Surgical Correction of Large Talar Tilt in Varus Ankle Osteoarthritis: Lessons from Clinical Experience and a Review of the Literature
Abstract
1. Introduction
2. Preoperative Considerations
2.1. Fundamental Radiographic Parameters
2.2. Definition of Large Varus Talar Tilt and Surgical Limits
2.3. Type of Varus Ankle Osteoarthritis
2.4. Radiographic Correction Goals
2.5. Age Limitation in Varus Talar Tilt Correction
3. Intraoperative Considerations: Supramalleolar Osteotomy
3.1. Osteotomy Type and Location
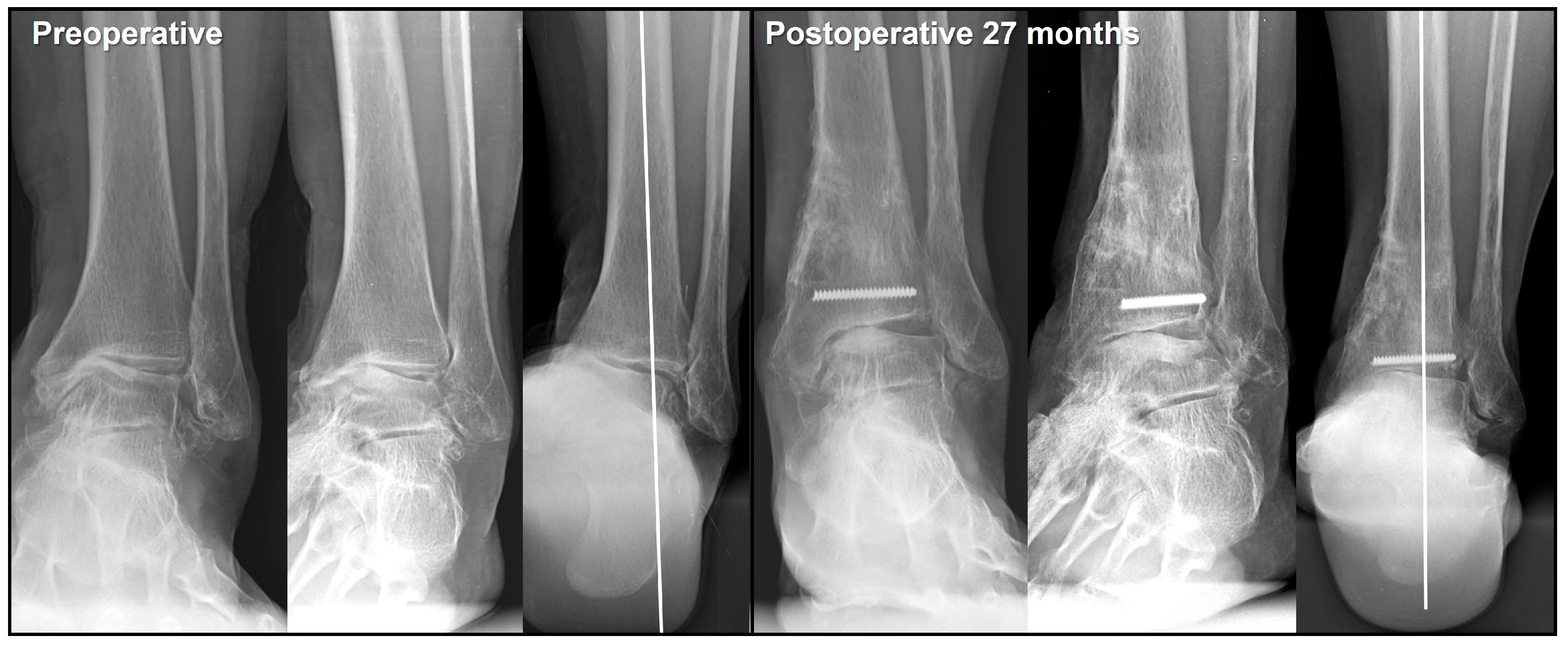
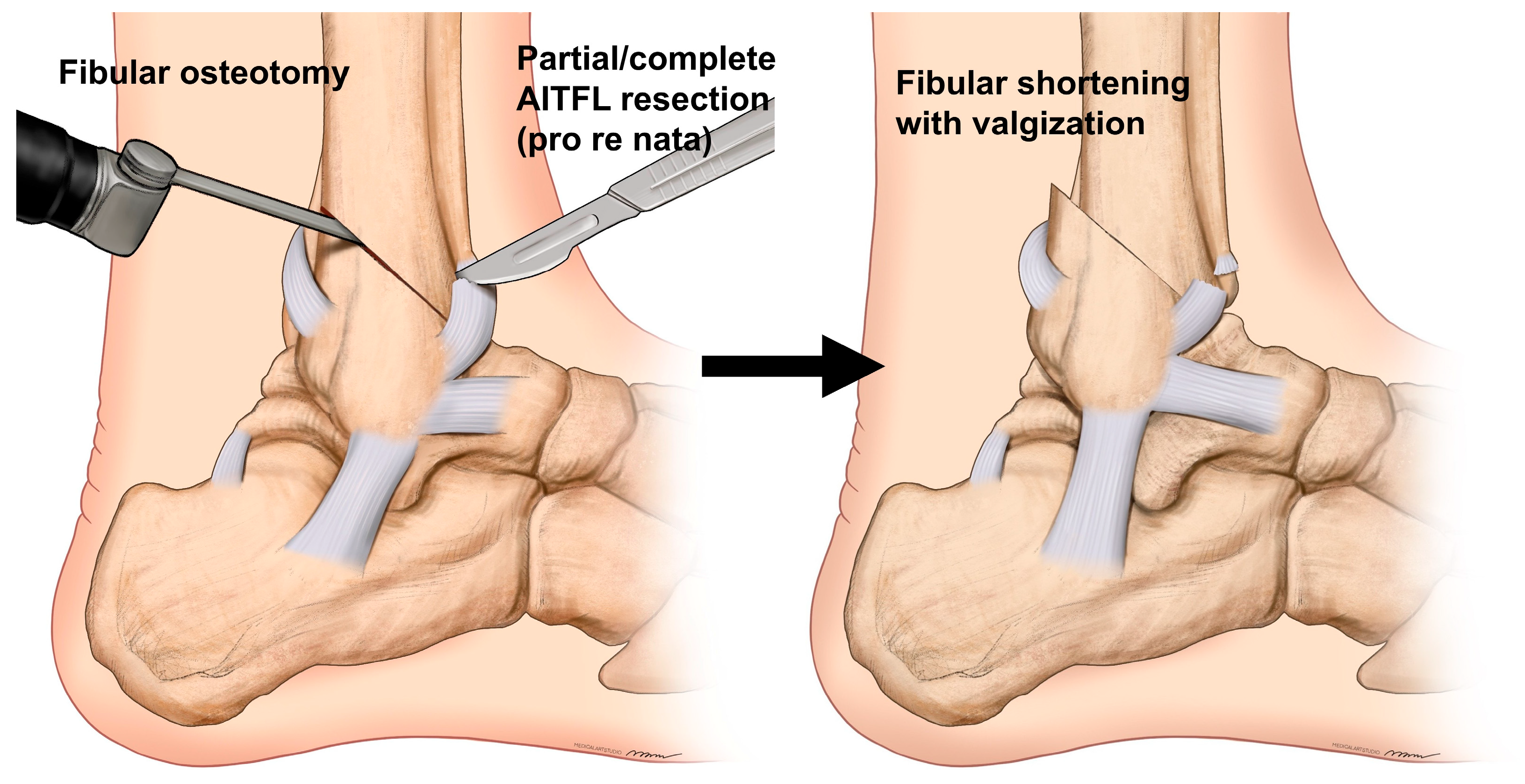
3.2. Fibular Osteotomy
3.3. Bone Marrow Stimulation of the Medial Talar Dome
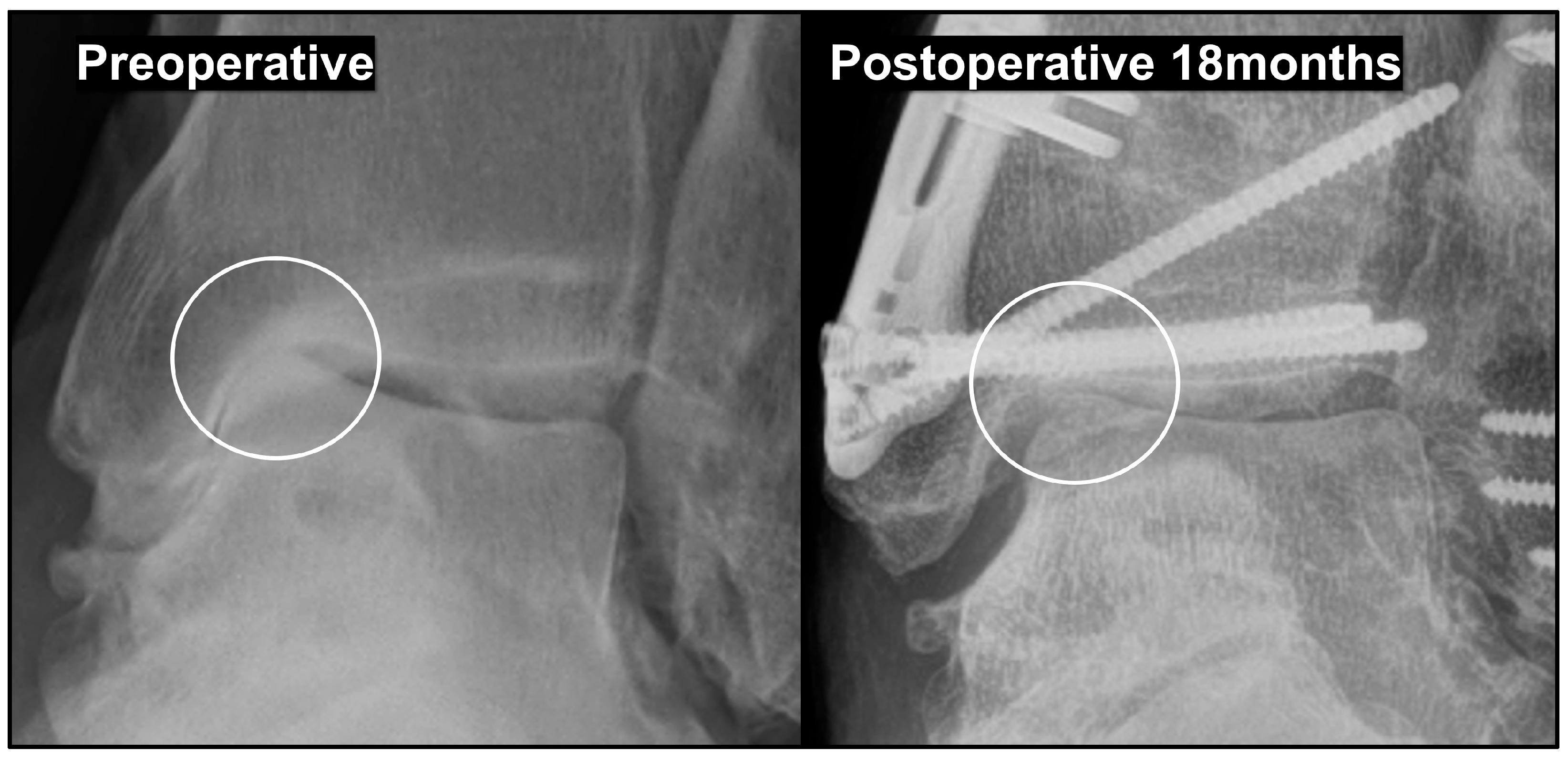
3.4. Effects and Prevention of Hinge Fracture
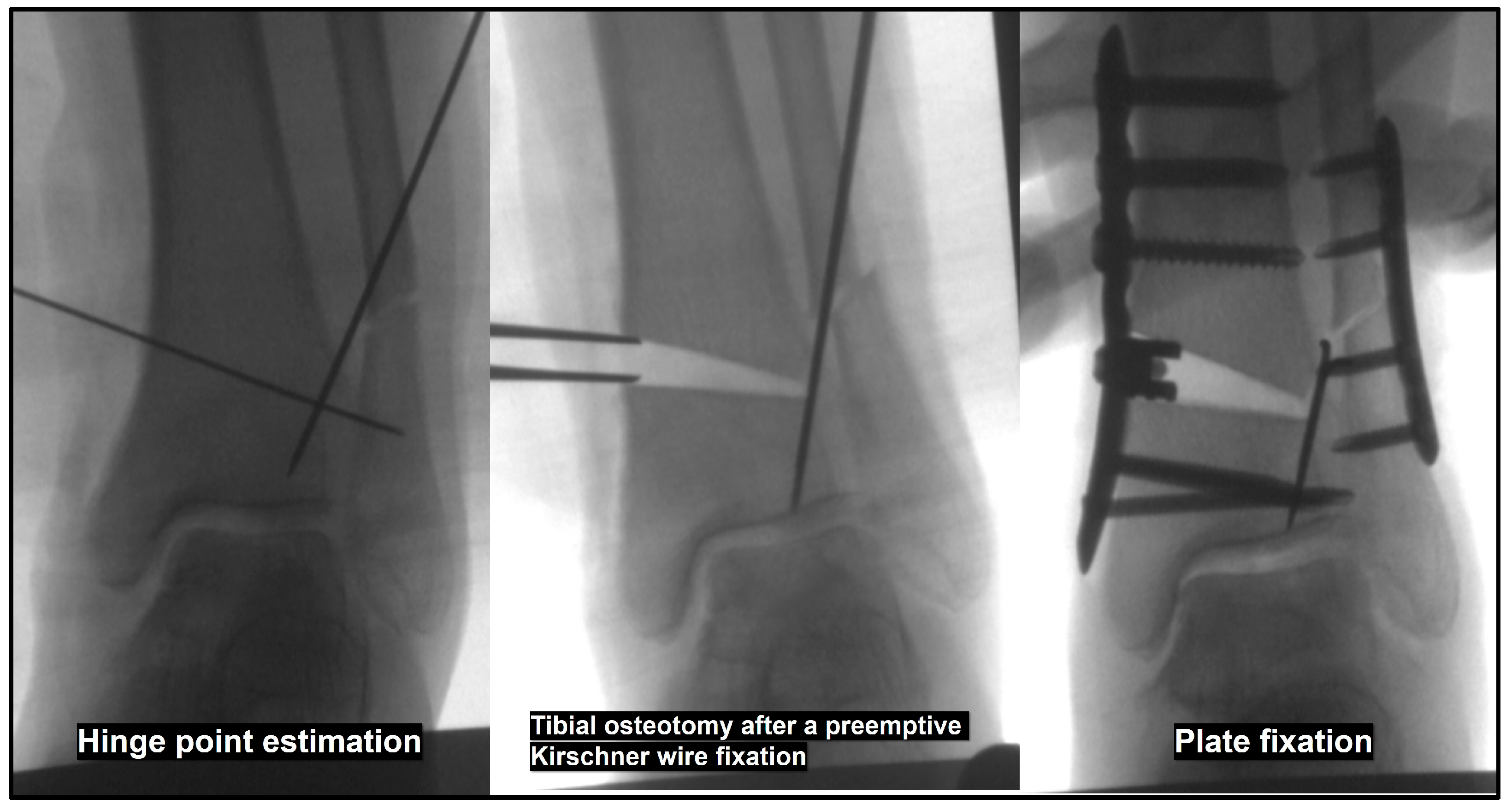
4. Intraoperative Considerations: Inframalleolar Correction
4.1. Calcaneal Osteotomy
4.2. Soft Tissue Procedure on the Medial Aspect
4.3. Soft Tissue Procedure on the Lateral Aspect
4.4. Additional Procedures
5. Surgical Sequence
- Calcaneal osteotomy and internal fixation
- Fibular osteotomy
- Preemptive Kirschner wire fixation at the anticipated tibial hinge site
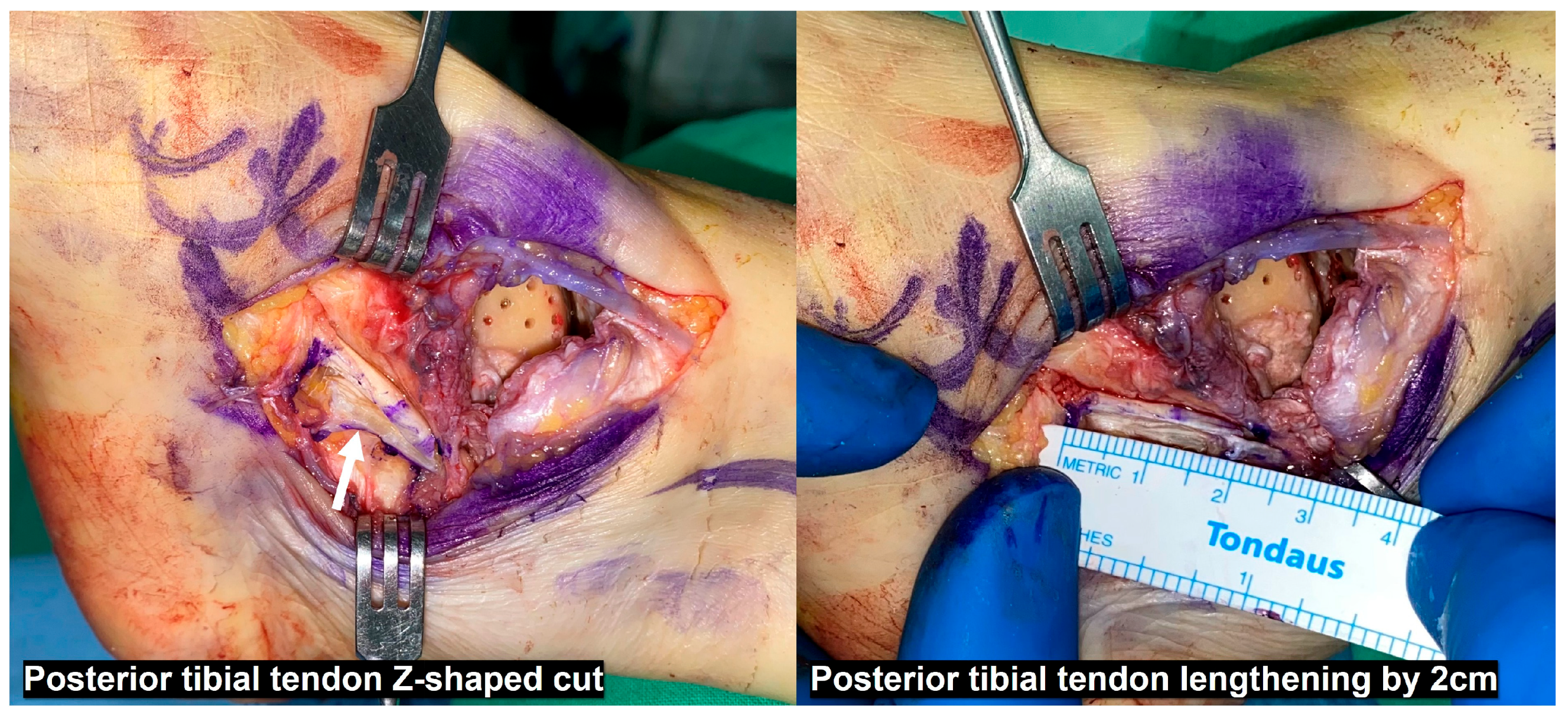
- Deltoid ligament release from the medial malleolus, multiple drilling on the medial talar dome, and PTT Z-shaped cut
- Distal syndesmotic SMO
- Opening of the tibial osteotomy site, followed by plate fixation with a metal wedge or tricortical bone graft
- Fibular fixation using two Kirschner wires
- PTT repair with lengthening
- ATFL and CFL repair or reconstruction as needed

6. Postoperative Management
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lloyd, J.; Elsayed, S.; Hariharan, K.; Tanaka, H. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int. 2006, 27, 793–796. [Google Scholar] [CrossRef] [PubMed]
- Kimizuka, M.; Kurosawa, H.; Fukubayashi, T. Load-bearing pattern of the ankle joint. Contact area and pressure distribution. Arch. Orthop. Trauma Surg. 1980, 96, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.H.; Daniels, T.R. Ankle arthritis. J. Bone Jt. Surg. Am. 2003, 85, 923–936. [Google Scholar] [CrossRef] [PubMed]
- Lacorda, J.B.; Jung, H.G.; Im, J.M. Supramalleolar distal tibiofibular osteotomy for medial ankle osteoarthritis: Current concepts. Clin. Orthop. Surg. 2020, 12, 271–278. [Google Scholar] [CrossRef]
- Barg, A.; Pagenstert, G.I.; Hügle, T.; Gloyer, M.; Wiewiorski, M.; Henninger, H.B.; Valderrabano, V. Ankle osteoarthritis: Etiology, diagnostics, and classification. Foot Ankle Clin. 2013, 18, 411–426. [Google Scholar] [CrossRef]
