Hyaluronic Acid Gel-Based Scaffolds as Potential Carrier for Growth Factors: An In Vitro Bioassay on Its Osteogenic Potential
Abstract
:1. Introduction
2. Methods
2.1. Hyaluronic Acid and Recombinant Human BMP9
2.2. ELISA Protein Release of rhBMP9 from HA
2.3. Proliferation Assay
2.4. ALP Activity Assay
2.5. Real-Time PCR for Osteoblast Differentiation Markers
2.6. Alizarin Red Staining
2.7. Statistical Analysis
3. Results
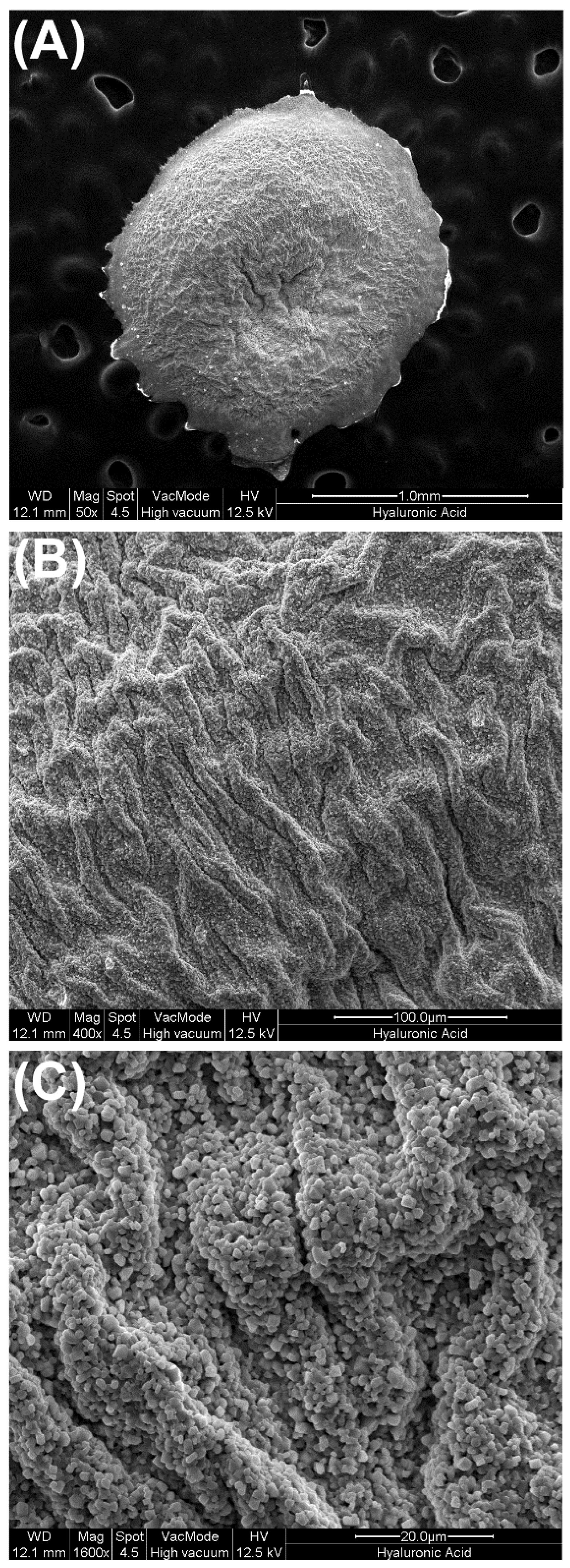
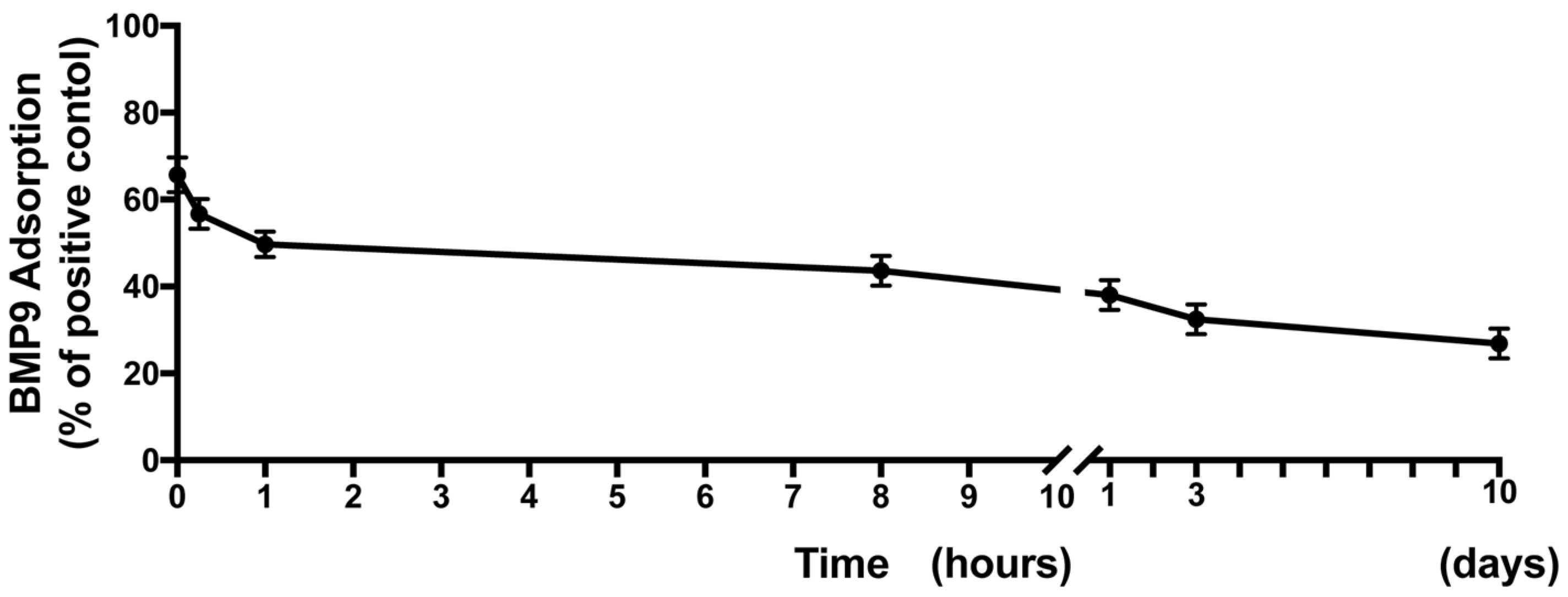
3.1. Surface Characteristics of HA Scaffolds and Ability to Hold and Release rhBMP9 over Time
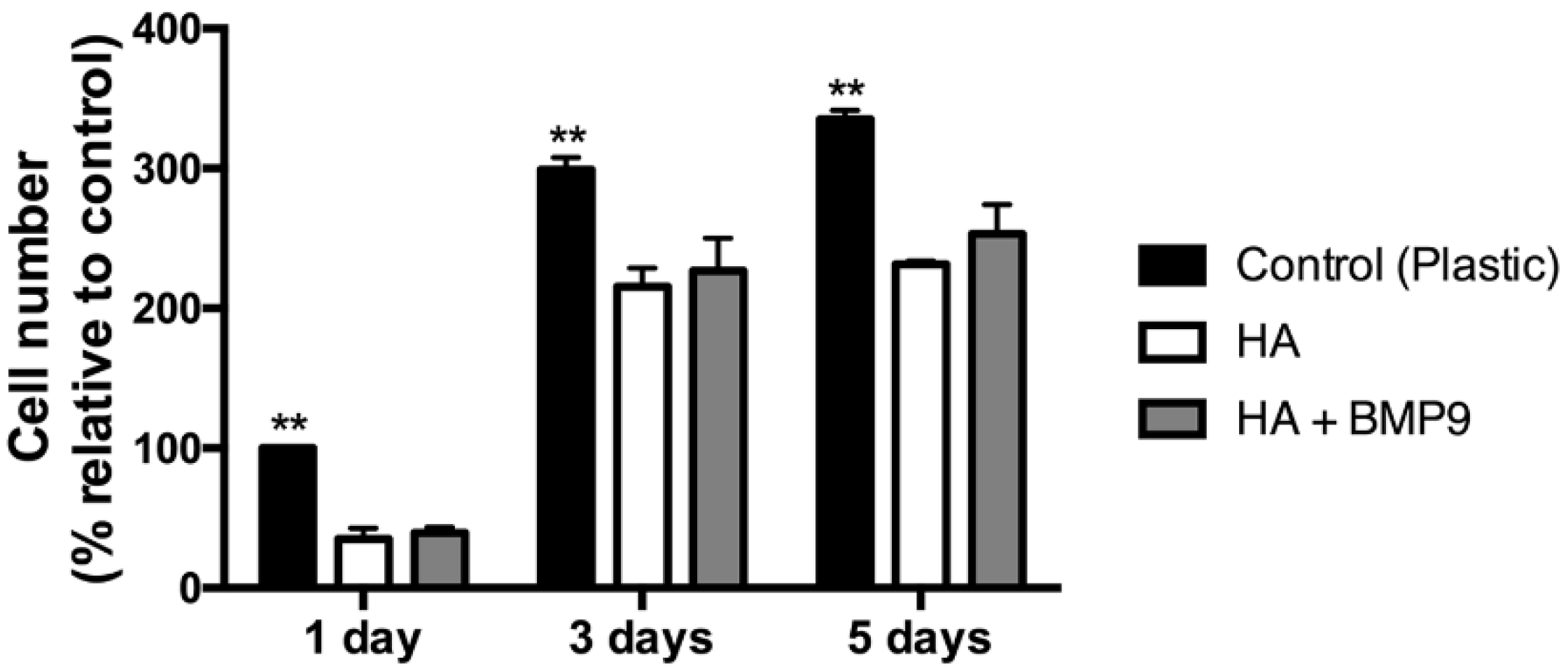
3.2. Effect of HA Alone and in Combination with rhBMP9 on ST2 Cell Proliferation
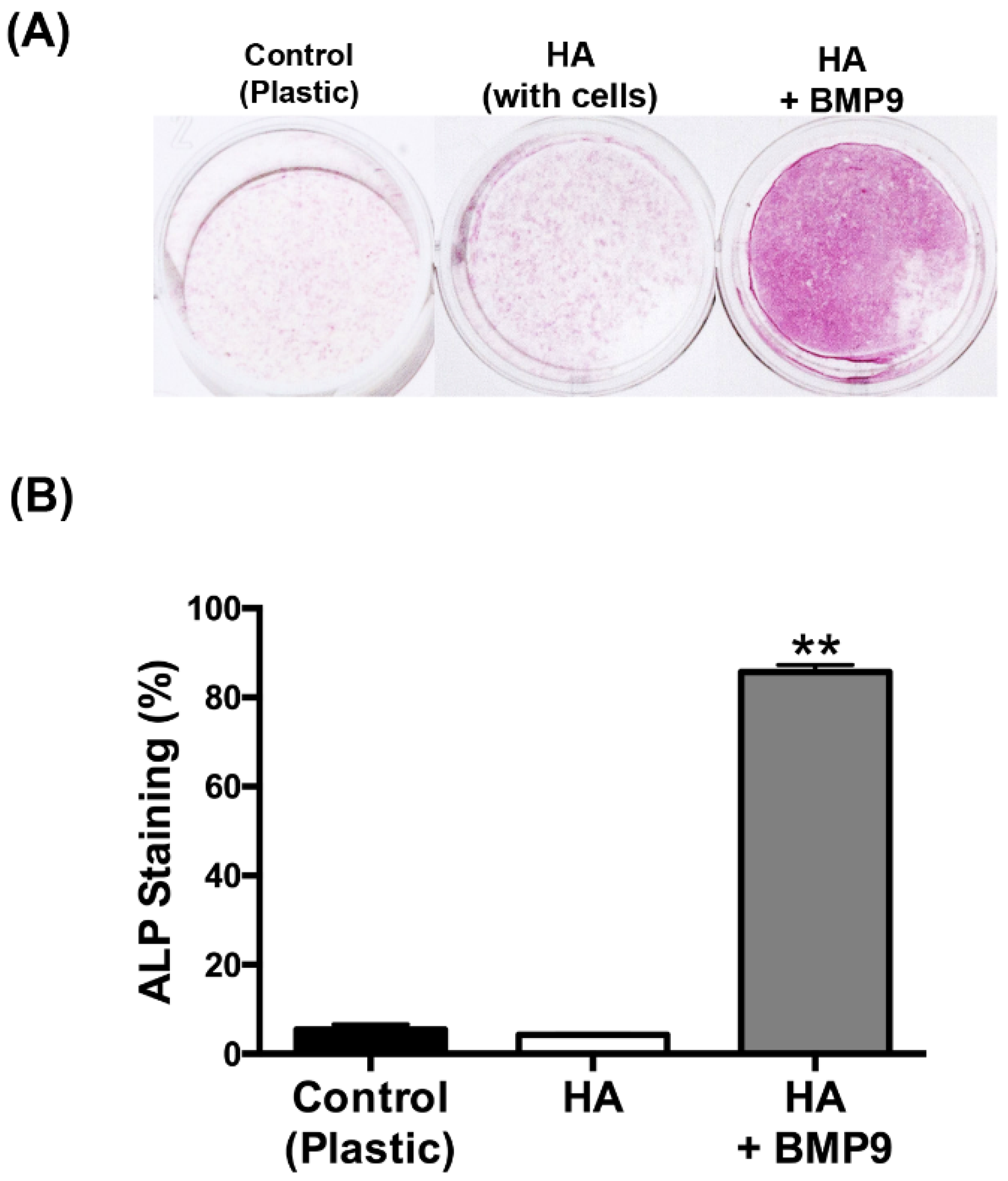
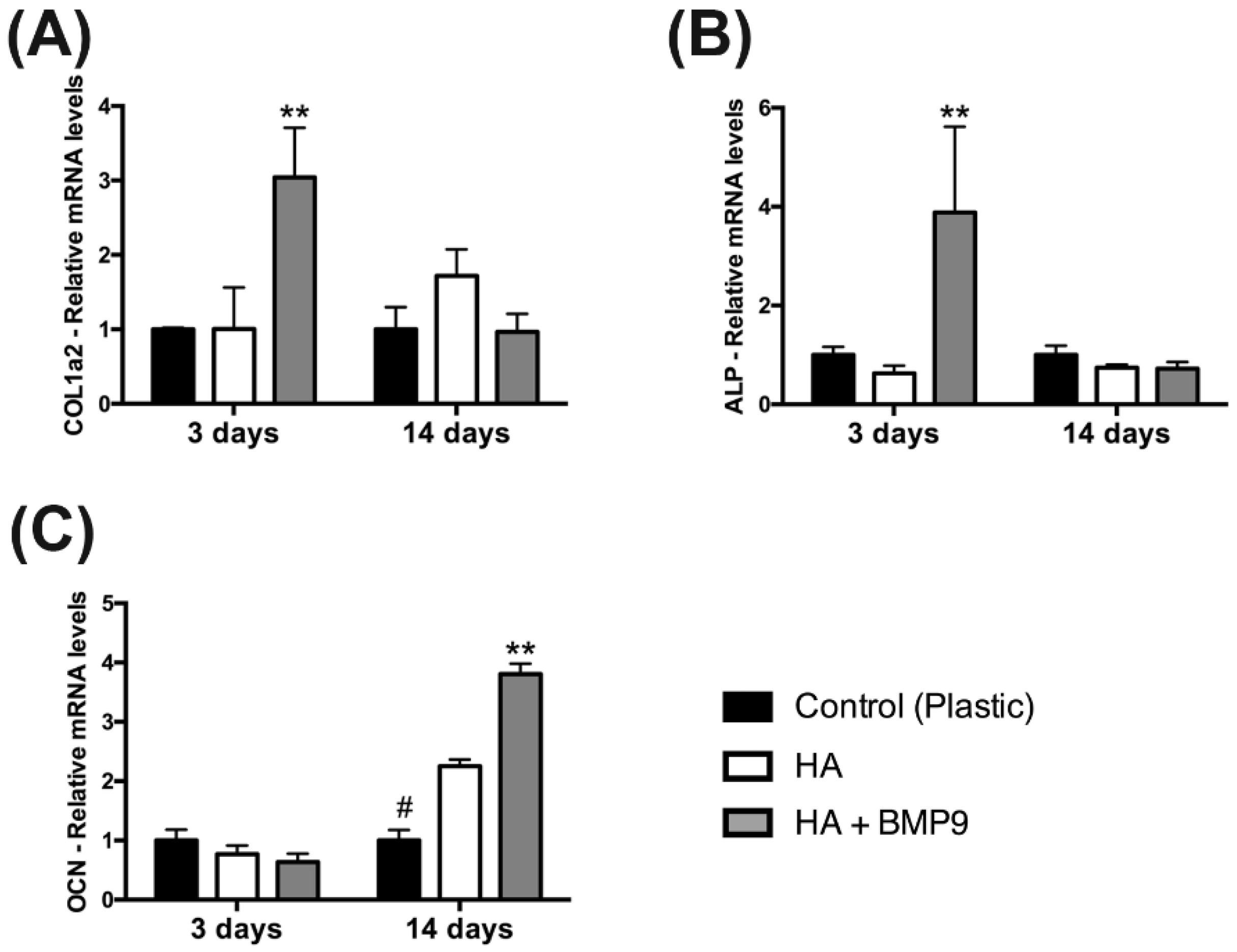
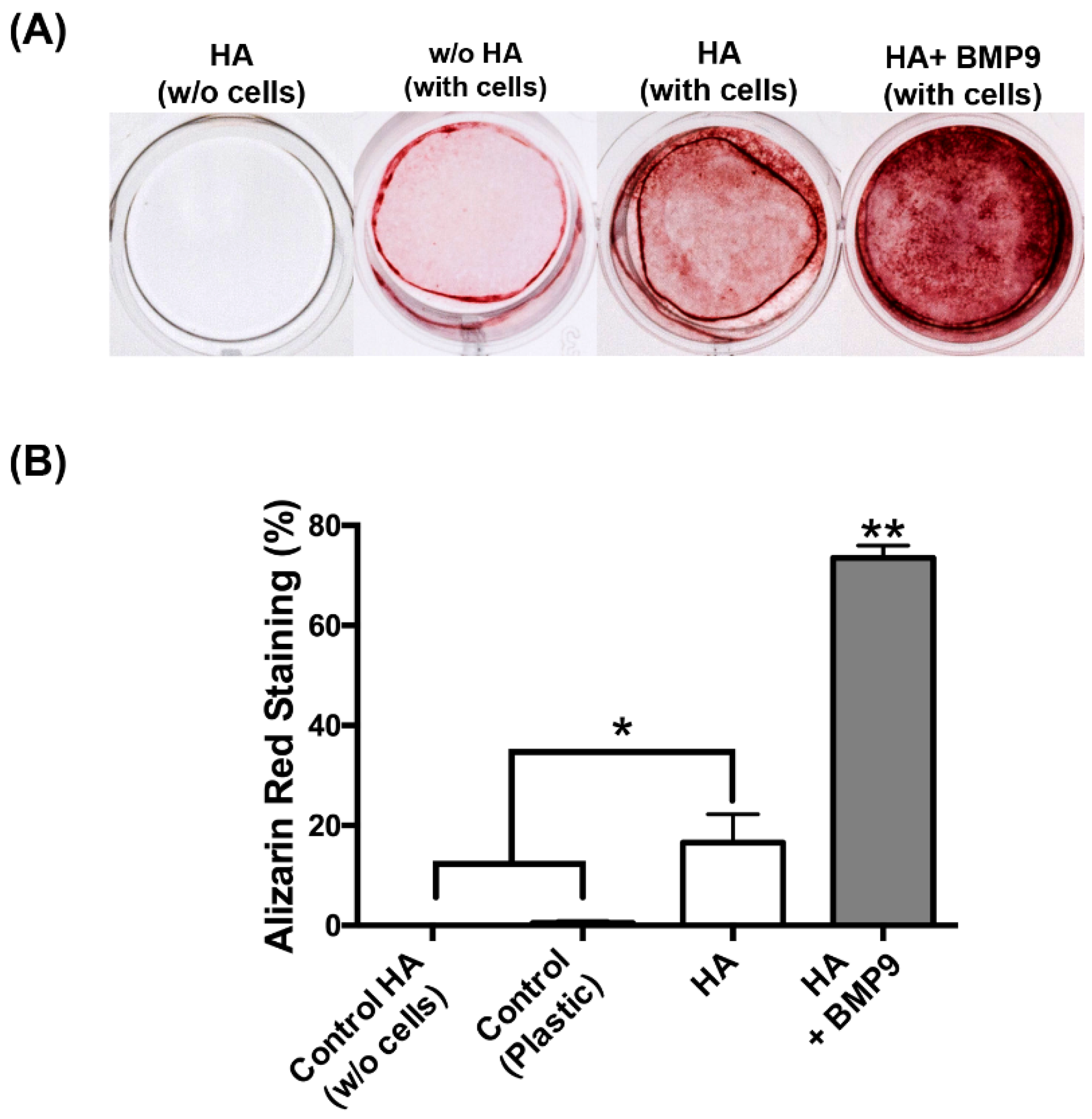
3.3.Effect of HA on ST2 Cell Differentiation When Combined with rhBMP9
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Rosen, V. BMP and BMP inhibitors in bone. Ann. N. Y. Acad. Sci. 2006, 1068, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Bessa, P.C.; Casal, M.; Reis, R.L. Bone morphogenetic proteins in tissue engineering: The road from laboratory to clinic, part II (BMP delivery). J. Tissue Eng. Regen. Med. 2008, 2, 81–96. [Google Scholar] [CrossRef] [PubMed]
- Bessa, P.C.; Casal, M.; Reis, R.L. Bone morphogenetic proteins in tissue engineering: The road from the laboratory to the clinic, part I (basic concepts). J. Tissue Eng. Regen. Med. 2008, 2, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Carreira, A.C.; Lojudice, F.H.; Halcsik, E.; Navarro, R.D.; Sogayar, M.C.; Granjeiro, J.M. Bone morphogenetic proteins: facts, challenges, and future perspectives. J. Dent. Res. 2014, 93, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Kang, Q.; Sun, M.H.; Cheng, H.; Peng, Y.; Montag, A.G.; Deyrup, A.T.; Jiang, W.; Luu, H.H.; Luo, J.; Szatkowski, J.P.; et al. Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther. 2004, 11, 1312–1320. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Jiang, W.; Phillips, F.M.; Haydon, R.C.; Peng, Y.; Zhou, L.; Luu, H.H.; An, N.; Breyer, B.; Vanichakarn, P.; et al. Osteogenic activity of the fourteen types of human bone morphogenetic proteins (BMPs). J. Bone Jt. Surg. Am. 2003, 85, 1544–1552. [Google Scholar] [CrossRef]
- Balmayor, E.R.; van Griensven, M. Gene therapy for bone engineering. Front. Bioeng. Biotech. 2015, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Song, J.J.; Celeste, A.J.; Kong, F.M.; Jirtle, R.L.; Rosen, V.; Thies, R.S. Bone morphogenetic protein-9 binds to liver cells and stimulates proliferation. Endocrinology 1995, 136, 4293–4297. [Google Scholar] [PubMed]
- Blunk, T.; Sieminski, A.L.; Appel, B.; Croft, C.; Courter, D.L.; Chieh, J.J.; Goepferich, A.; Khurana, J.S.; Gooch, K.J. Bone morphogenetic protein 9: A potent modulator of cartilage development in vitro. Growth Factors (Chur, Switzerland) 2003, 21, 71–77. [Google Scholar] [CrossRef]
- Leblanc, E.; Trensz, F.; Haroun, S.; Drouin, G.; Bergeron, E.; Penton, C.M.; Montanaro, F.; Roux, S.; Faucheux, N.; Grenier, G. BMP-9-induced muscle heterotopic ossification requires changes to the skeletal muscle microenvironment. J. Bone Miner. Res. 2011, 26, 1166–1177. [Google Scholar] [CrossRef] [PubMed]
- Lamplot, J.D.; Qin, J.; Nan, G.; Wang, J.; Liu, X.; Yin, L.; Tomal, J.; Li, R.; Shui, W.; Zhang, H.; et al. BMP9 signaling in stem cell differentiation and osteogenesis. Am. J. Stem Cells 2013, 2, 1–21. [Google Scholar] [PubMed]
