Sleep Quality and Its Association with Quality of Life and Mortality in Hemodialysis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Quality of Life Questionnaire
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. QOL Scores According to Sleep Score Tertiles
3.3. Multiple Analysis
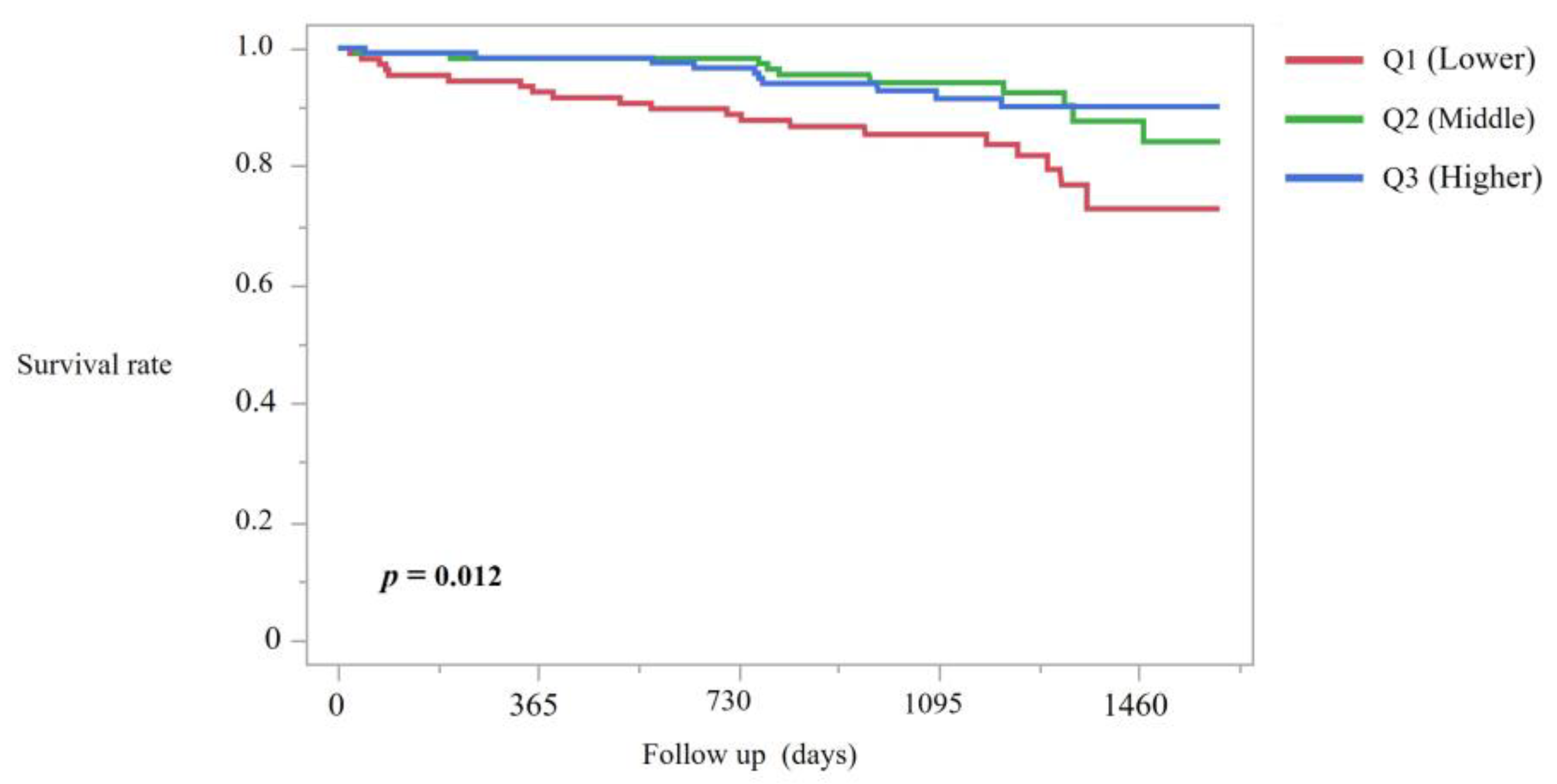
3.4. Mortality Analysis
3.5. Multiple Analysis of Mortality
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Alb | Albumin |
| AUC | Area under the curve |
| BIA | Bioelectrical impedance analysis |
| BUN | Blood urea nitrogen |
| BMI | Body mass index |
| Ca | Calcium |
| CI | Confidence interval |
| Cl | Chloride |
| Cr | Creatinine |
| CRP | C-reactive protein |
| CVD | Cardiovascular disease |
| DM | Diabetes mellitus |
| DBP | Diastolic blood pressure |
| ECW/ICW | Extracellular water to intracellular water ratio |
| GNRI | Geriatric nutritional risk index |
| Hb | Hemoglobin |
| HD | Hemodialysis |
| HDL-C | High-density lipoprotein cholesterol |
| HR | Hazard ratio |
| iPTH | Intact parathyroid hormone |
| Kt/V | Urea clearance normalized by distribution volume |
| K | Potassium; |
| Na | Sodium |
| NT-proBNP | N-terminal pro-brain natriuretic peptide |
| P | Phosphate |
| PA | Phase angle |
| PEW | Protein-energy wasting |
| QOL | Quality of life |
| ROC | Receiver operating characteristic |
| SBP | Systolic blood pressure |
| SF-36 | 36-Item Short Form Health Survey |
| TG | Triglycerides |
| TP | Total protein |
| UA | Uric acid |
| β2MG | Beta-2 microglobulin |
| LDL-C | Low-density lipoprotein cholesterol |
References
- Morin, C.M.; Jarrin, D.C. Epidemiology of Insomnia: Prevalence, Course, Risk Factors, and Public Health Burden. Sleep Med. Clin. 2022, 17, 173–191. [Google Scholar] [CrossRef]
- Hanafusa, N.; Abe, M.; Joki, N.; Ogawa, T.; Kanda, E.; Kikuchi, K.; Goto, S.; Taniguchi, M.; Nakai, S.; Naganuma, T.; et al. Annual dialysis data report 2019, JSDT Renal Data Registry. Ren. Replace. Ther. 2023, 9, 47. [Google Scholar] [CrossRef]
- Tan, L.H.; Chen, P.S.; Chiang, H.Y.; King, E.; Yeh, H.C.; Hsiao, Y.L.; Chang, D.R.; Chen, S.H.; Wu, M.Y.; Kuo, C.C. Insomnia and Poor Sleep in CKD: A Systematic Review and Meta-analysis. Kidney Med. 2022, 4, 100458. [Google Scholar] [CrossRef] [PubMed]
- Matsui, K.; Yoshiike, T.; Nagao, K.; Utsumi, T.; Tsuru, A.; Otsuki, R.; Ayabe, N.; Hazumi, M.; Suzuki, M.; Saitoh, K.; et al. Association of Subjective Quality and Quantity of Sleep with Quality of Life among a General Population. Int. J. Environ. Res. Public Health 2021, 18, 12835. [Google Scholar] [CrossRef]
