Coping Strategies and Health-Related Quality of Life in Individuals with Heart Failure
Abstract
:1. Introduction
- 1.
- Examine the associations between HF severity (i.e., HF classification) and the types of coping strategies (i.e., problem-focused, active emotion-focused, and avoidant emotion-focused coping).
- 2.
- Examine relationships between the influencing factors (i.e., age, sex, education, income, and HF duration) and the three types of coping strategies.
- 3.
- Identify associations between coping strategies and physical and emotional HRQoL.
2. Methods
2.1. Sample and Setting
2.2. Measures
2.2.1. HF Severity
2.2.2. Influencing Factors
2.2.3. Coping Strategies
2.2.4. Health-Related Quality of Life (HRQoL)
2.3. Statistical Analysis
3. Results
Participant Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HF | Heart Failure |
| HRQoL | Health-related Quality of Life |
| NYHA | the New York Heart Association |
| RCT | Randomized Controlled Trial |
| Brief COPE | Brief Coping Orientation to Problems Experienced Inventory |
| MLHFQ | the Minnesota Living with Heart Failure Questionnaire |
References
- Hwang, B.; Pelter, M.M.; Moser, D.K.; Dracup, K. Effects of an educational intervention on heart failure knowledge, self-care behaviors, and health-related quality of life of patients with heart failure: Exploring the role of depression. Patient Educ. Couns. 2020, 103, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. Defining Health-Related Quality of Life (HRQOL). Available online: https://archive.cdc.gov/#/details?url=https://www.cdc.gov/hrqol/index.htm (accessed on 16 July 2021).
- Jurgens, C.Y.; Lee, C.S.; Aycock, D.M.; Creber, R.M.; Denfeld, Q.E.; DeVon, H.A.; Evers, L.R.; Jung, M.; Pucciarelli, G.; Streur, M.M.; et al. State of the science: The relevance of symptoms in cardiovascular disease and research: A scientific statement from the American Heart Association. Circulation 2022, 146, e173–e184. [Google Scholar] [CrossRef] [PubMed]
- Lavalle, C.; Mariani, M.V.; Severino, P.; Palombi, M.; Trivigno, S.; D’Amato, A.; Silvetti, G.; Pierucci, N.; Di Lullo, L.; Chimenti, C.; et al. Efficacy of Modern Therapies for Heart Failure with Reduced Ejection Fraction in Specific Population Subgroups: A Systematic Review and Network Meta-Analysis. Cardiorenal Med. 2024, 14, 570–580. [Google Scholar] [CrossRef]
- McHugh, K.; DeVore, A.D.; Wu, J.; Matsouaka, R.A.; Fonarow, G.C.; Heidenreich, P.A.; Yancy, C.W.; Green, J.B.; Altman, N.; Hernandez, A.F.; et al. Heart failure with preserved ejection fraction and diabetes: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019, 73, 602–611. [Google Scholar] [CrossRef]
- Liu, M.-H.; Chiou, A.-F.; Wang, C.-H.; Yu, W.-P.; Lin, M.-H. Relationship of symptom stress, care needs, social support, and meaning in life to quality of life in patients with heart failure from the acute to chronic stages: A longitudinal study. Health Qual. Life Outcomes 2021, 19, 252. [Google Scholar] [CrossRef]
