Use of Cangrelor in Türkiye: A Multicenter Real-Life Study
Abstract
1. Introduction
2. Methods
3. Statistical Analysis
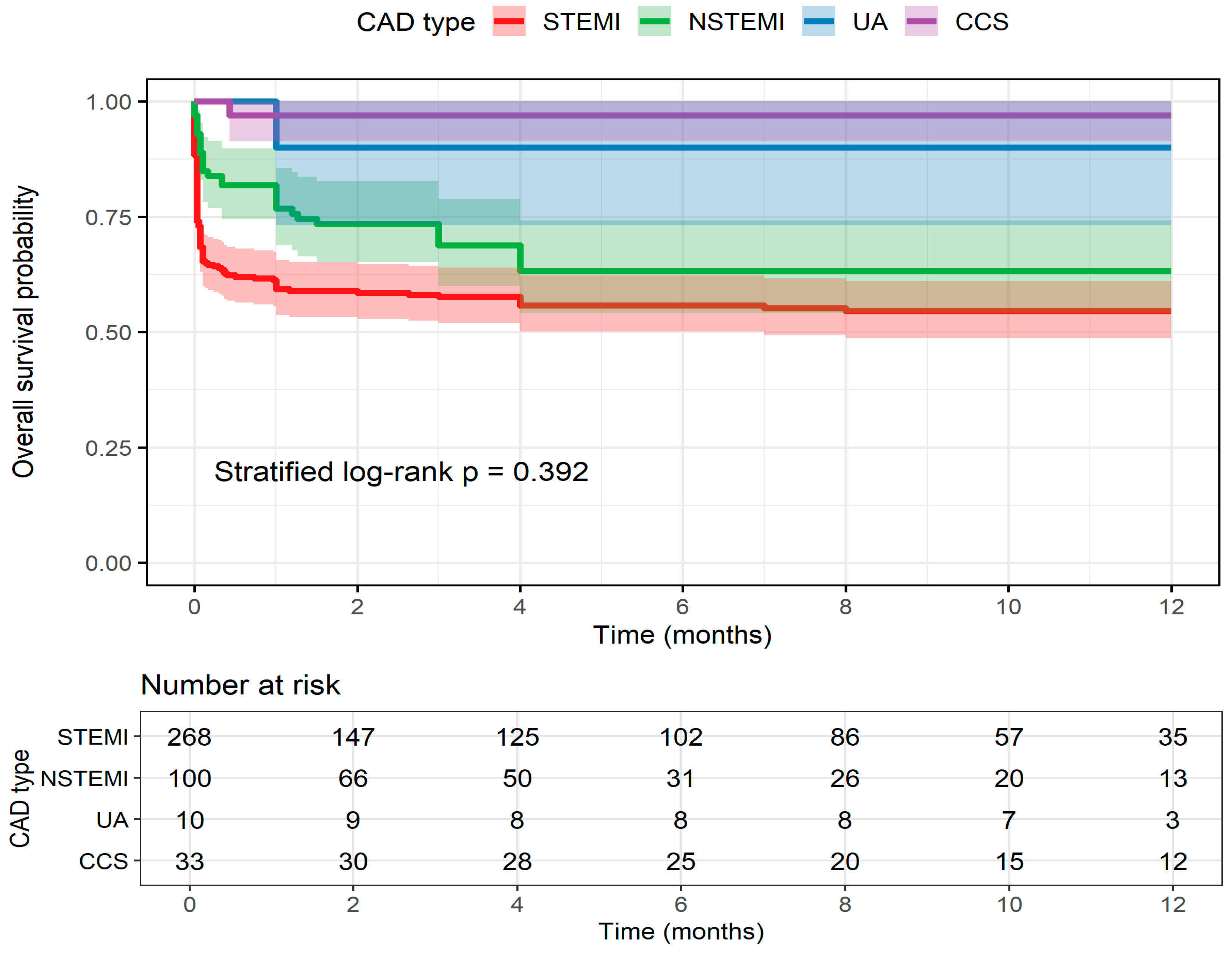
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826, Erratum in Eur. Heart J. 2024, 45, 1145. https://doi.org/10.1093/eurheartj/ehad870. [Google Scholar] [CrossRef] [PubMed]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur. Heart J. 2024, 45, 3415–3537, Erratum in Eur. Heart J. 2025, 46, 1565. https://doi.org/10.1093/eurheartj/ehaf079. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar] [CrossRef]
- Fox, K.A.; Mehta, S.R.; Peters, R.; Zhao, F.; Lakkis, N.; Gersh, B.J.; Yusuf, S. Clopidogrel in Unstable angina to prevent Recurrent ischemic Events Trial. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: The Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004, 110, 1202–1208. [Google Scholar] [CrossRef]
- Forsberg, J.; Bedard, E.; Mahmoud, S.H. Bioavailability of Orally Administered Drugs in Critically Ill Patients. J. Pharm. Pract. 2023, 36, 967–979. [Google Scholar] [CrossRef]
- Tavenier, A.H.; Hermanides, R.S.; Ottervanger, J.P.; Tolsma, R.; van Beurden, A.; Slingerland, R.J.; Ter Horst, P.G.J.; Gosselink, A.T.M.; Dambrink, J.E.; van Leeuwen, M.A.H.; et al. Impact of opioids on P2Y12 receptor inhibition in patients with ST-elevation myocardial infarction who are pre-treated with crushed ticagrelor: Opioids aNd crushed Ticagrelor In Myocardial infarction Evaluation (ON-TIME 3) trial. Eur. Heart J. Cardiovasc. Pharmacother. 2022, 8, 4–12. [Google Scholar] [CrossRef]
