Medical Cannabis for Older Patients—Treatment Protocol and Initial Results
Abstract
1. Introduction
1.1. Efficacy and Indications for Medical Cannabis in Older Adults
1.2. Chronic Pain
1.3. Parkinson’s Disease
1.4. Sleep Difficulties
1.5. Nausea and Vomiting
1.6. Post-Traumatic Stress Disorder (PTSD)
1.7. Dementia
1.8. Palliative Treatment
2. Special Considerations and Precautions
2.1. Pharmacokinetics, Pharmacodynamics, and Drug Interactions
2.2. Nervous System Impairment
2.3. Cardiovascular Risks
3. Methods
3.1. Patients and Methods
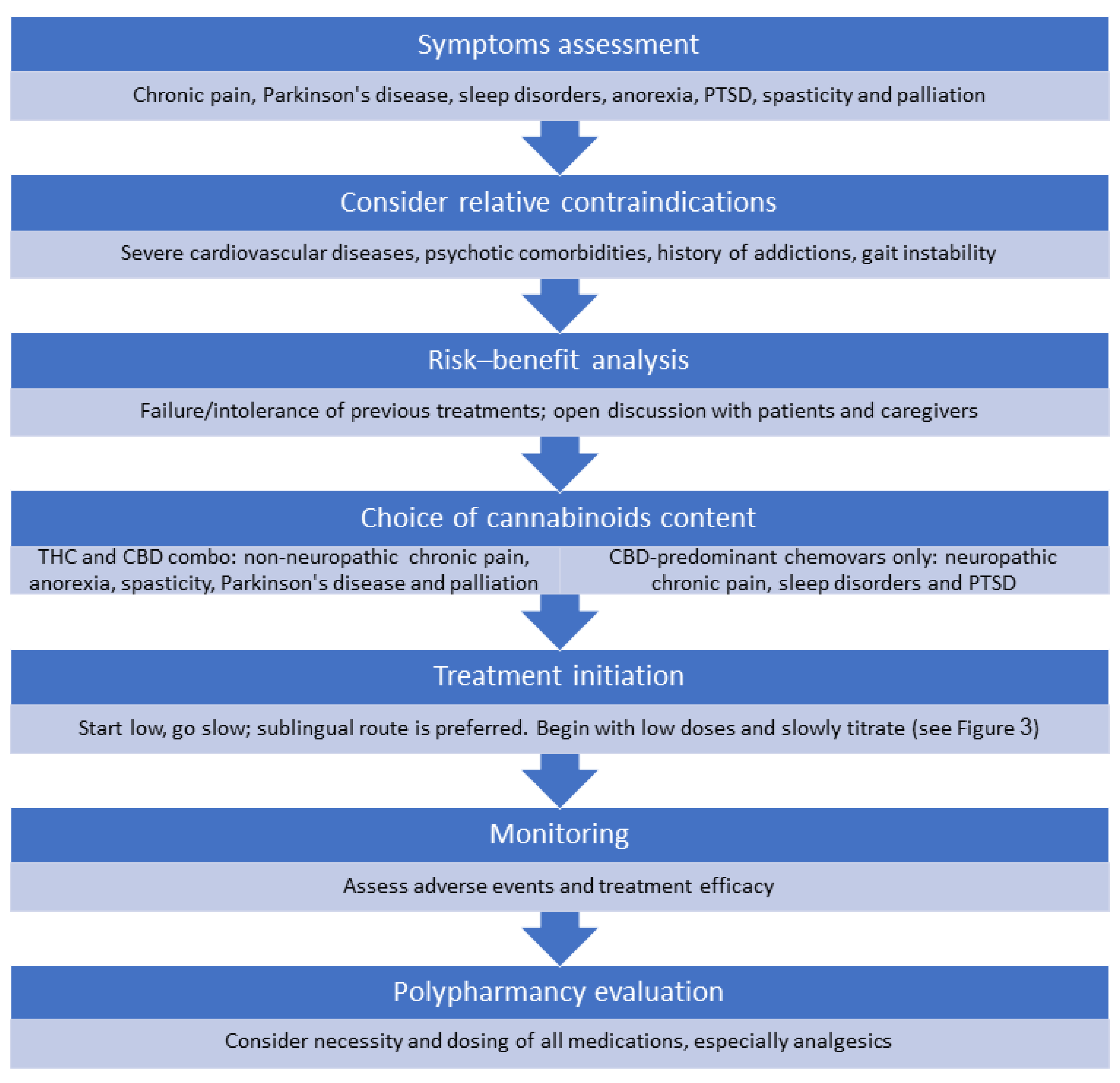
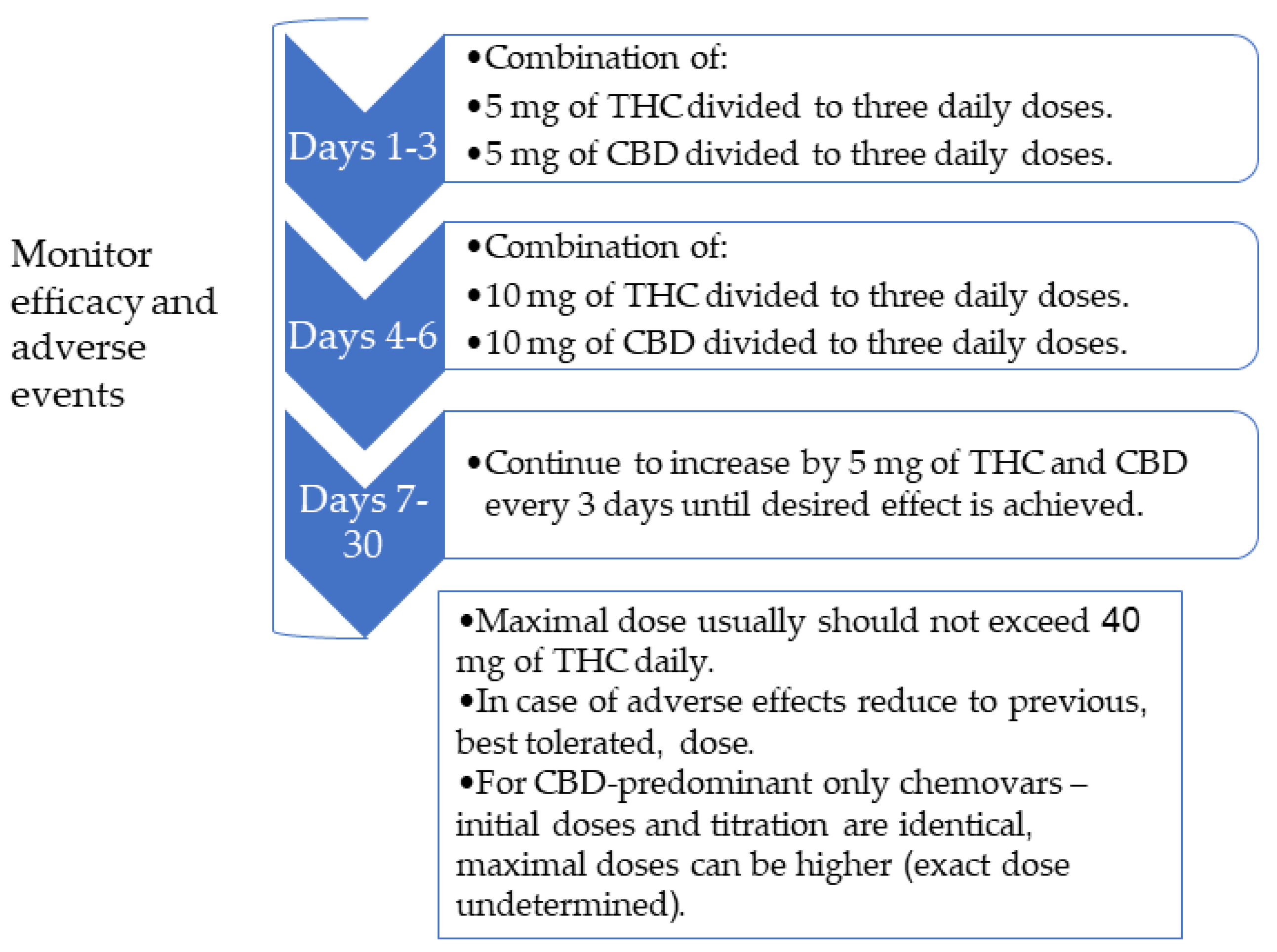
3.2. The Treatment Protocol
3.3. Ethics
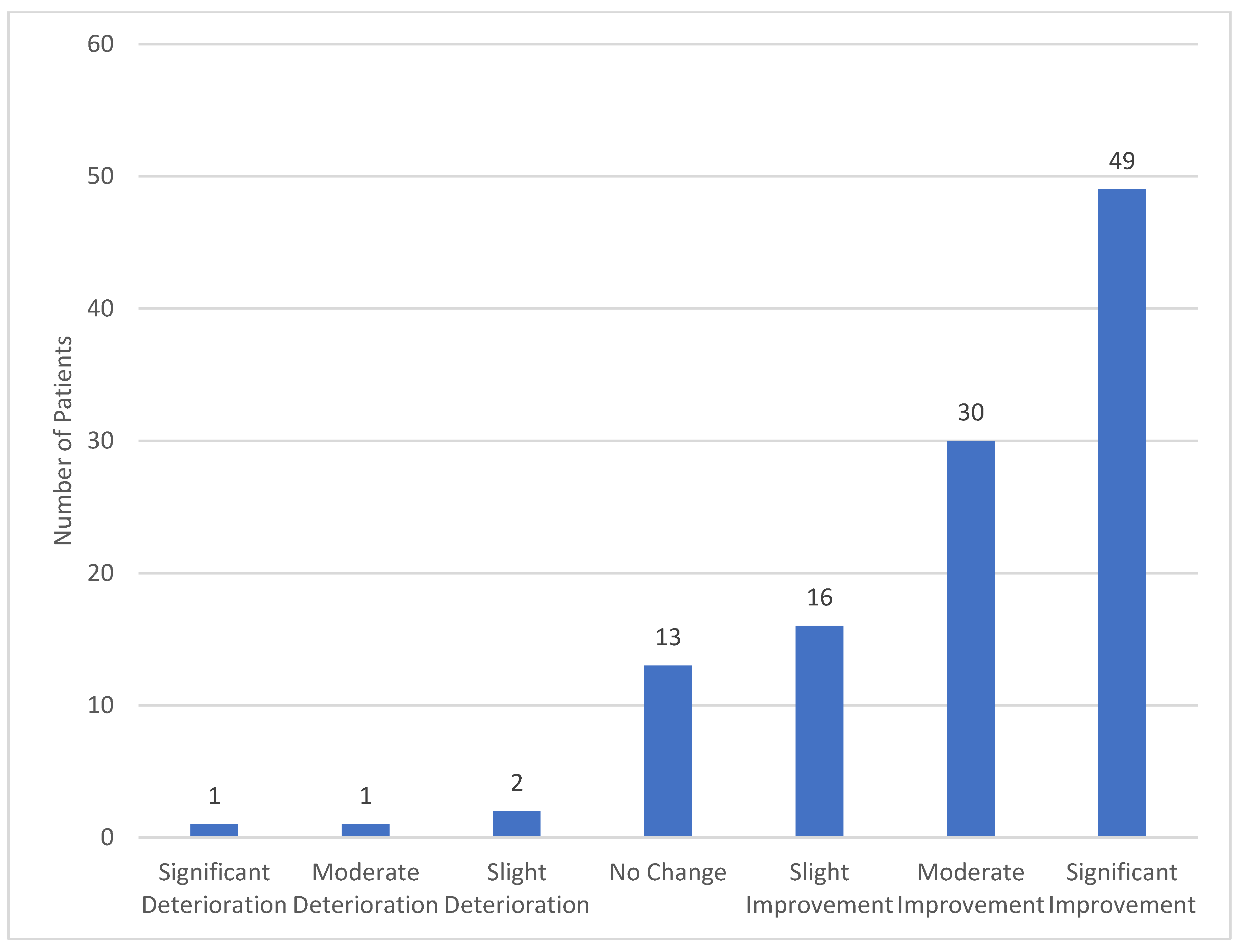
4. Results
5. Discussion
5.1. Patient Selection
5.2. Selection of The Compound
5.3. Selection of The Delivery Method
5.4. Addressing Patients Concerns
5.5. Follow-Up
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Abuhasira, R.; Shbiro, L.; Landschaft, Y. Medical use of cannabis and cannabinoids containing products—Regulations in Europe and North America. Eur. J. Intern. Med. 2018, 49, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Schleider, L.B.