Assessment of Quality of Life of Children and Adolescents with Type 1 Diabetes in Bahrain Using PedsQL 3.2 Diabetes Module
Abstract
1. Introduction
2. Methods
2.1. Participants
- n = required sample size;
- Z = Z-value (1.96 for a 95% confidence level);
- p = estimated proportion of the population (assumed to be 0.5 for maximum variability);
- E = margin of error (0.05).
2.2. Demographic and Diabetes-Related Information Questionnaire
2.3. Data Collection
2.4. Measures
3. Data Analysis
4. Results
5. Discussion
6. Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hilliard, M.E.; Minard, C.G.; Marrero, D.G.; de Wit, M.; Thompson, D.; DuBose, S.N.; Verdejo, A.; Monzavi, R.; Wadwa, R.P.; Jaser, S.S.; et al. Assessing Health-Related Quality of Life in Children and Adolescents with Diabetes: Development and Psychometrics of the Type 1 Diabetes and Life (T1DAL) Measures. J. Pediatr. Psychol. 2020, 45, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Murillo, M.; Bel, J.; Perez, J.; Corripio, R.; Carreras, G.; Herrero, X.; Mengibar, J.M.; Rodriguez-Arjona, D.; Ravens-Sieberer, U.; Raat, H.; et al. Health-related quality of life (HRQOL) and its associated factors in children with Type 1 Diabetes Mellitus (T1DM). BMC Pediatr. 2017, 17, 16. [Google Scholar] [CrossRef]
- Bekele, B.T.; Demie, T.G.; Worku, F. Health-Related Quality-of-Life and Associated Factors Among Children and Adolescents with Type 1 Diabetes Mellitus: A Cross-Sectional Study. Pediatric. Health Med. Ther. 2022, 13, 243–256. [Google Scholar] [CrossRef] [PubMed]
- Streisand, R.; Monaghan, M. Young children with type 1 diabetes: Challenges, research, and future directions. Curr. Diab. Rep. 2014, 14, 520. [Google Scholar] [CrossRef]
- Al-Agha, A.E.; Alafif, M.M.; Abd-Elhameed, I.A. Glycemic control, complications, and associated autoimmune diseases in children and adolescents with type 1 diabetes in Jeddah, Saudi Arabia. Saudi Med. J. 2015, 36, 26–31. [Google Scholar] [CrossRef]
- Ausili, E.; Tabacco, F.; Focarelli, B.; Padua, L.; Crea, F.; Caliandro, P.; Pazzaglia, C.; Marietti, G.; Rendeli, C. Multidimensional study on quality of life in children with type 1 diabetes. Eur. Rev. Med. Pharmacol. Sci. 2007, 11, 249–255. [Google Scholar]
- Fayyaz, F.; Aghamahdi, F.; Noorian, S.; Tabatabaei-Malazy, O.; Qorbani, M. Associated factors to insulin adherence in type 1 diabetes in Tehran and Karaj, Iran. J. Diabetes Metab. Disord. 2022, 21, 1591–1597. [Google Scholar] [CrossRef]
- Gomes, M.B.; Negrato, C.A. Adherence to insulin therapeutic regimens in patients with type 1 diabetes. A nationwide survey in Brazil. Diabetes Res. Clin. Pract. 2016, 120, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Al-Qerem, W.; Jarab, A.; Hammad, A.; Eberhardt, J.; Alasmari, F.; Alkaee, S.M.; Alsabaa, Z.H.; Al-Ibadah, M. The association between health literacy and quality of life of patients with type 2 diabetes mellitus: A cross-sectional study. PLoS ONE 2024, 19, e0312833. [Google Scholar] [CrossRef]
- Alhaddad, J.A.; Alshakes, N.A.; Aljasim, M.N. Quality of Life Among Children with Type 1 Diabetes Mellitus in Alahsa: A Cross-Sectional Study. Cureus 2023, 15, e40766. [Google Scholar] [CrossRef]
- Pintus, D.; Ng, S.M. Freestyle libre flash glucose monitoring improves patient quality of life measures in children with Type 1 diabetes mellitus (T1DM) with appropriate provision of education and support by healthcare professionals. Diabetes Metab. Syndr. 2019, 13, 2923–2926. [Google Scholar] [CrossRef] [PubMed]
- Ministy of Health Bahrain. Diabetes. Available online: https://www.moh.gov.bh/Services/Diabetes?lang=en (accessed on 23 December 2024).
- International Diabtes Federation. Bahrain Diabetes Report 2000–2045. Available online: https://www.diabetesatlas.org/data/en/country/15/bh.html (accessed on 23 December 2023).
