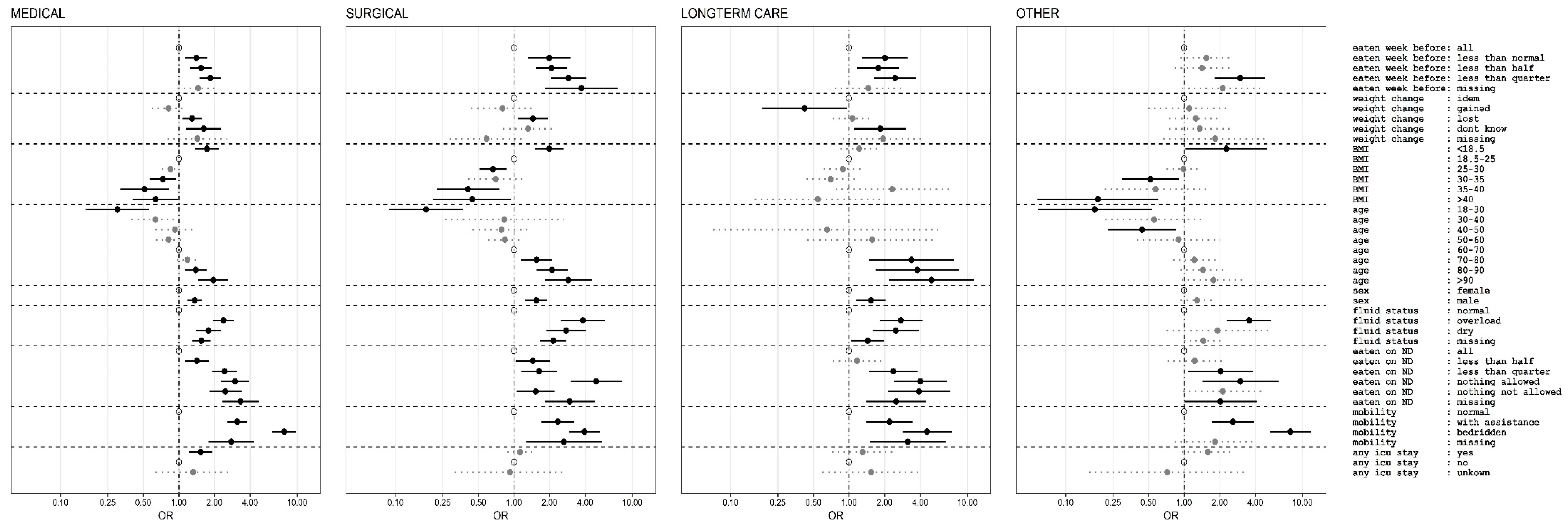
3.3. Outcome
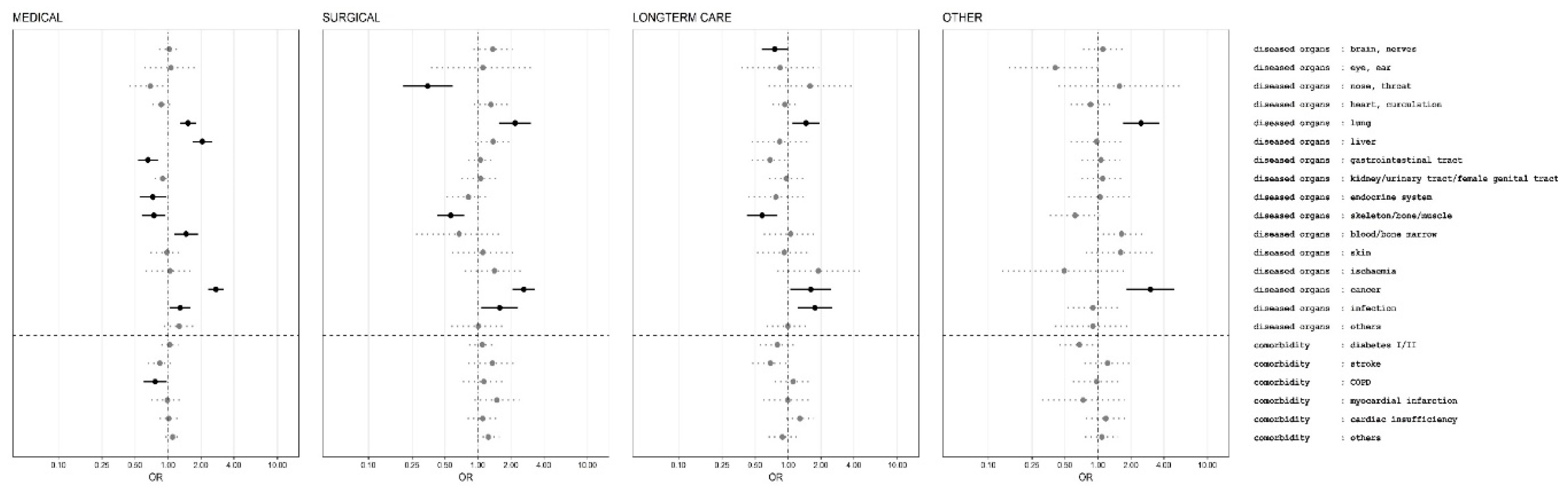
Multivariate Outcome Analysis
4. Discussion
4.1. Nutrition Care
4.2. Political Action Derived from Observations
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Butterworth, C.E., Jr. Editorial: Malnutrition in the hospital. JAMA 1974, 230, 879. [Google Scholar] [CrossRef]
- Bistrian, B.R.; Blackburn, G.L.; Vitale, J.; Cochran, D.; Naylor, J. Prevalence of malnutrition in general medical patients. JAMA 1976, 235, 1567–1570. [Google Scholar] [CrossRef]
- Council of Europe Committee of Ministers. Resolution ResAP (2003) 3 on Food and Nutritional Care in Hospitals. Available online: https://search.coe.int/ (accessed on 18 November 2019).
- Hiesmayr, M.; Schindler, K.; Pernicka, E.; Schuh, C.; Schoeniger-Hekele, A.; Bauer, P.; Laviano, A.; Lovell, A.D.; Mouhieddine, M.; Schuetz, T.; et al. Decreased food intake is a risk factor for mortality in hospitalised patients: The NutritionDay survey 2006. Clin. Nutr. 2009, 28, 484–491. [Google Scholar] [CrossRef]
- Hiesmayr, M.; Frantal, S.; Schindler, K.; Themessl-Huber, M.; Mouhieddine, M.; Schuh, C.; Pernicka, E.; Schneider, S.; Singer, P.; Ljunqvist, O.; et al. The Patient- And Nutrition-Derived Outcome Risk Assessment Score (PANDORA): Development of a Simple Predictive Risk Score for 30-Day In-Hospital Mortality Based on Demographics, Clinical Observation, and Nutrition. PLoS ONE 2015, 10, e0127316. [Google Scholar] [CrossRef]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Schindler, K.; Pernicka, E.; Laviano, A.; Howard, P.; Schutz, T.; Bauer, P.; Grecu, I.; Jonkers, C.; Kondrup, J.; Ljungqvist, O.; et