Inspiratory Muscle Training Included in Therapeutic and Training Regimens for Middle-Distance Runners
Abstract
1. Introduction
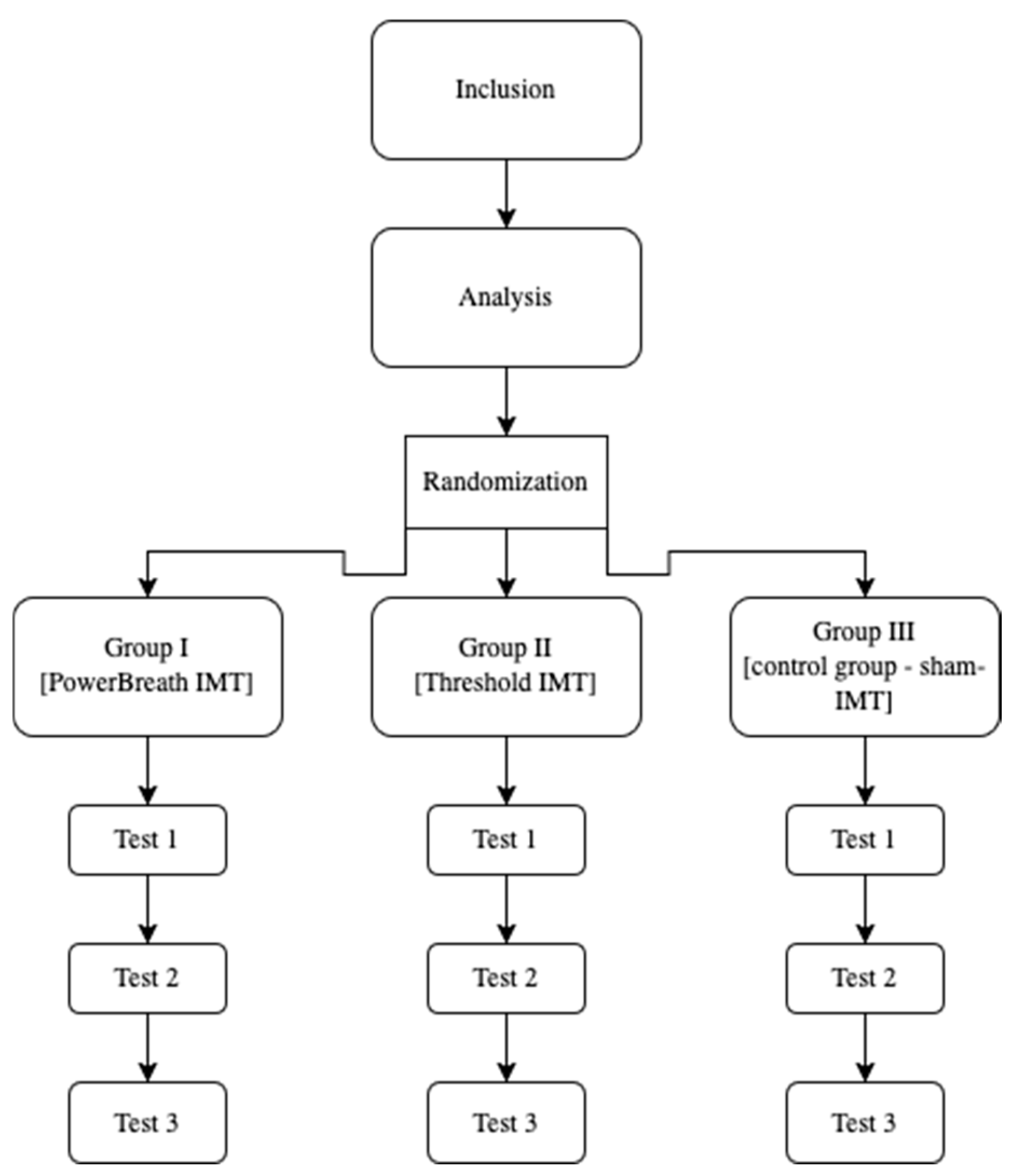
2. Materials and Methods
2.1. Participants
- –
- Five female runners who received additional IMT with the PowerBreathe device;
- –
- Six male runners who received additional IMT with the PowerBreathe device;
- –
- Five female runners who received additional IMT with the Threshold IMT device;
- –
- Six male runners who received additional IMT with the Threshold IMT device;
- –
- The control group (sham-IMT), consisting of five female runners who received additional IMT using the Threshold IMT device with a 5% load;
- –
- The control group (sham-IMT), consisting of 5 male runners who received additional IMT using the Threshold IMT device with a 5% load.