- Glazebrook, M.; Daniels, T.; Younger, A.; Foote, C.J.; Penner, M.; Wing, K.; Lau, J.; Leighton, R.; Dunbar, M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J. Bone Jt. Surg. Am. 2008, 90, 499–505. [Google Scholar] [CrossRef]
- Saltzman, C.L.; Salamon, M.L.; Blanchard, G.M.; Huff, T.; Hayes, A.; Buckwalter, J.A.; Amendola, A. Epidemiology of ankle arthritis: Report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop. J. 2005, 25, 44–46. [Google Scholar]
- Valderrabano, V.; Hintermann, B.; Horisberger, M.; Fung, T.S. Ligamentous posttraumatic ankle osteoarthritis. Am. J. Sports Med. 2006, 34, 612–620. [Google Scholar] [CrossRef]
- Hintermann, B.; Knupp, M.; Barg, A. Supramalleolar osteotomies for the treatment of ankle arthritis. J. Am. Acad. Orthop. Surg. 2016, 24, 424–432. [Google Scholar] [CrossRef]
- Knupp, M.; Stufkens, S.A.; Bolliger, L.; Barg, A.; Hintermann, B. Classification and treatment of supramalleolar deformities. Foot Ankle Int. 2011, 32, 1023–1031. [Google Scholar] [CrossRef]
- Takakura, Y.; Tanaka, Y.; Kumai, T.; Tamai, S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J. Bone Jt. Surg. Br. 1995, 77, 50–54. [Google Scholar] [CrossRef]
- Hintermann, B.; Ruiz, R. Joint preservation strategies for managing varus ankle deformities. Foot Ankle Clin. 2022, 27, 37–56. [Google Scholar] [CrossRef] [PubMed]
- Christidis, P.; Lampridis, V.; Kalitsis, C.; Kantas, T.; Biniaris, G.; Gougoulias, N. Supramalleolar osteotomies for ankle arthritis: A systematic review. Arch. Orthop. Trauma Surg. 2023, 143, 5549–5564. [Google Scholar] [CrossRef]
- Alajlan, A.; Santini, S.; Alsayel, F.; Teoh, K.H.; Alharbi, W.; Puls, L.; Camathias, C.; Herrera-Pérez, M.; Tejero, S.; Barg, A.; et al. Joint-Preserving Surgery in Varus Ankle Osteoarthritis. J. Clin. Med. 2022, 11, 2194. [Google Scholar] [CrossRef]
- Beijk, I.; Burgerhof, J.; de Vries, A.J.; van Raaij, T.M. Is there an optimal degree of correction for ankle varus deformity after supramalleolar osteotomy? A systematic review. Foot Ankle Surg. 2022, 28, 1139–1149. [Google Scholar] [CrossRef]
- Xue, W.; Chen, T.; Wahafu, P.; Li, F.; Xiahatai, A.; Wufuer, A.; Tuo, Y.; Zhao, B.; Wang, C. Efficacy evaluation and systematic review of supramalleolar osteotomy for treatment of varus-type ankle arthritis. J. Orthop. Surg. 2022, 30, 10225536221122286. [Google Scholar] [CrossRef]