al. How nutritional risk is assessed and managed in European hospitals: A survey of 21,007 patients findings from the 2007–2008 cross-sectional nutritionDay survey. Clin. Nutr. 2010, 29, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Navarro, D.A.; Boaz, M.; Krause, I.; Elis, A.; Chernov, K.; Giabra, M.; Levy, M.; Giboreau, A.; Kosak, S.; Mouhieddine, M.; et al. Improved meal presentation increases food intake and decreases readmission rate in hospitalizd patients. Clin. Nutr. 2016, 35, 1153–1158. [Google Scholar] [CrossRef]
- Correia, M.I.; Waitzberg, D.L. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin. Nutr. 2003, 22, 235–239. [Google Scholar] [CrossRef]
- Lim, S.L.; Ong, K.C.; Chan, Y.H.; Loke, W.C.; Ferguson, M.; Daniels, L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin. Nutr. 2012, 31, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Reber, E.; Norman, K.; Endrich, O.; Schuetz, P.; Frei, A.; Stanga, Z. Economic Challenges in Nutritional Management. J. Clin. Med. 2019, 8, 1005. [Google Scholar] [CrossRef]
- Reber, E.; Strahm, R.; Bally, L.; Schuetz, P.; Stanga, Z. Efficacy and Efficiency of Nutritional Support Teams. J. Clin. Med. 2019, 8, 1281. [Google Scholar] [CrossRef] [PubMed]
- Bendavid, I.; Singer, P.; Theilla, M.; Themessl-Huber, M.; Sulz, I.; Mouhieddine, M.; Schuh, C.; Mora, B.; Hiesmayr, M. NutritionDay ICU: A 7 year worldwide prevalence study of nutrition practice in intensive care. Clin. Nutr. 2017, 36, 1122–1129. [Google Scholar] [CrossRef] [PubMed]
