Coping Strategies in Male Patients under Treatment for Substance Use Disorders and/or Severe Mental Illness: Influence in Clinical Course at One-Year Follow-Up
Abstract
1. Introduction
2. Experimental Section
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Sociodemographic and Clinical Variables
2.3.2. Coping Strategies Assessment
2.4. Data Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
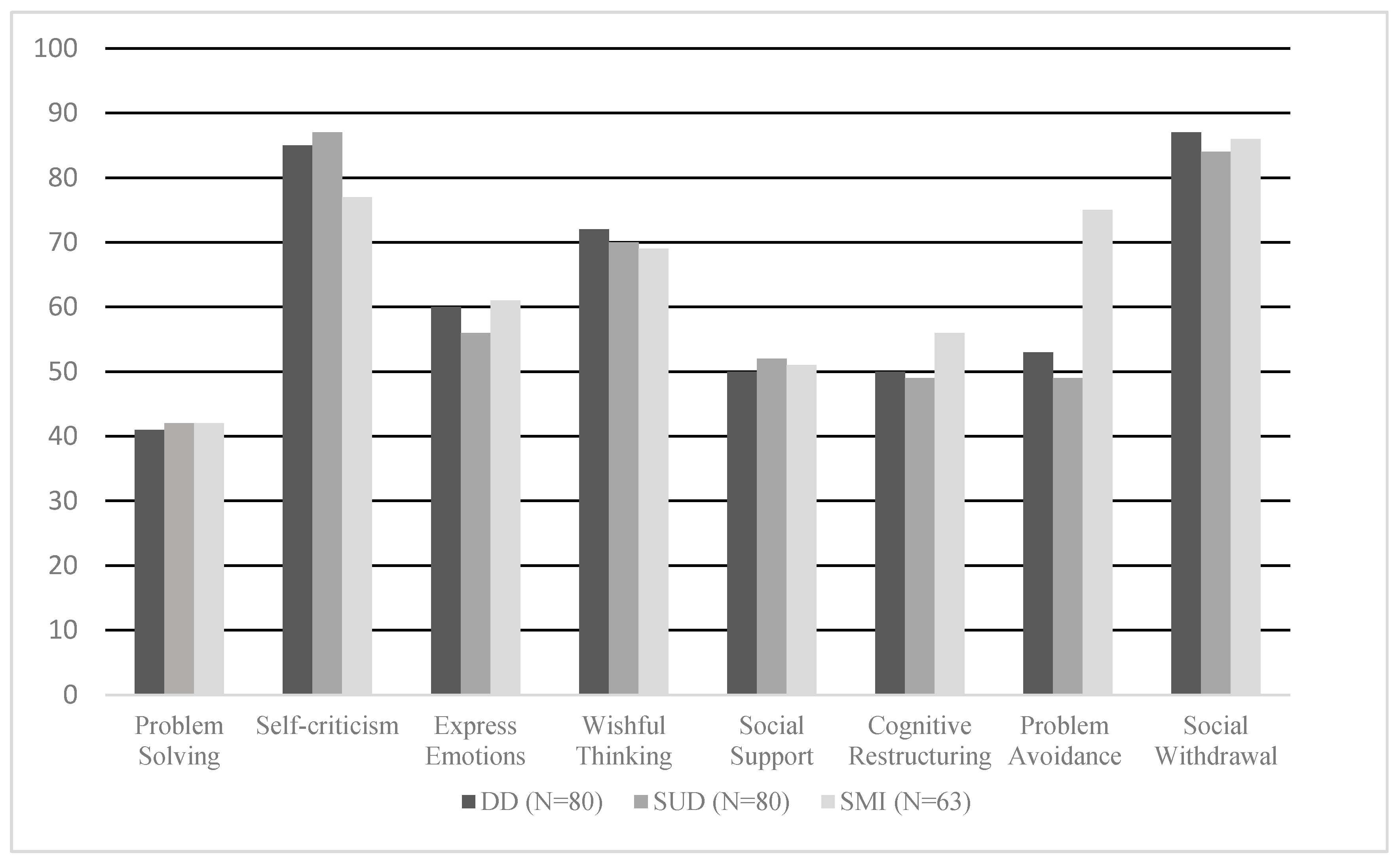
3.2. Coping Strategies in the DD, SUD, and SMI groups
3.3. Follow-Up Data at Three, Six, and Twelve Months
3.4. Differences in Coping Strategies Considering One-Year Follow-Up Data
3.5. Coping Strategies as Predictors of Relapses at One-Year Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nava Quiroz, C.; Ollua Méndez, P.; Vega Valero, C.Z.; Soria Trujano, R. Inventory of strategies of coping: A replication. Psicol. Salud 2010, 20, 213–220. [Google Scholar]
- Thoits, P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [PubMed]
- Wills, T.A.; Ainette, M.G. Social support and health. In Cambridge Handbook of Psychology, Health and Medicine, 2nd ed.; Cambridge University Press: Cambridge, UK, 2014; ISBN 9780511543579. [Google Scholar]
- Skinner, E.A.; Edge, K.; Altman, J.; Sherwood, H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol. Bull. 2003, 129, 216–269. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Connor-Smith, J. Personality and coping. Annu. Rev. Psychol. 2010, 61, 679–704. [Google Scholar] [CrossRef] [PubMed]
- Dashora, P.; Erdem, G.; Slesnick, N. Better to bend than to break: Coping strategies utilized by substance-abusing homeless youth. J. Health Psychol. 2011, 16, 158–168. [Google Scholar] [CrossRef]
- Scott, R.M.; Hides, L.; Allen, J.S.; Lubman, D.I. Coping style and ecstasy use motives as predictors of current mood symptoms in ecstasy users. Addict. Behav. 2013, 38, 2465–2472. [Google Scholar] [CrossRef]
- Kiluk, B.D.; Nich, C.; Carroll, K.M. Relationship of cognitive function and the acquisition of coping skills in computer assisted treatment for substance use disorders. Drug Alcohol Depend. 2011, 114, 169–176. [Google Scholar] [CrossRef]
- Blevins, C.E.; Stephens, R.S.; Walker, D.D.; Roffman, R. Situational determinants of use and treatment outcomes in marijuana dependent adults. Addict. Behav. 2014, 39, 546–552. [Google Scholar] [CrossRef]
- Gillen, C.T.A.; Barry, C.T.; Bater, L.R. Anxiety symptoms and coping motives: Examining a potential path to substance use-related problems in adolescents with psychopathic traits. Subst. Use Misuse 2016, 51, 1920–1929. [Google Scholar] [CrossRef]
- Forys, K.; McKellar, J.; Moos, R. Participation in specific treatment components predicts alcohol-specific and general coping skills. Addict. Behav. 2007, 32, 1669–1680. [Google Scholar] [CrossRef]