2.2. Training Characteristics of Middle-Distance Runners
2.3. Methods
2.4. Inspiratory Muscle Training Using the PowerBreathe Device
2.5. Inspiratory Muscle Training Using the Threshold Device
2.6. Inspiratory Muscle Training Sham-IMT
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| VO2max | maximal oxygen consumption |
| VCO2max | carbon dioxide output |
| RER | respiratory exchange ratio |
| VE | minute ventilation |
| VC | vital capacity |
| FEV1 | forced expiratory in one second |
| PEF | peak expiratory flow |
| PImax | inspiratory muscle strength |
| PEmax | expiratory muscle strength |
References
- Winslow, C.; Rozovsky, J. Effect of Spinal Cord Injury on the Respiratory System. Am. J. Phys. Med. Rehabil. 2003, 82, 803–814. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, T.; Hall, A.; Viana, R. The Influence of Inspiratory Muscle Training on Lung Function in Female Basketball Players—A Randomized Controlled Trial. Porto Biomed. J. 2017, 2, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Ker, J.A.; Schultz, C. Respiratory Muscle Fatigue after an Ultra-Marathon Measured as Inspiratory Task Failure. Int. J. Sports Med. 1996, 17, 493–496. [Google Scholar] [CrossRef]
- Lomax, M.E.; McConnell, A.K. Inspiratory Muscle Fatigue in Swimmers after a Single 200 m Swim. J. Sports Sci. 2003, 21, 659–664. [Google Scholar] [CrossRef]
- Aaron, E.A.; Seow, K.C.; Johnson, B.D.; Dempsey, J.A. Oxygen Cost of Exercise Hyperpnea: Implications for Performance. J. Appl. Physiol. 1992, 72, 1818–1825. [Google Scholar] [CrossRef]
- Enright, S.J.; Unnithan, V.B. Effect of Inspiratory Muscle Training Intensities on Pulmonary Function and Work Capacity in Healthy Individuals: A Randomized Controlled Trial. Phys. Ther. 2011, 91, 894–905. [Google Scholar] [CrossRef] [PubMed]
- Lorca-Santiago, J.; Jiménez, S.L.; Pareja-Galeano, H.; Lorenzo, A. Inspiratory Muscle Training in Intermittent Sports Modalities: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4448. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Romer, L.; Rodman, J.; Miller, J.; Smith, C. Consequences of Exercise-Induced Respiratory Muscle Work. Respir. Physiol. Neurobiol. 2006, 151, 242–250. [Google Scholar] [CrossRef]
- Markus, A. Pulmonary System Limitations to Endurance Exercise Performance in Humans. Exp. Physiol. 2012, 93, 311–318. [Google Scholar]
- Sheel, A.W.; Derchak, P.A.; Morgan, B.J.; Pegelow, D.F.; Jacques, A.J.; Dempsey, J.A. Fatiguing Inspiratory Muscle Work Causes Reflex Reduction in Resting Leg Blood Flow in Humans. J. Physiol. 2001, 537, 277–289. [Google Scholar] [CrossRef]
- Pastre, C.M.; Carvalho Filho, G.; Monteiro, H.L.; Netto, J.; Padovani, C.R. Sports Injuries in Brazilian Elite Athletics: Study Based on Referred Morbidity. Rev. Bras. Med. Esporte 2005, 11, 43–47. [Google Scholar] [CrossRef]
- Johnson, B.D.; Aaron, E.A.; Babcock, M.A.; Dempsey, J.A. Respiratory Muscle Fatigue During Exercise: Implications for Performance. Med. Sci. Sports Exerc. 1996, 28, 1129–1137. [Google Scholar] [CrossRef] [PubMed]
- Romer, L.M.; McConnell, A.K.; Jones, D.A. Effects of inspiratory muscle training upon recovery time during high intensity, repetitive sprint activity. Int J Sports Med. 2002, 23, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Ammous, O.; Feki, W.; Lotfi, T.; Khamis, A.M.; Gosselink, R.; Rebai, A.; Kammoun, S. Inspiratory Muscle Training, with or without Concomitant Pulmonary Rehabilitation, for Chronic Obstructive Pulmonary Disease (COPD). Cochrane Database Syst. Rev. 2023, 1, CD013778. [Google Scholar]
- Craighead, D.H.; Freeberg, K.A.; McCarty, N.P.; Seals, D.R. Time-Efficient, High-Resistance Inspiratory Muscle Strength Training for Cardiovascular Aging. Exp. Gerontol. 2021, 154, 111515. [Google Scholar] [CrossRef]
- Okrzymowska, P.; Kurzaj, M.; Seidel, W.; Rożek-Piechura, K. Eight Weeks of Inspiratory Muscle Training Improves Pulmonary Function in Disabled Swimmers—A Randomized Trial. Int. J. Environ. Res. Public Health 2019, 16, 1747. [Google Scholar] [CrossRef]
- Hajghanbari, B.; Yamabayashi, C.; Buna, T.R.; Coelho, J.D.; Freedman, K.D.; Morton, T.A.; Palmer, S.A.; Toy, M.A.; Walsh, C.; Sheel, A.W.; et al. Effects of Respiratory Muscle Training on Performance in Athletes: A Systematic Review with Meta-Analyses. J. Strength Cond. Res. 2013, 27, 1643–1663. [Google Scholar] [CrossRef]
- Sales, A.T.; Fregonezi, G.A.; Ramsook, A.H.; Guenette, J.A.; Lima, I.N.; Reid, W.D. Respiratory Muscle Endurance after Training in Athletes and Non-Athletes: A Systematic Review and Meta-Analysis. Phys. Ther. Sport 2015, 17, 76–86. [Google Scholar] [CrossRef]
- Rożek-Piechura, K.; Kurzaj, M.; Okrzymowska, P.; Kucharski, W.; Stodółka, J.; Maćkała, K. Influence of Inspiratory Muscle Training of Various Intensities on the Physical Performance of Long-Distance Runners. J. Hum. Kinet. 2020, 75, 127–137. [Google Scholar] [CrossRef]
- Kwok, T.M.K.; Jones, A.Y.M. Target-Flow Inspiratory Muscle Training Improves Running Performance in Recreational Runners: A Randomized Controlled Trial. Hong Kong Physiother. J. 2009, 27, 48–54. [Google Scholar] [CrossRef]
- Mickleborough, T.D.; Stager, J.M.; Chatham, K.; Lindley, M.R.; Ionescu, A.A. Pulmonary Adaptations to Swim and Inspiratory Muscle Training. Eur. J. Appl. Physiol. 2008, 103, 635–646. [Google Scholar] [CrossRef] [PubMed]
- West, J.B. Respiratory Physiology: The Essentials, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004. [Google Scholar]
- Chang, Y.-C.; Chang, H.-Y.; Ho, C.-C.; Lee, P.-F.; Chou, Y.-C.; Tsai, M.-W.; Chou, L.-W. Effects of 4-Week Inspiratory Muscle Training on Sport Performance in College 800-Meter Track Runners. Medicina 2021, 57, 72. [Google Scholar] [CrossRef] [PubMed]