- Schindler, K.; Pichard, C.; Sulz, I.; Volkert, D.; Streicher, M.; Singer, P.; Ljungqvist, O.; Van Gossum, A.; Bauer, P.; Hiesmayr, M. nutritionDay: 10 years of growth. Clin. Nutr. 2017, 36, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Streicher, M.; Themessl-Huber, M.; Schindler, K.; Sieber, C.C.; Hiesmayr, M.; Volkert, D. nutritionDay in Nursing Homes-The Association of Nutritional Intake and Nutritional Interventions With 6-Month Mortality in Malnourished Residents. J. Am. Med. Dir. Assoc. 2017, 18, 162–168. [Google Scholar] [CrossRef]
- Schindler, K.; Themessl-Huber, M.; Hiesmayr, M.; Kosak, S.; Lainscak, M.; Laviano, A.; Ljungqvist, O.; Mouhieddine, M.; Schneider, S.; de van der Schueren, M.; et al. To eat or not to eat? Indicators for reduced food intake in 91,245 patients hospitalized on nutritionDays 2006–2014 in 56 countries worldwide: A descriptive analysis. Am. J. Clin. Nutr. 2016, 104, 1393–1402. [Google Scholar] [CrossRef]
- Man, F.D. Optimal Nutrition Care for All (ONCA). Available online: https://european-nutrition.org (accessed on 21 August 2019).
- European Patient Forum. Available online: http://www.eu-patient.eu/ (accessed on 21 August 2019).
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Cardenas, D.; Bermudez, C.; Barazzoni, R. The Cartagena Declaration: A call for global commitment to fight for the right to nutritional care. Clin. Nutr. 2019. [Google Scholar] [CrossRef]
- United Nations. Sustainable Development Goals; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Cederholm, T.; Jensen, G.L.; Correia, M.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- World Health Organisation. Body Mass Index. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 10 September 2019).