- Kordis, P.; Berden, J.; Mikuz, U.; Noc, M. Immediate Platelet Inhibition Strategy for Comatose Out-of-Hospital Cardiac Arrest Survivors Undergoing Percutaneous Coronary Intervention and Mild Therapeutic Hypothermia. J. Clin. Med. 2024, 13, 2121. [Google Scholar] [CrossRef]
- Harrington, R.A.; Stone, G.W.; McNulty, S.; White, H.D.; Lincoff, A.M.; Gibson, C.M.; Pollack, C.V.J.; Montalescot, G.; Mahaffey, K.W.; Kleiman, N.S.; et al. Platelet inhibition with cangrelor in patients undergoing PCI. N. Engl. J. Med. 2009, 361, 2318–2329. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Lincoff, A.M.; Gibson, C.M.; Stone, G.W.; McNulty, S.; Montalescot, G.; Kleiman, N.S.; Goodman, S.G.; White, H.D.; Mahaffey, K.W.; et al. Intravenous platelet blockade with cangrelor during PCI. N. Engl. J. Med. 2009, 361, 2330–2341. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Stone, G.W.; Mahaffey, K.W.; Gibson, C.M.; Steg, P.G.; Hamm, C.W.; Price, M.J.; Leonardi, S.; Gallup, D.; Bramucci, E.; et al. Effect of platelet in hibition with cangrelor during PCI on ischemic events. N. Engl. J. Med. 2013, 368, 1303–1313. [Google Scholar] [CrossRef]
- Rao, S.V.; O’Donoghue, M.L.; Ruel, M.; Rab, T.; Tamis-Holland, J.E.; Alexander, J.H.; Baber, U.; Baker, H.; Cohen, M.G.; Cruz-Ruiz, M.; et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients with Acute Coronary Syndromes: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2025, 151, e771–e862. [Google Scholar] [CrossRef]
- Available online: https://www.sgk.gov.tr/Duyuru/Detay/20230316-Degisiklik-Tebligi-Islenmis-Guncel-2013-SUT-2023-06-05-03-02-46 (accessed on 14 November 2025).