- Kim, J.B.; Yi, Y.; Kim, J.Y.; Cho, J.H.; Kwon, M.S.; Choi, S.H.; Lee, W.C. Weight-bearing computed tomography findings in varus ankle osteoarthritis: Abnormal internal rotation of the talus in the axial plane. Skelet. Radiol. 2017, 46, 1071–1080. [Google Scholar] [CrossRef]
- Song, J.H.; Kang, C.; Kim, T.G.; Lee, G.S.; Lee, J.K.; Ahn, K.J.; Kim, D.H.; Lee, S.W. Perioperative axial loading computed tomography findings in varus ankle osteoarthritis: Effect of supramalleolar osteotomy on abnormal internal rotation of the talus. Foot Ankle Surg. 2021, 27, 217–223. [Google Scholar] [CrossRef]
- Kurokawa, H.; Taniguchi, A.; Ueno, Y.; Miyamoto, T.; Tanaka, Y. Risk factors for the progression of varus ankle osteoarthritis. Foot Ankle Orthop. 2023, 8, 24730114231178763. [Google Scholar] [CrossRef]
- Haraguchi, N.; Ota, K.; Tsunoda, N.; Seike, K.; Kanetake, Y.; Tsutaya, A. Weight-bearing-line analysis in supramalleolar osteotomy for varus-type osteoarthritis of the ankle. J. Bone Jt. Surg. Am. 2015, 97, 333–339. [Google Scholar] [CrossRef]
- Barg, A.; Bailey, T.; Richter, M.; de Cesar Netto, C.; Lintz, F.; Burssens, A.; Phisitkul, P.; Hanrahan, C.J.; Saltzman, C.L. Weightbearing computed tomography of the foot and ankle: Emerging technology topical review. Foot Ankle Int. 2018, 39, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; de Cesar Netto, C.; Lintz, F.; Barg, A.; Burssens, A.; Ellis, S. The assessment of ankle osteoarthritis with weight-bearing computed tomography. Foot Ankle Clin. 2022, 27, 13–36. [Google Scholar] [CrossRef] [PubMed]
- Faict, S.; Burssens, A.; van Oevelen, A.; Maeckelbergh, L.; Mertens, P.; Buedts, K. Correction of ankle varus deformity using patient-specific dome-shaped osteotomy guides designed on weight-bearing CT: A pilot study. Arch. Orthop. Trauma Surg. 2023, 143, 791–799. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, K.A.M.; Barbachan Mansur, N.S.; de Cesar Netto, C. Cone-beam weight-bearing computed tomography of ankle arthritis and total ankle arthroplasty. Foot Ankle Clin. 2023, 28, 509–528. [Google Scholar] [CrossRef]
- Kim, J.; Kim, J.; Kim, S.; Yi, Y. Weight-bearing CT for diseases around the ankle joint. Diagnostics 2024, 14, 1641. [Google Scholar] [CrossRef]
- Tanaka, Y. The concept of ankle joint preserving surgery: Why does supramalleolar osteotomy work and how to decide when to do an osteotomy or joint replacement. Foot Ankle Clin. 2012, 17, 545–553. [Google Scholar] [CrossRef]