- Frantal, S.; Pernicka, E.; Hiesmayr, M.; Schindler, K.; Bauer, P. Length bias correction in one-day cross-sectional assessments—The nutritionDay study. Clin. Nutr. 2016, 35, 522–527. [Google Scholar] [CrossRef]
- Schuetz, P.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Tribolet, P.; Bregenzer, T.; Braun, N.; et al. Individualised nutritional support in medical inpatients at nutritional risk: A randomised clinical trial. Lancet 2019, 393, 2312–2321. [Google Scholar] [CrossRef]
| 1. Within the hospital | ||
| a. Patients and their relatives | ||
| b. Care persons | ||
| i. Nurses | Screening, diet ordering, documentation | |
| ii. Physicians | Assessment, ordering, documentation, information | |
| iii. Dieticians | Assessment, documentation | |
| iv. Physiotherapists | Effect monitoring | |
| v. Speech Therapists | Swallowing disorders | |
| vi. Pharmacists | Clinical nutrition supply and counselling | |
| c. Kitchen/Catering services | ||
| i. Administrators | Budget | |
| ii. Chefs | Standards, variety, quality control | |
| iii. Kitchen aids | Presentation | |
| iv. Delivering staff | Monitoring | |
| d. Hospital administration | Budget, planning, controlling | |
| 2. Outside the hospital | ||
| a. Patients and relatives | ||
| b. Extramural medical services/family medicine/primary health care centres | ||
| c. Extramural care services/mobile nursing | ||
| d. Services for disabled and dependent persons | ||
| e. Local food producers | ||
| f. Medical food producing industries | ||
| 3. Scientific societies and stakeholder associations | ||
| a. Medical | Guidelines, standards | |
| b. Nursing | Guidelines, standards | |
| c. Dietician | Guidelines, standards | |
| d. Nutrition science | Research, standards | |
| e. Patient organizations | Guidelines | |
| 4. Policy maker | ||
| a. Health care system | Reimbursement | |
| b. Social affairs | Equity | |
| c. Agriculture | Local production integration | |
| d. Environmental affairs | Sustainable planning, waste prevention | |
| 5. Payers | ||
| a. Reimbursement of the nutrition care process in the whole health care system | ||
| b. Public procurement of food supply and services | ||
| Medical | Surgical | Long-Term Care | Others | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | n (%) | Mean ± SD | n (%) | Mean ± SD | n (%) | Mean ± SD | n (%) | Mean ± SD |
| Age (year) | 59,046 | 65.1 ± 17.2 | 61.2 ± 18.0 | 80.7 ± 12.4 | 61.2 ± 18.8 | |||
| Gender (female) | 28,535 (49%) | 30,445 (49%) | 6937 (62%) | 9992 (51%) | ||||
| Weight (kg) | 52,735 (89%) | 71.3 ± 19.4 | 71.9 ± 18.1 | 66.4 ± 16.9 | 71.8 ± 18.3 | |||
| Height (cm) | 52,735 | 166.1 ± 10.3 | 166.6 ± 10.2 | 163.0 ± 9.5 | 166.7 ± 10.4 | |||
| BMI * (kg·cm−2) | 52,735 | 25.7 ± 6.3 | 25.8 ± 5.8 | 24.9 ± 5.8 | 25.7 ± 5.9 | |||
| Weight change within three months | ||||||||
| Unchanged * | 19,139 (32%) | 25,164 (40%) | 3153 (28%) | 7338 (37%) | ||||
| Increase | 4335 (7.3%) | 4997 (8%) | 671 (6%) | 1990 (10%) | ||||
| Loss | 26,790 (45%) | 24,928 (39%) | 4989 (44%) | 7356 (37%) | ||||
| Do not know | 4020 (6.8%) | 3679 (6%) | 1339 (12%) | 1205 (6%) | ||||