- Fujioka-Kobayashi, M.; Sawada, K.; Kobayashi, E.; Schaller, B.; Zhang, Y.; Miron, R.J. Recombinant Human Bone Morphogenetic Protein 9 (rhBMP9) Induced Osteoblastic Behaviour on a Collagen Membrane Compared With rhBMP2. J. Periodontol. 2016, 1, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Fujioka-Kobayashi, M.; Sawada, K.; Kobayashi, E.; Schaller, B.; Zhang, Y.; Miron, R.J. Osteogenic potential of rhBMP9 combined with a bovine-derived natural bone mineral scaffold compared to rhBMP2. Clin. Oral Implants Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Zhang, Y.F. Osteoinduction: A review of old concepts with new standards. J. Dent. Res. 2012, 91, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, S.; Zhou, W.; Fu, H.; Qian, L.; Miron, R.J. Addition of a Synthetically Fabricated Osteoinductive Biphasic Calcium Phosphate Bone Graft to BMP2 Improves New Bone Formation. Clin. Implant Dent. Res. 2015. [Google Scholar] [CrossRef] [PubMed]
- Donegan, G.C.; Hunt, J.A.; Rhodes, N. Investigating the importance of flow when utilizing hyaluronan scaffolds for tissue engineering. J. Tissue Eng. Regen. Med. 2010, 4, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.G.; Nanau, R.M.; Oruna-Sanchez, L.; Coto, G. Hyaluronic acid and wound healing. J. Pharm. Pharm. Sci. 2015, 18, 53–60. [Google Scholar] [CrossRef]
- Price, R.D.; Berry, M.G.; Navsaria, H.A. Hyaluronic acid: the scientific and clinical evidence. JPRAS 2007, 60, 1110–1119. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Piccotti, F.; Guarda-Nardini, L. Hyaluronic acid in the treatment of TMJ disorders: A systematic review of the literature. Cranio 2010, 28, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Guarda-Nardini, L.; Cadorin, C.; Frizziero, A.; Ferronato, G.; Manfredini, D. Comparison of 2 hyaluronic acid drugs for the treatment of temporomandibular joint osteoarthritis. J. Oral Maxillofac. Surg. 2012, 70, 2522–2530. [Google Scholar] [CrossRef] [PubMed]