-L.; Abuhasira, R.; Novack, V. Medical cannabis: Aligning use to evidence-based medicine approach. Br. J. Clin. Pharmacol. 2018, 84, 2458–2462. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, I.R.; Fixen, D.R.; Parnes, B.L.; Lum, H.D.; Shanbhag, P.; Church, S.; Linnebur, S.A.; Orosz, G. Characteristics and Patterns of Marijuana Use in Community-Dwelling Older Adults. J. Am. Geriatr. Soc. 2018, 66, 2167–2171. [Google Scholar] [CrossRef] [PubMed]
- Kaskie, B.; Ayyagari, P.; Milavetz, G.; Shane, D.; Arora, K. The Increasing Use of Cannabis Among Older Americans: A Public Health Crisis or Viable Policy Alternative? Gerontologist 2017, 57, 1166–1172. [Google Scholar] [CrossRef]
- Hazekamp, A.; Ware, M.A.; Müller-Vahl, K.R.; Abrams, D.; Grotenhermen, F. The Medicinal Use of Cannabis and Cannabinoids—An International Cross-Sectional Survey on Administration Forms. J. Psychoact. Drugs 2013, 45, 199–210. [Google Scholar] [CrossRef]
- Han, B.H.; Sherman, S.; Mauro, P.M.; Martins, S.S.; Rotenberg, J.; Palamar, J.J. Demographic trends among older cannabis users in the United States, 2006–2013. Addiction 2017, 112, 516–525. [Google Scholar] [CrossRef]