- Pasupathy, S.; Tavella, R.; McRae, S.; Beltrame, J.F. Myocardial Infarction With Non-obstructive Coronary Arteries—Diagnosis and Management. Eur. Cardiol. 2015, 10, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Bakhshi, H.; Gibson, C.M. MINOCA: Myocardial infarction no obstructive coronary artery disease. Am. Heart J. Plus 2023, 33, 100312. [Google Scholar] [CrossRef] [PubMed]
- Yalta, K.; Madias, J.E.; Kounis, N.G.; Y-Hassan, S.; Polovina, M.; Altay, S.; Mebazaa, A.; Yilmaz, M.B.; Lopatin, Y.; Mamas, M.A.; et al. Takotsubo Syndrome: An International Expert Consensus Report on Practical Challenges and Specific Conditions (Part-2: Specific Entities, Risk Stratification and Challenges After Recovery). Balkan Med. J. 2024, 41, 442–457. [Google Scholar] [CrossRef] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Wells, G.A.; Elliott, J.; Kelly, S.; Bai, Z.; Boucher, M.; Skidmore, B. Bleeding Classification System Definitions. 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542934/ (accessed on 25 November 2021).
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized bleeding definitions for cardiovascular clinical trials. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Levey, A.S.; Levin, A.; Kellum, J.A. Definition and classification of kidney diseases. Am. J. Kidney Dis. 2013, 61, 686–688. [Google Scholar] [CrossRef]
- Birinci, Ş. A Digital Opportunity for Patients to Manage Their Health: Turkey National Personal Health Record System (The e-Nabız). Balkan Med. J. 2023, 40, 215–221. [Google Scholar] [CrossRef]
- Akers, W.S.; Oh, J.J.; Oestreich, J.H.; Ferraris, S.; Wethington, M.; Steinhubl, S.R. Pharmacokinetics and pharmacodynamics of a bolus and infusion of cangrelor: A direct, parenteral P2Y12 receptor antagonist. J. Clin. Pharmacol. 2010, 50, 27–35. [Google Scholar] [CrossRef]
- Kubica, J.; Adamski, P.; Dobrzycki, S.; Gajda, R.; Gąsior, M.; Gierlotka, M.; Jaguszewski, M.; Legutko, J.; Lesiak, M.; Navarese, E.P.; et al. Cangrelor—Expanding therapeutic options in patients with acute coronary syndrome. Cardiol. J. 2024, 31, 133–146. [Google Scholar] [CrossRef]
- Bennar, W.; Garin, D.; Zhi, Y.; Schaffner, C.; Pittet, T.; Attinger, A.; Togni, M.; Cuculi, F.; Cook, S.; Bossard, M.; et al. Safety and Efficacy of Cangrelor in Acute Myocardial Infarction-Related Cardiogenic Shock with and Without Cardiac Arrest. Catheter. Cardiovasc. Interv. 2025, 106, 2395–2409. [Google Scholar] [CrossRef]
- Rollini, F.; Franchi, F. Cangrelor in Patients with Cardiogenic Shock or Cardiac Arrest. JACC Cardiovasc. Interv. 2025, 18, 863–865. [Google Scholar] [CrossRef] [PubMed]
- Ferlini, M.; Raone, L.; Bendotti, S.; Currao, A.; Primi, R.; Bongiorno, A.; Fava, C.; Dall’Oglio, L.; Adamo, M.; Ghiraldin, D.; et al. Cangrelor in Patients Undergoing Percutaneous Coronary Intervention After Out-of-Hospital Cardiac Arrest. J. Clin. Med. 2025, 14, 76. [Google Scholar] [CrossRef] [PubMed]