- Yoldi-Vergara, C.; Conget-Donlo, I.; Cardona-Hernandez, R.; Ramon-Krauel, M. Influence of socioeconomic factors on glycemic control, therapeutic adherence and quality of life in children and adolescents with type 1 diabetes. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2024, 71, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Delamater, A.M.; Hood, K.K.; Raymond, J.K.; Chang, N.T.; Driscoll, K.A.; Wong, J.C.; Yi-Frazier, J.P.; Grishman, E.K.; Faith, M.A.; et al. PedsQL 3.2 Diabetes Module for Children, Adolescents, and Young Adults: Reliability and Validity in Type 1 Diabetes. Diabetes Care 2018, 41, 2064–2071. [Google Scholar] [CrossRef] [PubMed]
- Majedah, A.-R.; AlOtaibi, F.; AlMahdi, M.; AlKandari, K. Reliability and validity of the Arabic version of the PedsQLTM 4.0 generic ore scales and PedsQLTM 3.0 diabetes module. J. Diabetes Mellit. 2012, 2, 301–307. [Google Scholar]
- Nakamura, N.; Sasaki, N.; Kida, K.; Matsuura, N.; Study Group of Health Sciences, R. Health-related and diabetes-related quality of life in Japanese children and adolescents with type 1 and type 2 diabetes. Pediatr. Int. 2010, 52, 224–229. [Google Scholar] [CrossRef]
- Lukacs, A.; Varga, B.; Kiss-Toth, E.; Soos, A.; Barkai, L. Factors influencing the diabetes-specific health-related quality of life in children and adolescents with type 1 diabetes mellitus. J. Child. Health Care 2014, 18, 253–260. [Google Scholar] [CrossRef]
- Lafontaine, S.; Mok, E.; Frei, J.; Henderson, M.; Rahme, E.; Dasgupta, K.; Nakhla, M. Associations of Diabetes-related and Health-related Quality of Life with Glycemic Levels in Adolescents with Type 1 Diabetes Preparing to Transition to Adult Care. Can. J. Diabetes 2023, 47, 525–531. [Google Scholar] [CrossRef]
- Alshammari, F.; Ansari, M.; Khan, K.U.; Neupane, D.; Hussain, A.; Anwar, S.; Alshammari, B.; Alrasheeday, A.; Jamshed, S.; Sapkota, B.; et al. Health-related quality of life among people with diabetes: A cross-sectional study in Hail region, Saudi Arabia. PLoS ONE 2024, 19, e0299995. [Google Scholar] [CrossRef]
- Alfaleh, A.; Alkattan, A.; Alzaher, A.; Alhabib, D.; Alshatri, A.; Alnamshan, A.; Almalki, O.; Almutairi, L.; Khairat, M.; Sagor, K.; et al. Quality of life among schoolchildren with type 1 diabetes mellitus and the satisfaction of their guardians towards school health care in Saudi Arabia. Diabetes Res. Clin. Pract. 2023, 204, 110901. [Google Scholar] [CrossRef]
- Wilson, V. Barriers to effective communication between patients using insulin pump therapy technology to enable intensive diabetes self-management and the health professionals providing their diabetes care. J. Assist. Technol. 2008, 2, 26–33. [Google Scholar] [CrossRef]
- Ghazanfar, H.; Rizvi, S.W.; Khurram, A.; Orooj, F.; Qaiser, I. Impact of insulin pump on quality of life of diabetic patients. Indian J. Endocrinol. Metab. 2016, 20, 506–511. [Google Scholar] [CrossRef]