- Lee, W.C.; Moon, J.S.; Lee, K.; Byun, W.J.; Lee, S.H. Indications for supramalleolar osteotomy in patients with ankle osteoarthritis and varus deformity. J. Bone Jt. Surg. Am. 2011, 93, 1243–1248. [Google Scholar] [CrossRef]
- Choi, J.Y.; Kim, K.W.; Suh, J.S. Low tibial valgization osteotomy for more severe varus ankle arthritis. Foot Ankle Int. 2020, 41, 1122–1132. [Google Scholar] [CrossRef]
- Choi, W.; Chung, C.Y.; Park, M.S.; Lee, S.; Lee, K.M. Radiographic differences in the concomitant deformities in two types of medial ankle osteoarthritis. PLoS ONE 2021, 16, e0247816. [Google Scholar] [CrossRef]
- Tanaka, Y.; Takakura, Y.; Hayashi, K.; Taniguchi, A.; Kumai, T.; Sugimoto, K. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J. Bone Jt. Surg. Br. 2006, 88, 909–913. [Google Scholar] [CrossRef]
- Choi, S.; Kim, J.; Yi, Y.; Lee, W.C. Correction target of supramalleolar osteotomy for early varus ankle arthritis: Is overcorrection necessary? Foot Ankle Int. 2025, 46, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, J.H.; Kim, B.G.; Suh, J.S. Critical factors in enhancing the correction efficacy for varus talar tilt in patients with varus ankle osteoarthritis: Relative fibular shortening to the tibia and syndesmotic widening. Arch. Orthop. Trauma Surg. 2025, 145, 156. [Google Scholar] [CrossRef]
- Choi, J.Y.; Lee, G.H.; Suh, J.S. Low tibial valgization osteotomy for varus ankle arthritis—Does age effect the outcome? Foot Ankle Surg. 2021, 27, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Harstall, R.; Lehmann, O.; Krause, F.; Weber, M. Supramalleolar lateral closing wedge osteotomy for the treatment of varus ankle arthrosis. Foot Ankle Int. 2007, 28, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Henry, J.K.; Kim, J.B.; Lee, W.C. Dome supramalleolar osteotomies for the treatment of ankle pain with opposing coronal plane deformities between ankle and the lower limb. Foot Ankle Int. 2022, 43, 474–485. [Google Scholar] [CrossRef]
- Suh, J.W.; Park, K.H.; Lee, J.W.; Han, S.H. Outcomes of oblique supramalleolar osteotomy without fibular osteotomy for congruent- and incongruent-type medial ankle arthritis. Foot Ankle Surg. 2022, 28, 603–609. [Google Scholar] [CrossRef]
- Kobayashi, H.; Kageyama, Y.; Shido, Y. Treatment of varus ankle osteoarthritis and instability with a novel mortise-plasty osteotomy procedure. J. Foot Ankle Surg. 2016, 55, 60–67. [Google Scholar] [CrossRef]
- Lee, K.B.; Cho, Y.J. Oblique supramalleolar opening wedge osteotomy without fibular osteotomy for varus deformity of the ankle. Foot Ankle Int. 2009, 30, 565–567. [Google Scholar] [CrossRef]