| Missing | 4842 (8.2%) | 4521 (7%) | 1127 (10%) | 1887 (10%) | ||||
| Eating last week | ||||||||
| Normal * | 24,679 (42%) | 29,898 (47%) | 4731 (42%) | 9973 (50%) | ||||
| Less than normal | 12,613 (21%) | 12,618 (20%) | 2526 (22%) | 4047 (20%) | ||||
| Less than a half | 8979 (15%) | 7894 (12%) | 1628 (14%) | 2262 (11%) | ||||
| Less than a quarter | 7358 (12%) | 7691 (12%) | 1076 (9%) | 1433 (7%) | ||||
| Missing | 5497 (9.3%) | 5188 (8%) | 1318 (12%) | 2061 (10%) | ||||
| Eating on nutritionDay | ||||||||
| All * | 22,046 (37%) | 22,232 (35%) | 4131 (37%) | 8496 (43%) | ||||
| Half | 15,327 (26%) | 15,141 (24%) | 3363 (30%) | 5054 (26%) | ||||
| Quarter | 8256 (14%) | 7262 (11%) | 1592 (14%) | 2206 (11%) | ||||
| Nothing (eating allowed) | 3696 (6.3%) | 3666 (6%) | 698 (6%) | 927 (5%) | ||||
| Nothing (eating not allowed) | 3686 (6.2%) | 8717 (14%) | 372 (3%) | 875 (4%) | ||||
| Missing | 6115 (10%) | 6271 (10%) | 1123 (10%) | 2218 (11%) | ||||
| Mobility on nutritionDay | ||||||||
| Normal | 35,846 (61%) | 37,439 (59%) | 3731 (33%) | 12,227 (62%) | ||||
| With help | 12,299 (21%) | 14,110 (22%) | 4557 (40%) | 3838 (19%) | ||||
| Bedridden | 5587 (9.4%) | 6832 (11%) | 1841 (16%) | 1732 (9%) | ||||
| Missing | 5394 (9.1%) | 4908 (8%) | 1150 (10%) | 1979 (10%) | ||||
| Fluid status on nutritionDay | ||||||||
| Normal * | 28,499 (48%) | 3619 (6%) | 1147 (10%) | 1284 (6%) | ||||
| Overload | 6214 (11%) | 33,636 (53%) | 5836 (51%) | 1142 (58%) | ||||
| Deficit | 3267 (6%) | 2723 (4%) | 985 (9%) | 886 (4%) | ||||
| Missing | 21,146 (36%) | 23,311 (37%) | 3311 (29%) | 6178 (31%) | ||||
| Any Intensive Care Stay before nutritionDay | 4143 (7.0%) | 10,465 (17%) | 564 (5%) | 1464 (8%) | ||||
| Medical specialty | ||||||||
| General internal medicine | 29,173 (49%) | 3958 (6%) | ||||||
| Oncology | 11,412 (19%) | 1953 (3%) | ||||||
| Gastroenterology/Hepatology | 9744 (16%) | 1350 (2%) | ||||||
| Cardiology | 5401 (9.1%) | 1405 (2%) | ||||||
| Nephrology | 1785 (3.0%) | 370 (1%) | ||||||
| Infectiology | 1611 (2.7%) | 149 (0%) | ||||||
| Neurology | 592 (1%) | 4442 (22%) | ||||||
| Psychiatry | 17 (0%) | 1409 (7%) | ||||||
| ENT | 2195 (3%) | 1272 (6%) | ||||||
| General surgery | 28,310 (45%) | |||||||
| Cardiothorcic surgery | 2013 (3%) | |||||||
| Orthopaedic surgery | 7803 (12%) | |||||||
| Trauma | 2160 (3%) | |||||||
| Neurosurgery | 1717 (3%) | |||||||
| Gynecology | 1198 (2%) | 1151(6%) | ||||||
| Long-term care | 526 (1%) | 9885 (88%) | ||||||
| Other | 5955 (9%) | 11,401(58%) | ||||||
| Pediatrics | 46 (0%) | 101 (1%) | ||||||
| Geriatrics | 1572 (2%) | 1785 (12%) | ||||||
| Oral | ONS | EN | PN | Othercomb | ||
|---|---|---|---|---|---|---|
| Medical | all | 19,484 (88.4%) | 1651 (7.5%) | 1154 (5.2%) | 289 (1.3%) | 794 (3.6%) |
| n = 59,126 | half | 13,657 (89.1%) | 1560 (10.2%) | 770 (5%) | 311 (2%) | 544 (3.5%) |
| quarter | 7176 (87%) | 1132 (13.7%) | 426 (5.2%) | 354 (4.3%) | 332 (4%) | |
| nothing_a | 2760 (74.7%) | 448 (12.1%) | 428 (11.6%) | 306 (8.3%) | 278 (7.5%) | |
| nothing_na | 2391 (65%) | 226 (6.1%) | 329 (8.9%) | 417 (11.3%) | 521 (14.1%) | |
| missing | 3377 (55.2%) | 462 (7.6%) | 1083 (17.7%) | 381 (6.2%) | 323 (5.3%) | |