- Losso, R.L.; Minhoto, G.R.; Riella, M.C. Sleep disorders in patients with end-stage renal disease undergoing dialysis: Comparison between hemodialysis, continuous ambulatory peritoneal dialysis and automated peritoneal dialysis. Int. Urol. Nephrol. 2015, 47, 369–375. [Google Scholar] [CrossRef]
- Xu, J.; Yoon, I.Y.; Chin, H.J. The effect of sleep apnea on all-cause mortality in nondialyzed chronic kidney disease patients. Sleep Med. 2016, 27–28, 32–38. [Google Scholar] [CrossRef]
- Jhamb, M.; Ran, X.; Abdalla, H.; Roumelioti, M.E.; Hou, S.; Davis, H.; Patel, S.R.; Yabes, J.; Unruh, M. Association of Sleep Apnea with Mortality in Patients with Advanced Kidney Disease. Clin. J. Am. Soc. Nephrol. 2020, 15, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Reynaga-Ornelas, L.; Baldwin, C.M.; Arcoleo, K.; Quan, S.F. Impact of Sleep and Dialysis Mode on Quality of Life in a Mexican Population. Southwest J. Pulm. Crit. Care 2019, 18, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Elder, S.J.; Pisoni, R.L.; Akizawa, T.; Fissell, R.; Andreucci, V.E.; Fukuhara, S.; Kurokawa, K.; Rayner, H.C.; Furniss, A.L.; Port, F.K.; et al. Sleep quality predicts quality of life and mortality risk in haemodialysis patients: Results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transpl. 2008, 23, 998–1004. [Google Scholar] [CrossRef]
- Kuna, K.; Szewczyk, K.; Gabryelska, A.; Białasiewicz, P.; Ditmer, M.; Strzelecki, D.; Sochal, M. Potential Role of Sleep Deficiency in Inducing Immune Dysfunction. Biomedicines 2022, 10, 2159. [Google Scholar] [CrossRef]
- Fitzpatrick, J.; Kerns, E.S.; Kim, E.D.; Sozio, S.M.; Jaar, B.G.; Estrella, M.M.; Tereshchenko, L.G.; Monroy-Trujillo, J.M.; Parekh, R.S.; Bourjeily, G. Functional outcomes of sleep predict cardiovascular intermediary outcomes and all-cause mortality in patients on incident hemodialysis. J. Clin. Sleep Med. 2021, 17, 1707–1715. [Google Scholar] [CrossRef]
- Hays, R.D.; Kallich, J.D.; Mapes, D.L.; Coons, S.J.; Carter, W.B. Development of the Kidney Disease Quality of Life (KDQOLTM) Instrument. Qual. Life Res. 1994, 3, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Fukuhara, S.; Shinzato, T.; Miura, Y.; Wada, S.; Hays, R.D.; Tabata, R.; Otsuka, H.; Takai, I.; Maeda, K.; et al. Translation, cultural adaptation, and initial reliability and multitrait testing of the Kidney Disease Quality of Life instrument for use in Japan. Qual. Life Res. 2001, 10, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Shinzato, T.; Nakai, S.; Fujita, Y.; Takai, I.; Morita, H.; Nakane, K.; Maeda, K. Determination of Kt/V and protein catabolic rate using pre- and postdialysis blood urea nitrogen concentrations. Nephron 1994, 67, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef]
