Isokinetic Muscle Strengthening of the Lower Limbs in People with Stroke: A Systematic Review of Randomized Controlled Trials
Abstract
1. Introduction
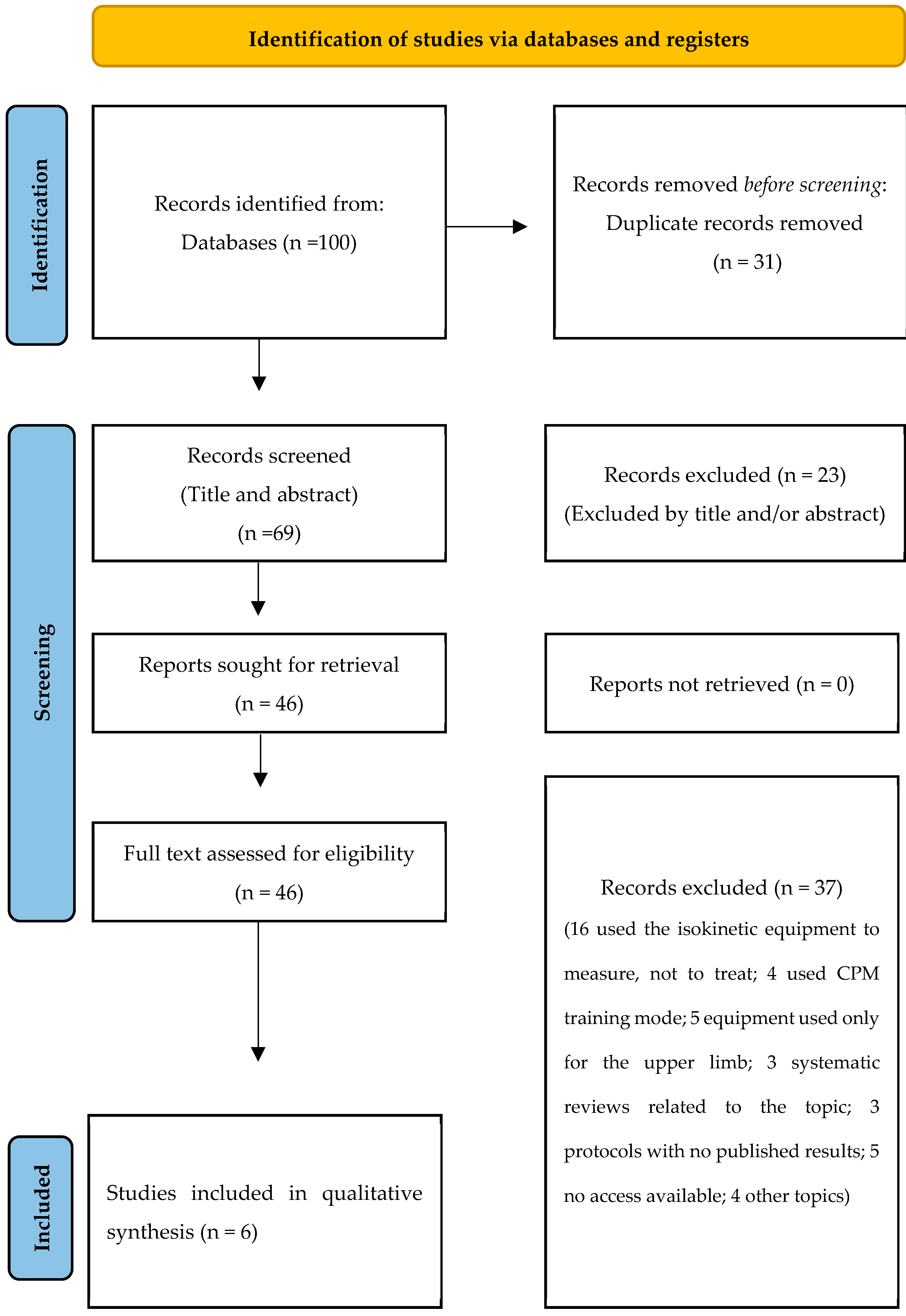
2. Methods
2.1. Design
2.2. Search Strategy and Selection of Studies
2.3. Eligibility Criteria
2.3.1. Types of Studies
2.3.2. Types of Participants
2.3.3. Types of Interventions
2.3.4. Types of Outcome Measures
2.4. Data Extraction
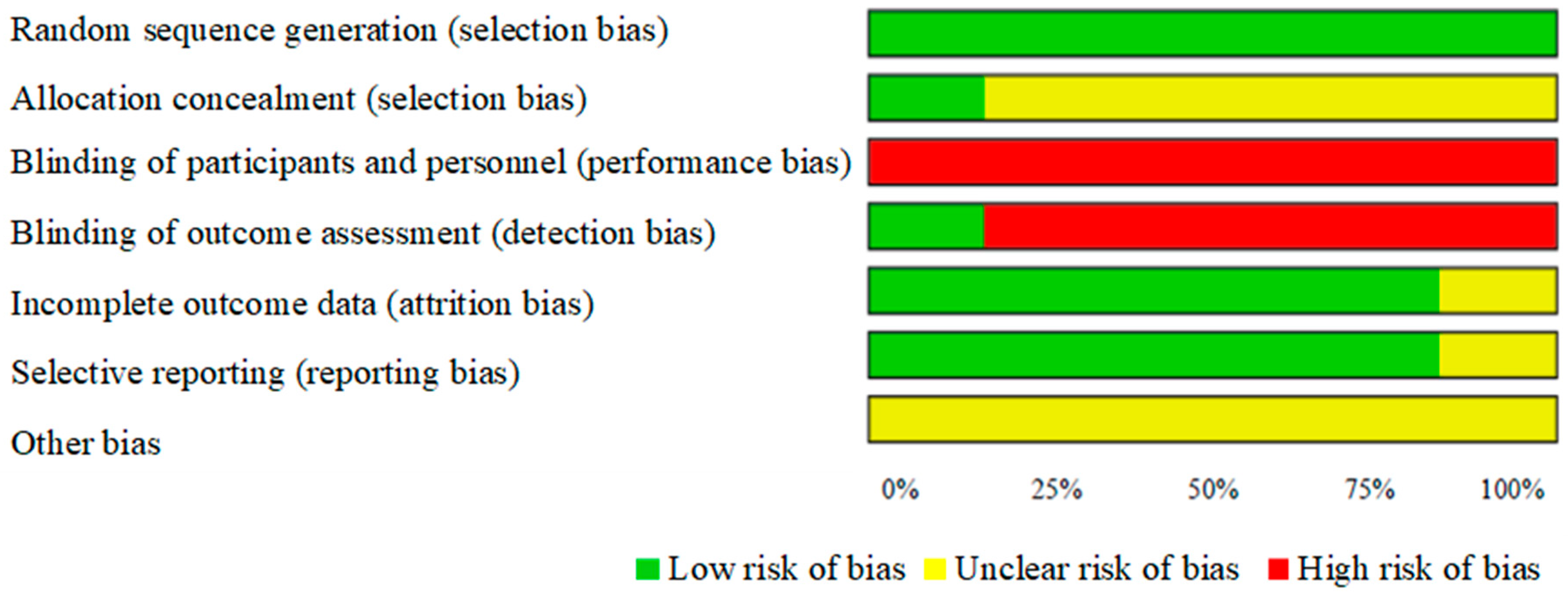
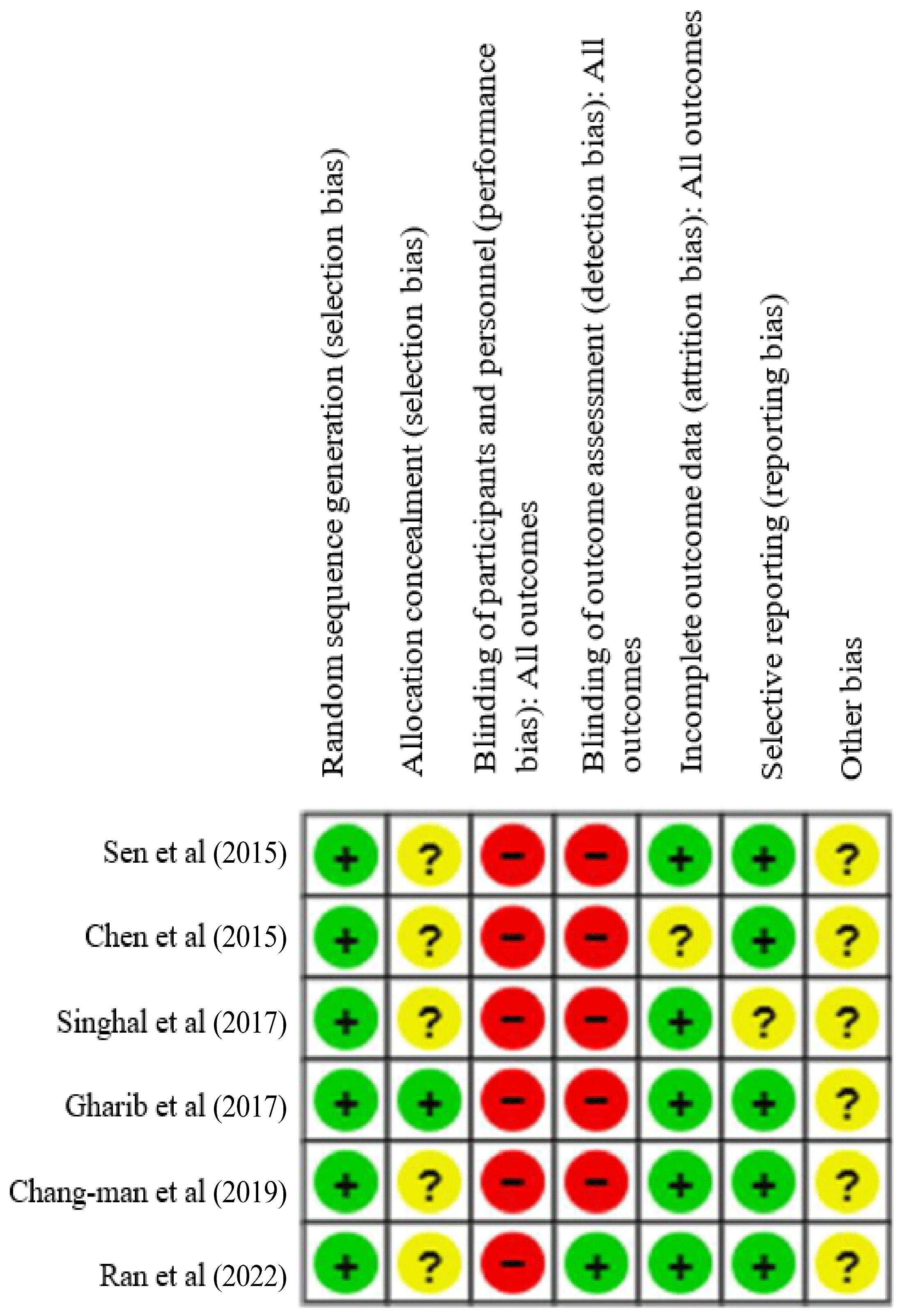
2.5. Assessment of the Quality and Risk of Bias of the Individual Studies
3. Results
3.1. Characteristics of the Participants
3.2. Characteristics of the Interventions
3.3. Outcome Measures
3.4. Results of the Individual Studies: Effects of the Interventions
3.5. Comparison Between Isokinetic Muscle Strengthening and Conventional Physical Therapy