- Molton, I.R.; Terrill, A.L. Overview of persistent pain in older adults. Am. Psychol. 2014, 69, 197–207. [Google Scholar] [CrossRef]
- Pringsheim, T.; Jette, N.; Frolkis, A.; Steeves, T.D.L. The prevalence of Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1583–1590. [Google Scholar] [CrossRef]
- Steffens, D.C. Prevalence of Depression and Its Treatment in an Elderly Population: The Cache County Study. Arch. Gen. Psychiatry 2000, 57, 601–607. [Google Scholar] [CrossRef]
- Jongenelis, K.; Pot, A.; Eisses, A.; Beekman, A.; Kluiter, H.; Ribbe, M. Prevalence and risk indicators of depression in elderly nursing home patients: The AGED study. J. Affect. Disord. 2004, 83, 135–142. [Google Scholar] [CrossRef]
- Saccomano, S.J. Sleep disorders in older adults. J. Gerontol. Nurs. 2014, 40, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.K.; Hanlon, J.T.; Marcum, Z.A. Adverse effects of analgesics commonly used by older adults with osteoarthritis: Focus on non-opioid and opioid analgesics. Am. J. Geriatr. Pharmacother. 2012, 10, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Glass, J.; Lanctot, K.L.; Herrmann, N.; Sproule, B.A.; Busto, U.E. Sedative hypnotics in older people with insomnia: Meta-analysis of risks and benefits. BMJ 2005, 331, 1169. [Google Scholar] [CrossRef]
- Volkow, N.D.; Frieden, T.R.; Hyde, P.S.; Cha, S.S. Medication-Assisted Therapies—Tackling the Opioid-Overdose Epidemic. N. Engl. J. Med. 2014, 370, 2063–2066. [Google Scholar] [CrossRef]
- Elsen, G.V.D.; Ahmed, A.; Lammers, M.; Kramers, C.; Verkes, R.; Van Der Marck, M.; Rikkert, M.O. Efficacy and safety of medical cannabinoids in older subjects: A systematic review. Ageing Res. Rev. 2014, 14, 56–64. [Google Scholar] [CrossRef]
- Minerbi, A.; Häuser, W.; Fitzcharles, M.-A. Medical Cannabis for Older Patients. Drugs Aging 2018, 36, 39–51. [Google Scholar] [CrossRef]
- Briscoe, J.; Casarett, D. Medical Marijuana Use in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 859–863. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research; National Academies Press (US): Washington, DC, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK423845/ (accessed on 7 October 2019).