| Total | 48,845 (82.6%) | 5479 (9.3%) | 4190 (7.1%) | 2058 (3.5%) | 2792 (4.7%) | |
| Surgical | all | 19,368 (87.1%) | 1468 (6.6%) | 1286 (5.8%) | 429 (1.9%) | 1184 (5.3%) |
| n = 63,289 | half | 13,106 (86.6%) | 1294 (8.5%) | 913 (6%) | 506 (3.3%) | 906 (6%) |
| quarter | 6066 (83.5%) | 779 (10.7%) | 472 (6.5%) | 381 (5.2%) | 536 (7.4%) | |
| nothing_a | 2384 (65%) | 324 (8.8%) | 448 (12.2%) | 415 (11.3%) | 573 (15.6%) | |
| nothing_na | 4611 (53%) | 301 (3.5%) | 810 (9.3%) | 1535 (17.6%) | 1906 (21.9%) | |
| missing | 3596 (57.3%) | 392 (6.3%) | 819 (13.1%) | 605 (9.6%) | 689 (11%) | |
| Total | 49,131 (77.6%) | 4558 (7.2%) | 4748 (7.5%) | 3871 (6.1%) | 5794 (9.2%) | |
| Longterm | all | 3480 (84.3%) | 824 (19.9%) | 370 (9%) | 15 (0.4%) | 135 (3.3%) |
| n = 11,279 | half | 2858 (85%) | 790 (23.5%) | 268 (8%) | 29 (0.9%) | 113 (3.4%) |
| quarter | 1312 (82.4%) | 482 (30.3%) | 130 (8.2%) | 28 (1.8%) | 70 (4.4%) | |
| nothing_a | 473 (67.8%) | 225 (32.2%) | 111 (15.9%) | 41 (5.9%) | 53 (7.6%) | |
| nothing_na | 200 (53.8%) | 75 (20.2%) | 85 (22.8%) | 46 (12.4%) | 43 (11.6%) | |
| missing | 672 (59.8%) | 177 (15.8%) | 247 (22%) | 36 (3.2%) | 45 (4%) | |
| Total | 8995 (79.7%) | 2573 (22.8%) | 1211 (10.7%) | 195 (1.7%) | 459 (4.1%) | |
| Others | all | 7435 (87.5%) | 509 (6%) | 672 (7.9%) | 70 (0.8%) | 392 (4.6%) |
| n = 19,776 | half | 4398 (87%) | 380 (7.5%) | 403 (8%) | 84 (1.7%) | 258 (5.1%) |
| quarter | 1885 (85.4%) | 267 (12.1%) | 147 (6.7%) | 78 (3.5%) | 118 (5.3%) | |
| nothing_a | 628 (67.7%) | 84 (9.1%) | 160 (17.3%) | 68 (7.3%) | 90 (9.7%) | |
| nothing_na | 544 (62.2%) | 49 (5.6%) | 100 (11.4%) | 101 (11.5%) | 131 (15%) | |
| missing | 1214 (54.7%) | 124 (5.6%) | 355 (16%) | 91 (4.1%) | 128 (5.8%) | |
| Total | 16,104 (81.4%) | 1413 (7.1%) | 1837 (9.3%) | 492 (2.5%) | 1117 (5.6%) |
| Outcome | Surgery | Medical | Longterm | Other |
|---|---|---|---|---|
| in hospital | 5740 (9.1%) | 4639 (7.8%) | 1560 (13.8%) | 2303 (11.6%) |
| transfer other hospital | 1500 (2.4%) | 1343 (2.3%) | 290 (2.6%) | 390 (2%) |
| transfer longterm care | 1424 (2.2%) | 2109 (3.6%) | 1471 (13%) | 574 (2.9%) |
| transfer rehabilitation | 1967 (3.1%) | 1341 (2.3%) | 441 (3.9%) | 535 (2.7%) |
| discharge home | 39,705 (62.7%) | 36,439 (61.6%) | 4710 (41.8%) | 11,049 (55.9%) |
| death within 30 days | 1053 (1.7%) | 2721 (4.6%) | 541 (4.8%) | 512 (2.6%) |
| other destination | 948 (1.5%) | 1033 (1.7%) | 322 (2.9%) | 376 (1.9%) |
| missing | 10,952 (17.3%) | 9501 (16.1%) | 1944 (17.2%) | 4037 (20.4%) |
| Problem Area | Political Action |
|---|---|
| Education of all healthcare professionals directly involved in patient care in disease related malnutrition and nutrition care insufficient. | Mandatory inclusion of disease related malnutrition and nutrition care processes in curriculum for nurses, doctors, dieticians, etc. |
| Limited awareness of the importance of nutrition in disease states in the public especially the population at risk. | National nutrition care campaigns targeting the general population, residents of nursing homes and also targeted nutrition campaigns run through general practitioners. Availability of an education platform for patients and families. |
