Current Concepts of Radiographic Evaluation and Surgical Treatment for Hallux Valgus Deformity
Abstract
1. Introduction
2. Radiographic Evaluation of Hallux Valgus
2.1. X-Ray
2.2. Weight-Bearing Computed Tomography
3. Operative Treatment of Hallux Valgus
3.1. Open Surgery
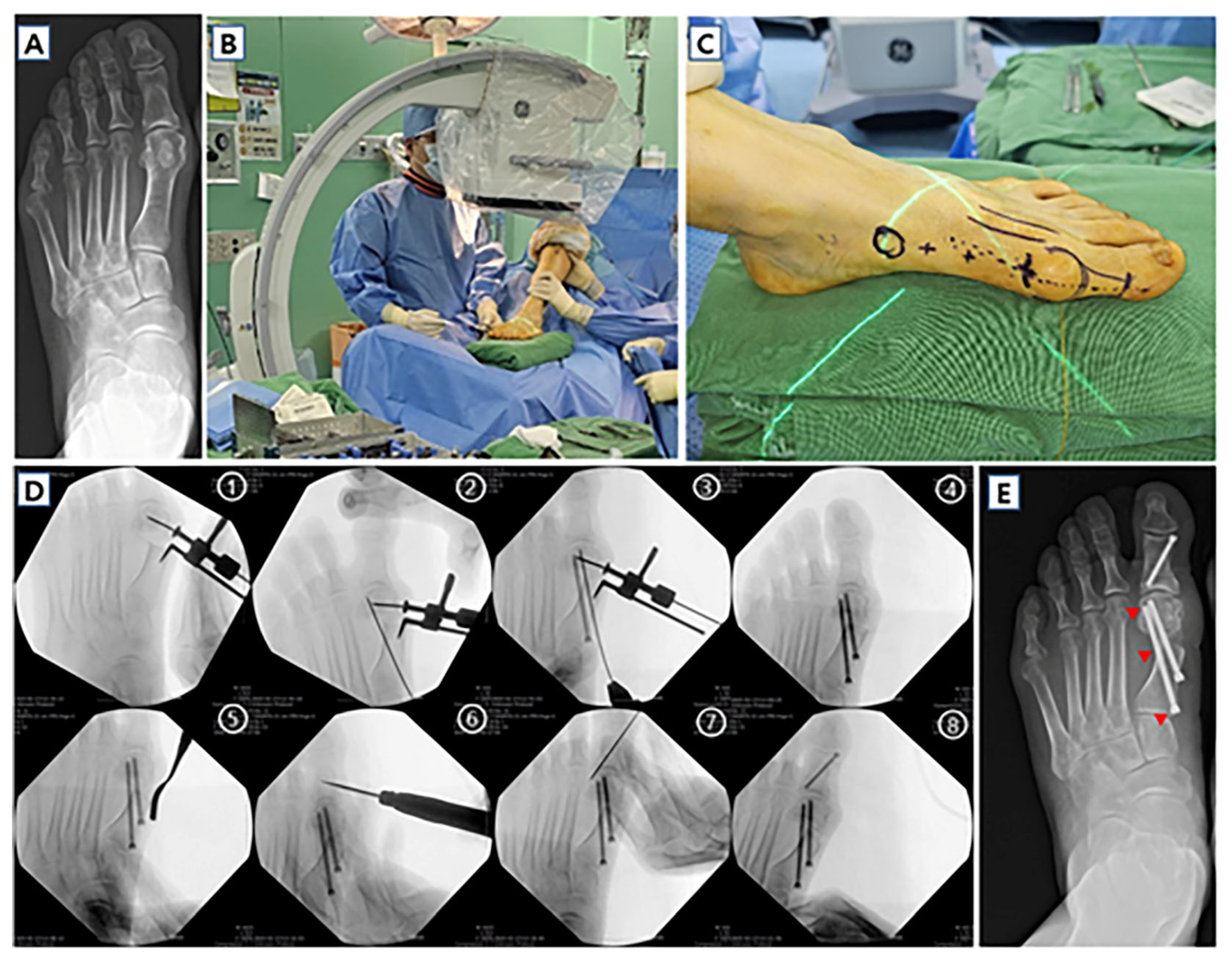
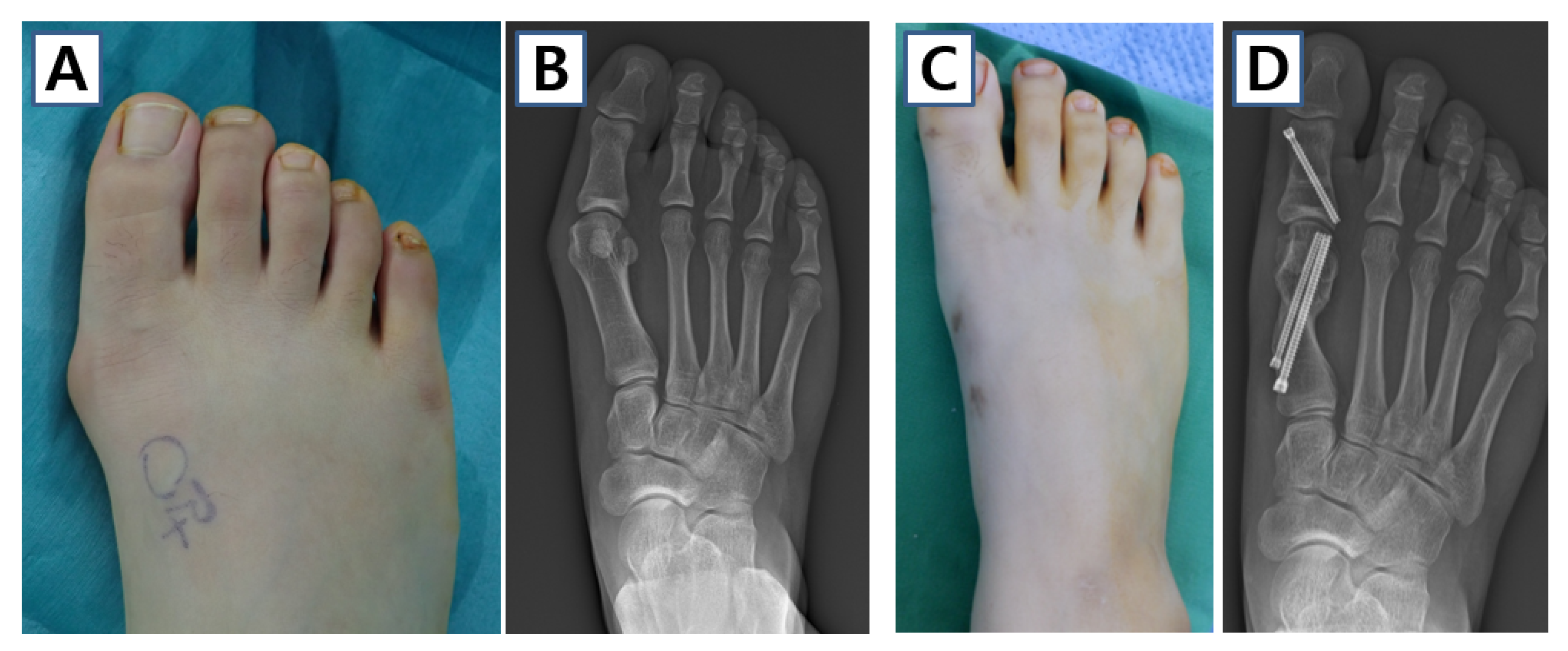
3.2. Minimally Invasive Surgery
3.3. Prognosis of Surgery
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Coughlin, M.J.; Jones, C.P. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007, 28, 759–777. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, K.A.; Fayed, A.; Barbachan, N.S.; Godoy-Santos, A.L.; Talusan, P.; Chrea, B.; de Cesar Netto, C.; Johnson, A.H.; Dalmau-Pastor, M. Anatomical and Micro-CT Assessment of the First Metatarsal Head Vascularization and Soft Tissue Envelope Following Minimally Invasive Chevron Osteotomy for Hallux Valgus Deformity. Foot Ankle Int. 2025, 46, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kang, C.; Hwang, D.S.; Lee, G.S.; Lee, S.B. Comparison of radiographic and clinical results after extended distal chevron osteotomy with distal soft tissue release with moderate versus severe hallux valgus. Foot Ankle Int. 2019, 40, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Easley, M.E.; Trnka, H.-J. Current concepts review: Hallux valgus part 1: Pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007, 28, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Easley, M.E.; Trnka, H.-J. Current concepts review: Hallux valgus part II: Operative treatment. Foot Ankle Int. 2007, 28, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Deenik, A.; van Mameren, H.; de Visser, E.; de Waal Malefijt, M.; Draijer, F.; de Bie, R. Equivalent correction in scarf and chevron osteotomy in moderate and severe hallux valgus: A randomized controlled trial. Foot Ankle Int. 2008, 29, 1209–1215. [Google Scholar] [CrossRef] [PubMed]
- Mahadevan, D.; Lines, S.; Hepple, S.; Winson, I.; Harries, W. Extended plantar limb (modified) chevron osteotomy versus scarf osteotomy for hallux valgus correction: A randomised controlled trial. Foot Ankle Surg. 2016, 22, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Braito, M.; Dammerer, D.; Hofer-Picout, P.; Kaufmann, G. Proximal opening wedge osteotomy with distal chevron osteotomy of the first metatarsal for the treatment of moderate to severe hallux valgus. Foot Ankle Int. 2019, 40, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Glazebrook, M.; Copithorne, P.; Boyd, G.; Daniels, T.; Lalonde, K.-A.; Francis, P.; Hickey, M. Proximal opening wedge osteotomy with wedge-plate fixation compared with proximal chevron osteotomy for the treatment of hallux valgus: A prospective, randomized study. J. Bone Jt. Surg. Am. 2014, 96, 1585–1592. [Google Scholar] [CrossRef] [PubMed]