- Lasaite, L.; Dobrovolskiene, R.; Danyte, E.; Stankute, I.; Razanskaite-Virbickiene, D.; Schwitzgebel, V.; Marciulionyte, D.; Verkauskiene, R. Diabetes distress in males and females with type 1 diabetes in adolescence and emerging adulthood. J. Diabetes Complicat. 2016, 30, 1500–1505. [Google Scholar] [CrossRef]
- Galler, A.; Tittel, S.R.; Baumeister, H.; Reinauer, C.; Brosig, B.; Becker, M.; Haberland, H.; Hilgard, D.; Jivan, M.; Mirza, J.; et al. Worse glycemic control, higher rates of diabetic ketoacidosis, and more hospitalizations in children, adolescents, and young adults with type 1 diabetes and anxiety disorders. Pediatr. Diabetes 2021, 22, 519–528. [Google Scholar] [CrossRef]
- Yilmaz Karaman, I.G.; Altinoz, A.E.; Aydin Buyruk, B.; Yorulmaz, G.; Kosger, F.; Kirel, B. Comparison of anxiety, stress, and social support levels of female patients with type 1 diabetes and mothers whose children have type 1 diabetes. J. Diabetes Metab. Disord. 2023, 22, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Wang, Y.; Cai, X.; Li, R.; Li, M.; Liu, H.; Xu, J. Resilience Among Parents of Adolescents With Type 1 Diabetes: Associated With Fewer Parental Depressive Symptoms and Better Pediatric Glycemic Control. Front. Psychiatry 2022, 13, 834398. [Google Scholar] [CrossRef] [PubMed]
- Samardzic, M.; Tahirovic, H.; Popovic, N.; Popovic-Samardzic, M. Health-related quality of life in children and adolescents with type 1 diabetes mellitus from Montenegro: Relationship to metabolic control. J. Pediatr. Endocrinol. Metab. 2016, 29, 663–668. [Google Scholar] [CrossRef]
- Levesque, A.R.; MacDonald, S.; Berg, S.A.; Reka, R. Assessing the Impact of Changes in Household Socioeconomic Status on the Health of Children and Adolescents: A Systematic Review. Adolesc. Res. Rev. 2021, 6, 91–123. [Google Scholar] [CrossRef] [PubMed]
- Rohilla, L.; Gujjar, N.; Kaur, G.; Walia, P.; Dayal, D. Financial burden for families of children with type 1 diabetes: A cross-sectional survey from North India. Diabetol. Int. 2022, 13, 665–671. [Google Scholar] [CrossRef]
- Bittner, J.M.P.; Gilman, S.E.; Zhang, C.; Chen, Z.; Cheon, B.K. Relationships between early-life family poverty and relative socioeconomic status with gestational diabetes, preeclampsia, and hypertensive disorders of pregnancy later in life. Ann. Epidemiol. 2023, 86, 8–15. [Google Scholar] [CrossRef]
- Ozguven Oztornaci, B.; Ardahan Akgul, E.; Yanar, N.; Akyol, S.; Yetim, P.; Bas, G.; Yildirim Sari, H.; Dundar, B.N. The Effect of Parental Collaboration on Diabetes Self-Efficacy, Quality of Life and HbA1c Level in Adolescents Diagnosed with Type 1 Diabetes. J. Clin. Res. Pediatr. Endocrinol. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Alsahli, M.A.; Alalwan, A.; Aburisheh, K.H.; Alarifi, F.F.; Alshaya, H.M.; Alkholaif, A.F.; Shadid, A.M.; Alsahli, S.A.; Alsahly, A.A.; Alkhalifah, M.K. Assessing satisfaction, quality of life, and HbA1c changes in type 1 diabetes patients who are using freestyle libre glucose monitoring. J. Fam. Med. Prim. Care 2024, 13, 2367–2374. [Google Scholar] [CrossRef]