- Health Canada. Information for Health Care Professionals: Cannabis (Marihuana, Marijuana) and the Cannabinoids. 2018. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/medical-use-marijuana/information-medical-practitioners/information-health-care-professionals-cannabis-marihuana-marijuana-cannabinoids.html (accessed on 7 October 2019).
- Freeman, M.; Low, A.; Kondo, K.; Elven, C.; Zakher, B.; Motu’Apuaka, M.; Paynter, R.; Kansagara, D.; Nugent, S.M.; Morasco, B.J.; et al. The Effects of Cannabis among Adults with Chronic Pain and an Overview of General Harms. Ann. Intern. Med. 2017, 167, 319. [Google Scholar]
- Ware, M.A.; Wang, T.; Shapiro, S.; Collet, J.-P.; Boulanger, A.; Esdaile, J.M.; Gordon, A.; Lynch, M.; Moulin, D.E.; O’Connell, C. Cannabis for the Management of Pain: Assessment of Safety Study (COMPASS). J. Pain 2015, 16, 1233–1242. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef] [PubMed]
- Mahlknecht, P.; Seppi, K.; Poewe, W. The Concept of Prodromal Parkinson’s Disease. J. Park. Dis. 2015, 5, 681–697. [Google Scholar] [CrossRef] [PubMed]
- Carroll, C.B.; Bain, P.G.; Teare, L.; Liu, X.; Joint, C.; Wroath, C.; Parkin, S.G.; Fox, P.; Wright, D.; Hobart, J.; et al. Cannabis for dyskinesia in Parkinson disease: A randomized double-blind crossover study. Neurology 2004, 63, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Chagas, M.H.N.; Zuardi, A.W.; Tumas, V.; Pena-Pereira, M.A.; Sobreira, E.T.; Bergamaschi, M.M.; Dos Santos, A.C.; Teixeira, A.L.; Hallak, J.E.; Crippa, J.A.S. Effects of cannabidiol in the treatment of patients with Parkinson?s disease: An exploratory double-blind trial. J. Psychopharmacol. 2014, 28, 1088–1098. [Google Scholar] [CrossRef]
- Balash, Y.; Schleider, L.B.-L.; Korczyn, A.D.; Shabtai, H.; Knaani, J.; Rosenberg, A.; Baruch, Y.; Djaldetti, R.; Giladi, N.; Gurevich, T. Medical Cannabis in Parkinson Disease. Clin. Neuropharmacol. 2017, 40, 268–272. [Google Scholar] [CrossRef]
- Foley, D.J.; Monjan, A.A.; Brown, S.L.; Simonsick, E.M.; Wallace, R.B.; Blazer, D.G. Sleep Complaints Among Elderly Persons: An Epidemiologic Study of Three Communities. Sleep 1995, 18, 425–432. [Google Scholar] [CrossRef]
- Vitiello, M.V.; Moe, K.E.; Prinz, P.N. Sleep complaints cosegregate with illness in older adults: Clinical research informed by and informing epidemiological studies of sleep. J. Psychosom. Res. 2002, 53, 555–559. [Google Scholar] [CrossRef]
- Babson, K.A.; Sottile, J.; Morabito, D. Cannabis, Cannabinoids, and Sleep: A Review of the Literature. Curr. Psychiatry Rep. 2017, 19, 23. [Google Scholar] [CrossRef]
- Suzuki, K.; Miyamoto, M.; Hirata, K. Sleep disorders in the elderly: Diagnosis and management. J. Gen. Fam. Med. 2017, 18, 61–71. [Google Scholar] [CrossRef]
- Gates, P.J.; Albertella, L.; Copeland, J. The effects of cannabinoid administration on sleep: A systematic review of human studies. Sleep Med. Rev. 2014, 18, 477–487. [Google Scholar] [CrossRef]