| Nomination of responsible person or team for patient nutrition care missing. No monitoring of nutrition care processes part of hospital quality control. | Mandatory designation of a nutrition team/responsible person in each hospital with a threefold responsibility: coordination of expertise, definition of processes and regular benchmarking of applications of processes through initiatives like nutritionDay, the Dutch nutrition benchmarking program, the British malnutrition awareness week and the analysis of electronic patients records. |
| Inconsistent screening and collection of data. Missing documentation of nutrition risk factors and communication of nutrition status and care at discharge to the next sector. | Mandatory inclusion of data in a nutrition care benchmarking program. Definition and inclusion of mandatory harmonized fields for a systematic collection and documentation of nutrition risks factors and nutrition care processes in the electronic patient record. Inclusion of planned nutrition treatment recorded in patient’s discharge letter/information to patients and relatives. |
| Missing patients and families empowerment due to insufficient communication of nutrition status and care to the patients and their families. | Mandatory monitoring of communication processes in quality assurance programs. |
| Lack of a harmonized reimbursement schemes for nutrition related processes such as screening, assessment and treatment such as oral nutritional supplements, enteral or parenteral nutrition. | Clear reimbursement schemes. |
| Missing a partnership for hospital food provision and of a positive image for hospital food. | Creation of a public best practice platform for food provision in hospitals. Supported use of local food in hospital kitchen for the creation of wealth not only for the community using the hospital but also for the local community. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hiesmayr, M.; Tarantino, S.; Moick, S.; Laviano, A.; Sulz, I.; Mouhieddine, M.; Schuh, C.; Volkert, D.; Simon, J.; Schindler, K. Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective. J. Clin. Med. 2019, 8, 2048. https://doi.org/10.3390/jcm8122048
Hiesmayr M, Tarantino S, Moick S, Laviano A, Sulz I, Mouhieddine M, Schuh C, Volkert D, Simon J, Schindler K. Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective. Journal of Clinical Medicine. 2019; 8(12):2048. https://doi.org/10.3390/jcm8122048
Chicago/Turabian StyleHiesmayr, Michael, Silvia Tarantino, Sigrid Moick, Alessandro Laviano, Isabella Sulz, Mohamed Mouhieddine, Christian Schuh, Dorothee Volkert, Judit Simon, and Karin Schindler. 2019. "Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective" Journal of Clinical Medicine 8, no. 12: 2048. https://doi.org/10.3390/jcm8122048
APA StyleHiesmayr, M., Tarantino, S., Moick, S., Laviano, A., Sulz, I., Mouhieddine, M., Schuh, C., Volkert, D., Simon, J., & Schindler, K. (2019). Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective. Journal of Clinical Medicine, 8(12), 2048. https://doi.org/10.3390/jcm8122048