- Ohya, T.; Yamanaka, R.; Hagiwara, M.; Oriishi, M.; Suzuki, Y. The 400- and 800-m Track Running Induces Inspiratory Muscle Fatigue in Trained Female Middle-Distance Runners. J. Strength Cond. Res. 2016, 30, 1433–1437. [Google Scholar] [CrossRef]
- Enright, S.; Chatham, K.; Ionescu, A.A.; Unnithan, V.B.; Shale, D.J. Inspiratory Muscle Training Improves Lung Function and Exercise Capacity in Adults with Cystic Fibrosis. Chest 2004, 126, 405–411. [Google Scholar] [CrossRef]
- Powers, S.K.; Howley, E.T. Exercise Physiology: Theory and Application to Fitness and Performance, 10th ed.; McGraw-Hill: New York, NY, USA, 2017. [Google Scholar]
- Ramos, I.; Barreira, S.; Viana, R. Inspiratory Muscle Training on Lung Function of Male Roller Hockey Players: A Randomized Controlled Trial Pilot Study. Porto Biomed. J. 2020, 5, e075. [Google Scholar] [CrossRef]
- McConnell, A.K.; Romer, L.M. Dyspnoea in Health and Obstructive Pulmonary Disease: The Role of Respiratory Muscle Function and Training. Sports Med. 2004, 34, 117–132. [Google Scholar] [CrossRef] [PubMed]
- Torres-Tamayo, N.; García-Martínez, D.; Lois Zlolniski, S.; Torres-Sánchez, I.; García-Río, F.; Bastir, M. 3D Analysis of Sexual Dimorphism in Size, Shape and Breathing Kinematics of Human Lungs. J. Anat. 2018, 232, 227–237. [Google Scholar] [CrossRef]
- Mitchell, R.A.; Schaeffer, M.R.; Ramsook, A.H.; Wilkie, S.S.; Guenette, J.A. Sex Differences in Respiratory Muscle Activation Patterns during High-Intensity Exercise in Healthy Humans. Respir. Physiol. Neurobiol. 2018, 247, 57–60. [Google Scholar] [CrossRef]
- Welch, J.F.; Archiza, B.; Guenette, J.A.; West, C.R.; Sheel, A.W. Sex Differences in Diaphragmatic Fatigue: The Cardiovascular Response to Inspiratory Resistance. J. Physiol. 2018, 596, 4017–4032. [Google Scholar] [CrossRef]
- Guenette, J.A.; Martens, A.M.; Lee, A.L.; Tyler, G.D.; Richards, J.C.; Foster, G.E.; Warburton, D.E.; Sheel, A.W. Variable Effects of Respiratory Muscle Training on Cycle Exercise Performance in Men and Women. Appl. Physiol. Nutr. Metab. 2006, 31, 159–166. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Quanjer, P.H.; Tammeling, G.J.; Cotes, E.J.; Pedersen, O.F.; Peslin, R.; Yernault, J.C. Lung Volumes and Forced Ventilatory Flows. Eur. Respir. J. 1993, 6, 5–40. [Google Scholar] [CrossRef] [PubMed]
- Degens, P.; Merget, R. Reference Values for Spirometry of the European Coal and Steel Community: Time for Change. Eur. Respir. J. 2008, 31, 687–688. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on Respiratory Muscle Testing. Am. J. Respir. Crit. Care Med. 2002, 166, 518–624. [Google Scholar] [CrossRef]
- Janssens, L.; Brumagne, S.; McConnell, A.K.; Raymaekers, J.; Goossens, N.; Gayan-Ramirez, G.; Hemans, G.; Trooters, T. The Assessment of Inspiratory Muscle Fatigue in Healthy Individuals: A Systematic Review. Respir. Med. 2013, 107, 331–346. [Google Scholar] [CrossRef]
- Agnihotri, D.S.; Bhise, A.R.; Patel, S.M. Effect of Inspiratory Muscle Trainer on Running Performance and Respiratory Muscle Strength in Athletes. IAIM 2016, 3, 159–163. [Google Scholar]
- Kim, K.T.; Lee, S.; Oh, E.-S. Athletes with Disabilities in the Paralympic Games: A Framing Analysis of Television News. Manag. Sport Leis. 2017, 22, 255–275. [Google Scholar] [CrossRef]
- Williams, J.S.; Wongsathikun, J.; Boon, S.M.; Acevedo, E.O. Inspiratory Muscle Training Fails to Improve Endurance Capacity in Athletes. Med. Sci. Sports Exerc. 2002, 34, 1194–1198. [Google Scholar] [CrossRef]
- Støa, E.M.; Helgerud, J.; Rønnestad, B.R.; Hansen, J.; Ellefsen, S.; Støren, Ø. Factors Influencing Running Velocity at Lactate Threshold in Male and Female Runners at Different Levels of Performance. Front. Physiol. 2020, 11, 585267. [Google Scholar] [CrossRef]
- Santisteban, K.J.; Lovering, A.T.; Halliwill, J.R.; Minson, C.T. Sex Differences in VO2max and the Impact on Endurance-Exercise Performance. Int. J. Environ. Res. Public Health 2022, 19, 4946. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yáñez-Sepúlveda, R.; Verdugo-Marchese, H.; Duclos-Bastías, D.; Tuesta, M.; Alvear-Ordenes, I. Effects of Inspiratory Muscle Training on Muscle Oxygenation During Vascular Occlusion Testing in Trained Healthy Adult Males. Int. J. Environ. Res. Public Health 2022, 19, 16766. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rehder-Santos, P.; Abreu, R.M.; de Signini, É.F.; da Silva, C.D.; Sakaguchi, C.A.; Dato, C.C.; Catai, A.M. Moderate- and High-Intensity Inspiratory Muscle Training Equally Improves Inspiratory Muscle Strength and Endurance—A Double-Blind Randomized Controlled Trial. Int. J. Sports Physiol. Perform. 2021, 16, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- LoMauro, A.; Aliverti, A. Sex Differences in Respiratory Function. Breathe (Sheff.) 2018, 14, 131–140. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aliverti, A. Lung and Chest Wall Mechanics During Exercise: Effects of Expiratory Flow Limitation. Respir. Physiol. Neurobiol. 2008, 163, 90–99. [Google Scholar] [CrossRef]
- Cunha, M.; Mendes, F.; Paciência, I.; Rodolfo, A.; Carneiro-Leão, L.; Rama, T.; Rufo, J.; Delgado, L.; Moreira, A. The Effect of Inspiratory Muscle Training on Swimming Performance, Inspiratory Muscle Strength, Lung Function, and Perceived Breathlessness in Elite Swimmers. Porto Biomed. J. 2019, 4, 49. [Google Scholar] [CrossRef]
- Hartz, C.S.; Sindorf, M.A.G.; Lopes, C.R.; Batista, J.; Moreno, M.A. Effect of Inspiratory Muscle Training on Performance of Handball Athletes. J. Hum. Kinet. 2018, 63, 43–51. [Google Scholar] [CrossRef]


 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, 3, p = 0.123.