- Bartold, P.M.; Xiao, Y.; Lyngstaadas, S.P.; Paine, M.L.; Snead, M.L. Principles and applications of cell delivery systems for periodontal regeneration. Periodontology 2000 2006, 41, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.C.; Yoo, M.A.; Lee, S.Y.; Lee, H.J.; Son, D.H.; Jung, J.; Noh, I.; Kim, C.W. Modulation of biomechanical properties of hyaluronic acid hydrogels by crosslinking agents. J. Biomed. Mat. Res. Part A 2015, 103, 3072–3080. [Google Scholar] [CrossRef] [PubMed]
- Collins, M.N.; Birkinshaw, C. Hyaluronic acid based scaffolds for tissue engineering—A review. Carbohydr. Polym. 2013, 92, 1262–1279. [Google Scholar] [CrossRef] [PubMed]
- Takeda, K.; Sakai, N.; Shiba, H.; Nagahara, T.; Fujita, T.; Kajiya, M.; Iwata, T.; Matsuda, S.; Kawahara, K.; Kawaguchi, H.; Kurihara, H. Characteristics of high-molecular-weight hyaluronic acid as a brain-derived neurotrophic factor scaffold in periodontal tissue regeneration. Tissue Eng. Part A 2011, 17, 955–967. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Hedbom, E.; Saulacic, N.; Zhang, Y.; Sculean, A.; Bosshardt, D.D.; Buser, D. Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. J. Dent. Res. 2011, 90, 1428–1433. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Bosshardt, D.D.; Buser, D.; Zhang, Y.; Tugulu, S.; Gemperli, A.; Dard, M.; Caluseru, O.M.; Chandad, F.; Sculean, A. Comparison of the capacity of enamel matrix derivative gel and enamel matrix derivative in liquid formulation to adsorb to bone grafting materials. J. Periodontol. 