- Tate, R.; Beydoun, M. Sleep quality, cognitive aging, and mortality among middle to older aged us adults. Innov. Aging 2024, 8, 1160–1161. [Google Scholar] [CrossRef]
- Cukor, D.; Unruh, M.; McCurry, S.M.; Mehrotra, R. The challenge of insomnia for patients on haemodialysis. Nat. Rev. Nephrol. 2021, 17, 147–148. [Google Scholar] [CrossRef]
- Wood, A.M.; Joseph, S.; Lloyd, J.; Atkins, S. Gratitude influences sleep through the mechanism of pre-sleep cognitions. J. Psychosom. Res. 2009, 66, 43–48. [Google Scholar] [CrossRef]
- Palmer, C.A.; John-Henderson, N.A.; Bawden, H.; Massey, A.; Powell, S.L.; Hilton, A.; Carter, J.R. Sleep restriction reduces positive social emotions and desire to connect with others. Sleep 2023, 46, zsac265. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Haack, M. The Sleep-Immune Crosstalk in Health and Disease. Physiol. Rev. 2019, 99, 1325–1380. [Google Scholar] [CrossRef]
- Lee, H.W.; Yoon, H.S.; Yang, J.J.; Song, M.; Lee, J.K.; Lee, S.A.; Choi, J.Y.; Kang, D. Association of sleep duration and quality with elevated hs-CRP among healthy Korean adults. PLoS ONE 2020, 15, e0238053. [Google Scholar] [CrossRef]
- Garvin, P.; Nilsson, E.; Ernerudh, J.; Kristenson, M. The joint subclinical elevation of CRP and IL-6 is associated with lower health-related quality of life in comparison with no elevation or elevation of only one of the biomarkers. Qual. Life Res. 2016, 25, 213–221. [Google Scholar] [CrossRef]
- Proctor, M.J.; McMillan, D.C.; Horgan, P.G.; Fletcher, C.D.; Talwar, D.; Morrison, D.S. Systemic inflammation predicts all-cause mortality: A glasgow inflammation outcome study. PLoS ONE 2015, 10, e0116206. [Google Scholar] [CrossRef] [PubMed]
- Gales-Villar, G.J.; Lu, A. #1601 Sleep disorders and sleep quality among hemodialysis patients in a Tertiary Hospital in Valenzuela, Philippines: A one center cross sectional study. Nephrol. Dial. Transpl. 2025, 40 (Suppl. 3), gfaf116.1672. [Google Scholar] [CrossRef]
- Dai, W.D.; Zhang, D.L.; Cui, W.Y.; Liu, W.H. Effect of long intermittent hemodialysis on improving dialysis adequacy of maintenance hemodialysis patients. Chin. Med. J. 2013, 126, 4655–4659. [Google Scholar] [CrossRef] [PubMed]