3.6. Comparison Between Isokinetic Muscle Strengthening and Other Strengthening Methods
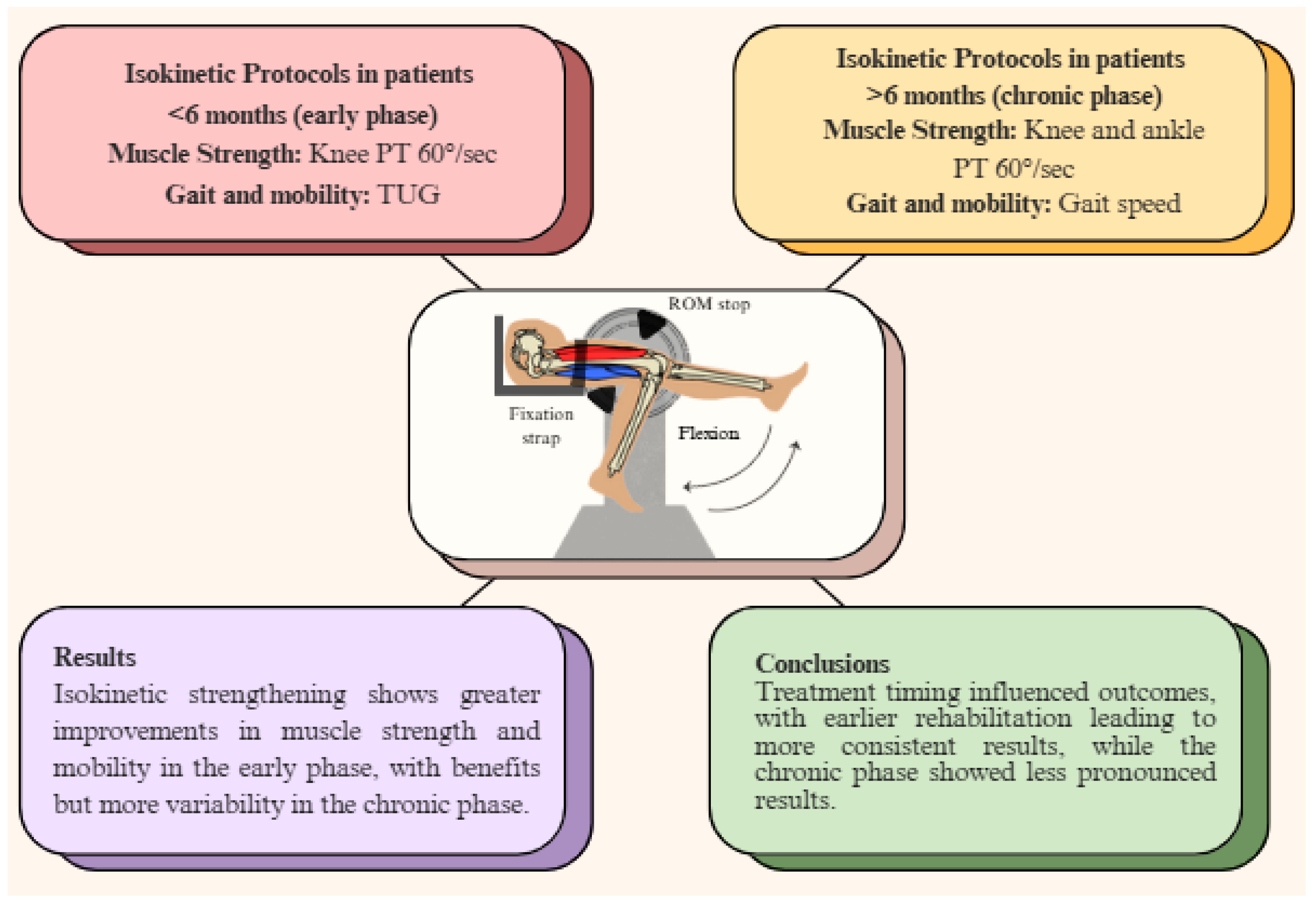
3.7. Comparison of Early (<6 Months) and Chronic (>6 Months) Post-Stroke Treatment Effects
3.8. Effect Size and Statistical Measures
3.9. Assessment of the Quality and Risk of Bias of Individual Studies
4. Discussion
4.1. Limitations
4.2. Clinical Implications of the Review and Future Research Lines
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Plaza, I. Sociedad Española de Neurología. Grupo de Estudio de Enfermedades Cerebrovasculares de la SEN. Valencia: Sociedad Valenciana de Neurología, Instituto Médico Valenciano. 2006. El Ictus Manual. Capítulo 1: ¿qué es un ictus? [1 pantalla]. Available online: http://ictus.sen.es/?page_id=25 (accessed on 5 June 2024).
- National Institutes of Health. United States: National Heart, Lung, and Blood Institute; 2023. What Is a Stroke? Available online: https://www.nhlbi.nih.gov/health/stroke (accessed on 15 October 2024).