- De Mar Capella, M.; Adan, A. The age of onset of substance use is related to the coping strategies to deal with treatment in men with substance use disorder. PeerJ 2017, 5, e366. [Google Scholar]
- Monras, M.; Mondon, S.; Jou, J. Estrategias de afrontamiento en enfermos alcohólicos. Diferencias según el consumo de benzodiacepinas, los trastornos de la personalidad y el deterioro cognitivo. Adicciones 2010, 22, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Stappenbeck, C.A.; Luterek, J.A.; Kaysen, D.; Rosenthal, C.F.; Gurrad, B.; Simpson, T.L. A controlled examination of two coping skills for daily alcohol use and PTSD symptom severity among dually diagnosed individuals. Behav. Res. Ther. 2015, 66, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Coriale, G.; Bilotta, E.; Leone, L.; Cosimi, F.; Porrari, R.; De Rosa, F.; Ceccanti, M. Avoidance coping strategies, alexithymia and alcohol abuse: A mediation analysis. Addict. Behav. 2012, 37, 1224–12249. [Google Scholar] [CrossRef]
- Boden, M.T.; Moos, R. Dually diagnosed patients’ responses to substance use disorder treatment. J. Subst. Abus. Treat. 2009, 37, 335–345. [Google Scholar] [CrossRef]
- Mueser, K.T.; Gingerich, S. Treatment of co-occurring psychotic and substance use disorders. Soc. Work Public Health 2013, 28, 424–439. [Google Scholar] [CrossRef]
- Jiménez-Castro, L.; Raventós-Vorst, H.; Escamilla, M. Substance use disorder and schizophrenia: Prevalence and sociodemographic characteristics in the latin american population. Actas Españolas Psiquiatr. 2011, 39, 123–130. [Google Scholar]
- Lev-Ran, S.; Imtiaz, S.; Rehm, J.; Le Foll, B. Exploring the association between lifetime prevalence of mental illness and transition from substance use to substance use disorders: Results from the national epidemiologic survey of alcohol and related conditions (NESARC). Am. J. Addict. 2013, 22, 93–98. [Google Scholar] [CrossRef]
- Timko, C.; Cronkite, R.C.; McKellar, J.; Zemore, S.; Moos, R.H. Dually diagnosed patients’ benefits of mutual-help groups and the role of social anxiety. J. Subst. Abus. Treat. 2013, 44, 216–233. [Google Scholar] [CrossRef]
- Di Lorenzo, R.; Galliani, A.; Guicciardi, A.; Landi, G.; Ferri, P. A retrospective analysis focusing on a group of patients with dual diagnosis treated by both mental health and substance use services. Neuropsychiatr. Dis. Treat. 2014, 10, 1479–1488. [Google Scholar] [CrossRef]
- Magidson, J.F.; Wang, S.; Lejuez, C.W.; Iza, M.; Blanco, C. Prospective study of substance-induced and independent major depressive disorder among individuals with substance use disorders in a nationally representative sample. Depress. Anxiety 2013, 30, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Drake, R.E.; McHugo, G.J.; Xie, L.; Mohandas, A. The 10-year course of remission, abstinence, and recovery in dual diagnosis. J. Subst. Abus. Treat. 2010, 39, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Hunt, G.E.; Large, M.M.; Cleary, M.; Lai, H.M.X.; Saunders, J.B. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Depend. 2018, 191, 234–258. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Capella, M.D.M.; Prat, G.; Forero, D.A.; Lopez-Vera, S.; Navarro, J.F. Executive functioning in men with schizophrenia and substance use disorders. Influence of lifetime suicide attempts. PLoS ONE 2017, 12, e0169943. [Google Scholar] [CrossRef]