Sham IMT—control group, and trials 1, 2, 3, p = 0.123.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, 3, p = 0.123.
Sham IMT—control group, and trials 1, 2, 3, p = 0.123.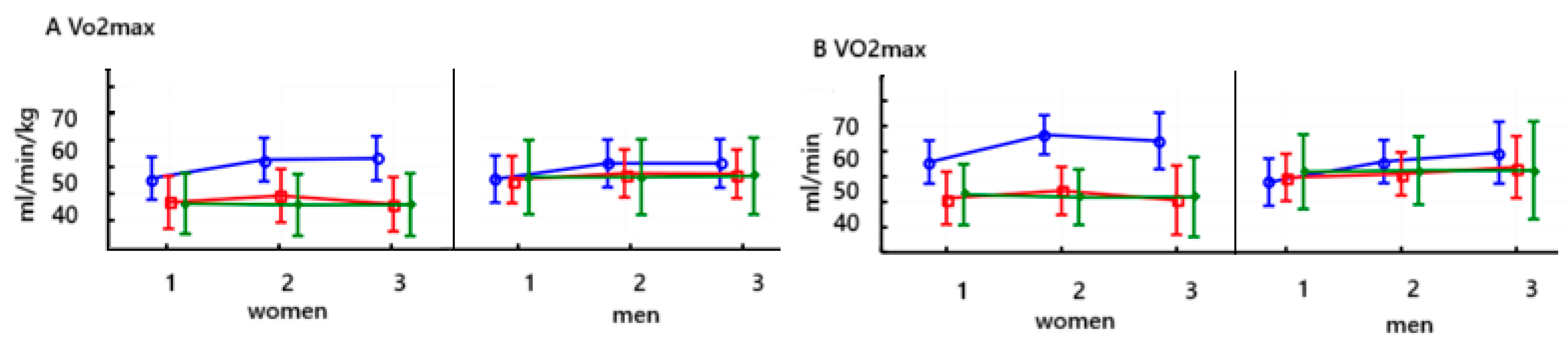
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.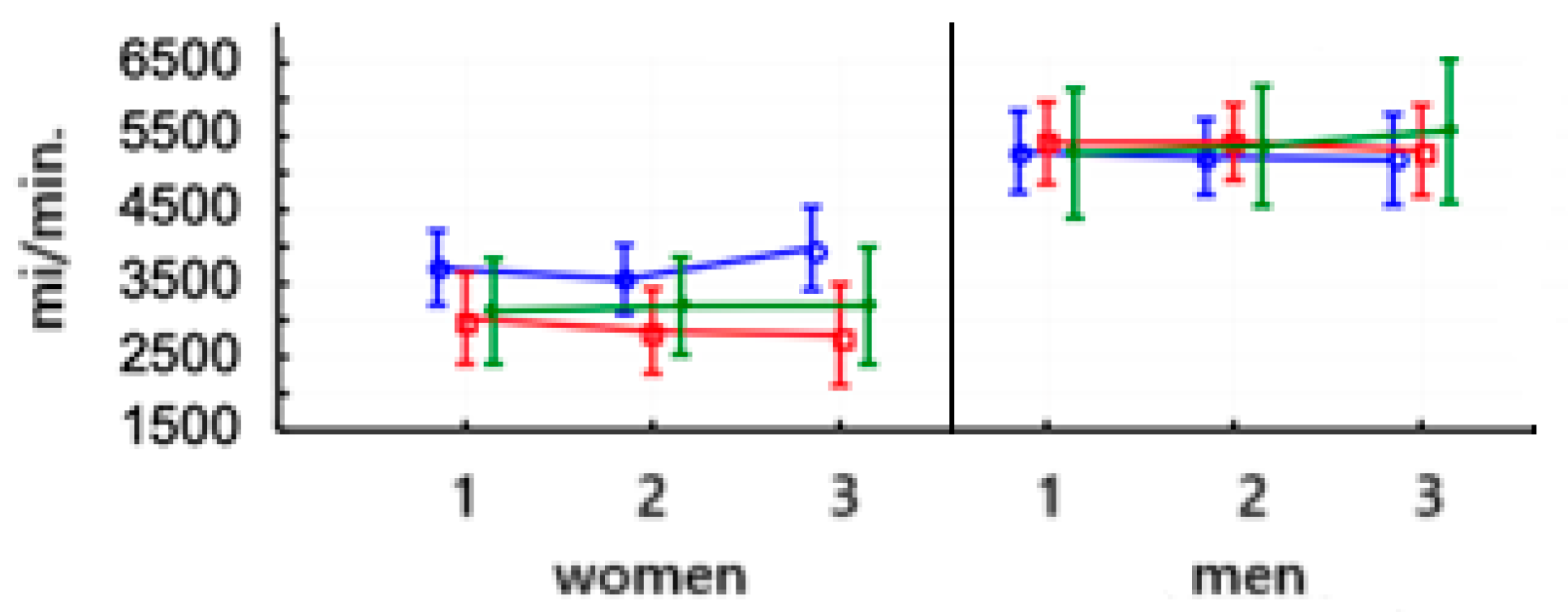
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.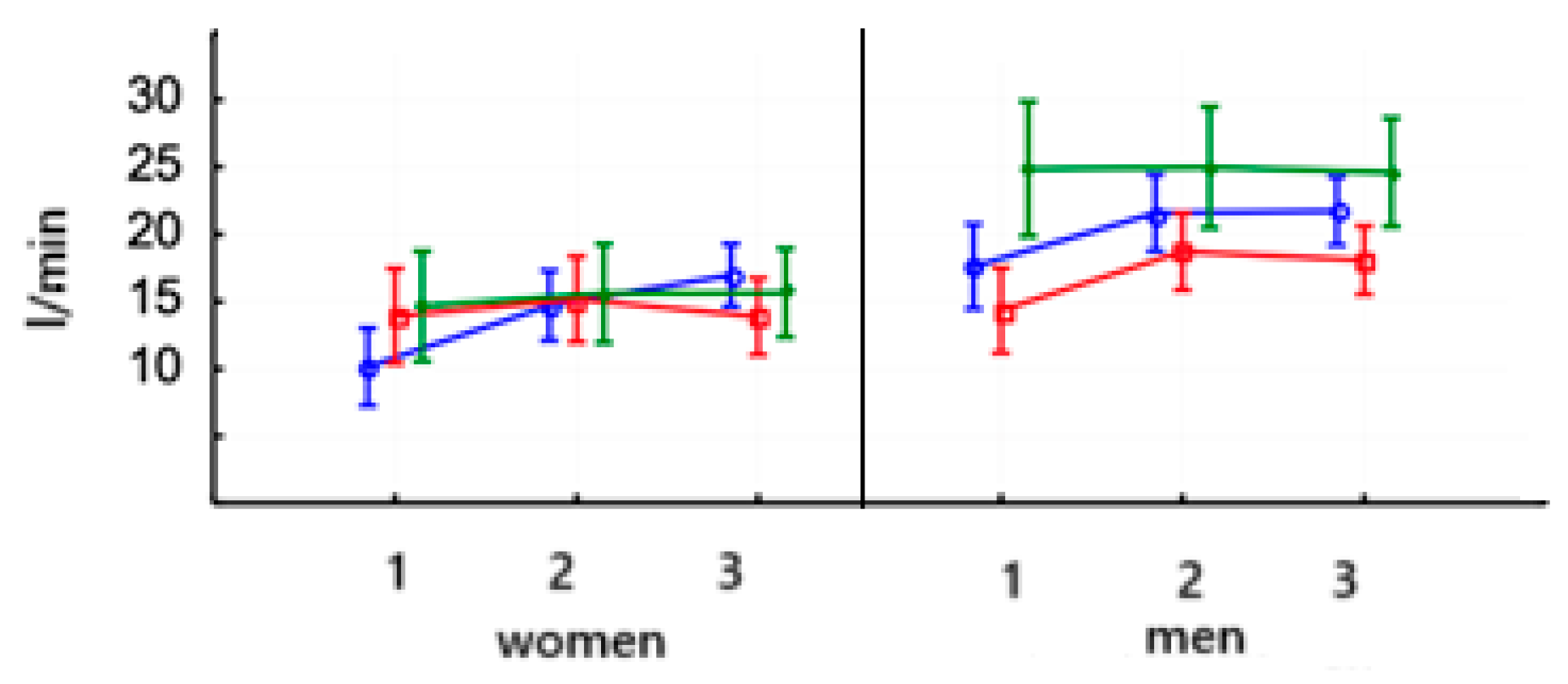
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.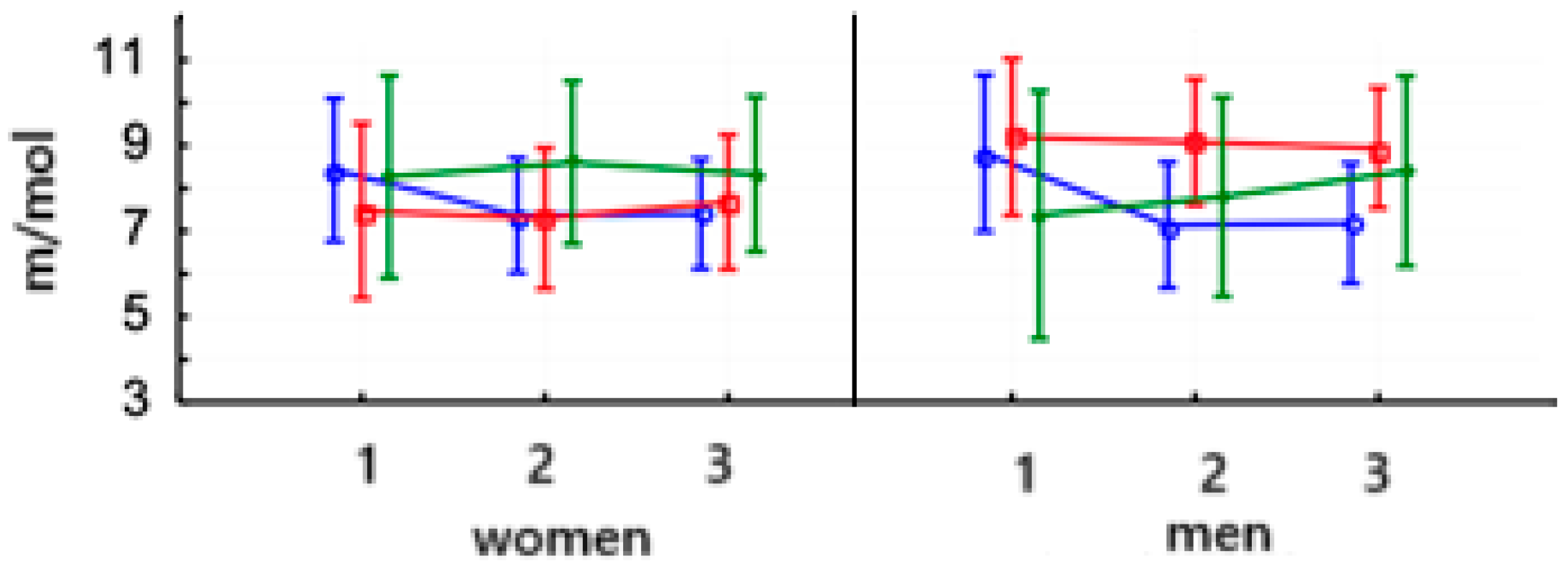
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.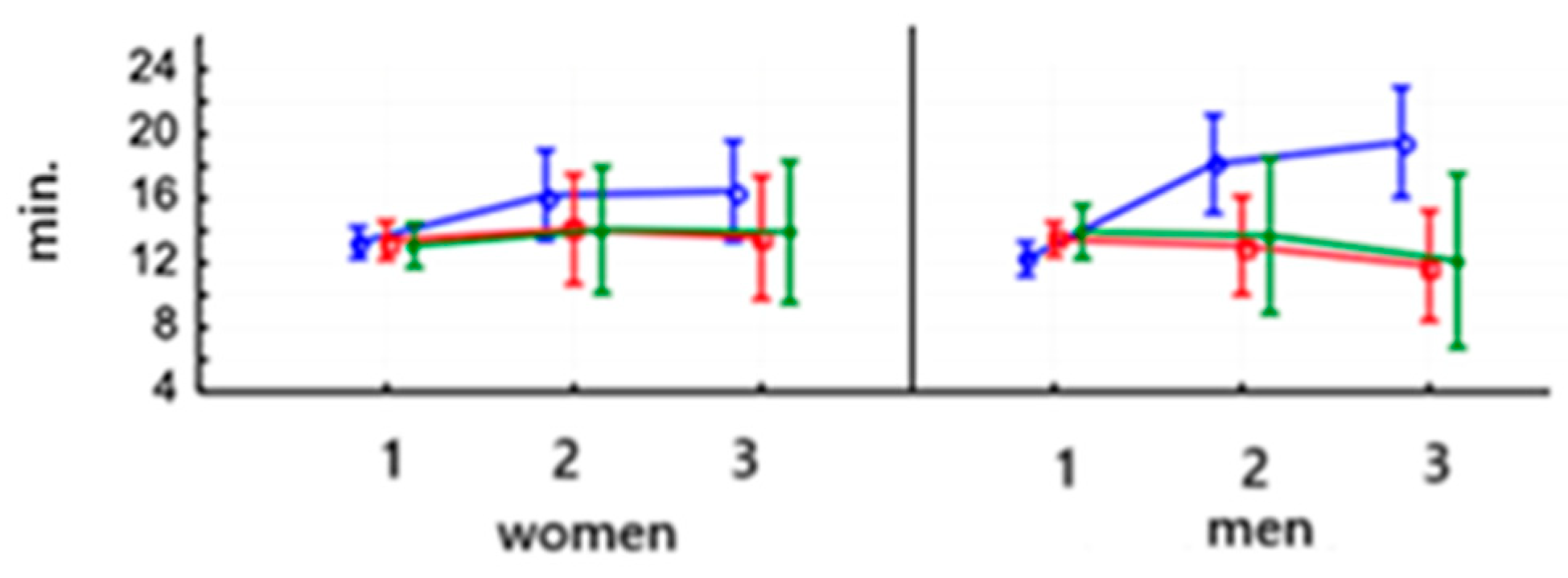
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.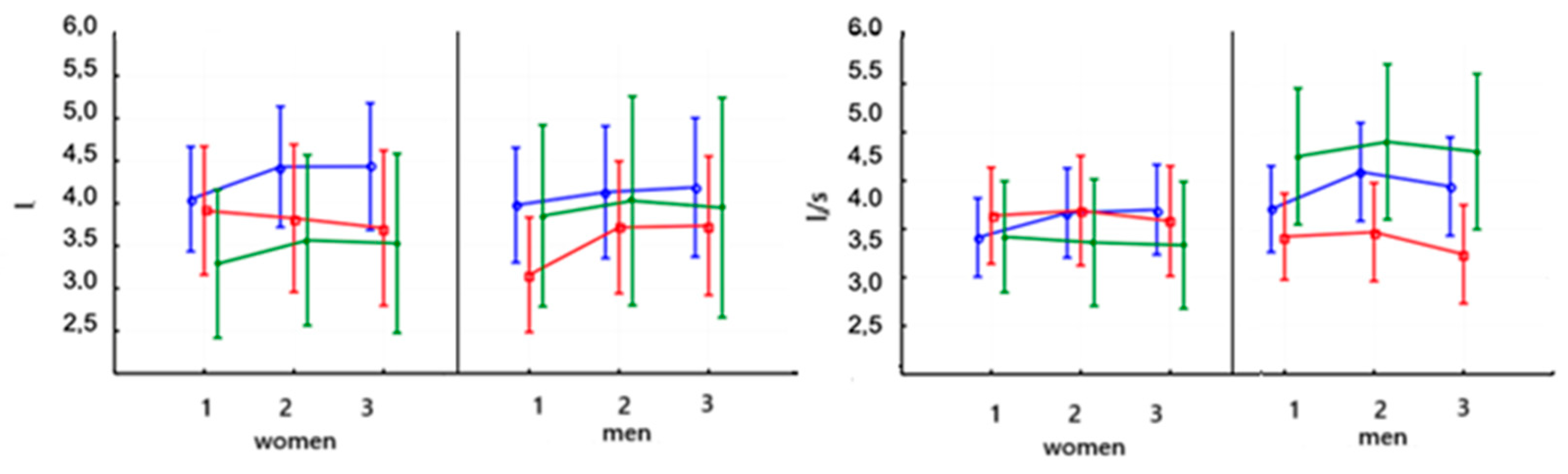
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.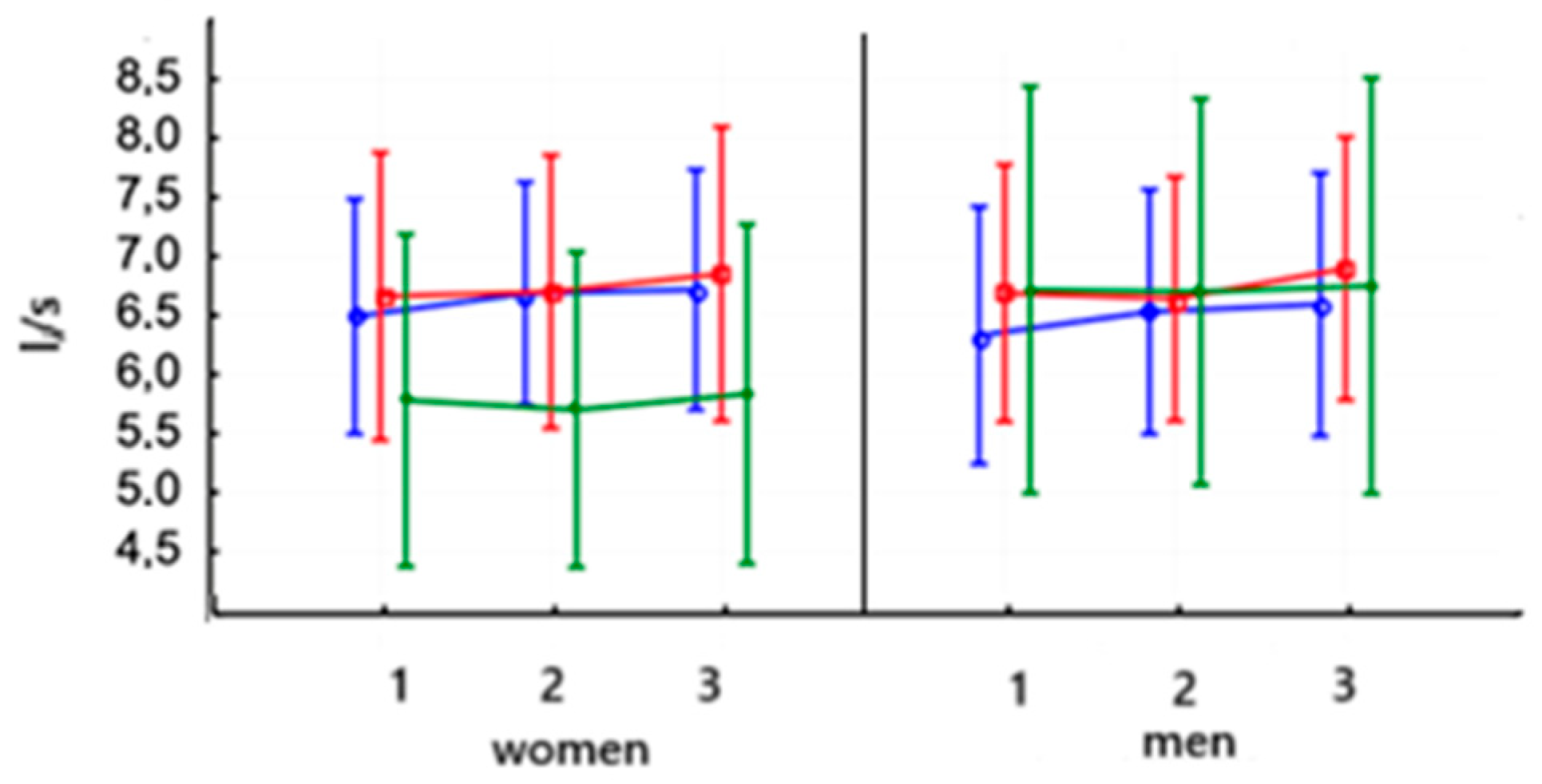
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.
 PowerBreathe IMT,
PowerBreathe IMT,  Threshold IMT,
Threshold IMT,  Sham IMT—control group, and trials 1, 2, and 3.
Sham IMT—control group, and trials 1, 2, and 3.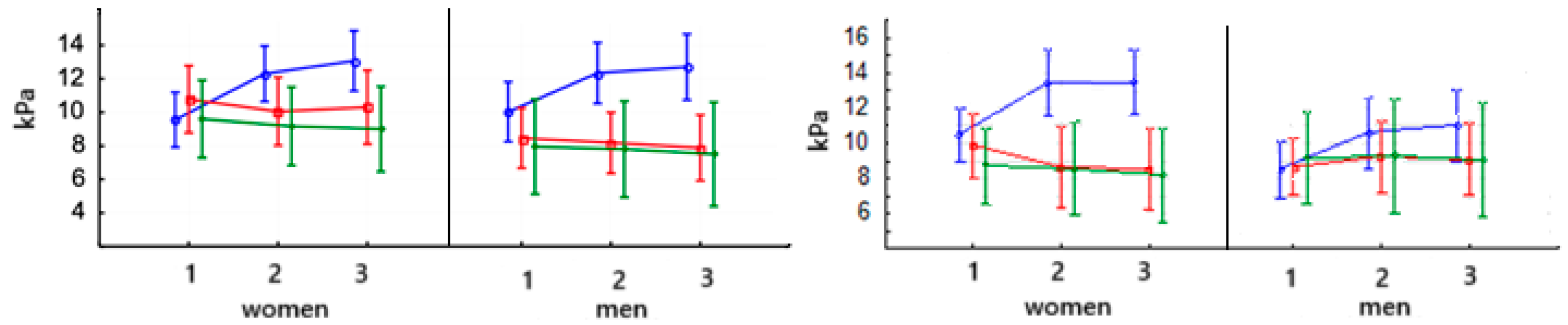
| Variable | Sex | Group I [PowerBreathe IMT] | Group II [Threshold IMT] | Group III [Control Group] |
|---|---|---|---|---|
| Age [years] | W | 23.3 ± 1.83 | 22.0 ± 3.4 | 21.5 ± 2.82 |
| M | 22.3 ± 2.98 | 23.5 ± 3.54 | 22.5 ± 1.9 | |