- Erol, M.K.; Kayıkçıoğlu, M.; Kılıçkap, M.; Arın, C.B.; Kurt, I.H.; Aktaş, I.; Güneş, Y.; Özkan, E.; Şen, T.; Ince, O.; et al. Baseline clinical characteristics and patient profile of the TURKMI registry: Results of a nation-wide acute myocardial infarction registry in Turkey. Anatol. J. Cardiol. 2020, 24, 43–53. [Google Scholar] [CrossRef]
- Tokgözoğlu, L.; Kayıkçıoğlu, M.; Altay, S.; Aydoğdu, S.; Barçın, C.; Bostan, C.; Çakmak, H.A.; Çatakoğlu, A.B.; Emet, S.; Ergene, O.; et al. EUROASPIRE-IV: Avrupa Kardiyoloji Derneği’nin koroner arter hastalarında yaşam tarzı, risk faktörleri ve tedavi yaklaşımı üzerine çalışması: Türkiye verileri [EUROASPIRE-IV: European Society of Cardiology study of lifestyle, risk factors, and treatment approaches in patients with coronary artery disease: Data from Turkey]. Turk Kardiyol. Dern. Ars. 2017, 45, 134–144. [Google Scholar]
- Schiele, F.; Gale, C.P.; Simon, T.; Fox, K.A.A.; Bueno, H.; Lettino, M.; Tubaro, M.; Puymirat, E.; Ferrières, J.; Meneveau, N.; et al. Assessment of Quality Indicators for Acute Myocardial Infarction in the FAST-MI (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) Registries. Circ. Cardiovasc. Qual. Outcomes 2017, 10, 003336. [Google Scholar] [CrossRef]
- Pitta, S.R.; Grzybowski, M.; Welch, R.D.; Frederick, P.D.; Wahl, R.; Zalenski, R.J. ST-segment depression on the initial electrocardiogram in acute myocardial infarction-prognostic significance and its effect on short-term mortality: A report from the National Registry of Myocardial Infarction (NRMI-2, 3, 4). Am. J. Cardiol. 2005, 95, 843–848. [Google Scholar] [CrossRef]
- Wilkinson, C.; Weston, C.; Timmis, A.; Quinn, T.; Keys, A.; Gale, C.P. The Myocardial Ischaemia National Audit Project (MINAP). Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 19–22. [Google Scholar] [CrossRef] [PubMed]
- De Sio, V.; Gragnano, F.; Cesaro, A.; Moscarella, E.; Guarnaccia, N.; Capolongo, A.; Maddaluna, P.; Verde, G.; Acerbo, V.; Scherillo, G.; et al. Cangrelor in percutaneous coronary interventions: Advances in evidence, clinical applications, and future directions. Expert Rev. Cardiovasc. Ther. 2025, 23, 507–519. [Google Scholar] [CrossRef] [PubMed]
- Salgia, A.; Krueger, C.K.; Gillette, M.A. Perioperative Antiplatelet Bridging with Cangrelor: A Cohort Study and Narrative Review. Ann. Pharmacother. 2023, 57, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Angiolillo, D.J.; Rollini, F.; Storey, R.F.; Bhatt, D.L.; James, S.; Schneider, D.J.; Sibbing, D.; So, D.Y.F.; Trenk, D.; Alexopoulos, D.; et al. International Expert Consensus on Switching Platelet P2Y12 Receptor-Inhibiting Therapies. Circulation 2017, 136, 1955–1975. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Calabrò, P.; Chirillo, F.; Rolfo, C.; Menozzi, A.; Capranzano, P.; Menichelli, M.; Nicolini, E.; Mauro, C.; Trani, C.; et al. Use of cangrelor in patients with acute coronary syndromes undergoing percutaneous coronary intervention: Study design and interim analysis of the ARCANGELO study. Clin. Cardiol. 2022, 45, 913–920. [Google Scholar] [CrossRef]