- Thordarson, D.B.; Leventen, E.O. Hallux valgus correction with proximal metatarsal osteotomy: Two-year follow-up. Foot Ankle Int. 1992, 13, 321–326. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, K.A.M.; Baptista, A.D.; de Cesar Netto, C.; Johnson, A.H.; Dalmau-Pastor, M. Minimally invasive chevron-Akin for correction of moderate and severe hallux valgus deformities: Clinical and radiologic outcomes with a minimum 2-year follow-up. Foot Ankle Int. 2022, 43, 1317–1330. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.K.; Tang, Z.H.; Shim, D.W.; Rhyu, H.J.; Han, S.H.; Lee, J.W.; Park, K.H. Minimally invasive transverse distal metatarsal osteotomy (MITO) for hallux valgus correction: Early outcomes of mild to moderate vs. severe deformities. Foot Ankle Int. 2023, 44, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Lau, B.; Alkhalfan, Y.; Trowbridge, S.; Gordon, D.; Vernois, J.; Lam, P.; Ray, R. Fourth-generation minimally invasive hallux valgus surgery with metaphyseal extra-articular transverse and akin osteotomy (META): 12 month clinical and radiologic results. Foot Ankle Int. 2023, 44, 178–191. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Robinson, P.W.; Ray, R.; Dearden, P.M.; Goff, T.A.; Watt, C.; Lam, P. Five-year follow-up of third-generation percutaneous chevron and Akin osteotomies (PECA) for hallux valgus. Foot Ankle Int. 2023, 44, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Hochheuser, G. Complications of Minimally Invasive Surgery for Hallux Valgus and How to Deal with Them. Foot Ankle Clin. 2020, 25, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Crespo, R.E.; Peñuela, C.R.; Gómez, G.S.; Arias, A.A.; Arcas, O.A.; Gálvez, G.J.; Crespo, R.R. Percutaneous forefoot surgery for treatment of hallux valgus deformity: An intermediate prospective study. Musculoskelet. Surg. 2017, 101, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.J.; Friedmann, A.J.; Hanselman, A.E.; Vaida, J.; Dayton, P.D.; Hatch, D.J.; Smith, B.; Santrock, R.D. Hallux valgus. Foot Ankle Orthop. 2019, 4, 2473011419838500. [Google Scholar] [CrossRef] [PubMed]
- Hardy, R.H.; Clapham, J.C. Observations on hallux valgus. J. Bone Jt. Surg. Br. 1951, 33, 376–391. [Google Scholar] [CrossRef] [PubMed]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J. Bone Jt. Surg. Am. 2007, 89, 2163–2172. [Google Scholar] [CrossRef]
- Collan, L.; Kankare, J.A.; Mattila, K. The biomechanics of the first metatarsal bone in hallux valgus: A preliminary study utilizing a weight bearing extremity CT. Foot Ankle Surg. 2013, 19, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Kubota, M.; Suzuki, N.; Hattori, A.; Saito, M. Weightbearing computed tomography and 3-dimensional analysis of mobility changes of the first ray after proximal oblique osteotomy for hallux valgus. Foot Ankle Int. 2021, 42, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Kubota, M.; Taguchi, T.; Suzuki, N.; Hattori, A.; Marumo, K. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system: A comparison with normal feet. J. Bone Jt. Surg. Am. 2017, 99, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Barg, A.; Bailey, T.; Richter, M.; de Cesar Netto, C.; Lintz, F.; Burssens, A.; Phisitkul, P.; Hanrahan, C.J.; Saltzman, C.L. Weightbearing computed tomography of the foot and ankle: Emerging technology topical review. Foot Ankle Int. 2018, 39, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.H.; Kang, C.; Hwang, D.S.; Song, J.H.; Song, S.H. The value of axial loading three dimensional (3D) CT as a substitute for full weightbearing (standing) 3D CT: Comparison of reproducibility according to degree of load. Foot Ankle Surg. 2019, 25, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kim, J.S.; Young, K.W.; Naraghi, R.; Cho, H.K.; Lee, S.Y. A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int. 2015, 36, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Mansur, N.S.B.; Lalevee, M.; Schmidt, E.; Dibbern, K.; Wagner, P.; Wagner, E.; de Souza Nery, C.A.; de Cesar Netto, C. Correlation between indirect radiographic parameters of first metatarsal rotation in hallux valgus and values on weight-bearing computed tomography. Int. Orthop. 2021, 45, 3111–3118. [Google Scholar] [CrossRef] [PubMed]
- Lalevée, M.; Barbachan Mansur, N.S.; Lee, H.Y.; Maly, C.J.; Iehl, C.J.; Nery, C.; Lintz, F.; de Cesar Netto, C.J.F. Distal metatarsal articular angle in hallux valgus deformity. Fact or fiction? A 3-dimensional weightbearing CT assessment. Foot Ankle Int. 2022, 43, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Chun, D.I.; Cho, J.; Won, S.H.; Nomkhondorj, O.; Kim, J.; An, C.Y.; Yi, Y.J.D. Weight-Bearing CT: Advancing the Diagnosis and Treatment of Hallux Valgus, Midfoot Pathology, and Progressive Collapsing Foot Deformity. Diagnostics 2025, 15, 343. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-S.; Huánuco Casas, E.J.; Luo, E.J.; Acker, A.S.; Easley, M.E.; de Cesar Netto, C.J.F. A Comprehensive Weightbearing Computed Tomography Study on Patients With Hallux Valgus: Exploring Multiplanar Deformity Interrelationships. Foot Ankle Int. 2025, 46, 10711007241309912. [Google Scholar] [CrossRef] [PubMed]
- Park, H.W.; Lee, K.B.; Chung, J.Y. Comparison of outcomes between proximal and distal chevron osteotomy, both with supplementary lateral soft-tissue release, for severe hallux valgus deformity: A prospective randomised controlled trial. Bone Jt. J. 2013, 95, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Jeuken, R.M.; Schotanus, M.G.; Kort, N.P.; Deenik, A.; Jong, B.; Hendrickx, R.P. Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int. 2016, 37, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Al Hussainy, H.; Ali, F.; Betts, R.P.; Flowers, M.J. Scarf osteotomy for hallux valgus: A prospective clinical and pedobarographic study. J. Bone Jt. Surg. Br. 2004, 86, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Badwey, T.M.; Dutkowsky, J.P.; Graves, S.C.; Richardson, E.G. An anatomical basis for the degree of displacement of the distal chevron osteotomy in the treatment of hallux valgus. Foot Ankle Int. 1997, 18, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Edwards, W.H. Avascular necrosis of the first metatarsal head. Foot Ankle Clin. 2005, 10, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.; Limbers, J. Modern