- Scher, N.; Guetta, L.; Draghi, C.; Yahiaoui, S.; Terzioglu, M.; Butaye, E.; Henriques, K.; Alavoine, M.; Elharar, A.; Guetta, A.; et al. Sleep Disorders and Quality of Life in Patients with Cancer: Prospective Observational Study of the Rafael Institute. JMIR Form. Res. 2022, 6, e37371. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Benz, F.; Dressle, R.J.; Espie, C.A.; Johann, A.F.; Blanken, T.F.; Leerssen, J.; Wassing, R.; Henry, A.L.; Kyle, S.D.; et al. Insomnia disorder: State of the science and challenges for the future. J. Sleep Res. 2022, 31, e13604. [Google Scholar] [CrossRef]




| Item | Q1 Median (IQR) | Q2 Median (IQR) | Q3 Median (IQR) | p Value |
|---|---|---|---|---|
| Age (years) | 67 (52–74) | 66 (56–73) | 67 (58–73) | 0.559 |
| BMI (kg/m2) | 22.11 (19.60–25.12) | 22.15 (19.96–25.85) | 22.04 (19.51–24.98) | 0.617 |
| HD history (months) | 66 (27.50–126) | 74 (36.50–128.5) | 67 (37–138.5) | 0.840 |
| Initial SBP (mmHg) | 148 (130–162) | 144.5 (128–164.75) | 146 (130–159.5) | 0.834 |
| Initial DBP (mmHg) | 76 (68–87) | 74 (66–87.5) | 78 (68–85) | 0.857 |
| TP(g/dL) | 6.5 (6.3–6.9) | 6.6 (6.2–6.8) | 6.5 (6.2–6.8) | 0.973 |
| Alb (g/dL) | 3.7 (3.4–3.8) | 3.6 (3.4–3.8) | 3.6 (3.45–3.8) | 0.697 |
| Na (mEq/L) | 139 (137–141) | 139 (138–141) | 139 (138–140) | 0.786 |
| K (mEq/L) | 4.8 (4.3–5.25) | 4.8 (4.3–5.275) | 4.8 (4.45–5.4) | 0.453 |
| Cl (mEq/L) | 103 (102–105) | 103 (101–106) | 103 (102–105) | 0.688 |
| TG (mg/dL) | 97 (67.5–145.5) | 108 (75–151) | 103 (68–152.5) | 0.856 |
| LDL-C (mg/dL) | 87 (70–105) | 85.5 (66–103.75) | 85 (71–110) | 0.449 |
| UA (mg/dL) | 7.8 (7–8.7) | 7.8 (6.9–8.4) | 7.5 (6.65–8.45) | 0.060 |
| BUN (mg/dL) | 58.6 (49.2–67.05) | 57.35 (48.025–72.025) | 55.2 (45.85–66.35) | 0.433 |
| Cr (mg/dL) | 10.13 (8.63–12.09) | 10.455 (8.9825–11.76) | 10.16 (8.855–11.445) | 0.705 |
| Ca (mg/dL) | 8.7 (8.2–9) | 8.7 (8.3–9) | 8.6 (8.3–8.9) | 0.477 |
| P (mg/dL) | 5.6 (5.1–6.3) | 5.6 (4.8–6.275) | 5.4 (4.7–6.2) | 0.303 |
| HbA1c (%) | 6.25 (5.7–6.875) | 6.2 (5.6–6.8) | 6.3 (5.6–6.775) | 0.753 |
| iPTH (pg/mL) | 174 (109–222) | 134.5 (87.25–205.75) | 158 (113.5–210.5) | 0.315 |
| β2MG (mg/L) | 26.6 (22.55–29.75) | 26.8 (23.95–29.55) | 26 (23.3–29.25) | 0.63 |
| CRP (mg/dL) | 0.13 (0.05–0.296) | 0.1135 (0.04525–0.3525) | 0.08 (0.04–0.2035) | 0.060 |
| Hb (g/dL) | 11.2 (10.5–12) | 11.3 (10.7–11.8) | 11.3 (10.725–11.975) | 0.956 |
| Plasma Water Index | 2.64 (1.41–3.40) | 2.42 (1.53–3.30) | 2.39 (1.69–3.15) | 0.565 |
| KT/Vurea (D) | 1.74 (1.60–1.95) | 1.81 (1.65–2.07) | 1.88 (1.68–2.12) | 0.034 |
| NT-proBNP (pg/mL) | 3330 (1365–8175) | 3940 (1945–8870) | 3140 (1905–6615) | 0.541 |
| GNRI | 97.23 (90.06–103.67) | 96.34 (89.69–103.29) | 95.92 (89.59–101.82) | 0.90 |
| Test Item | Q1 Median (IQR) | Q2 Median (IQR) | Q3 Median (IQR) | p Value |
|---|---|---|---|---|
| Physical Functioning | 70 (40–80) | 80 (65–95) | 80 (65–95) | <0.001 |