- Alipour, A.; Zare, H.; Poursharifi, H.; Aerab Sheibani, K.; Ardekani, M.A. The intermediary role of self-efficacy in relation with stress, glycosylated haemoglobin and health-related quality of life in patients with type2 diabetes. Iran J. Public Health 2012, 41, 76–80. [Google Scholar] [PubMed]
- Oakley, N.J.; Kneale, D.; Mann, M.; Hilliar, M.; Dayan, C.; Gregory, J.W.; French, R. Type 1 diabetes mellitus and educational attainment in childhood: A systematic review. BMJ Open 2020, 10, e033215. [Google Scholar] [CrossRef] [PubMed]
- Martens, T.; Beck, R.W.; Bailey, R.; Ruedy, K.J.; Calhoun, P.; Peters, A.L.; Pop-Busui, R.; Philis-Tsimikas, A.; Bao, S.; Umpierrez, G.; et al. Effect of Continuous Glucose Monitoring on Glycemic Control in Patients With Type 2 Diabetes Treated With Basal Insulin: A Randomized Clinical Trial. JAMA 2021, 325, 2262–2272. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | % |
|---|---|---|
| Age (mean ± SD) | 12.21 ± 2.86 | |
| Age group | ||
| 6–8 | 24 | 13.2 |
| 9–12 | 67 | 36.8 |
| 13–16 | 91 | 50.0 |
| Age at diagnosis (mean ± SD) | 6.83 ± 3.11 | |
| Age at diagnosis | ||
| 1–2 years | 15 | 8.2 |
| 2–5 years | 48 | 26.4 |
| 6–11 years | 105 | 57.7 |
| 12–16 years | 14 | 7.7 |
| Sex | ||
| Male | 95 | 52.2 |
| Female | 87 | 47.8 |
| BMI (mean ± SD) | 21.89 ± 6.90 | |
| BMI | ||
| <18.5 | 58 | 31.9 |
| 18.5–24.99 | 89 | 48.9 |
| 25–29.99 | 20 | 11.0 |
| ≥30 | 15 | 8.2 |
| Family’s income | ||
| <500 | 44 | 24.2 |
| 500–1000 | 90 | 49.5 |
| >1000 | 48 | 26.4 |
| School | ||
| Primary | 52 | 28.6 |
| Secondary | 130 | 71.4 |
| Child’s school performance | ||
| Poor | 5 | 2.7 |
| Good | 24 | 13.2 |
| Very good | 47 | 25.8 |
| Excellent | 106 | 58.2 |
| HbA1c group | ||
| ≤7.5 | 44 | 24.2 |
| >7.5 | 138 | 75.8 |
| Type of glucometer | ||
| Standard glucose meter | 114 | 62.6 |
| Continuous glucose monitor | 68 | 37.4 |
| What type of insulin regimens is the patient in? | ||
| Subcutaneous | 83 | 45.6 |
| Pump | 99 | 54.4 |
| Do you have any chronic disease or mental illness? | ||
| Yes | 17 | 9.3 |
| No | 165 | 90.7 |
| Number of emergency department visits in 2023 | ||
| 0 | 98 | 53.8 |
| 1–2 | 65 | 35.7 |
| >2 | 19 | 10.4 |
| Number of diabetic ketoacidosis in 2023 | ||
| 0 | 110 | 60.4 |
| 1–2 | 58 | 31.9 |
| >2 | 14 | 7.7 |
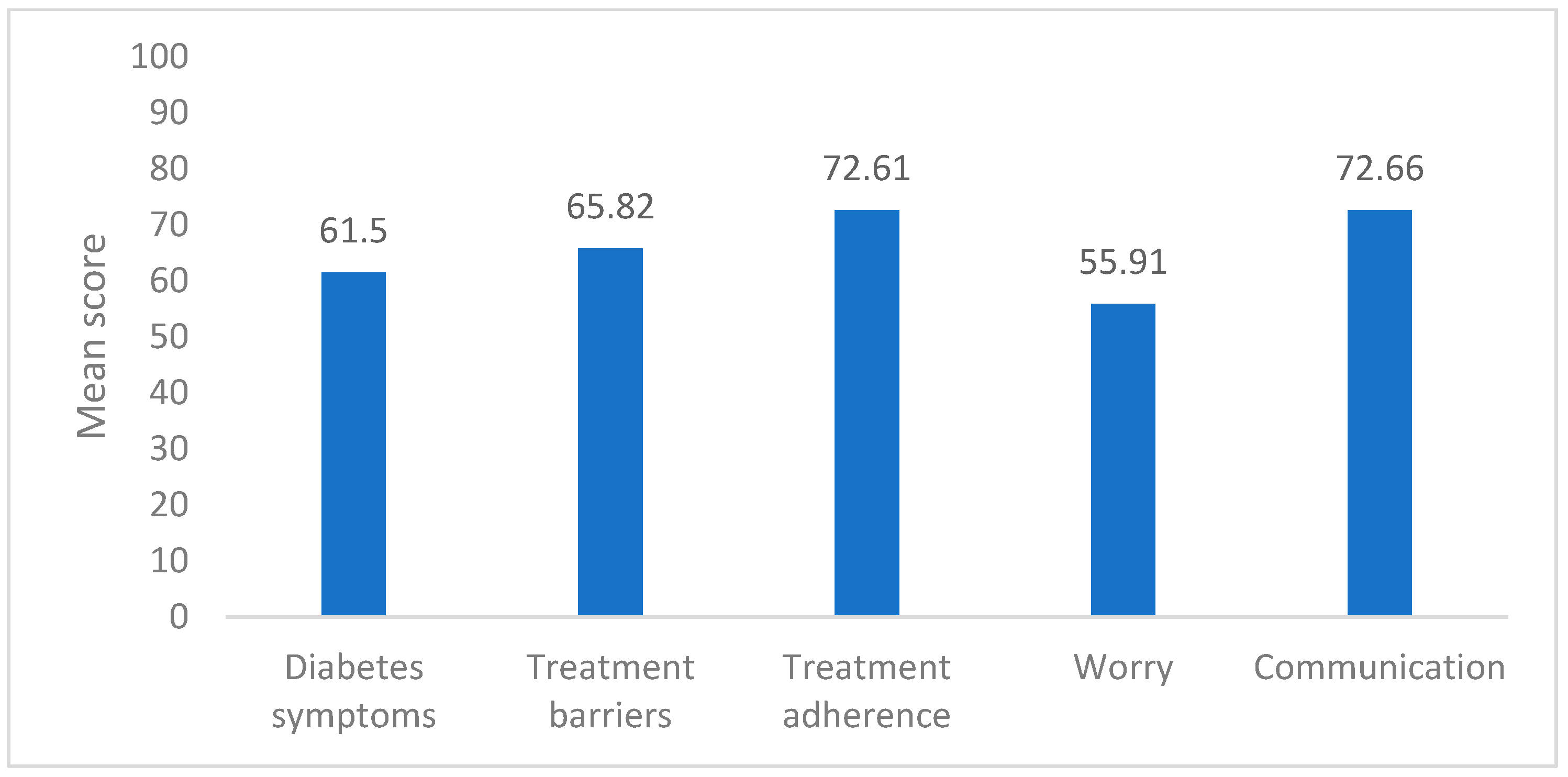
| Domain | Mean ± SD | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|
| Diabetes symptoms | 61.50 ± 14.10 | 61.67 (51.67, 71.67) | 20.0 | 98.33 |
| Treatment barriers | 65.82 ± 19.89 | 67.50 (50.0, 80.0) | 20.0 | 100.0 |