- Cano-De-La-Cuerda, R.; Collado-Vázquez, S. Neurorrehabilitación: Métodos Específicos de Valoración y Tratamiento, 1st ed.; Médica Panamericana: Madrid, Spain, 2012. [Google Scholar]
- Ulla-Britt, F.; Downham, D.; Lexell, J. Knee muscle strength, gait performance and perceived participation after stroke. Arch. Phys. Med. Rehabil. 2006, 87, 974–980. [Google Scholar]
- Khan, F.; Anjamparuthikal, H.; Chevidikunnan, M.F. The comparison between isokinetic knee muscles strength in the ipsilateral and contralateral limbs and correlating with function of patients with stroke. J. Neurosci. Rural. Pract. 2019, 10, 683–689. [Google Scholar]
- Hunnicut, J.L.; Gregory, C.M. Skeletal muscle changes following stroke: A systematic review and comparison to healthy individuals. Top. Stroke Rehabil. 2017, 24, 463–471. [Google Scholar]
- Peñaloza-González, J.A.; González-Mejía, S.; García-Melo, J.I. Development of a control strategy in an isokinetic device for physical rehabilitation. Sensors 2023, 23, 5827. [Google Scholar] [CrossRef]
- Soto-Cámara, R.; González-Bernal, J.J.; González-Santos, J.; Aguilar-Parra, J.M.; Trigueros, R.; López-Liria, R. Knowledge on Signs and Risk Factors in Stroke Patients. J. Clin. Med. 2020, 9, 2557. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffman, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. Declaración PRISMA 2020: Una guía actualizada para la publicación de revisiones sistemáticas. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [PubMed]
- Physiotherapy Evidence Database. PEDro. Sydney: Physiotherapy Evidence Database; 1999. Escala PEDro. Available online: https://pedro.org.au/spanish/resources/pedro-scale/ (accessed on 10 October 2024).