- Smith, L.A.; Azariah, F.; Lavender, V.T.; Stoner, N.S.; Bettiol, S. Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.M.; Shamliyan, T.A. Cannabinoids in Patients with Nausea and Vomiting Associated with Malignancy and Its Treatments. Am. J. Med. 2018, 131, 755–759. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Andrysiak, T.; Fairbanks, L.; Goodnight, J.; Sarna, G.; Jamison, K. Cannabis and cancer chemotherapy. A comparison of oral delta-9-thc and prochlorperazine. Cancer 1982, 50, 636–645. [Google Scholar] [CrossRef]
- Ferri, C.P.; Prince, M.; Brayne, C.; Brodaty, H.; Fratiglioni, L.; Ganguli, M.; Hall, K.; Hasegawa, K.; Hendrie, H.; Huang, Y.; et al. Global prevalence of dementia: A Delphi consensus study. Lancet 2005, 366, 2112–2117. [Google Scholar] [CrossRef]
- Volicer, L.; Stelly, M.; Morris, J.; McLaughlin, J.; Volicer, B.J. Effects of dronabinol on anorexia and disturbed behavior in patients with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 1997, 12, 913–919. [Google Scholar] [CrossRef]
- Woodward, M.R.; Harper, D.G.; Stolyar, A.; Forester, B.P.; Ellison, J.M. Dronabinol for the Treatment of Agitation and Aggressive Behavior in Acutely Hospitalized Severely Demented Patients with Noncognitive Behavioral Symptoms. Am. J. Geriatr. Psychiatry 2014, 22, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Walther, S.; Schüpbach, B.; Seifritz, E.; Homan, P.; Strik, W. Randomized, Controlled Crossover Trial of Dronabinol, 2.5 mg, for Agitation in 2 Patients with Dementia. J. Clin. Psychopharmacol. 2011, 31, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Elsen, G.A.V.D.; Ahmed, A.I.; Verkes, R.-J.; Kramers, C.; Feuth, T.; Rosenberg, P.B.; Van Der Marck, M.A.; Rikkert, M.G.O. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: A randomized controlled trial. Neurology 2015, 84, 2338–2346. [Google Scholar] [CrossRef]
- Mücke, M.; Weier, M.; Carter, C.; Copeland, J.; Degenhardt, L.; Cuhls, H.; Radbruch, L.; Häuser, W.; Conrad, R. Systematic review and meta-analysis of cannabinoids in palliative medicine. J. Cachexia Sarcopenia Muscle 2018, 9, 220–234. [Google Scholar] [CrossRef]
- Mangoni, A.A.; Jackson, S.H.D. Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br. J. Clin. Pharmacol. 2003, 57, 6–14. [Google Scholar] [CrossRef]
- Ahmed, A.I.; Elsen, G.A.V.D.; Colbers, A.; Van Der Marck, M.A.; Burger, D.M.; Feuth, T.B.; Rikkert, M.G.O.; Kramers, C. Safety and pharmacokinetics of oral delta-9-tetrahydrocannabinol in healthy older subjects: A randomized controlled trial. Eur. Neuropsychopharmacol. 2014, 24, 1475–1482. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.I.A.; Elsen, G.A.H.V.D.; Colbers, A.; Kramers, C.; Burger, D.M.; Van Der Marck, M.A.; Rikkert, M.G.M.O. Safety, pharmacodynamics, and pharmacokinetics of multiple oral doses of delta-9-tetrahydrocannabinol in older persons with dementia. Psychopharmacology 2015, 232, 2587–2595. [Google Scholar] [CrossRef] [PubMed]