2015, 86, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Saulacic, N.; Buser, D.; Iizuka, T.; Sculean, A. Osteoblast proliferation and differentiation on a barrier membrane in combination with BMP2 and TGFbeta1. Clin. Oral Investig. 2013, 17, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Shou, P.; Zheng, C.; Jiang, M.; Cao, G.; Yang, Q.; Cao, J.; Xie, N.; Velletri, T.; Zhang, X.; et al. Fate decision of mesenchymal stem cells: Adipocytes or osteoblasts? Cell Death Differ. 2016, 23, 1128–1139. [Google Scholar] [CrossRef] [PubMed]
- Midha, S.; Murab, S.; Ghosh, S. Osteogenic signaling on silk-based matrices. Biomaterials 2016, 97, 133–153. [Google Scholar] [CrossRef] [PubMed]
- Saltz, A.; Kandalam, U. Mesenchymal stem cells and alginate microcarriers for craniofacial bone tissue engineering: A review. J. Biomed. Mater. Res. Part A 2016, 104, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Salazar, V.S.; Gamer, L.W.; Rosen, V. BMP signalling in skeletal development, disease and repair. Nat. Rev. Endocrinol. 2016, 12, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Scarfi, S. Use of bone morphogenetic proteins in mesenchymal stem cell stimulation of cartilage and bone repair. World J. Stem Cells 2016, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Nevins, M.; Nevins, M.L.; Karimbux, N.; Kim, S.W.; Schupbach, P.; Kim, D.M. The combination of purified recombinant human platelet-derived growth factor-BB and equine particulate bone graft for periodontal regeneration. J. Periodontology 2012, 83, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Sculean, A.; Cochran, D.L.; Froum, S.; Zucchelli, G.; Nemcovsky, C.; Donos, N.; Lyngstadaas, S.P.; Deschner, J.; Dard, M.; et al. Twenty years of Enamel Matrix Derivative: The past, the present and the future. J. Clin. Periodontol 2016, 43, 668–683. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Gruber, R.; Hedbom, E.; Saulacic, N.; Zhang, Y.; Sculean, A.; Bosshardt, D.D.; Buser, D. Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin. Implant Dent. Res. 2013, 15, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Guillemette, V.; Zhang, Y.; Chandad, F.; Sculean, A. Enamel matrix derivative in combination with bone grafts: A review of the literature. Quintessence Int. (Berlin, Germany) 2014, 45, 475–487. [Google Scholar]
- Barati, D.; Shariati, S.R.; Moeinzadeh, S.; Melero-Martin, J.M.; Khademhosseini, A.; Jabbari, E. Spatiotemporal release of BMP-2 and VEGF enhances osteogenic and vasculogenic differentiation of human mesenchymal stem cells and endothelial colony-forming cells co-encapsulated in a patterned hydrogel. J. Control. Release 2016, 223, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Fujioka-Kobayashi, M.; Ota, M.S.; Shimoda, A.; Nakahama, K.; Akiyoshi, K.; Miyamoto, Y.; Iseki, S. Cholesteryl group- and acryloyl group-bearing pullulan nanogel to deliver BMP2 and FGF18 for bone tissue engineering. Biomaterials 2012, 33, 7613–7620. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, C.; Hasegawa, U.; Saita, Y.; Hemmi, H.; Hayata, T.; Nakashima, K.; Ezura, Y.; Amagasa, T.; Akiyoshi, K.; Noda, M. Osteoblastic bone formation is induced by using nanogel-crosslinking hydrogel as novel scaffold for bone growth factor. J. Cell. Physiol. 2009, 220, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, Y.; Geng, S.; Miron, R.J.; Zhang, Q.; Wu, C.; Zhang, Y. In vivo experimental study on bone regeneration in critical bone defects using PIB nanogels/boron-containing mesoporous bioactive glass composite scaffold. Int. J. Nanomed. 2015, 10, 839–846. [Google Scholar]