- Miller, K.J.; Suárez-Iglesias, D.; Seijo-Martínez, M.; Ayán, C. Fisioterapia para la congelación de la marcha en la enfermedad de Parkinson: Revisión sistemática y metaanálisis. Rev. Neurol. 2020, 70, 161–170. [Google Scholar] [PubMed]
- Centre for Evidence-Based Medicine. Oxford: CEBM; 2009. Oxford Centre for Evidence-Based Medicine Levels of Evidence (March 2009). Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 15 March 2024).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, D5928. [Google Scholar]
- Sen, S.B.; Demir, S.O.; Ekiz, T.; Özgirgin, N. Effects of the bilateral isokinetic strengthening training on functional parameters, gait, and the quality of life in patients with stroke. Int. J. Clin. Exp. Med. 2015, 8, 16871–16879. [Google Scholar]
- Chen, C.L.; Chang, K.J.; Wu, P.Y.; Chi, C.H.; Chang, S.T.; Cheng, Y.Y. Comparison of the effects between isokinetic and isotonic strength training in subacute stroke patients. J. Stroke Cerebrovasc. Dis. 2015, 24, 1317–1323. [Google Scholar]
- Singhal, S.; Pattnaik, M.; Mohanty, P. Comparison of isokinetic strengthening with functional strengthening of lower limb and their effect on gait in hemiparesis due to stroke. J. Neurol. Neurorehabil. Res. 2017, 2, 46–54. [Google Scholar] [CrossRef]
- Gharib, N.M.; Mohamed, R.A. Isokinetic strength training in patients with stroke: Effects on muscle strength, gait and functional mobility. Int. J. Physiother. Res. 2017, 5, 1976–1986. [Google Scholar] [CrossRef]
- An, C.M.; Roh, J.S. Effects of isokinetic strength exercise of the hemiparetic knee joint on lower extremity sensorimotor and gait functions in patients with chronic stroke: Open kinetic chain versus closed kinetic chain. Phys. Ther. Korea 2019, 26, 49–60. [Google Scholar] [CrossRef]
- Ran, L.F.; Ye, Z.Q.; Guo, J.H.; Liu, X.X.; Wang, N. Effect of isokinetic muscle strength training combined with aerobic exercise on cardiopulmonary function and lower limb movement function in stroke patients. Chin. J. Conval. Med. 2022, 31, 1298–1302. [Google Scholar]
- Wang, J.; Zhang, H.; Ma, J.; Gu, L.; Li, X. Efficacy of combined non-invasive brain stimulation and robot-assisted gait training on lower extremity recovery post-stroke: A systematic review and meta-analysis of randomized controlled trials. Front. Neurol. 2025, 16, 1500020. [Google Scholar] [CrossRef]
- Pontes, S.S.; de Carvalho, A.L.R.; Almeida, K.O.; Neves, M.P.; Ribeiro Schindler, I.F.S.; Alves, I.G.N.; Arcanjo, F.L.; Gomes-Neto, M. Effects of isokinetic muscle strengthening on muscle strength, mobility, and gait in post-stroke patients: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Otálora, J.D.; Jaramillo, B.Y.; Meneses, C.Y.; Ramírez, L.M. Efectividad de la Isocinesia Robótica en la Función Motora de Pacientes con Hemiplejía. Revisión Sistemática y Metanálisis. Corporación Universitaria Iberoamericana. 2019. Available online: https://repositorio.ibero.edu.co/handle/001/904 (accessed on 6 September 2024).