| Treatment adherence | 72.61 ± 23.92 | 80.0 (60.0, 91.25) | 5.0 | 100.0 |
| Worry | 55.91 ± 28.85 | 58.33 (39.58, 75.0) | 0 | 100.0 |
| Communication | 72.66 ± 23.11 | 75.0 (56.25, 93.75) | 6.25 | 100.0 |
| Variables | Diabetes Symptoms Mean ± SD | p-Value | Treatment Barriers Median (IQR) | p-Value | Treatment Adherence Median (IQR) | p-Value |
|---|---|---|---|---|---|---|
| Age group | ||||||
| 6–8 | 64.31 ± 13.25 | 0.546 * | 57.50 (45.0, 73.75) | <0.001 # | 50.0 (35.0, 70.0) | <0.001 # |
| 9–12 | 61.54 ± 14.57 | 65.0 (50.0, 70.0) | 70.0 (55.0, 85.0) | |||
| 13–16 | 60.73 ± 14.03 | 70.0 (60.0, 85.0) | 85.0 (70.0, 100.0) | |||
| Age at diagnosis | ||||||
| 1–2 years | 58.44 ± 18.12 | 0.759 * | 60.0 (45.0, 85.0) | 0.655 # | 70.0 (50.0, 83.33) | <0.001 # |
| 2–5 years | 60.80 ± 14.13 | 67.50 (45.0, 80.0) | 65.0 (36.25, 88.75) | |||
| 6–11 years | 62.32 ± 13.66 | 70.0 (55.0, 80.0) | 80.0 (65.0, 95.0) | |||
| 12–16 years | 61.07 ± 13.50 | 67.50 (60.0, 90.0) | 95.0 (82.5, 100.0) | |||
| Sex | ||||||
| Male | 61.54 ± 13.83 | 0.967 ^ | 65.0 (50.0, 80.0) | 0.508 @ | 85.0 (60.0, 95.0) | 0.013 @ |
| Female | 61.46 ± 14.48 | 70.0 (50.0, 80.0) | 70.0 (55.0, 85.0) | |||
| BMI | ||||||
| <18.5 | 59.28 ± 14.71 | 0.547 * | 65.0 (48.75, 75.0) | 0.398 # | 70.0 (83.75, 91.25) | 0.036 # |
| 18.5–24.99 | 62.40 ± 13.62 | 70.0 (57.50, 80.0) | 80.0 (65.0, 95.0) | |||
| 25–29.99 | 62.92 ± 14.20 | 70.0 (51.25, 80.0) | 80.0 (41.25, 90.0) | |||
| ≥30 | 62.89 ± 14.86 | 60.0 (45.0, 85.0) | 60.0 (25.0, 90.0) | |||
| Family’s income | ||||||
| <500 | 56.97 ± 14.26 | 0.009 * | 65.0 (40.0, 75.0) | 0.076 # | 85.0 (45.0, 100.0) | 0.071 # |
| 500–1000 | 64.54 ± 14.21 | 70.0 (50.0, 80.0) | 80.0 (63.75, 91.25) | |||
| >1000 | 59.97 ± 12.58 | 70.0 (56.25, 80.0) | 70.0 (60.0, 80.0) | |||
| School | ||||||
| Primary | 61.70 ± 14.53 | 0.906 ^ | 57.50 (45.0, 73.75) | 0.001 @ | 62.50 (45.0, 85.0) | <0.001 @ |
| Secondary | 61.42 ± 13.99 | 70.0 (60.0, 80.0) | 80.0 (65.0, 95.0) | |||
| Child’s school performance | ||||||
| Poor | 41.33 ± 16.35 | <0.001 * | 60.0 (52.50, 72.50) | 0.787 # | 70.0 (35.0, 92.50) | 0.905 # |
| Good | 58.89 ± 9.16 | 67.50 (50.0, 80.0) | 75.0 (55.0, 93.75) | |||
| Very good | 58.37 ± 13.79 | 65.0 (45.0, 75.0) | 80.0 (55.0, 95.0) | |||
| Excellent | 64.43 ± 14.04 | 70.0 (50.0, 80.0) | 80.0 (60.0, 91.25) | |||
| HbA1c group | ||||||
| ≤7.5 | 67.31 ± 14.69 | 0.002 ^ | 70.0 (60.0, 78.75) | 0.412 @ | 70.0 (52.50, 93.75) | 0.439 @ |
| >7.5 | 59.64 ± 13.45 | 65.0 (48.75, 80.0) | 80.0 (60.0, 91.25) | |||
| Type of glucometer | ||||||
| Standard | 62.31 ± 14.12 | 0.318 ^ | 65.0 (45.0, 75.0) | 0.029 @ | 80.0 (58.75, 90.0) | 0.163 @ |
| Continuous | 60.15 ± 14.07 | 70.0 (60.0, 80.0) | 80.0 (60.0, 100.0) | |||
| What type of insulin regimens is the patient in? | ||||||
| Subcutaneous | 62.29 ± 14.11 | 0.492 ^ | 60.0 (45.0, 70.0) | <0.001 | 80.0 (50.0, 95.0) | 0.815 @ |