| Height [cm] | W | 1.63 ± 0.04 | 1.69 ± 0.06 | 1.61 ± 0.08 |
| M | 1.82 ± 0.06 | 1.82 ± 0.04 | 1.84 ± 0.03 | |
| Body weight [kg] | W | 55.5 ± 3.24 | 62.0 ± 1.65 | 51.0 ± 8.38 |
| M | 70.4 ± 5.46 | 75.2 ± 4.32 | 76.5 ± 3.56 | |
| BMI [kg/m2] | W | 21.43 ± 0.4 | 22.03 ± 0.33 | 20.15 ± 0.72 |
| M | 22.39 ± 0.84 | 22.65 ± 1.3 | 22.71 ± 0.43 |
| Type of Training Modality (Workout) | Training Session (7-Day Microcycle) Middle Distance | |
|---|---|---|
| Number of Performance (n) | Mileage (km) | |
| Strength endurance (combined with circuit training) | 1 | |
| GE1 (general endurance: 65–79% max HR or 1–2 mmol LA) | 4 | 40–50 |
| GE2 (general durance: 75–85% max HR or 2–4 mmol LA) | 1 | 5–10 |
| SP (special endurance: 85–95% max HR or 6–8 mmol LA) | 2 | 5–10 |
| Tempo (interval training: 85–95% max HR or 8–10 mmol LA) | 1 | 3–5 |
| SRE (strength running endurance: skips and hill running) | 2 | 3 |
| General fitness (supplementary session) | 2 | |
| Recovery (swimming, massage, cryotherapy) | 1 | |
| Day off (rest) | 1 | |
| Total training workouts per module | 15 | 56–78 |
| Training Week | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Training load | 50% PImax | 50% PImax | 50% PImax | 60% PImax | 60% PImax | 60% PImax | 70% PImax | 70% PImax |
| Training session (series × number of breaths) | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 |