- Chiquito-Freile, C.J. Valores de Referencia de Fuerza Isocinética a 60°/Segundo de Extensores y Flexores de Rodilla en Deportistas de Selecciones Colombia. Universidad el Bosque. 2019. Available online: https://repositorio.unbosque.edu.co/items/02213d51-10b6-44aa-ab56-774f51a84c62 (accessed on 27 November 2024).
- Bai, Z.; Zhang, D.; Liang, D.; Chen, X.; Shi, X.; Chen, S. Effect of eccentric training with different durations, intensities, and contraction velocities on upper limb muscle strength: A meta-analysis. Life 2025, 15, 456. [Google Scholar] [CrossRef]
- Dutra-Barbosa, D.; Ruff-Trojahn, M.; Gularte-Porto, D.V.; Scotta-Hentschke, G.; Scotta-Hentschke, V. Strength training protocols in hemiparetic individuals post stroke: A systematic review. Fisioter. Mov. 2018, 31, e003127. [Google Scholar]
- Wei, X.; Sun, S.; Zhang, M.; Zhao, Z. A systematic review and meta-analysis of clinical efficacy of early and late rehabilitation interventions for ischemic stroke. BMC Neurol. 2024, 8, 91. [Google Scholar] [CrossRef]
- Dilshad, U.; Ambreen, F.; Ashraf, W.; Arif, K.; Mohsin, A. Comparing the effectiveness of traditional physiotherapy combined with virtual reality for post-stroke patients. Insights-J. Health Rehabil. 2025, 3, 470–478. [Google Scholar] [CrossRef]
- Akınoğlu, B.; Paköz, B.; Yilmaz, A.E.; Shehu, S.U.; Kocahan, T. Effect of contraction type at varying angular velocities on isokinetic muscle strength training. J. Exerc. Rehabil. 2023, 19, 228–236. [Google Scholar] [CrossRef] [PubMed]
| Dialnet | Type of article: journal article Publication years: 2014–2024 |
| PEDro | Publication years: 2014–2024 |
| PubMed | Article accessibility: full text Publication date: last 10 years |
| SCOPUS | Document type: clinical trial Publication years: 2014–2023 |
| Cochrane | Publication years: 2014–2024 |
| MEDLINE | Publication years: 2014–2023 |
| Web of Science | Publication years: 2014–2024 |
| Participants | Intervention Group | Control Group | Joints and Movements | |
|---|---|---|---|---|
| Sen et al. [14] | Sample: 50 Period: >3 months Age: 40–65 years Sex: 33 men and 17 women Losses: 0 | (n = 25) Conventional physiotherapy + isokinetic muscle strengthening | (n = 25) Conventional physiotherapy | Knee and ankle Concentric flexion and extension Bilateral |
| Chen et al. [15] | Sample: 31 Period: <6 months Age: 51–78 years Sex: 13 men and 11 women Losses: 7 | (n = 12) Conventional physiotherapy + isokinetic muscle strengthening | (n = 12) Conventional physiotherapy + isotonic muscle strengthening | Knee Concentric and eccentric flexion and extension Bilateral |
| Singhal et al. [16] | Sample: 30 Period: 4–21 months Age: 38–66 years Sex: 26 men and 4 women Losses: 0 | (n = 15) Conventional physiotherapy + isokinetic muscle strengthening | (n = 15) Conventional physiotherapy + functional muscle strengthening | Hip, knee, and ankle Concentric flexion and extension Affected side |
| Gharib et al. [17] | Sample: 30 Period: 6–18 months Age: 46–62 years Sex: 16 men and 14 women Losses: 0 | (n = 15) Conventional physiotherapy (60 min) + isokinetic muscle strengthening | (n = 15) Conventional physiotherapy (60 min) | Knee and ankle Concentric flexion and extension Affected side |
| Chang-man et al. [18] | Sample: 30 Period: >6 months Age: 42–66 years Sex: 17 men and 13 women Losses: 0 | (n = 15) Conventional physiotherapy + isokinetic muscle strengthening in open kinetic chain (45 min) | (n = 15) Conventional physiotherapy + isokinetic muscle strengthening in closed kinetic chain (45 min) | Knee Concentric flexion and extension Affected side |
| Ran et al. [19] | Sample: 80 Period: >2 months Age: 60–75 years Sex: not provided Losses: 0 | (n = 40) Conventional physiotherapy + 20 min aerobic exercise + 20 min isokinetic training | (n = 40) Conventional physiotherapy + 40 min aerobic exercise | Knee Concentric flexion and extension Affected side |
| Equipment | Training (Dosage) | Duration and Frequency | |
|---|---|---|---|