concepts in the treatment of hallux valgus. J. Bone Jt. Surg. Br. 2005, 87, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, J.C. Scarf osteotomy for hallux valgus repair: The dark side. Foot Ankle Int. 2003, 24, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, R.E.; Saltzman, C.L.; Kile, T.A.; Johnson, K.A. Modified chevron osteotomy for hallux valgus. Foot Ankle Int. 1994, 15, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Lee, H.S.; Choi, Y.R. Relationship between proximal to distal phalangeal articular angle and Hallux Pronation in Hallux Valgus deformity. Sci. Rep. 2025, 15, 92. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.; Kim, Y.M. Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision. J. Bone Jt. Surg. Am. 2007, 89, 82–89. [Google Scholar]
- Easley, M.E.; Kiebzak, G.M.; Davis, W.H.; Anderson, R.B. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996, 17, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.T.; Berlet, G.C.; Shurnas, P.S.; Lee, T.H. Proximal opening-wedge osteotomy of the first metatarsal for correction of hallux valgus. Surg. Technol. Int. 2007, 16, 215–219. [Google Scholar] [PubMed]
- Shurnas, P.S.; Watson, T.S.; Crislip, T.W. Proximal first metatarsal opening wedge osteotomy with a low profile plate. Foot Ankle Int. 2009, 30, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Park, E.H.; Jo, J.; Koh, Y.G.; Lee, J.W.; Choi, W.J.; Kim, Y.S. First metatarsal proximal opening wedge osteotomy for correction of hallux valgus deformity: Comparison of straight versus oblique osteotomy. Yonsei Med. J. 2015, 56, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.; Demetracopoulos, C.A.; Sofka, C.M.; Ellis, S.J. High rate of recurrence following proximal medial opening wedge osteotomy for correction of moderate hallux valgus. Foot Ankle Int. 2015, 36, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Badekas, A.; Georgiannos, D.; Lampridis, V.; Bisbinas, I.J. Proximal opening wedge metatarsal osteotomy for correction of moderate to severe hallux valgus deformity using a locking plate. Int. Orthop. 2013, 37, 1765–1770. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kang, C.; Park, W.H.; Lee, G.S.; Lee, J.K.; Kim, D.H.; Lee, S.W. Extended distal Chevron osteotomy and Akin osteotomy using bioabsorbable materials for treatment of moderate to severe hallux valgus. J. Foot Ankle Surg. 2021, 60, 1110–1116. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Park, K.H.; Jo, J.; Lee, M.; Lee, J.W.; Kim, H.J.; Shin, G.J.; Choi, G.W. Percutaneous distal chevron osteotomy is associated with lower immediate postoperative pain and a greater range of motion than the open technique: A prospective randomized study. Int. Orthop. 2024, 48, 2383–2394. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Park, C.H. Minimally invasive forefoot surgeries using the Shannon burr: A comprehensive review. Diagnostics 2024, 14, 1896. [Google Scholar] [CrossRef] [PubMed]