- Lee, W.C. Extraarticular supramalleolar osteotomy for managing varus ankle osteoarthritis, Alternatives for osteotomy: How and why? Foot Ankle Clin. 2016, 21, 27–35. [Google Scholar] [CrossRef]
- Mann, H.A.; Filippi, J.; Myerson, M.S. Intra-articular opening medial tibial wedge osteotomy (plafond-plasty) for the treatment of intra-articular varus ankle arthritis and instability. Foot Ankle Int. 2012, 33, 255–261. [Google Scholar] [CrossRef]
- Xu, Y.; Li, X.C.; Guo, C.J.; Xu, X.Y. Intra-articular opening osteotomy combined with lateral ligament reconstruction for varus ankle arthritis. J. Orthop. Surg. Res. 2021, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Zielli, S.O.; Mazzotti, A.; Artioli, E.; Marcolli, D.; Arceri, A.; Bonelli, S.; Faldini, C. Indications, associated procedures, and results of ankle plafond-plasty for varus ankle osteoarthritis: A systematic review and meta-analysis. Foot Ankle Spec. 2024, 19386400241236321, epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Nha, K.W.; Lee, S.H.; Rhyu, I.J.; Kim, H.J.; Song, J.G.; Han, J.H.; Yeo, E.D.; Lee, Y.K. Safe zone for medial open-wedge supramalleolar osteotomy of the ankle: A cadaveric study. Foot Ankle Int. 2016, 37, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Cho, J.H.; Song, T.H.; Suh, J.S. Radiographic outcomes of proximal vs distal syndesmotic low tibial osteotomy. Foot Ankle Int. 2022, 43, 211–222. [Google Scholar] [CrossRef]
- Lim, J.W.; Kang, S.J.; Im, J.M.; Kwon, S.H.; Jung, H.G. Evaluation of clinico-radiological outcome of fibular valgization osteotomy with supra-malleolar osteotomy in patients with ankle osteoarthritis. Int. Orthop. 2023, 47, 2013–2021. [Google Scholar] [CrossRef]
- Hongmou, Z.; Xiaojun, L.; Yi, L.; Hongliang, L.; Junhu, W.; Cheng, L. Supramalleolar osteotomy with or without fibular osteotomy for varus ankle arthritis. Foot Ankle Int. 2016, 37, 1001–1007. [Google Scholar] [CrossRef]
- Liang, J.Q.; Wang, J.H.; Zhang, Y.; Wen, X.D.; Liu, P.L.; Liang, X.J.; Lu, J.; Li, Y.; Zhao, H.M. Fibular osteotomy is helpful for talar reduction in the treatment of varus ankle osteoarthritis with supramalleolar osteotomy. J. Orthop. Surg. Res. 2021, 16, 575. [Google Scholar] [CrossRef]
- Zhao, H.; Liang, X.; Li, Y.; Yu, G.; Niu, W.; Zhang, Y. The role of fibular for supramalleolar osteotomy in treatment of varus ankle arthritis: A biomechanical and clinical study. J. Orthop. Surg. Res. 2016, 11, 127. [Google Scholar] [CrossRef]