- Draenert, F.G.; Nonnenmacher, A.L.; Kammerer, P.W.; Goldschmitt, J.; Wagner, W. BMP-2 and bFGF release and in vitro effect on human osteoblasts after adsorption to bone grafts and biomaterials. Clin. Oral Implants Res. 2013, 24, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Fiorellini, J.P.; Howell, T.H.; Cochran, D.; Malmquist, J.; Lilly, L.C.; Spagnoli, D.; Toljanic, J.; Jones, A.; Nevins, M. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J. Periodontol. 2005, 76, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Leknes, K.N.; Yang, J.; Qahash, M.; Polimeni, G.; Susin, C.; Wikesjo, U.M. Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2: Radiographic observations. Clin. Oral Implants Res. 2008, 19, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Rothamel, D.; Herten, M.; Ferrari, D.; Sager, M.; Becker, J. Lateral ridge augmentation using particulated or block bone substitutes biocoated with rhGDF-5 and rhBMP-2: An immunohistochemical study in dogs. Clin. Oral Implants Res. 2008, 19, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, R.T.; Wang, D.; Krebsbach, P.H.; Rutherford, R.B. Gene therapy for bone formation: In vitro and in vivo osteogenic activity of an adenovirus expressing BMP7. J. Cell. Biochem. 2000, 78, 476–486. [Google Scholar] [CrossRef]
- Tannoury, C.A.; An, H.S. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. 2014, 14, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Cortivo, R.; Brun, P.; Rastrelli, A.; Abatangelo, G. In vitro studies on biocompatibility of hyaluronic acid esters. Biomaterials 1991, 12, 727–730. [Google Scholar] [CrossRef]
- Bonafe, F.; Govoni, M.; Giordano, E.; Caldarera, C.M.; Guarnieri, C.; Muscari, C. Hyaluronan and cardiac regeneration. J. Biomed. Sci. 2014, 21, 100. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Wang, X.; Qin, L.; Zhai, M.; Yuan, J.; Chen, J.; Li, D. Effect of hyaluronic acid in bone formation and its applications in dentistry. J. Biomed. Mater. Res. Part A 2016, 6, 1560–1569. [Google Scholar] [CrossRef] [PubMed]