- Daigre, C.; Perea-Ortueta, M.; Berenguer, M.; Esculies, O.; Sorribes-Puertas, M.; Palma-Alvarez, R.; Martínez-Luna, N.; Ramos-Quiroga, J.A.; Grau-López, L. Psychiatric factors affecting recovery after a long term treatment program for substance use disorder. Psychiatry Res. 2019, 276, 283–289. [Google Scholar] [CrossRef]
- Marquez-Arrico, J.E.; Benaiges, I.; Adan, A. Strategies to cope with treatment in substance use disorder male patients with and without schizophrenia. Psychiatry Res. 2015, 228, 752–759. [Google Scholar] [CrossRef]
- Lai, H.M.X.; Cleary, M.; Sitharthan, T.; Hunt, G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 154, 1–13. [Google Scholar] [CrossRef]
- Thornton, L.K.; Baker, A.L.; Lewin, T.J.; Kay-Lambkin, F.J.; Kavanagh, D.; Richmond, R.; Kelly, B.; Johnson, M.P. Reasons for substance use among people with mental disorders. Addict. Behav. 2012, 37, 427–434. [Google Scholar] [CrossRef]
- Pollack, L.E.; Cramer, R.D.; Varner, R.V. Psychosocial functioning of people with substance abuse and bipolar disorders. Subst. Abus. 2000, 21, 193–203. [Google Scholar] [CrossRef]
- Adan, A.; Antúnez, J.M.; Navarro, J.F. Coping strategies related to treatment in substance use disorder patients with and without comorbid depression. Psychiatry Res. 2017, 251, 325–332. [Google Scholar] [CrossRef]
- Bergman, B.G.; Greene, M.C.; Slaymaker, V.; Hoeppner, B.B.; Kelly, J.F. Young adults with co-occurring disorders: Substance use disorder treatment response and outcomes. J. Subst. Abus. Treat. 2014, 46, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, G.; Weldon, S.; Freeman, L.; Macpherson, G.; Davies, K. Outcomes of a drug and alcohol relapse prevention programme in a population of mentally disordered offenders. Br. J. Forensic Pract. 2011, 13, 32–43. [Google Scholar] [CrossRef]
- Cooke, M.; Peters, E.; Fannon, D.; Anilkumar, A.P.P.; Aasen, I.; Kuipers, E.; Kumari, V. Insight, distress and coping styles in schizophrenia. Schizophr. Res. 2007, 94, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Rohsenow, D.J.; Monti, P.M.; Martin, R.A.; Colby, S.M.; Myers, M.G.; Gulliver, S.B.; Brown, R.A.; Mueller, T.I.; Gordon, A.; Abrams, D.B. Motivational enhancement and coping skills training for cocaine abusers: Effects on substance use outcomes. Addiction 2004, 99, 862–874. [Google Scholar] [CrossRef]
- Bergly, T.H.; Grawe, R.W.; Hagen, R. Domains and perceived benefits of treatment among patients with and without co-occurring disorders in inpatient substance use treatment. J. Dual Diagn. 2014, 10, 91–97. [Google Scholar] [CrossRef]