- Isham, S.A. The Reverdin-lsham Procedure for the Correction of Hallux Abducto Valgus: A Distal Metatarsal Osteotomy Procedure. Clin. Podiatr. Med. Surg. 1991, 8, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Bösch, P.; Wanke, S.; Legenstein, R. Hallux valgus correction by the method of Bösch: A new technique with a seven-to-ten-year follow-up. Foot Ankle Clin. 2000, 5, 485–498. [Google Scholar] [PubMed]
- Frigg, A.; Zaugg, S.; Maquieira, G.; Pellegrino, A. Stiffness and range of motion after minimally invasive chevron-akin and open scarf-akin procedures. Foot Ankle Int. 2019, 40, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Kadakia, A.R.; Smerek, J.P.; Myerson, M.S. Radiographic results after percutaneous distal metatarsal osteotomy for correction of hallux valgus deformity. Foot Ankle Int. 2007, 28, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Walsh, J.; Smith, M.M.; Ling, J.; Wines, A.; Lam, P. Hallux valgus correction comparing percutaneous chevron/akin (PECA) and open scarf/akin osteotomies. Foot Ankle Int. 2017, 38, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, G.; Mörtlbauer, L.; Hofer-Picout, P.; Dammerer, D.; Ban, M.; Liebensteiner, M. Five-year follow-up of minimally invasive distal metatarsal chevron osteotomy in comparison with the open technique: A randomized controlled trial. J. Bone Jt. Surg. Am. 2020, 102, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Aiyer, A.; Massel, D.H.; Siddiqui, N.; Acevedo, J.I. Biomechanical comparison of 2 common techniques of minimally invasive hallux valgus correction. Foot Ankle Int. 2021, 42, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, B.H.; Suh, J.S. A prospective study to compare the operative outcomes of minimally invasive proximal and distal chevron metatarsal osteotomy for moderate-to-severe hallux valgus deformity. Int. Orthop. 2021, 45, 2933–2943. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Song, T.H.; Suh, J.S. Outcome comparison of minimally invasive proximal and distal chevron Akin osteotomies in patients with severe hallux valgus deformity: A randomized prospective study. Int. Orthop. 2024, 48, 2153–2163. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.S.; Khurana, A.; Kapoor, D.; Katekar, S.; Kumar, A.; Vishwakarma, G. Minimally invasive vs. open distal metatarsal osteotomy for hallux valgus-a systematic review and meta-analysis. J. Clin. Orthop. Trauma 2020, 11, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Kafagi, A.-H.; Kafagi, A.-R.; Tahoun, M.; Al Zareeni, O.T.; El Aloul, K.; Ahmad, M.U.; Pillai, A. Comparative Outcomes of Minimally Invasive Versus Open Hallux Valgus Surgery: A Systematic Review and Meta-Analysis. Osteology 2025, 5, 3. [Google Scholar] [CrossRef]