| Gene | Primer Sequence |
|---|---|
| mCOL1a2 F | GAGCTGGTGTAATGGGTCCT |
| mCOL1a2 R | GAGACCCAGGAAGACCTCTG |
| mALP F | GGACAGGACACACACACACA |
| mALP R | CAAACAGGAGAGCCACTTCA |
| mOCN F | CAGACACCATGAGGACCATC |
| mOCN R | GGACTGAGGCTCTGTGAGGT |
| mGAPDH F | AGGTCGGTGTGAACGGATTTG |
| mGAPDH R | TGTAGACCATGTAGTTGAGGTCA |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujioka-Kobayashi, M.; Schaller, B.; Kobayashi, E.; Hernandez, M.; Zhang, Y.; Miron, R.J. Hyaluronic Acid Gel-Based Scaffolds as Potential Carrier for Growth Factors: An In Vitro Bioassay on Its Osteogenic Potential. J. Clin. Med. 2016, 5, 112. https://doi.org/10.3390/jcm5120112
Fujioka-Kobayashi M, Schaller B, Kobayashi E, Hernandez M, Zhang Y, Miron RJ. Hyaluronic Acid Gel-Based Scaffolds as Potential Carrier for Growth Factors: An In Vitro Bioassay on Its Osteogenic Potential. Journal of Clinical Medicine. 2016; 5(12):112. https://doi.org/10.3390/jcm5120112
Chicago/Turabian StyleFujioka-Kobayashi, Masako, Benoit Schaller, Eizaburo Kobayashi, Maria Hernandez, Yufeng Zhang, and Richard J. Miron. 2016. "Hyaluronic Acid Gel-Based Scaffolds as Potential Carrier for Growth Factors: An In Vitro Bioassay on Its Osteogenic Potential" Journal of Clinical Medicine 5, no. 12: 112. https://doi.org/10.3390/jcm5120112
APA StyleFujioka-Kobayashi, M., Schaller, B., Kobayashi, E., Hernandez, M., Zhang, Y., & Miron, R. J. (2016). Hyaluronic Acid Gel-Based Scaffolds as Potential Carrier for Growth Factors: An In Vitro Bioassay on Its Osteogenic Potential. Journal of Clinical Medicine, 5(12), 112. https://doi.org/10.3390/jcm5120112