- Bluman, E.M.; Chiodo, C.P. Valgus ankle deformity and arthritis. Foot Ankle Clin. 2008, 13, 443–470. [Google Scholar] [CrossRef]
- Lambert, K.L. The weight-bearing function of the fibula. A strain gauge study. J. Bone Jt. Surg. Am. 1971, 53, 507–513. [Google Scholar] [CrossRef]
- Stufkens, S.A.; van Bergen, C.J.; Blankevoort, L.; van Dijk, C.N.; Hintermann, B.; Knupp, M. The role of the fibula in varus and valgus deformity of the tibia: A biomechanical study. J. Bone Jt. Surg. Br. 2011, 93, 1232–1239. [Google Scholar] [CrossRef] [PubMed]
- Thordarson, D.B.; Motamed, S.; Hedman, T.; Ebramzadeh, E.; Bakshian, S. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J. Bone Jt. Surg. Am. 1997, 79, 1809–1815. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Whittle, M.; Cunningham, J.; Kenwright, J. Fibula and its ligaments in load transmission and ankle joint stability. Clin. Orthop. Relat. Res. 1996, 330, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Boden, S.D.; Labropoulos, P.A.; McCowin, P.; Lestini, W.F.; Hurwitz, S.R. Mechanical considerations for the syndesmosis screw. A cadaver study. J. Bone Jt. Surg. Am. 1989, 71, 1548–1555. [Google Scholar] [CrossRef]
- Kyung, M.G.; Cho, Y.J.; Lee, J.; Lee, W.; Kim, D.Y.; Lee, D.O.; Lee, D.Y. Relationship between talofibular impingement and increased talar tilt in incongruent varus ankle osteoarthritis. J. Orthop. Surg. 2021, 29, 23094990211045219. [Google Scholar] [CrossRef]
- Choi, J.Y.; Suh, J.S. Joint preserving procedures for Takakura stage IIIB varus ankle osteoarthritis. BMJ Case Rep. 2024, 17, e260585. [Google Scholar] [CrossRef]
- Kim, Y.S.; Park, E.H.; Koh, Y.G.; Lee, J.W. Supramalleolar osteotomy with bone marrow stimulation for varus ankle osteoarthritis: Clinical results and second-look arthroscopic evaluation. Am. J. Sports Med. 2014, 42, 1558–1566. [Google Scholar] [CrossRef]
- Lim, J.W.; Eom, J.S.; Kang, S.J.; Lee, D.O.; Kang, H.J.; Jung, H.G. The effect of supramalleolar osteotomy without marrow stimulation for medial ankle osteoarthritis: Second-look arthroscopic evaluation of 29 ankles. J. Bone Jt. Surg. Am. 2021, 103, 1844–1851. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, Y.B.; Koh, Y.G. Prognostic factors affecting correction angle changes after supramalleolar osteotomy using an opening wedge plate for varus ankle osteoarthritis. J. Foot Ankle Surg. 2019, 58, 417–422. [Google Scholar] [CrossRef]