- De Luca, L.; Calabrò, P.; Capranzano, P.; Di Mario, C.; Chirillo, F.; Rolfo, C.; Menozzi, A.; Menichelli, M.; Bolognese, L.; Musumeci, G. Safety of cangrelor and transition to oral P2Y12 inhibitors in patients undergoing percutaneous coronary intervention: The ARCANGELO study. Eur. Heart J. Open 2023, 3, oead076. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Harrington, R.A.; Stone, G.W.; Deliargyris, E.N.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Menozzi, A.; Prats, J.; et al. Evaluation of Ischemic and Bleeding Risks Associated with 2 Parenteral Antiplatelet Strategies Comparing Cangrelor with Glycoprotein IIb/IIIa Inhibitors: An Exploratory Analysis from the CHAMPION Trials. JAMA Cardiol. 2017, 2, 127–135. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Harrington, R.A.; Stone, G.W.; Deliargyris, E.N.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Menozzi, A.; Prats, J.; et al. Cangrelor with and Without Glycoprotein IIb/IIIa Inhibitors in Patients Undergoing Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2017, 69, 176–185. [Google Scholar] [CrossRef]
- Capranzano, P.; Calabrò, P.; Musumeci, G.; Mario, C.D.; Chirillo, F.; Rolfo, C.; Menozzi, A.; Menichelli, M.; Maffeo, D.; Talanas, G.; et al. Use of Cangrelor in Older Patients: Findings from the itAlian pRospective Study on CANGrELOr Study. Am. J. Cardiol. 2025, 240, 31–37. [Google Scholar] [CrossRef]
- Capodanno, D.; Bhatt, D.L.; Gibson, C.M.; James, S.; Kimura, T.; Mehran, R.; Rao, S.V.; Steg, P.G.; Urban, P.; Valgimigli, M.; et al. Bleeding avoidance strategies in percutaneous coronary intervention. Nat. Rev. Cardiol. 2022, 19, 117–132. [Google Scholar] [CrossRef]
- Nanna, M.G.; Sutton, N.R.; Kochar, A.; Rymer, J.A.; Lowenstern, A.M.; Gackenbach, G.; Hummel, S.L.; Goyal, P.; Rich, M.W.; Kirkpatrick, J.N.; et al. Assessment and Management of Older Adults Undergoing PCI, Part 1: A JACC: Advances Expert Panel. JACC Adv. 2023, 2, 100389. [Google Scholar] [CrossRef]
- De Luca, G.; Nardin, M.; Algowhary, M.; Uguz, B.; Oliveira, D.C.; Ganyukov, V.; Zimbakov, Z.; Cercek, M.; Jensen, L.O.; Loh, P.H.; et al. Impact of hypertension on mortality in patients with ST-Elevation myocardial infarction undergoing primary angioplasty: Insights from the international multicenter ISACS-STEMI registry. J. Hypertens. 2025, 43, 246–254. [Google Scholar] [CrossRef]
- Akkuş, O.; Yadsıbaş, R.; Demirkıran, R.F.; Elitaş, V.; Bekler, Ö.; Şen, F.; Binokay, H.; Akkuş, G.; Okuyan, E. Changes in Acute Coronary Syndrome Clinic after the Devastating Earthquake in Türkiye. Anatol. J. Cardiol. 2024, 28, 446–453. [Google Scholar] [CrossRef]
- Gutierrez, J.A.; Harrington, R.A.; Blankenship, J.C.; Stone, G.W.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Généreux, P.; Prats, J.; et al. The effect of cangrelor and access site on ischaemic and bleeding events: Insights from CHAMPION PHOENIX. Eur. Heart J. 2016, 37, 1122–1130. [Google Scholar] [CrossRef]
- Uzun, F.; Güner, A.; Çizgici, A.Y.; Çiloğlu, K.; Aktürk, I.F. A Novel Modified Mini-Crush Technique for Complex Coronary Bifurcation Lesions: Controlled Balloon-Crush. Balkan Med. J. 2025, 42, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.J.; Okamoto, N.; Murphy, J.; Vengrenyuk, Y.; Sharma, S.K.; Kini, A.S. Management of calcified coronary artery bifurcation lesions. Catheter. Cardiovasc. Interv. 2021, 97, 1407–1416. [Google Scholar] [CrossRef]