| Pump | 60.84 ± 14.14 | 75.0 (60.0, 85.0) | 80.0 (60.0, 90.0) | |||
| Do you have any chronic disease or mental illness? | ||||||
| Yes | 62.35 ± 14.39 | 0.795 ^ | 70.0 (45.0, 77.50) | 0.718 @ | 60.0 (42.50, 80.0) | 0.008 @ |
| No | 61.41 ± 14.12 | 65.0 (50.0, 80.0) | 80.0 (60.0, 95.0) | |||
| Number of EMD visits in 2023 | ||||||
| 0 | 65.39 ± 12.71 | <0.001 | 70.0 (58.75, 85.0) | 0.516 # | 80.0 (60.0, 95.0) | 0.656 # |
| 1–2 | 57.82 ± 15.43 | 65.0 (45.0, 75.0) | 80.0 (55.0, 90.0) | |||
| >2 | 54.04 ± 9.66 | 65.0 (45.0, 75.0) | 80.0 (60.0, 95.0) | |||
| Number of diabetic ketoacidosis in 2023 | ||||||
| 0 | 65.24 ± 13.60 | <0.001 * | 70.0 (53.75, 85.0) | 0.647 # | 80.0 (60.0, 95.0) | 0.689 # |
| 1–2 | 56.55 ± 13.60 | 65.0 (50.0, 75.0) | 80.0 (60.0, 90.0) | |||
| >2 | 52.62 ± 9.71 | 62.50 (45.0, 85.0) | 72.5 (53.75, 95.0) |
| Variables | Worry Median (IQR) | p-Value | Communication Median (IQR) | p-Value |
|---|---|---|---|---|
| Age group | ||||
| 6–8 | 50.0 (18.75, 93.75) | 0.712 # | 71.88 (39.06, 85.94) | 0.005 # |
| 9–12 | 58.33 (41.67, 75.0) | 75.0 (50.0, 87.50) | ||
| 13–16 | 58.33 (33.33, 75.0) | 75.0 (62.50, 100.0) | ||
| Age at diagnosis | ||||
| 1–2 years | 50.0 (25.0, 83.33) | 0.064 # | 62.5 (37.5, 75.0) | <0.001 # |
| 2–5 years | 50.0 (25.0, 66.67) | 62.50 (45.31, 75.0) | ||
| 6–11 years | 58.33 (41.67, 75.0) | 81.25 (62.50, 100.0) | ||
| 12–16 years | 75.0 (50.0, 93.75) | 90.63 (67.19, 100.0) | ||
| Sex | ||||
| Male | 66.67 (50.0, 83.33) | 0.002 @ | 75.0 (62.50, 93.75) | 0.408 @ |
| Female | 50.0 (33.33, 66.67) | 75.0 (50.0, 93.75) | ||
| BMI | ||||
| <18.5 | 58.33 (41.67, 75.0) | 0.691 # | 75.0 (50.0, 89.06) | 0.313 # |
| 18.5–24.99 | 58.33 (41.67, 75.0) | 75.0 (59.38, 100.0) | ||
| 25–29.99 | 50.0 (12.5, 83.33) | 75.0 (40.63, 96.88) | ||
| ≥30 | 66.67 (33.33, 100.0) | 75.0 (56.25, 87.50) | ||
| Family’s income | ||||
| <500 | 50.0 (16.67, 75.0) | 0.075 # | 75.0 (57.81, 100.0) | 0.552 # |
| 500–1000 | 58.33 (41.67, 83.33) | 75.0 (54.69, 100.0) | ||
| >1000 | 50.0 (33.33, 66.67) | 75.0 (50.0, 87.50) | ||
| School | ||||
| Primary | 58.33 (41.67, 75.0) | 0.883 @ | 75.0 (45.31, 87.50) | 0.045 @ |
| Secondary | 58.33 (33.33, 75.0) | 75.0 (56.25, 100.0) | ||
| Child’s school performance | ||||
| Poor | 100.0 (79.17, 100.0) | 0.029 # | 62.50 (40.63, 81.25) | 0.268 # |
| Good | 50.0 (27.08, 75.0) | 87.50 (70.31, 100.0) | ||
| Very good | 58.33 (41.67, 75.0) | 75.0 (50.0, 100.0) | ||
| Excellent | 58.33 (33.33, 77.08) | 75.0 (50.0, 89.06) | ||
| HbA1c group | ||||
| ≤7.5 | 66.67 (41.67, 97.92) | 0.019 @ | 75.0 (51.56, 92.19) | 0.540 @ |
| >7.5 | 50.0 (33.33, 75.0) | 75.0 (56.25, 100.0) | ||
| Type of glucometer | ||||
| Standard | 50.0 (33.33, 75.0) | 0.219 @ | 75.0 (56.25, 100.0) | 0.317 @ |
| Continuous | 58.33 (41.67, 81.25) | 75.0 (51.56, 87.50) | ||
| What type of insulin regimens is the patient in? | ||||