- Del Vecchio, J.J.; Ghioldi, M.E.; Uzair, A.E.; Chemes, L.N.; Manzanares-Céspedes, M.C.; Dealbera, E.D.; Dalmau-Pastor, M. Percutaneous, intra-articular, chevron osteotomy (PeICO) for the treatment of hallux valgus: A cadaveric study. Foot Ankle Int. 2019, 40, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, J.L.; Golanó, P.; Roshan-Zamir, S.; Darcel, V.; Chauveaux, D.; Laffenêtre, O. Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L Chevron (PERC) osteotomy. Bone Jt. J. 2016, 98, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Dalmau-Pastor, M.; Malagelada, F.; Cordier, G.; Del Vecchio, J.J.; Ghioldi, M.E.; Vega, J. Anatomical study of minimally invasive lateral release techniques for hallux valgus treatment. Foot Ankle Int. 2020, 41, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Corradin, M.; Petretta, I.; Aldegheri, R. Endolog technique for correction of hallux valgus: A prospective study of 30 patients with 4-year follow-up. J. Orthop. Surg. Res. 2015, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Izzo, A.; Vallefuoco, S.; Basso, M.A.; Ray, R.; Smeraglia, F.; Cozzolino, A.; Mariconda, M.; Bernasconi, A. Role of lateral soft tissue release in percutaneous hallux valgus surgery: A systematic review and meta-analysis of the literature. Arch. Orthop. Trauma Surg. 2023, 143, 3997–4007. [Google Scholar] [CrossRef] [PubMed]
- Goh, G.S.; Tay, A.Y.; Thever, Y.; Koo, K. Effect of age on clinical and radiological outcomes of hallux valgus surgery. Foot Ankle Int. 2021, 42, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Choi, Y.R.; Lee, H.S.; Bak, G.G.; Moon, S.H. Relationship between Hallux Valgus recurrence and sesamoid position on Anteroposterior standing radiographs after distal Chevron Metatarsal Osteotomy. Foot Ankle Int. 2023, 44, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Lee, W.-C. Recurrence of hallux valgus can be predicted from immediate postoperative non-weight-bearing radiographs. J. Bone Jt. Surg. Am. 2017, 99, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J. Bone Jt. Surg. Am. 2009, 91, 1637–1645. [Google Scholar] [CrossRef] [PubMed]
- Ezzatvar, Y.; López-Bueno, L.; Fuentes-Aparicio, L.; Dueñas, L. Prevalence and predisposing factors for recurrence after hallux valgus surgery: A systematic review and meta-analysis. J. Clin. Med. 2021, 10, 5753. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.K.; Park, J.K.; Choi, S.M.; SooHoo, N.F. Is generalized ligamentous laxity a prognostic factor for recurred hallux valgus deformity? Foot Ankle Int. 2019, 25, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.M.; Lee, J.S.; Lim, J.W.; Im, J.M.; Kho, D.H.; Jung, H.G. Effect of metatarsus adductus on hallux valgus treated with proximal reverse chevron metatarsal osteotomy. Foot Ankle Int. 2021, 42, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Heyes, G.J.; Vosoughi, A.R.; Weigelt, L.; Mason, L.; Molloy, A. Pes planus deformity and its association with hallux valgus recurrence following scarf osteotomy. Foot Ankle Int. 2020, 41, 1212–1218. [Google Scholar] [CrossRef] [PubMed]
- Saur, M.; Lucas, y.; Hernandez, J.; Barouk, P.; Bejarano-Pineda, L.; Maynou, C.; Laffenetre, O. Average 4-year outcomes of distal oblique first metatarsal osteotomy for stage 1 to 3 hallux rigidus. Foot Ankle Int. 2022, 43, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, A.; Ikari, K.; Yamada, A.; Yano, K.; Okazaki, K. Outcomes of Joint-Preserving Surgery for Forefoot Deformities in Patients with Rheumatoid Arthritis. Foot Ankle Int. 2024, 45, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Jones, C.P. Hallux valgus and first ray mobility: A prospective study. J. Bone Jt. Surg. Am. 2007, 89, 1887–1898. [Google Scholar] [CrossRef]