- Alsherbiny, M.A.; Li, C.G. Medicinal Cannabis—Potential Drug Interactions. Medicines 2018, 6, 3. [Google Scholar] [CrossRef] [PubMed]
- Stout, S.M.; Cimino, N.M. Exogenous cannabinoids as substrates, inhibitors, and inducers of human drug metabolizing enzymes: A systematic review. Drug Metab. Rev. 2014, 46, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Mahvan, T.D.; Hilaire, M.L.; Mann, A.; Brown, A.; Linn, B.; Gardner, T.; Lai, B. Marijuana Use in the Elderly: Implications and Considerations. Consult. Pharm. 2017, 32, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Singh-Manoux, A.; Kivimaki, M.; Glymour, M.M.; Elbaz, A.; Berr, C.; Ebmeier, K.P.; Ferrie, J.E.; Dugravot, A. Timing of onset of cognitive decline: Results from Whitehall II prospective cohort study. BMJ 2012, 344, d7622. [Google Scholar] [CrossRef]
- Ganzer, F.; Bröning, S.; Kraft, S.; Sack, P.-M.; Thomasius, R. Weighing the Evidence: A Systematic Review on Long-Term Neurocognitive Effects of Cannabis Use in Abstinent Adolescents and Adults. Neuropsychol. Rev. 2016, 26, 186–222. [Google Scholar] [CrossRef]
- Schreiner, A.M.; Dunn, M.E. Residual effects of cannabis use on neurocognitive performance after prolonged abstinence: A meta-analysis. Exp. Clin. Psychopharmacol. 2012, 20, 420–429. [Google Scholar] [CrossRef]
- Rezkalla, S.; Stankowski, R.; Kloner, R.A. Cardiovascular effects of marijuana. Trends Cardiovasc. Med. 2018, 21, 452–455. [Google Scholar]
- Ponto, L.L.B.; O’Leary, D.S.; Koeppel, J.; Block, R.I.; Watkins, G.L.; Richmond, J.C.W.; Ward, C.A.; Clermont, D.A.; Schmitt, B.A.; Hichwa, R.D. Effect of Acute Marijuana on Cardiovascular Function and Central Nervous System Pharmacokinetics of [15O] Water: Effect in Occasional and Chronic Users. J. Clin. Pharmacol. 2004, 44, 751–766. [Google Scholar] [CrossRef]
- Abuhasira, R.; Schleider, L.B.-L.; Mechoulam, R.; Novack, V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur. J. Intern. Med. 2018, 49, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Maccallum, C.A.; Russo, E.B. Practical considerations in medical cannabis administration and dosing. Eur. J. Intern. Med. 2018, 49, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Arora, K.; Qualls, S.H.; Bobitt, J.; Lum, H.D.; Milavetz, G.; Croker, J.; Kaskie, B. Measuring Attitudes Toward Medical and Recreational Cannabis Among Older Adults in Colorado. Gerontologist 2019. [Google Scholar] [CrossRef] [PubMed]
- Bargnes, V.; Hart, P.; Gupta, S.; Mechtler, L. Safety and Efficacy of Medical Cannabis in Elderly Patients: A Retrospective Review in a Neurological Outpatient Setting. (P4.1-014); On behalf of the American Academy of Neurology; Wolters Kluwer Health, Inc.: Philadelphiaon, PA, USA, 2019; Volume 92. [Google Scholar]
- Hazekamp, A.; Fischedick, J.T. Cannabis—From cultivar to chemovar. Drug Test. Anal. 2012, 4, 660–667. [Google Scholar] [CrossRef]
- Russo, E.B. Taming THC: Potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br. J. Pharmacol. 2011, 163, 1344–1364. [Google Scholar] [CrossRef]