- Bradizza, C.M.; Stasiewicz, P.R.; Dermen, K.H. Behavioral interventions for individuals dually diagnosed with a severe mental illness and a substance use disorder. Curr. Addict. Rep. 2014, 1, 243–250. [Google Scholar] [CrossRef]
- Torrents, O.; Mora, A.; Massana, L.; Robert, A.; Tejero, A. Resultados de efectividad de un grupo de estrategias de afrontamiento para pacientes dependientes de sustancias en el contexto de un hospital de día. Trastor. Adict. 2011, 13, 135–143. [Google Scholar] [CrossRef]
- Melemis, S.M. Relapse prevention and the five rules of recovery. Yale J. Biol. Med. 2015, 88, 325–332. [Google Scholar]
- Tirado-Muñoz, J.; Farré, A.; Mestre-Pintó, J.; Torrens, M.; Szerman, N. Dual diagnosis in depression: Treatment recommendations. Adicciones 2018, 30, 66–76. [Google Scholar]
- Worley, J. Recovery in substance use disorders: What to know to inform practice. Issues Ment. Health Nurs. 2017, 38, 80–91. [Google Scholar] [CrossRef]
- Grant, B.F.; Saha, T.D.; Ruan, W.J.; Goldstein, R.B.; Chou, S.P.; Jung, J.; Zhang, H.; Smith, S.M.; Pickering, R.P.; Huang, B.; et al. Epidemiology of DSM-5 drug use disorder: Results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry 2016, 73, 39–47. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Gibbon, M. The structured clinical interview for DSM-IV axis I disorders (SCID-I) and the structured clinical interview for DSM-IV axis II disorders (SCID-II). In Comprehensive Handbook of Psychological Assessment, Vol. 2: Personality Assessment; John Wiley & Sons: Hoboken, NJ, USA, 2004; pp. 134–143. ISBN 0-471-41612-6. [Google Scholar]
- Skinner, H.A. The drug abuse screening test. Addict. Behav. 1982, 7, 363–371. [Google Scholar] [CrossRef]
- Peralta, V.; Cuesta, M.J. Validación de la escala de los síndromes positivo y negativo (PANSS) en una muestra de esquizofrénicos españoles. Actas Luso Esp. Neurol. Psiquiatr. Cienc. Afines 1994, 22, 171–177. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Rush, A.J.J.; First, M.B.; Blacker, D. (Eds.) Handbook of Psychiatric Measures, 2nd ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 2008. [Google Scholar]
- Tobin, D.; Holroyd, K.A.; Reynolds, R.V.; Kigal, J.K. The hierarchical factor structure of the coping strategies inventory. Cogn. Ther. Res. 1989, 4, 343–361. [Google Scholar] [CrossRef]
- Cano García, F.J.; Rodríguez Franco, L.; García Martínez, J. Spanish version of the coping strategies inventory. Actas Esp. Psiquiatr. 2007, 35, 29–39. [Google Scholar]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Poudel, A.; Gautam, S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatry 2017, 17, 10. [Google Scholar] [CrossRef]
- Chen, L.; Selvendra, A.; Stewart, A.; Castle, D. Risk factors in early and late onset schizophrenia. Compr. Psychiatry 2018, 80, 155–162. [Google Scholar] [CrossRef]