- Johansson, I.; Joseph, P.; Balasubramanian, K.; McMurray, J.J.; Lund, L.H.; Ezekowitz, J.A.; Kamath, D.; Alhabib, K.; Bayes-Genis, A.; Budaj, A.; et al. Health-Related Quality of Life and Mortality in Heart Failure: The Global Congestive Heart Failure Study of 23,000 Patients from 40 Countries. Circulation 2021, 143, 2129–2142. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.A.; Riegel, B.; Bittner, V.; Nichols, J. Validity and reliability of the NYHA classes for measuring research outcomes in patients with cardiac disease. Heart Lung 2002, 31, 262–270. [Google Scholar] [CrossRef]
- Alanazi, M.O.; Given, C.W.; Deka, P.; Lehto, R.; Wyatt, G. A literature review of coping strategies and health-related quality of life among patients with heart failure. Eur. J. Cardiovasc. Nurs. 2022, 22, 236–244. [Google Scholar] [CrossRef]
- Alhurani, A.S.; Dekker, R.; Ahmad, M.; Miller, J.; Yousef, K.M.; Abdulqader, B.; Salami, I.; Lennie, T.A.; Randall, D.C.; Moser, D.K. Stress, cognitive appraisal, coping, and event free survival in patients with heart failure. Heart Lung 2018, 47, 205–210. [Google Scholar] [CrossRef]
- Bose, C.N.; Saboonchi, F.; Persson, H.; Björling, G.; Elfström, M.L. Adaptation of Coping Effectiveness Training for Patients With Heart Failure and Patient-Reported Experience of the Intervention. J. Patient Exp. 2020, 7, 1054–1061. [Google Scholar] [CrossRef]
- McLean, L.; Gaul, D.; Penco, R. Perceived social support and stress: A study of 1st year students in Ireland. Int. J. Ment. Health Addict. 2022, 21, 2101–2121. [Google Scholar] [CrossRef] [PubMed]
- Biggs, A.; Brough, P.; Drummond, S. Lazarus and Folkman’s psychological stress and coping theory. In The Handbook of Stress and Health: A Guide to Research and Practice; Wiley: Hoboken, NJ, USA, 2017; pp. 351–364. [Google Scholar]
- Kyriakou, M.; Middleton, N.; Ktisti, S.; Philippou, K.; Lambrinou, E. Supportive care interventions to promote health-related quality of life in patients living with heart failure: A systematic review and meta-analysis. Heart Lung Circ. 2020, 29, 1633–1647. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Yang, C.Y.; Inder, K.; Chan, S.W.C. Illness perceptions, coping strategies, and quality of life in people with multiple chronic conditions. J. Nurs. Sch. 2020, 52, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Lynggaard, V.; Nielsen, C.V.; Zwisler, A.D.; Taylor, R.S.; May, O. The patient education—Learning and Coping Strategies—Improves adherence in cardiac rehabilitation (LC-REHAB): A randomised controlled trial. Int. J. Cardiol. 2017, 236, 65–70. [Google Scholar] [CrossRef]
- Schneider, A.; Minke HTHartman, K.N.; Werhahn, S.M.; Wachter, R.; Herrmann-Lingen, C. Coping Styles as Predictors for Quality of Life and Prognosis in Patients at Risk for or with a Diagnosis of Heart Failure: Results from the Observational DIAST-CHF Study. J. Psychosom. Res. 2023, 170, 111384. [Google Scholar] [CrossRef]
- Roohafza, H.; Askari, M.; Nouri, F.; Talaei, M.; Sarrafzadegan, N.; Sadeghi, M. Do coping strategies really affect cardiovascular events? The Isfahan cohort study of adults in Eastern Mediterranean Regional Office. Eur. J. Cardiovasc. Nurs. 2022, 21, 483–490. [Google Scholar] [CrossRef]
- Rong, X.; Peng, Y.; Yu, H.; Li, D. Factors associated with adoption of coping strategies among Chinese patients with heart failure in ethnic minority regions. J. Clin. Nurs. 2018, 27, 3324–3334. [Google Scholar] [CrossRef]