| Surgical Method | Advantages | Disadvantages | Indications |
|---|---|---|---|
| Distal Chevron Osteotomy | Familiar technique; effective for mild-to-moderate deformities; structurally stable with V-shaped cut. | Limited correction of pronation; risk of osteonecrosis; less translation capacity. | Mild-to-moderate hallux valgus without significant pronation or instability. |
| Proximal Chevron Osteotomy | Provides greater correction; suitable for severe deformities; relatively simple fixation. | Higher complication rate; longer rehabilitation; risk of dorsal angulation and transfer metatarsalgia. | Severe hallux valgus needing substantial angular correction. |
| Proximal Medial Opening Wedge Osteotomy | Allows precise angular correction; good for moderate-to-severe deformities; compatible with locking plates. | Risk of instability and recurrence; technically demanding; longer learning curve. | Moderate-to-severe hallux valgus with need for precise correction; useful with locking plate systems. |
| Minimally Invasive Chevron Akin Osteotomy | Smaller incision; faster recovery; better range of motion; stable fixation with chevron geometry. | Potential for screw irritation; limited ability to correct large deformities; requires specialized equipment. | Mild-to-moderate hallux valgus; when faster recovery and cosmetic outcomes are desired. |
| Minimally Invasive Transverse Distal Metatarsal Osteotomy | Superior translational and rotational control; effective for pronation correction; good for compromised skin condition. | Higher screw irritation risk; technical challenges; risk of thermal injury and nerve damage. | Moderate-to-severe hallux valgus with pronation; cases requiring minimal soft tissue trauma. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, B.K.; Kang, D.H.; Kang, C.; Lee, G.S.; Song, J.H. Current Concepts of Radiographic Evaluation and Surgical Treatment for Hallux Valgus Deformity. J. Clin. Med. 2025, 14, 5072. https://doi.org/10.3390/jcm14145072
Cho BK, Kang DH, Kang C, Lee GS, Song JH. Current Concepts of Radiographic Evaluation and Surgical Treatment for Hallux Valgus Deformity. Journal of Clinical Medicine. 2025; 14(14):5072. https://doi.org/10.3390/jcm14145072
Chicago/Turabian StyleCho, Byung Ki, Dong Hun Kang, Chan Kang, Gi Soo Lee, and Jae Hwang Song. 2025. "Current Concepts of Radiographic Evaluation and Surgical Treatment for Hallux Valgus Deformity" Journal of Clinical Medicine 14, no. 14: 5072. https://doi.org/10.3390/jcm14145072
APA StyleCho, B. K., Kang, D. H., Kang, C., Lee, G. S., & Song, J. H. (2025). Current Concepts of Radiographic Evaluation and Surgical Treatment for Hallux Valgus Deformity. Journal of Clinical Medicine, 14(14), 5072. https://doi.org/10.3390/jcm14145072