| Subcutaneous | 58.33 (41.67, 83.33) | 0.201 @ | 75.0 (62.50, 100.0) | 0.164 @ |
| Pump | 50.0 (33.33, 75.0) | 75.0 (50.0, 93.75) | ||
| Do you have any chronic disease or mental illness? | ||||
| Yes | 50.0 (25.0, 75.0) | 0.315 @ | 75.0 (53.13, 90.63) | 0.901 @ |
| No | 58.33 (41.67, 75.0) | 75.0 (56.25, 93.75) | ||
| Number of emergency department visits in 2023 | ||||
| 0 | 50.0 (33.33, 66.67) | 0.357 # | 75.0 (50.0, 100.0) | 0.949 # |
| 1–2 | 58.33 (33.33, 83.33) | 75.0 (56.25, 93.75) | ||
| >2 | 66.67 (41.67, 100.0) | 75.0 (43.75, 93.75) | ||
| Number of diabetic ketoacidosis in 2023 | ||||
| 0 | 54.17 (41.67, 75.0) | 0.710 # | 75.0 (50.0, 100.0) | 0.646 # |
| 1–2 | 62.50 (33.33, 83.33) | 75.0 (56.25, 89.06) | ||
| >2 | 54.17 (33.33, 75.0) | 81.25 (59.38, 93.75) |
| Domain | Variables | β-Coefficient | 95% C.I. | p-Value § | |
|---|---|---|---|---|---|
| Diabetic symptoms | Family income | ||||
| <500 | 0.778 | −4.355 | 5.910 | 0.767 | |
| 500–1000 | 4.69 | 0.392 | 8.987 | 0.032 | |
| >1000 | 1.0 | ||||
| Child’s school performance | |||||
| Poor | −22.986 | −34.176 | −11.796 | <0.001 | |
| Good | −0.487 | −6.133 | 5.158 | 0.866 | |
| Very good | −4.569 | −8.786 | −0.353 | 0.034 | |
| Excellent | 1.0 | ||||
| HbA1c group | |||||
| ≤7.5 | 6.551 | 2.202 | 10.899 | 0.003 | |
| >7.5 | 1.0 | ||||
| Number of emergency department visits in 2023 | |||||
| 0 | 2.284 | −6.035 | 10.603 | 0.591 | |
| 1–2 | 1.131 | −6.775 | 9.038 | 0.779 | |
| >2 | 1.0 | ||||
| Number of diabetic ketoacidoses in 2023 | |||||
| 0 | 10.125 | 0.877 | 19.373 | 0.032 | |
| 1–2 | 2.954 | −5.973 | 11.881 | 0.517 | |
| >2 | 1.0 | ||||
| Treatment barriers | Age group | ||||
| 6–8 | −7.609 | −19.495 | 4.276 | 0.210 | |
| 9–12 | −10.041 | −16.819 | −3.262 | 0.004 | |
| 13–16 | 1.0 | ||||
| Family income | |||||
| <500 | −4.546 | −12.115 | 3.023 | 0.239 | |
| 500–1000 | 2.643 | −3.841 | 9.126 | 0.424 | |
| >1000 | 1.0 | ||||
| School | |||||
| Primary | −1.141 | −9.855 | 7.573 | 0.798 | |
| Secondary | 1.0 | ||||
| Type of glucometer | |||||
| Standard | −5.056 | −10.775 | 0.664 | 0.006 | |
| Continuous | 1.0 | ||||
| What type of insulin regimens is the patient in? | |||||
| Subcutaneous | −10.076 | −15.877 | −4.276 | 0.001 | |
| Pump | 1.0 | ||||
| Treatment adherence | Age group | ||||
| 6–8 | −20.651 | −35.101 | −6.200 | 0.005 | |
| 9–12 | −12.002 | −20.074 | −3.930 | 0.004 | |
| 13–16 | 1.0 | ||||
| Age at diagnosis | |||||
| 1–2 years | −12.809 | −28.182 | 2.564 | 0.102 | |
| 2–5 years | −13.091 | −26.264 | 0.081 | 0.051 | |
| 6–11 years | −4.526 | −16.452 | 7.399 | 0.457 | |
| 12–16 years | 1.0 | ||||
| Sex | |||||
| Male | 4.933 | −1.340 | 11.206 | 0.123 | |
| Female | 1.0 | ||||
| BMI group | |||||
| <18.5 | 17.252 | 5.331 | 29.173 | 0.005 | |
| 18.5–24.99 | 16.112 | 4.656 | 27.569 | 0.006 | |
| 25–29.99 | 14.473 | 1.006 | 27.941 | 0.035 | |