| Sen et al. [14] (Turkey) | Biodex System | Warm-up: (knee) 3 reps at 60°/s and 180°/s; (ankle) 3 reps at 60°/s and 120°/s. Cool-down: not reported. Training: (knee) 5 reps at 60°/s, 90°/s, 120°/s, 150°/s, and 10 reps at 180°/s (30 total); (ankle) 5 reps at 60°/s, 90°/s, 120°/s, and 10 reps at 150°/s (25 total). | 3 weeks 5 days/week (15 sessions) |
| Chen et al. [15] (China) | Biodex System | Warm-up and cool-down: not reported. Training: (isokinetic) 3 sets of 5 concentric + 5 eccentric reps at 60°/s (30 total); (isotonic) 3 sets of 10 reps at 60% maximum strength (30 total). | 4 weeks 5 days/week (20 sessions) |
| Singhal et al. [16] (India) | Humac/ Norm | Warm-up and cool-down: not reported. Training: (isokinetic) 3 sets of 5 concentric reps at 60°/s (15 total per joint); (functional) step exercises (multi-directional), single-leg supports, sit-to-stand transfers, and bridges. | 6 weeks 3 days/week (18 sessions) |
| Gharib et al. [17] (Egypt) | Biodex System | Warm-up and cool-down: not reported. Training: (knee and ankle) 3 sets of 5 concentric reps at 30°/s, and 5 eccentric at 90°/s (30 total per joint). | 8 weeks 3 days/week (24 sessions) |
| Chang-man et al. [18] (Korea) | Biodex System | Warm-up: 5 min on a stationary bike. Cool-down: 10 min passive stretching. Training: (open and close chain) 5 sets of 5 reps at 90°/s, 8 reps at 120°/s, 10 reps at 150°/s (115 total). “Leg press”-type knee accessory used for closed-chain. | 6 weeks 3 days/week (18 sessions) |
| Ran et al. [19] (China) | Humac/ Norm | Isokinetic warm-up: (3 min) 10 reps at 180°/s. Training: 10 reps at 180°/s, 120°/s, 90°/s and 60°/s (40 total). Aerobic warm-up: (3 min) and cool-down (2 min). Training: 15 min on a cycle-ergometer at level 12–15 on Borg scale. | 4 weeks 5 days/week (20 sessions) |
| Muscle Strength | Gait and Mobility | Main Results and Conclusions | |
|---|---|---|---|
| Sen et al. [14] | Knee PT at 60° and 180°/s Ankle PT at 60° and 120°/s | FIM SS-QOL 10-MWT 6MWT SCT TUG BBS RMI | Isokinetic training combined with physiotherapy showed significant improvements in muscle strength (p < 0.025), mobility, gait, balance, and quality of life, with greater results observed in the isokinetic group (p < 0.025, p < 0.05). Bilateral isokinetic training combined with physiotherapy appears to be more effective for muscle strengthening and improving functional outcomes in stroke patients. |
| Chen et al. [15] | Knee PT at 60° and 120°/s Isometric PT at 90°/s | SF-36 TUG | Both groups showed significant gains in knee flexion, SF-36 physical functioning, and TUG. The isokinetic group showed greater improvement, with significant differences in knee flexion at 60°/s and 120°/s (p < 0.05) on the affected side. If available, isokinetic training during the subacute phase of stroke may provide more significant benefits. |
| Singhal et al. [16] | Hip/Knee/ Ankle PT 60°/s | 6MWT SL | Both groups showed significant improvements in PT 60°/s (hip and knee) and 6MWT, with the isokinetic group showing more substantial results (p < 0.05). While both groups improved in PT 60°/s (ankle) and SL, no significant differences were observed between them. Lower limb isokinetic training is more effective than functional training for strengthening hip and knee muscles and improving 6MWT performance. |
| Gharib et al. [17] | Knee/Ankle PT 30° and 90°/s | TUG Qualisys Motion Capture System | Both groups showed significant improvements in PT 30 and 90°/s. The isokinetic group showed more remarkable results (p < 0.05). Significant differences in gait speed, gait cycle, single-leg support, and TUG favored the isokinetic group (p < 0.05). Isokinetic muscle strengthening combined with physiotherapy is effective for improving muscle strength, gait, and functional mobility in chronic phase stroke patients. |