| Training Week | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Training load | 30% PImax | 30% PImax | 40% PImax | 40% PImax | 40% PImax | 50% PImax | 50% PImax | 50% PImax |
| Training session (series × number of breaths) | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 | 2 × 30 |
| Training Week | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Training load | 15% PImax | |||||||
| Training session (series × number of breaths) | 1 × 60 | |||||||
| Variable | PowerBreathe IMT Mean Change (Test II—Test I) | Threshold IMT Mean Change (Test II—Test I) | Control Group Mean Change (Test II—Test I) | PowerBreathe IMT Mean Change (Test III—Test II) | Threshold IMT Mean Change (Test III—Test II) | Control Group Mean Change (Test III—Test II) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| sex | W | M | W | M | W | M | W | M | W | M | W | M |
| VO2max [mL/min] | 348.8 ** a | 294.4 *** c | 127.4 * b | 116.6 * b | −26.7 a | 4 a | 21.5 | 0 | −158.3 ** b | −10 | 5.3 | 17.5c |
| VO2/kg [(mL/mi)/kg] | 5.39 *** b | 4.08 * c | 1.45 b | 0.7 | −0.5 a | 0.25 b | 1.21 | −1.76 a | 1.85c | −1.34 | −0.07 | −0.05 |
| VCO2max [mL/min] | −157.5 a | −70.2 a | −176.0 | 11.06 | 70.0 a | 100.0 | 425.34 ** a | −33.0 | −51.0 | −113.3 a | 6.0 | 205.5 |