| ≥30 | 1.0 | ||||
| Family income | |||||
| <500 | 7.583 | −1.001 | 16.167 | 0.083 | |
| 500–1000 | 6.679 | −0.651 | 14.010 | 0.074 | |
| >1000 | 1.0 | ||||
| School | |||||
| Primary | −0.079 | −10.625 | 10.467 | 0.988 | |
| Secondary | 1.0 | ||||
| Type of glucometer | |||||
| Standard | −9.443 | −15.841 | −3.045 | 0.004 | |
| Continuous | 1.0 | ||||
| Do you have any chronic disease or mental illness | |||||
| Yes | −12.286 | −22.735 | −1.837 | 0.021 | |
| No | 1.0 | ||||
| Worry | Age at diagnosis | ||||
| 1–2 years | −15.102 | −34.763 | 4.560 | 0.132 | |
| 2–5 years | −16.033 | −32.641 | 0.575 | 0.058 | |
| 6–11 years | −11.027 | −26.334 | 4.279 | 0.158 | |
| 12–16 years | 1.0 | ||||
| Sex | |||||
| Male | 12.113 | 4.062 | 20.164 | 0.003 | |
| Female | 1.0 | ||||
| Family income | |||||
| <500 | −1.628 | −12.768 | 9.513 | 0.775 | |
| 500–1000 | 7.822 | −1.597 | 17.240 | 0.104 | |
| >1000 | 1.0 | ||||
| Child’s school performance | |||||
| Poor | 32.180 | 7.789 | 56.570 | 0.010 | |
| Good | −10.213 | −22.598 | 2.173 | 0.106 | |
| Very good | −3.820 | −13.329 | 5.689 | 0.431 | |
| Excellent | 1.0 | ||||
| HbA1c group | |||||
| ≤7.5 | 5.233 | −4.197 | 14.663 | 0.277 | |
| >7.5 | 1.0 | ||||
| Communication | Age group | ||||
| 6–8 | −16.325 | −30.973 | −1.677 | 0.029 | |
| 9–12 | −9.305 | −17.585 | −1.024 | 0.028 | |
| 13–16 | 1.0 | ||||
| School | |||||
| Primary | −1.275 | −12.094 | 9.543 | 0.817 | |
| Secondary | 1.0 | ||||
| What type of insulin regimens is the patient in? | |||||
| Subcutaneous | 7.737 | 1.018 | 14.457 | 0.024 | |
| Pump | 1.0 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlSaleh, A.; Ahmed, J.; Alsenani, I.; Alhousni, W.; AalAbdulsalam, R.; Alshammasi, M.T. Assessment of Quality of Life of Children and Adolescents with Type 1 Diabetes in Bahrain Using PedsQL 3.2 Diabetes Module. J. Clin. Med. 2025, 14, 2216. https://doi.org/10.3390/jcm14072216
AlSaleh A, Ahmed J, Alsenani I, Alhousni W, AalAbdulsalam R, Alshammasi MT. Assessment of Quality of Life of Children and Adolescents with Type 1 Diabetes in Bahrain Using PedsQL 3.2 Diabetes Module. Journal of Clinical Medicine. 2025; 14(7):2216. https://doi.org/10.3390/jcm14072216
Chicago/Turabian StyleAlSaleh, Aseel, Jamil Ahmed, Intisar Alsenani, Wijdaan Alhousni, Riham AalAbdulsalam, and Marya Tawfeek Alshammasi. 2025. "Assessment of Quality of Life of Children and Adolescents with Type 1 Diabetes in Bahrain Using PedsQL 3.2 Diabetes Module" Journal of Clinical Medicine 14, no. 7: 2216. https://doi.org/10.3390/jcm14072216
APA StyleAlSaleh, A., Ahmed, J., Alsenani, I., Alhousni, W., AalAbdulsalam, R., & Alshammasi, M. T. (2025). Assessment of Quality of Life of Children and Adolescents with Type 1 Diabetes in Bahrain Using PedsQL 3.2 Diabetes Module. Journal of Clinical Medicine, 14(7), 2216. https://doi.org/10.3390/jcm14072216