- Park, Y.H.; Lee, H.J.; Choi, J.W.; Kim, H.J. Value of postoperative computed tomography for the diagnosis of lateral hinge fracture in medial opening-wedge supramalleolar osteotomy. Arch. Orthop. Trauma Surg. 2023, 143, 1379–1385. [Google Scholar] [CrossRef]
- Choi, J.Y.; Suh, J.S.; Song, T.H. Protective Kirschner wire fixation to reduce the effect of lateral hinge fracture during the medial opening wedge low tibial osteotomy: A technical note. Tech. Orthop. 2024, 39, 17–19. [Google Scholar] [CrossRef]
- Burssens, A.; Devos Bevernage, B.; Buedts, K. Supramalleolar osteotomies in cavovarus foot deformity: Why patient-specific instruments make a difference. Foot Ankle Clin. 2023, 28, 843–856. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Wapner, K.L.; Park, S.S.; Kim, J.S.; Lee, D.H.; Sohn, D.W. Ligament reconstruction and calcaneal osteotomy for osteoarthritis of the ankle. Foot Ankle Int. 2009, 30, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, F.C. Osteotomy of the calcaneum for pes cavus. J. Bone Jt. Surg. Br. 1959, 41, 80–86. [Google Scholar] [CrossRef]
- Knupp, M.; Horisberger, M.; Hintermann, B. A new Z-shaped calcaneal osteotomy for 3-plane correction of severe varus deformity of the hindfoot. Tech. Foot Ankle Surg. 2008, 7, 90–95. [Google Scholar] [CrossRef]
- Duff, J.R.; Sarfani, S.; Ward, T.; Doty, J.F.; Murphy, G. Deltoid ligament release for varus deformity correction in total ankle arthroplasty. Foot Ankle Orthop. 2023, 8, 2473011423S00278. [Google Scholar] [CrossRef]
- Willegger, M.; Seyidova, N.; Schuh, R.; Windhager, R.; Hirtler, L. The tibialis posterior tendon footprint: An anatomical dissection study. J. Foot Ankle Res. 2020, 13, 25. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, J.B.; Kim, J.; Yi, Y.; Lee, W.C. Joint preservation surgery for varus ankle arthritis with large talar tilt. Foot Ankle Int. 2021, 42, 1554–1564. [Google Scholar] [CrossRef]
- Park, C.H.; Park, J.J.; Woo, I.H. Joint preservation surgery using supramalleolar osteotomy combined with posterior tibial tendon release and lateral ligament augmentation in advanced varus ankle arthritis. J. Clin. Med. 2024, 13, 4803. [Google Scholar] [CrossRef]