- Bose, N.C.; Bjorling, G.; Elfstrom, M.L.; Persson, H.; Saboonchi, F. Assessment of Coping Strategies and Their Associations With Health Related Quality of Life in Patients with Chronic Heart Failure: The Brief COPE Restructured. Cardiol. Res. 2015, 6, 239–248. [Google Scholar] [CrossRef]
- Bahall, M.; Legall, G.; Khan, K. Quality of Life Among Patients with Cardiac Disease: The Impact of Comorbid Depression. Health Qual. Life Outcomes 2020, 18, 189. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Holland, R.; Rechel, B.; Stepien, K.; Harvey, I.; Brooksby, I. Patients’ self-assessed functional status in heart failure by New York Heart Association class: A prognostic predictor of hospitalizations, quality of life and death. J. Card. Fail. 2010, 16, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Yeh, H.F.; Shao, J.H. Quality of Life and Associated Factors in Older Adults with Heart Failure. J. Nurs. Res. 2021, 29, e166. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Katona, C.; Livingston, G. Validity and reliability of the brief COPE in carers of people with dementia: The LASER-AD Study. J. Nerv. Ment. Dis. 2008, 196, 838–843. [Google Scholar] [CrossRef]
- Coolidge, F.L.; Segal, D.L.; Hook, J.N.; Stewart, S. Personality disorders and coping among anxious older adults. J. Anxiety Disord. 2000, 14, 157–172. [Google Scholar] [CrossRef]
- Bilbao, A.; Escobar, A.; García-Perez, L.; Navarro, G.; Quirós, R. The Minnesota living with heart failure questionnaire: Comparison of different factor structures. Health Qual. Life Outcomes 2016, 14, 23. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Lindenfeld, J.; Stolfo, D.; Adams, K.; Ahmad, T.; Desai, N.R.; Ammirati, E.; Gottlieb, S.S.; Psotka, M.A.; Rosano, G.M.; et al. Use of patient-reported outcomes in heart failure: From clinical trials to routine practice. Eur. J. Heart Fail. 2023, 25, 139–151. [Google Scholar] [CrossRef]
- Donders, A.R.T.; Van Der Heijden, G.J.; Stijnen, T.; Moons, K.G. A gentle introduction to imputation of missing values. J. Clin. Epidemiol. 2006, 59, 1087–1091. [Google Scholar] [CrossRef]
- Guo, S.; Zhong, S.; Zhang, A. Privacy-preserving Kruskal–Wallis test. Comput. Methods Programs Biomed. 2013, 112, 135–145. [Google Scholar] [CrossRef]
- Pereira, D.G.; Afonso, A.; Medeiros, F.M. Overview of Friedman’s test and post-hoc analysis. Commun. Stat.-Simul. Comput. 2015, 44, 2636–2653. [Google Scholar] [CrossRef]
- Holmbeck, G.N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J. Pediatr. Psychol. 2002, 27, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Leonidou, C.; Panayiotou, G.; Bati, A.; Karekla, M. Coping with psychosomatic symptoms: The bufering role of psychological fexibility and impact on quality of life. J. Health Psychol. 2019, 24, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.; Susan, H.; Bártolo, A.; Figueiredo, D.; Ribeiro, O. Illness perception and treatment adherence in haemodialysis: A systematic review. Psychol. Health Med. 2022, 28, 1641–1655. [Google Scholar] [CrossRef] [PubMed]
- Baah, F.O.; Chittams, J.; Carlson, B.; Sethares, K.A.; Daus, M.; Moser, D.K.; Riegel, B. Sociodemographic Indictors of Social Position and Self-care Maintenance in Adults with Heart Failure. Clin. Nurs. Res. 2021, 30, 847–854. [Google Scholar] [CrossRef]