- Şahin, A.; Doğan, Z.; Çinçin, A.; Gürel, E.; Sünbül, M.; Sayar, N. Stent Implantation Results in Long Lesions and Small Coronary Vessels. Inter. Cardio. Pers. 2025, 1, 6–12. [Google Scholar] [CrossRef]
- Zeymer, U.; Geisler, T.; Westermann, D.; Huber, K. The role of cangrelor in acute and high-risk PCI settings. Eur. Heart J. Cardiovasc. Pharmacother. 2025, 11, 540–551. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Steg, P.G.; Bhatt, D.L.; Capodanno, D.; Angiolillo, D.J. Cangrelor: Clinical Data, Contemporary Use, and Future Perspectives. J. Am. Heart Assoc. 2021, 10, e022125. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Evaluable Patients (n = 411) |
|---|---|
| Age (years) | 63.8 ± 12.7 |
| Sex | |
| Female | 98 (24%) |
| Male | 313 (76%) |
| Body mass index (kg/m2) | 28.3 ± 4.4 |
| Type of CAD | |
| STEMI | 268 (65%) |
| NSTEMI | 100 (24%) |
| UA | 10 (2.4%) |
| CCS | 33 (8.0%) |
| Indication for cangrelor | |
| Cardiogenic shock | 141 (34%) |
| Vomiting | 70 (17%) |
| Intubation | 113 (28%) |
| Dysphagia | 19 (4.6%) |
| Complex coronary intervention | 62 (15%) |
| Smoking | 193 (53%) |
| Hypertension | 255 (62%) |
| Diabetes mellitus | 189 (46%) |
| Hyperlipidemia | 200 (49%) |
| Family history | 163 (46%) |
| Prior MI | 106 (26%) |
| Prior PCI | 111 (27%) |
| Peripheral artery disease | 20 (4.9%) |
| Atrial fibrillation | 35 (8.5%) |
| Cerebrovascular disease | 27 (6.7%) |
| COPD | 38 (9.2%) |
| Gastrointestinal disease | 5 (1.3%) |
| CKD | 76 (18%) |
| Heart rate (bpm) | 86.0 [70.0; 105.0] |
| Systolic BP (mmHg) | 100.0 [80.0; 125.0] |
| Diastolic (mmHg) | 60.0 [45.0; 74.0] |
| Killip class at admission | |
| 1 | 185 (50%) |
| 2 | 52 (14%) |
| 3 | 22 (5.9%) |
| 4 | 111 (30%) |
| Hemoglobin (g/dL) | 13.0 ± 2.2 |
| eGFR (mL/min/1.73 m2) | 71.0 [50.0; 89.0] |
| LVEF (%) | 40.0 [30.0; 52.5] |
| Characteristic | Evaluable Patients (n = 411) |
|---|---|
| Catheter access site | |
| Femoral | 298 (72%) |
| Radial | 114 (28%) |
| No. of diseased vessels | |
| 1 | 172 (41%) |
| 2 | 139 (34%) |
| 3 | 95 (23%) |
| 4 | 4 (1.0%) |
| 5 | 1 (0.2%) |
| Culprit lesion vessel | |
| LAD | 216 (57%) |
| CX | 66 (17%) |
| RCA | 94 (25%) |
| LMCA | 3 (0.8%) |
| Diagonal | 3 (0.8%) |
| Bifurcation lesion | 71 (17%) |
| Type of the implanted stent | |
| DES | 376 (95%) |
| BMS | 11 (2.8%) |
| DCB | 7 (1.8%) |
| Stent brand/model | |
| Everolimus | 186 (54%) |
| Sirolimus | 73 (21%) |
| Rapamisin | 50 (14%) |
| Biolimus | 13 (3.8%) |
| Zotarolimus | 10 (2.9%) |
| Stent diameter (mm) | 3.0 [2.8; 3.5] |
| Total stent length (mm) | 29.0 [20.0; 44.0] |
| No. of implantend stents | 1.0 [1.0; 2.0] |
| PCI duration (min) | 39.0 [26.0; 55.0] |
| Contrast volume (mL) | 150.0 [110.0; 220.0] |
| Infusion time (min) | 2.0 [2.0; 2.0] |
| P2Y12 inhibitor type | |
| Clopidogrel | 231 (57%) |
| Ticagrelor | 172 (42%) |
| Prasugrel | 4 (1.0%) |
| P2Y12 initiation time (min) | 1.5 [1.0; 2.0] |