| RER | 4.56 *** c | 3.97 ** b | 1.25 a | 4.37 *** c | 0.94 b | 0.11 | 2.26 b | 0.15 | −1.29 a | −0.64 a | 0.04 | −0.38 a |
| V’E [L/min] | 14.67 *** c | 26.2 *** c | 11.25 *** c | 15.2 *** c | 0.33 | 0 | 0.66 | 4.2 ** a | −11.3 *** c | −12.4 *** c | −1.0 | −1.5 a |
| lactic acid [m/mL] | −1.06 ** a | −1.69 *** c | −0.12 | 0.33 | 0.42 a | 0.03 | 0.04 | 0.38 b | −0.14 | −0.27 | 0.6 c | |
| lactate threshold [min] | 2.94 ** c | 5.88 *** c | 0.7 b | −0.41 a | 0.97 a | −0.25 a | 0.25 | 1.35 a | −0.52 a | −1.24 c | −0.13 | −1.55 b |
| Variable | PowerBreathe IMT Mean Change (Test II–Test I) | Threshold IMT Mean Change (Test II–Test I) | Control Group Mean Change (Test II–Test I) | PowerBreathe IMT Mean Change (Test III–Test II) | Threshold IMT Mean Change (Test III–Test II) | Control Group Mean Change (Test III–Test II) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| sex | W | M | W | M | W | M | W | M | W | M | W | M |
| VC [L] | 0.38 * a | 0.15 a | −0.09 | 0.55 *** c | 0.27 a | 0.18 | 0 | 0.05 | −0.11 a | 0.02 | −0.03 | −0.08 |
| FEV1 [L/s] | 0.25 * a | 0.39 *** b | 0.05 | 0.04 | −0.06 | 0.15 | 0.04 | −0.15 a | −0.11 a | −0.22 a | −0.03 | −0.1 |
| PEF [L/s] | 0.19 | 0.2 a | 0.04 | −0.04 | −0.08 | −0.01 | 0.04 | 0.06 | 0.15 a | 0.26 a | 0.13 | 0.05 |