- Qu, W.; Xin, D.; Dong, S.; Li, W.; Zheng, Y. Supramalleolar osteotomy combined with lateral ligament reconstruction and talofibular immobilization for varus ankle osteoarthritis with excessive talar tilt angle. J. Orthop. Surg. Res. 2019, 14, 402. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, J.; Kim, J.B.; Lee, W.C. Repositional subtalar arthrodesis combined with supramalleolar osteotomy for late-stage varus ankle arthritis with hindfoot valgus. Foot Ankle Int. 2022, 43, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.M.; Wen, X.D.; Zhang, Y.; Liang, J.Q.; Liu, P.L.; Li, Y.; Lu, J.; Liang, X.J. Supramalleolar osteotomy with medial distraction arthroplasty for ankle osteoarthritis with talar tilt. J. Orthop. Surg. Res. 2019, 14, 120. [Google Scholar] [CrossRef] [PubMed]
- Nozaka, K.; Miyakoshi, N.; Kashiwagura, T.; Kasukawa, Y.; Saito, H.; Kijima, H.; Chida, S.; Tsuchie, H.; Shimada, Y. Effectiveness of distal tibial osteotomy with distraction arthroplasty in varus ankle osteoarthritis. BMC Musculoskelet. Disord. 2020, 21, 31. [Google Scholar] [CrossRef]


| Parameters | Clinical Implications | Reference Range |
|---|---|---|
| TAS | A quantitative measure of correction | 88–93° |
| TT | Aim of correction | ≤4° |
| TMMA | A quantitative measure of medial malleolar erosion | 20–25° |
| TCA | Relative fibular length measurement | 8–15° |
| TPI | Tibial plafond coronal alignment relative to the ground (a supplementary aim of correction) | N/A |
| TLS | Sagittal alignment parameter of the distal fragment after correction (anterior/posterior angulation) | 79–83° |
| HMA | A parameter assessing hindfoot alignment | Neutral alignment when the tibial bisecting line intersects the lowest point of the calcaneus |
| HAR | A parameter assessing hindfoot alignment | 0.3–0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.Y.; Suh, J.S. Surgical Correction of Large Talar Tilt in Varus Ankle Osteoarthritis: Lessons from Clinical Experience and a Review of the Literature. J. Clin. Med. 2025, 14, 2781. https://doi.org/10.3390/jcm14082781
Choi JY, Suh JS. Surgical Correction of Large Talar Tilt in Varus Ankle Osteoarthritis: Lessons from Clinical Experience and a Review of the Literature. Journal of Clinical Medicine. 2025; 14(8):2781. https://doi.org/10.3390/jcm14082781
Chicago/Turabian StyleChoi, Jun Young, and Jin Soo Suh. 2025. "Surgical Correction of Large Talar Tilt in Varus Ankle Osteoarthritis: Lessons from Clinical Experience and a Review of the Literature" Journal of Clinical Medicine 14, no. 8: 2781. https://doi.org/10.3390/jcm14082781
APA StyleChoi, J. Y., & Suh, J. S. (2025). Surgical Correction of Large Talar Tilt in Varus Ankle Osteoarthritis: Lessons from Clinical Experience and a Review of the Literature. Journal of Clinical Medicine, 14(8), 2781. https://doi.org/10.3390/jcm14082781