- Barrowclough, C.; Gregg, L.; Lobban, F.; Bucci, S.; Emsley, R. The impact of cannabis use on clinical outcomes in recent onset psychosis. Schizophr. Bull. 2014, 41, 382–390. [Google Scholar] [CrossRef]
- Park, S.C.; Hahn, S.W.; Hwang, T.Y.; Kim, J.M.; Jun, T.Y.; Lee, M.S.; Kim, J.B.; Yim, H.W.; Park, Y.C. Does age at onset of first major depressive episode indicate the subtype of major depressive disorder?: The clinical research center for depression study. Yonsei Med. J. 2014, 55, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Szerman, N.; Vega, P.; Grau-López, L.; Barral, C.; Basurte-Villamor, I.; Mesías, B.; Rodríguez-Cintas, L.; Martínez-Raga, J.; Casas, M.; Roncero, C. Dual diagnosis resource needs in Spain: A national survey of professionals. J. Dual Diagn. 2014, 10, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Szerman, N.; Peris, L. Precision psychiatry and dual disorders. J. Dual Diagn. 2018, 14, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Navrady, L.B.; Zeng, Y.; Clarke, T.-K.; Adams, M.J.; Howard, D.M.; Deary, I.J.; McIntosh, A.M. Genetic and environmental contributions to psychological resilience and coping. Wellcome Open Res. 2018, 3, 12. [Google Scholar] [CrossRef]
- Choi, K.W.; Stein, M.B.; Dunn, E.C.; Koenen, K.C.; Smoller, J.W. Genomics and psychological resilience: A research agenda. Mol. Psychiatry 2019. [Google Scholar] [CrossRef]
| Sociodemographic Variables | DD (N = 80) | SUD (N = 80) | SMI (N = 63) | Statistical Analyses |
|---|---|---|---|---|
| Age | 38.71 ± 0.91 | 37.41 ± 0.89 | 41.90 ± 1.51 | F(2,221) = 5.768 * |
| Civil status | χ2(4) = 7.754 ** | |||
| Single | 71.25% | 52.20% | 75.40% | |
| Married/Stable partner | 8.70% | 20.30% | 7.50% | |
| Divorced/Separated | 20.05% | 27.50% | 17.10% | |
| Living arrangements | χ2(4) = 11.643 ** | |||
| Alone | 22.60% | 25.50% | 8.10% | |
| With family/partner/parents | 58.10% | 47.30% | 51.40% | |
| With friends/protected flats | 19.40% | 27.20% | 40.50% | |
| Employment situation | χ2(4) = 19.388 ** | |||
| Working | 17.40% | 45.10% | 22.10% | |
| Unemployed | 21.30% | 35.50% | 12.90% | |
| Disability pension | 61.30% | 19.40% | 65.00% | |
| Education | χ2(4) = 3.286 | |||
| Primary | 56.60% | 45.80% | 51.20% | |
| Secondary | 26.30% | 34.70% | 35.90% | |
| University | 17.1% | 19.50% | 12.90% | |
| Clinical Variables | DD (N = 80) | SUD (N = 80) | SMI (N = 63) | Statistical Analyses |
|---|---|---|---|---|
| Age of SUD onset | 15.72 ± 2.51 | 17.38 ± 5.80 | F(2,158) = 6.294 * | |
| Age of SMI onset | 24.22 ± 9.05 | 28 ± 10.78 | F(2,121) = 5.976 * | |
| Duration of SUD (years) | 20.62 ± 8.11 | 22.16 ± 8.15 | F(2,158) = 1.317 | |
| Duration of SMI (years) | 15.64 ± 6.34 | 13.45 ± 3.49 | F(2,121) = 1.745 | |
| Medical disease comorbidity a | 44% | 25% | 43% | χ2(2) = 8.011 * |
| Respiratory | 16% | 15% | 22% | |