| PImax [kPa] | 2.74 *** c | 2.31 *** c | −0.72 b | −0.28 c | −0.43 a | −0.15 a | 0.76 * a | 0.36 | 0.25 | −0.3 | −0.17 | −0.3 b |
| PEmax [kPa] | 2.95 *** c | 2.95 *** c | −1.2 * c | 0.56 a | −0.17 | 0.05 | 0.19 | 0.4 a | −0.12 | −0.14 | −0.36 a | −0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okrzymowska, P.; Mackala, K.; Kucharski, W.; Rozek-Piechura, K. Inspiratory Muscle Training Included in Therapeutic and Training Regimens for Middle-Distance Runners. J. Clin. Med. 2025, 14, 3180. https://doi.org/10.3390/jcm14093180
Okrzymowska P, Mackala K, Kucharski W, Rozek-Piechura K. Inspiratory Muscle Training Included in Therapeutic and Training Regimens for Middle-Distance Runners. Journal of Clinical Medicine. 2025; 14(9):3180. https://doi.org/10.3390/jcm14093180
Chicago/Turabian StyleOkrzymowska, Paulina, Krzysztof Mackala, Wojciech Kucharski, and Krystyna Rozek-Piechura. 2025. "Inspiratory Muscle Training Included in Therapeutic and Training Regimens for Middle-Distance Runners" Journal of Clinical Medicine 14, no. 9: 3180. https://doi.org/10.3390/jcm14093180
APA StyleOkrzymowska, P., Mackala, K., Kucharski, W., & Rozek-Piechura, K. (2025). Inspiratory Muscle Training Included in Therapeutic and Training Regimens for Middle-Distance Runners. Journal of Clinical Medicine, 14(9), 3180. https://doi.org/10.3390/jcm14093180