| Chang-man et al. [18] | Knee PT/BW 60°/s Ankle PT/BW 30°/s | GAITRite mat | Both groups showed significant improvements in PT/BW (p < 0.01), with no significant differences between them. Significant improvements in gait speed were seen in both groups. The closed kinetic chain exercise group showed more considerable results in gait speed and spatial symmetry (p < 0.01). Isokinetic strengthening in the closed kinetic chain can effectively improve sensorimotor function, gait, and functional capacity in the chronic phase of stroke rehabilitation. |
| Ran et al. [19] | Knee PT 60°/s TW | FMA-LE VO2 max | Both groups showed statistically significant effects on all outcome measures (p < 0.05). Statistically significant differences favoring isokinetic strengthening were found compared to the control group (p < 0.05). Isokinetic training combined with aerobic exercise is more effective for improving cardiopulmonary and lower limb function in stroke patients and can be applied in clinical practice. |
| Time Post-Stroke | Muscle Strength | Gait and Mobility | Results | |
|---|---|---|---|---|
| Sen et al. [14] | <6 months | Knee and ankle PT 60°/s | 6MWT, TUG, RMI | Greater results in isokinetic group (p < 0.025, p < 0.05). |
| Chen et al. [15] | <6 months | Knee PT 60°/s | TUG | Better improvement in isokinetic group (p < 0.05). |
| Ran et al. [19] | <6 months | Knee PT 60°/s | FMA-LE | Greater results in isokinetic group (p < 0.05). |
| Singhal et al. [16] | >6 months | Hip, knee and ankle PT 60°/s | 6MWT, SL | Better improvement in isokinetic group (p < 0.05). No differences between groups for SL and ankle PT 60°/s. |
| Gharib et al. [17] | >6 months | Knee and ankle PT 30° and 90°/s | TUG, gait speed | Greater results in isokinetic group (p < 0.05). |
| Chang-man et al. [18] | >6 months | Knee and ankle PT 60°/s: | Gait speed | Both groups improved muscle strength (p < 0.01), with no differences between them. Greater results in gait speed for CKC group (p < 0.01) |
| Effect Size or Clinical Significance | Statistical Measures | |
|---|---|---|
| Sen et al. [14] | Not reported | p-value, change level |
| Chen et al. [15] | Not reported | p-value |
| Singhal et al. [16] | Not reported | p-value, percentage of improvement |
| Gharib et al. [17] | Not reported | p-value, t-value |
| Chang-man et al. [18] | Clinical significance on gait velocity: OKC 0.10 m/s, CKC 0.14 m/s. | p-value |
| Ran et al. [19] | Not reported | p-value, t-value |
| Author (Year) | Item | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | |
| Sen et al. (2015) [14] | Y | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 |
| Chen et al. (2015) [15] | Y | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5/10 |
| Singhal et al. (2017) [16] | Y | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5/10 |
| Gharib et al. (2017) [17] | Y | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 |
| Chang-man et al. (2019) [18] | Y | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 |
| Ran et al. (2022) [19] | Y | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7/10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguirre-Villanueva, E.A.; Cano-de-la-Cuerda, R.; Laguarta-Val, S. Isokinetic Muscle Strengthening of the Lower Limbs in People with Stroke: A Systematic Review of Randomized Controlled Trials. J. Clin. Med. 2025, 14, 2215. https://doi.org/10.3390/jcm14072215
Aguirre-Villanueva EA, Cano-de-la-Cuerda R, Laguarta-Val S. Isokinetic Muscle Strengthening of the Lower Limbs in People with Stroke: A Systematic Review of Randomized Controlled Trials. Journal of Clinical Medicine. 2025; 14(7):2215. https://doi.org/10.3390/jcm14072215
Chicago/Turabian StyleAguirre-Villanueva, Elsa Alejandra, Roberto Cano-de-la-Cuerda, and Sofía Laguarta-Val. 2025. "Isokinetic Muscle Strengthening of the Lower Limbs in People with Stroke: A Systematic Review of Randomized Controlled Trials" Journal of Clinical Medicine 14, no. 7: 2215. https://doi.org/10.3390/jcm14072215
APA StyleAguirre-Villanueva, E. A., Cano-de-la-Cuerda, R., & Laguarta-Val, S. (2025). Isokinetic Muscle Strengthening of the Lower Limbs in People with Stroke: A Systematic Review of Randomized Controlled Trials. Journal of Clinical Medicine, 14(7), 2215. https://doi.org/10.3390/jcm14072215