| Metabolic | 28% | 16% | 38% | |
| Infectious | 12% | 28% | 8% | |
| Other | 44% | 41% | 32% | |
| Main substance of dependence | χ2(2) = 4.483 | |||
| Alcohol | 33.8% | 25% | ||
| Cannabis | 18.8% | 11.3% | ||
| Cocaine | 43.8% | 61.3% | ||
| Opioids | 3.8% | 2.5% | ||
| Polydrug use | 56% | 50% | χ2(2) = 2.115 | |
| Abstinence period (months) | 7.48 ± 2.74 | 8.29 ± 2.70 | F(2,158) = 0.219 | |
| DAST-20 (severity of addiction) | 13.04 ± 1.15 | 12.30 ± 2.46 | F(2,158) = 1.061 | |
| Suicide attempts | 0.81 ± 1.52 | 0.74 ± 1.09 | 0.81 ± 1.33 | F(2,221) = 0.096 |
| Daily use of psychiatric medication | 96.8% | 51.7% | 100% | χ2(2) = 39.108 ** |
| PANSS scores (for Schizophrenia diagnosis) | ||||
| Positive symptoms | 8.95 ± 0.64 | 10.22 ± 0.73 | F(2,121) = 0.899 | |
| Negative symptoms | 13.83 ± 1.65 | 12.15 ± 1.87 | F(2,121) = 1.210 | |
| Composite | −5.63 ± 1.40 | −7.73 ± 1.81 | F(2,121) = 6.420 * | |
| General psychopathology | 24.18 ± 2.01 | 22.00 ± 1.82 | F(2,121) = 1.966 | |
| HDRS scores (for Major Depressive Disorder diagnosis) | 9.25 ± 0.18 | 8.02 ± 1.05 | F(2,121) = 0.688 |
| Coping Strategies Inventory | DD (N = 80) | SUD (N = 80) | SMI (N = 63) | F(2,121) | ηp2 | Bonferroni Post-Hoc Analyses |
|---|---|---|---|---|---|---|
| Problem Solving | 12.99 ± 0.59 | 12.98 ± 0.58 | 13.98 ± 0.58 | 0.23 | 0.002 | |
| Self-criticism | 13.33 ± 0.55 | 14.28 ± 0.55 | 10.46 ± 0.56 | 10.75 *** | 0.089 | DD, SUD > SMI |
| Express Emotions | 10.80 ± 0.63 | 10.25 ± 0.63 | 11.09 ± 0.73 | 0.40 | 0.004 | |
| Wishful Thinking | 15.84 ± 0.47 | 15.51 ± 0.47 | 15.35 ± 0.58 | 0.24 | 0.002 | |
| Social Support | 11.07 ± 0.61 | 11.29 ± 0.60 | 11.25 ± 0.69 | 0.23 | 0.000 | |
| Cognitive Restructuring | 10.39 ± 0.57 | 10.09 ± 0.58 | 11.37 ± 0.66 | 1.20 | 0.010 | |
| Problem Avoidance | 6.68 ± 0.55 | 6.68 ± 0.56 | 10.36 ± 0.63 | 14.12 *** | 0.114 | DD, SUD < SMI |
| Social Withdrawal | 11.68 ± 0.56 | 10.55 ± 0.57 | 11.68 ± 0.64 | 0.88 | 0.008 |
| Follow-Up Data | DD (N = 80) | SUD (N = 80) | SMI (N = 63) | Inter-Group Statistical Analyses (ANOVA or Chi-Square) | ||||
|---|---|---|---|---|---|---|---|---|
| 3 months | DD with Schizophrenia (N = 37) | DD with Depression (N = 43) | SMI with Schizophrenia (N = 32) | SMI with Depression (N = 31) | ||||
| Relapses | 28.8% | 27% | 30.2% | 21.3% | 11.1% | 6.3% | 16.1% | χ2(2) = 6.71 * |
| Patients’ treatment situation | χ2(2) = 5.22 | |||||||
| In treatment | 98.8% | 97.3% | 100% | 97.3% | 100% | 100% | 100% | |
| Drop-out from treatment | 1.3% | 2.7% | 0% | 1.4% | 0% | 0% | 0% | |
| Discharged from treatment | 0% | 0% | 0% | 1.4% | 0% | 0% | 0% | |
| Dismissed from treatment | 0% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Suicide attempts | 5.1% | 8.1% | 2.3% | 2.7% | 0% | 0% | 0% | χ2(2) = 3.81 * |
| Number of medical consultations 1 | 7.6 ± 0.88 | 5.44 ± 1.22 | 9.42 ± 1.88 | 1.5 ± 0.51 | 4.3 ± 0.39 | 3.56 ± 0.48 | 4.90 ± 0.60 | F(2,221) = 22.44 *** |