- Jackson, J.L.; Emery, C.F. Illness knowledge moderates the influence of coping style on quality of life among women with congestive heart failure. Heart Lung 2011, 40, 122–129. [Google Scholar] [CrossRef]
| Demographic Characteristics | Mean (SD) | Frequency | Percentage |
|---|---|---|---|
| Age | 37.03 ± 11.77 | ||
| Sex | |||
| Male | 62 | 57.4 | |
| Female | 46 | 42.6 | |
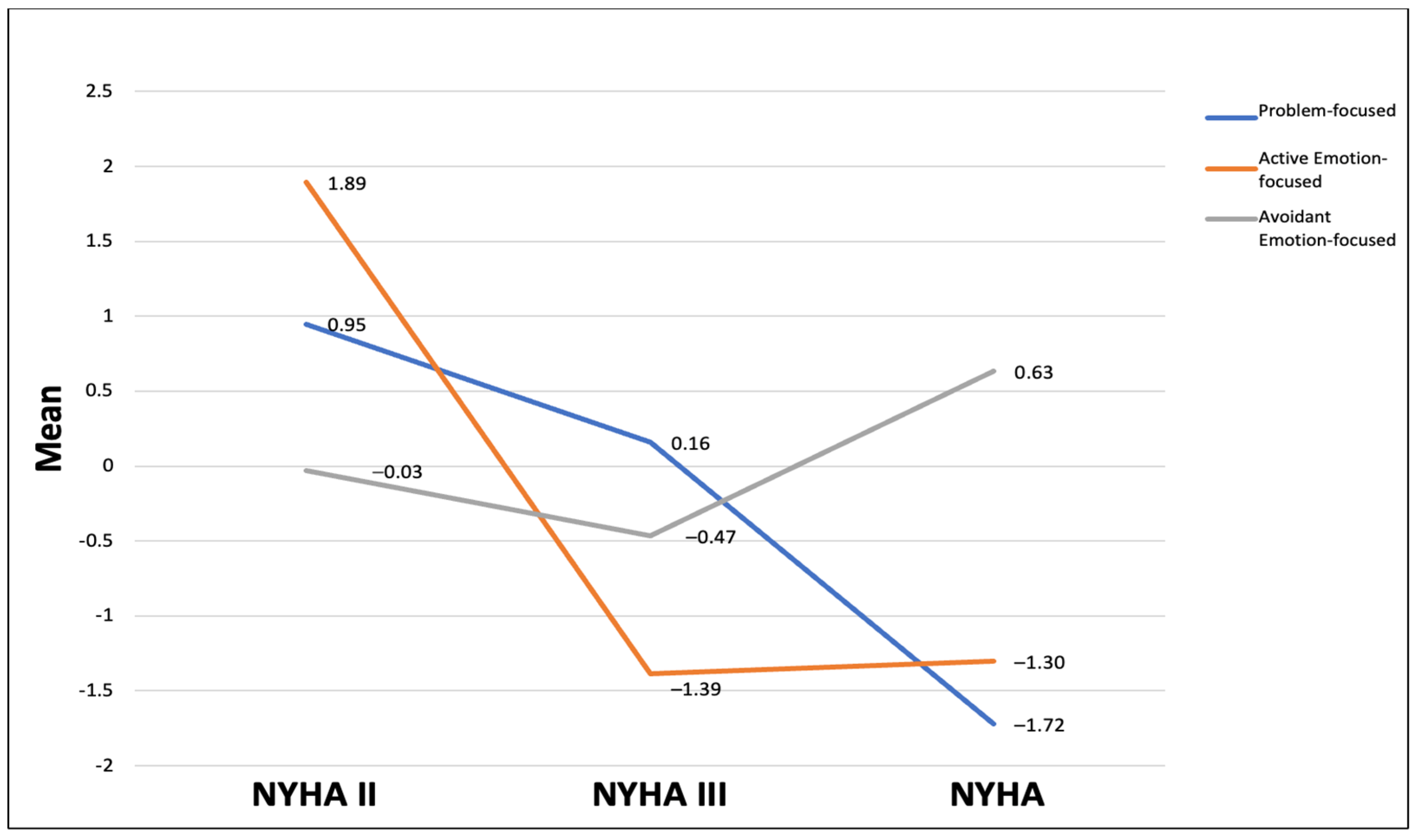
| NYHA Classification | |||
| NYHA II | 45 | 41.7 | |
| NYHA III | 35 | 32.4 | |
| NYHA IV | 28 | 25.9 | |
| Race | |||
| Black or African American | 65 | 60.2 | |
| White or Caucasian | 42 | 38.9 | |
| Hispanic or Latino | 1 | 0.9 | |
| Ethnic Background | |||
| Hispanic or Latino | 13 | 12.0 | |
| Non-Hispanic or Latino | 95 | 88.0 | |
| Living Situation | |||
| Living Alone | 15 | 13.9 | |
| Living with Spouse | 67 | 62.0 | |
| Living with Friend | 6 | 5.6 | |
| Living with Relatives | 20 | 18.5 | |
| Marital Status | |||
| Never Married | 23 | 21.3 | |
| Married or Living with Partner | 65 | 60.2 | |
| Divorced or separated | 9 | 8.3 | |
| Widowed | 11 | 10.2 | |
| Level of Education | |||
| Some grade school | 9 | 8.3 | |
| Completed grade school | 38 | 35.2 | |
| Completed high school | 16 | 14.8 | |
| Some high school | 3 | 2.8 | |
| Some college | 16 | 14.8 | |
| Completed college | 26 | 24.1 | |
| Income | |||
| Below $10,000–$20,000 | 17 | 15.7 | |
| $20,001–$30,000 | 13 | 12.0 | |
| $30,001–$60,000 | 12 | 11.1 | |
| $60,001–$100,000 | 49 | 45.4 | |
| $100,001 and above | 17 | 15.7 | |
| Employment Status | |||
| Employed Full Time | 60 | 55.6 | |
| Employed Part Time | 19 | 17.6 | |
| Unemployed | 10 | 9.3 | |
| Retired | 15 | 13.9 | |
| Full time homemaker | 4 | 3.7 |
| Characteristics | Mean (SD) | Minimum | Maximum | Range |
|---|---|---|---|---|
| Coping Strategies | ||||
| Problem-focused | 17.61 ± 4.31 | 11 | 24 | 6–24 |
| Active emotion-focused | 27.16 ± 6.58 | 14 | 40 | 10–40 |
| Avoidant emotion-focused | 25.868 ± 6.68 | 14 | 43 | 12–48 |
| HRQoL | ||||
| Physical HRQoL | 21.52 ± 6.35 | 8 | 38 | 0–40 |
| Emotional HRQoL | 13.32 ± 4.85 | 5 | 25 | 0–25 |
| HRQoL total | 34.84 ± 10.17 | 13 | 62 | 0–65 |
| HF Duration (years) | 2.95 ± 4.55 | 0 | 26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, M.O.; Deka, P.; Given, C.W.; Lehto, R.; Wyatt, G. Coping Strategies and Health-Related Quality of Life in Individuals with Heart Failure. J. Clin. Med. 2025, 14, 3073. https://doi.org/10.3390/jcm14093073
Alanazi MO, Deka P, Given CW, Lehto R, Wyatt G. Coping Strategies and Health-Related Quality of Life in Individuals with Heart Failure. Journal of Clinical Medicine. 2025; 14(9):3073. https://doi.org/10.3390/jcm14093073
Chicago/Turabian StyleAlanazi, Mohammed Owayrif, Pallav Deka, Charles W. Given, Rebecca Lehto, and Gwen Wyatt. 2025. "Coping Strategies and Health-Related Quality of Life in Individuals with Heart Failure" Journal of Clinical Medicine 14, no. 9: 3073. https://doi.org/10.3390/jcm14093073
APA StyleAlanazi, M. O., Deka, P., Given, C. W., Lehto, R., & Wyatt, G. (2025). Coping Strategies and Health-Related Quality of Life in Individuals with Heart Failure. Journal of Clinical Medicine, 14(9), 3073. https://doi.org/10.3390/jcm14093073