| Role-Physical | 25 (0–100) | 75 (0–100) | 100 (50–100) | <0.001 |
| Bodily Pain | 57.5 (32.5–87.5) | 67.5 (53.125–90) | 77.5 (55–100) | <0.001 |
| General Health | 35 (22.5–50) | 50 (35–50) | 50 (40–60) | <0.001 |
| Vitality | 40 (25–57.5) | 55 (45–70) | 65 (45–80) | <0.001 |
| Social Functioning | 75 (37.5–87.5) | 75 (62.5–100) | 87.5 (62.5–100) | <0.001 |
| Role-Emotional | 33.33 (0–100) | 100 (0–100) | 100 (33.3–100) | <0.001 |
| Mental Health | 60 (42–76) | 68 (56–84) | 80 (60–88) | <0.001 |
| Symptom | 75 (59.4–85.4) | 83.3 (77.1–91.7) | 87.5 (79.7–94.8) | <0.001 |
| Effect of Kidney Disease | 71.9 (48.4–84.5) | 78.1 (66.4–87.5) | 84.4 (75–93.8) | <0.001 |
| Burden of Kidney Disease | 31.3 (6.25–46.9) | 37.5 (25–50) | 43.75 (31.3–56.3) | <0.001 |
| Work Status | 50 (0–100) | 50 (0–100) | 50 (0–100) | 0.281 |
| Cognitive Function | 86.7 (66.7–100) | 93.3 (80–100) | 93.3 (86.7–100) | <0.001 |
| Social Interaction | 80 (53.3–100) | 86.7 (73.3–100) | 93.3 (80–100) | <0.001 |
| Social Support | 66.7 (50–83.3) | 66.7 (66.7–83.3) | 83.3 (66.7–100) | <0.001 |
| Dialysis Staff Encouragement | 75 (50–87.5) | 75 (50–87.5) | 75 (62.5–100) | <0.001 |
| Patient Satisfaction | 83.3 (66.7–100) | 83.3 (66.7–100) | 83.3 (83.3–100) | <0.001 |
| QOL Domain | Model 1 (Unadjusted) [95% CI] (Std β) | p Value | Model 2 (Adjusted) [95% CI] (Std β) | p Value | Model 3 (Adjusted) [95% CI] (Std β) | p Value |
|---|---|---|---|---|---|---|
| Physical Functioning | 0.45 [0.34, 0.56] (0.40) | <0.001 | 0.44 [0.33, 0.55] (0.39) | <0.001 | 0.44 [0.33, 0.55] (0.39) | <0.001 |
| Role-Physical | 0.70 [0.51, 0.90] (0.36) | <0.001 | 0.67 [0.48, 0.87] (0.34) | <0.001 | 0.68 [0.49, 0.87] (0.35) | <0.001 |
| Bodily Pain | 0.47 [0.35, 0.59] (0.38) | <0.001 | 0.47 [0.35, 0.60] (0.38) | <0.001 | 0.48 [0.35, 0.60] (0.38) | <0.001 |
| General Health | 0.35 [0.27, 0.43] (0.42) | <0.001 | 0.34 [0.26, 0.42] (0.40) | <0.001 | 0.33 [0.25, 0.41] (0.40) | <0.001 |
| Vitality | 0.47 [0.37, 0.58] (0.43) | <0.001 | 0.47 [0.36, 0.57] (0.43) | <0.001 | 0.46 [0.36, 0.57] (0.42) | <0.001 |
| Social Functioning | 0.46 [0.33, 0.59] (0.35) | <0.001 | 0.47 [0.34, 0.61] (0.36) | <0.001 | 0.48 [0.35, 0.62] (0.37) | <0.001 |
| Role-Emotional | 0.70 [0.50, 0.90] (0.34) | <0.001 | 0.69 [0.49, 0.89] (0.34) | <0.001 | 0.71 [0.51, 0.92] (0.35) | <0.001 |
| Mental Health | 0.44 [0.34, 0.54] (0.41) | <0.001 | 0.44 [0.34, 0.54] (0.41) | <0.001 | 0.45 [0.34, 0.55] (0.42) | <0.001 |
| Symptom | 0.50 [0.41, 0.59] (0.51) | <0.001 | 0.49 [0.40, 0.58] (0.50) | <0.001 | 0.49 [0.40, 0.59] (0.50) | <0.001 |