| 6 months | ||||||||
| Relapses | 33.8% | 32.4% | 34.9% | 28.8% | 14.3% | 9.4% | 19.4% | χ2(2) = 9.70 ** |
| Patients’ treatment situation | χ2(2) = 8.22 * | |||||||
| In treatment | 91.3% | 89.2% | 93.3% | 73.6% | 98% | 95% | 100% | |
| Drop-out from treatment | 5% | 8.1% | 4.7% | 8.3% | 2% | 3.1% | 0% | |
| Discharged from treatment | 2.3% | 0% | 2% | 9.7% | 0% | 0% | 0% | |
| Dismissed from treatment | 1.4% | 2.7% | 0% | 4.2% | 0% | 1.9% | 0% | |
| Suicide attempts | 5.1% | 8.1% | 2.3% | 6.3% | 1.6% | 3.1% | 0% | χ2(2) = 3.20 * |
| Number of medical consultations 1 | 15.71 ± 2.12 | 12.46 ± 2.96 | 18.55 ± 3.01 | 2.5 ± 0.74 | 8.4 ± 0.77 | 7.06 ± 0.92 | 9.74 ± 1.21 | F(2,221) = 23.63 *** |
| 12 months | ||||||||
| Relapses | 48.8% | 43.2% | 53.5% | 38.8% | 23.8% | 21.9% | 25.8% | χ2(2) = 12.43 ** |
| Patients’ treatment situation | χ2(2) = 10.53 ** | |||||||
| In treatment | 87.2% | 80% | 93% | 41.4% | 80.5% | 89.6% | 90.4% | |
| Drop-out from treatment | 9% | 14.3% | 4.7% | 21.4% | 7.1% | 6.4% | 3.2% | |
| Discharged from treatment | 2.4% | 2.9% | 2.3% | 33% | 8.3% | 3% | 3.2% | |
| Dismissed from treatment | 1.4% | 2.8% | 0% | 4.2% | 4.1% | 1% | 3.2% | |
| Suicide attempts | 21.8% | 19.5% | 23.7% | 5% | 7.25% | 9.4% | 6.5% | χ2(2) = 7.88 ** |
| Number of medical consultations 1 | 28.12 ± 3.74 | 23.17 ± 5.60 | 31.92 ± 5.02 | 4.7 ± 0.92 | 15.97 ± 1.73 | 11.48 ± 1.20 | 20.45 ± 3.07 | F(2,221) = 19.894 *** |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marquez-Arrico, J.E.; Río-Martínez, L.; Navarro, J.F.; Prat, G.; Forero, D.A.; Adan, A. Coping Strategies in Male Patients under Treatment for Substance Use Disorders and/or Severe Mental Illness: Influence in Clinical Course at One-Year Follow-Up. J. Clin. Med. 2019, 8, 1972. https://doi.org/10.3390/jcm8111972
Marquez-Arrico JE, Río-Martínez L, Navarro JF, Prat G, Forero DA, Adan A. Coping Strategies in Male Patients under Treatment for Substance Use Disorders and/or Severe Mental Illness: Influence in Clinical Course at One-Year Follow-Up. Journal of Clinical Medicine. 2019; 8(11):1972. https://doi.org/10.3390/jcm8111972
Chicago/Turabian StyleMarquez-Arrico, Julia E., Laura Río-Martínez, José Francisco Navarro, Gemma Prat, Diego A. Forero, and Ana Adan. 2019. "Coping Strategies in Male Patients under Treatment for Substance Use Disorders and/or Severe Mental Illness: Influence in Clinical Course at One-Year Follow-Up" Journal of Clinical Medicine 8, no. 11: 1972. https://doi.org/10.3390/jcm8111972
APA StyleMarquez-Arrico, J. E., Río-Martínez, L., Navarro, J. F., Prat, G., Forero, D. A., & Adan, A. (2019). Coping Strategies in Male Patients under Treatment for Substance Use Disorders and/or Severe Mental Illness: Influence in Clinical Course at One-Year Follow-Up. Journal of Clinical Medicine, 8(11), 1972. https://doi.org/10.3390/jcm8111972