- Ribeiro, L.I.; Ind, P.W. Effect of cannabis smoking on lung function and respiratory symptoms: A structured literature review. NPJ Prim. Care Respir. Med. 2016, 26, 16071. [Google Scholar] [CrossRef]
- Karschner, E.L.; Darwin, W.D.; Goodwin, R.S.; Wright, S.; Huestis, M.A. Plasma cannabinoid pharmacokinetics following controlled oral Δ 9-tetrahydrocannabinol and oromucosal cannabis extract administration. Clin. Chem. 2011, 57, 66–75. [Google Scholar] [CrossRef]
- Lucas, C.J.; Galettis, P.; Schneider, J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br. J. Clin. Pharmacol. 2018, 84, 2477–2482. [Google Scholar] [CrossRef]
- Grotenhermen, F. Pharmacokinetics and Pharmacodynamics of Cannabinoids. Clin. Pharmacokinet. 2003, 42, 327–360. [Google Scholar] [CrossRef]
- Huestis, M.A. Human cannabinoid pharmacokinetics. Chem. Biodivers. 2007, 4, 1770–1804. [Google Scholar] [CrossRef] [PubMed]
| Variable | Number of Patients (n = 184) |
|---|---|
| Demographic characteristics | |
| Age (years) | 65–74–31 (16.8%) |
| 75–84–91 (49.5%) | |
| ≥85–62 (33.7%) | |
| Female | 117 (63.6%) |
| Family status | Married–64 (34.8%) |
| Widowed–42 (22.8%) | |
| Divorced–7 (3.8%) | |
| Unknown–71 (38.6%) | |
| Comorbidities (n, %) | |
| Hypertension | 51 (27.7%) |
| Dyslipidemia | 30 (16.3%) |
| Diabetes Mellitus | 25 (13.6%) |
| Hypothyroidism | 19 (10.3%) |
| Osteoporosis | 17 (9.2%) |
| Spinal Stenosis | 12 (6.5%) |
| Obesity | 10 (5.4%) |
| Stroke or transient ischemic attack history | 9 (4.9%) |
| Ischemic heart disease | 9 (4.9%) |
| Atrial fibrillation | 9 (4.9%) |
| Parkinson’s disease | 8 (4.3%) |
| Malignancy (different types) | 7 (3.8%) |
| Depression | 7 (3.8%) |
| Dementia | 6 (3.3%) |
| Cannabis treatment indications (n, %) | |
| Non-specific chronic pain (including neuropathic pain) | 105 (57.1%) |
| Parkinson’s disease | 12 (6.5%) |
| Orthopedic pain | 10 (5.4%) |
| Oncologic treatment | 7 (3.8%) |
| Dementia | 5 (2.7%) |
| Arthritis | 5 (2.7%) |
| Restlessness | 3 (1.6%) |
| Fibromyalgia | 2 (1.1%) |
| Palliative treatment | 2 (1.1%) |
| Others | 33 (17.9%) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abuhasira, R.; Ron, A.; Sikorin, I.; Novack, V. Medical Cannabis for Older Patients—Treatment Protocol and Initial Results. J. Clin. Med. 2019, 8, 1819. https://doi.org/10.3390/jcm8111819
Abuhasira R, Ron A, Sikorin I, Novack V. Medical Cannabis for Older Patients—Treatment Protocol and Initial Results. Journal of Clinical Medicine. 2019; 8(11):1819. https://doi.org/10.3390/jcm8111819
Chicago/Turabian StyleAbuhasira, Ran, Addie Ron, Inbal Sikorin, and Victor Novack. 2019. "Medical Cannabis for Older Patients—Treatment Protocol and Initial Results" Journal of Clinical Medicine 8, no. 11: 1819. https://doi.org/10.3390/jcm8111819
APA StyleAbuhasira, R., Ron, A., Sikorin, I., & Novack, V. (2019). Medical Cannabis for Older Patients—Treatment Protocol and Initial Results. Journal of Clinical Medicine, 8(11), 1819. https://doi.org/10.3390/jcm8111819