| Effect of Kidney Disease on Daily Life | 0.51 [0.42, 0.61] (0.50) | <0.001 | 0.52 [0.42, 0.61] (0.50) | <0.001 | 0.53 [0.44, 0.63] (0.51) | <0.001 |
| Burden of Kidney Disease | 0.34 [0.24, 0.44] (0.33) | <0.001 | 0.32 [0.21, 0.42] (0.30) | <0.001 | 0.32 [0.22, 0.43] (0.31) | <0.001 |
| Work Status | 0.27 [0.08, 0.46] (0.15) | 0.006 | 0.25 [0.06, 0.43] (0.14) | 0.010 | 0.26 [0.07, 0.45] (0.14) | 0.006 |
| Cognitive Function | 0.46 [0.36, 0.56] (0.44) | <0.001 | 0.47 [0.37, 0.57] (0.44) | <0.001 | 0.47 [0.37, 0.58] (0.45) | <0.001 |
| Quality of Social Interaction | 0.47 [0.36, 0.57] (0.43) | <0.001 | 0.46 [0.36, 0.57] (0.42) | <0.001 | 0.46 [0.35, 0.57] (0.42) | <0.001 |
| Social Support | 0.53 [0.43, 0.64] (0.46) | <0.001 | 0.55 [0.44, 0.66] (0.47) | <0.001 | 0.54 [0.43, 0.65] (0.47) | <0.001 |
| Dialysis Staff Encouragement | 0.44 [0.33, 0.56] (0.37) | <0.001 | 0.45 [0.33, 0.57] (0.38) | <0.001 | 0.45 [0.32, 0.57] (0.37) | <0.001 |
| Patient Satisfaction with Dialysis Care | 0.50 [0.41, 0.60] (0.49) | <0.001 | 0.51 [0.41, 0.61] (0.50) | <0.001 | 0.51 [0.41, 0.61] (0.50) | <0.001 |
| Comparison | Model 1 > HR (95% CI), p Value | Model 2 > HR (95% CI), p Value | Model 3 > HR (95% CI), p Value |
|---|---|---|---|
| Q1 vs. Q3 | 2.58 (1.46–4.54), 0.001 | 2.85 (1.60–5.06), <0.001 | 2.04 (1.11–3.77), 0.023 |
| Q1 vs. Q2 | 2.37 (1.27–4.41), 0.006 | 2.39 (1.27–4.48), 0.007 | 1.88 (0.98–3.60), 0.058 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshida, N.; Tanaka, T.; Suzuki, Y.; Takahashi, S.; Hitaka, M.; Ishii, S.; Yamazaki, K.; Ohashi, Y. Sleep Quality and Its Association with Quality of Life and Mortality in Hemodialysis Patients. J. Clin. Med. 2025, 14, 8729. https://doi.org/10.3390/jcm14248729
Yoshida N, Tanaka T, Suzuki Y, Takahashi S, Hitaka M, Ishii S, Yamazaki K, Ohashi Y. Sleep Quality and Its Association with Quality of Life and Mortality in Hemodialysis Patients. Journal of Clinical Medicine. 2025; 14(24):8729. https://doi.org/10.3390/jcm14248729
Chicago/Turabian StyleYoshida, Norihito, Tatsuki Tanaka, Yusuke Suzuki, Sadamu Takahashi, Mai Hitaka, Shingo Ishii, Keisuke Yamazaki, and Yasushi Ohashi. 2025. "Sleep Quality and Its Association with Quality of Life and Mortality in Hemodialysis Patients" Journal of Clinical Medicine 14, no. 24: 8729. https://doi.org/10.3390/jcm14248729
APA StyleYoshida, N., Tanaka, T., Suzuki, Y., Takahashi, S., Hitaka, M., Ishii, S., Yamazaki, K., & Ohashi, Y. (2025). Sleep Quality and Its Association with Quality of Life and Mortality in Hemodialysis Patients. Journal of Clinical Medicine, 14(24), 8729. https://doi.org/10.3390/jcm14248729