| GP IIb/IIIa use | 44 (11%) |
| Bleeding Event | Evaluable Patients (n = 411) |
|---|---|
| Bleeding severity at 48 h (BARC) | |
| No bleeding | 383 (94.0%) |
| Type 1 | 16 (3.9%) |
| Type 2 | 3 (0.7%) |
| Type 3a | 6 (1.5%) |
| Type 5a | 1 (0.2%) |
| Bleeding severity at 48 h (GUSTO) | |
| No bleeding | 386 (94.0%) |
| Mild | 15 (3.6%) |
| Moderate | 7 (1.7%) |
| Severe | 3 (0.7%) |
| Bleeding site | |
| Vascular access site | 8 (2.0%) |
| Hematuria | 7 (1.7%) |
| Oral cavity | 4 (1.0%) |
| Gastro-intestinal system | 3 (0.7%) |
| Pericardium | 1 (0.2%) |
| Lung | 1 (0.2%) |
| Intracranial | 1 (0.2%) |
| Aortic dissection | 1 (0.2%) |
| Transfusion required | 15 (3.7%) |
| Surgical intervention required | 1 (0.2%) |
| Bleeding severity at 1 month (BARC) | |
| No bleeding | 273 (97.0%) |
| Type 1 | 6 (2.1%) |
| Type 2 | 1 (0.4%) |
| Type 3a | 1 (0.4%) |
| Type 5a | 0 (0.0%) |
| Bleeding severity at 1 month (GUSTO) | |
| No bleeding | 273 (97.0%) |
| Mild | 6 (2.1%) |
| Moderate | 1 (0.4%) |
| Severe | 1 (0.4%) |
| Any bleeding during follow-up | 2 (0.8%) |
| Timepoint | Scale | Category | NSTEMI | STEMI | UA |
|---|---|---|---|---|---|
| 48 h | BARC | Type 1 | 5 (71.4%) | 10 (55.6%) | 1 (50%) |
| Type 2 | 1 (14.3%) | 2 (11.1%) | 1 (50%) | ||
| Type 3a | 1 (14.3%) | 5 (27.8%) | – | ||
| Type 5a | – | 1 (5.6%) | – | ||
| 48 h | GUSTO | Mild | 5 (83.3%) | 8 (47.1%) | – |
| Moderate | 1 (16.7%) | 6 (35.3%) | 2 (100%) | ||
| Severe | – | 3 (17.6%) | – | ||
| 1 month | BARC | Type 1 | 3 (75%) | 3 (75%) | – |
| Type 2 | – | 1 (25%) | – | ||
| Type 3a | 1 (25%) | – | – | ||
| 1 month | GUSTO (corrected) | Mild | 2 (66.7%) | 1 (33.3%) | 2 (100%) |
| Moderate | 1 (33.3%) | 2 (66.7%) | – | ||
| Severe | – | – | – |
| Variables | OR (95% CI) | p |
|---|---|---|
| Age (for every 1 year) | 1.04 (1.01–1.08) | 0.018 |
| Hypertension | 0.32 (0.14–0.73) | 0.007 |
| Potent P2Y12 (Ticagrelor/Prasugrel) | 2.17 (0.96–4.92) | 0.064 |
| Cardiogenic shock (Killip 4) | 1.55 (0.65–3.71) | 0.326 |
| Diabetes Mellitus | 1.47 (0.64–3.39) | 0.361 |
| CKD | 1.09 (0.39–3.05) | 0.876 |
| Gender (female) | 0.93 (0.35–2.44) | 0.878 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altay, S.; Gül, İ.; Aytemiz, F.; Kibar, M.; Süleymaoğlu, C.; Fedai, H.; Çatakoğlu, A.B.; Çetin, Ş.; Yöndem, S.; Yazıcıoğlu, M.V.; et al. Use of Cangrelor in Türkiye: A Multicenter Real-Life Study. J. Clin. Med. 2025, 14, 8728. https://doi.org/10.3390/jcm14248728
Altay S, Gül İ, Aytemiz F, Kibar M, Süleymaoğlu C, Fedai H, Çatakoğlu AB, Çetin Ş, Yöndem S, Yazıcıoğlu MV, et al. Use of Cangrelor in Türkiye: A Multicenter Real-Life Study. Journal of Clinical Medicine. 2025; 14(24):8728. https://doi.org/10.3390/jcm14248728
Chicago/Turabian StyleAltay, Servet, İlker Gül, Fatih Aytemiz, Metehan Kibar, Cuma Süleymaoğlu, Halil Fedai, Alp Burak Çatakoğlu, Şükrü Çetin, Selin Yöndem, Mehmet Vefik Yazıcıoğlu, and et al. 2025. "Use of Cangrelor in Türkiye: A Multicenter Real-Life Study" Journal of Clinical Medicine 14, no. 24: 8728. https://doi.org/10.3390/jcm14248728
APA StyleAltay, S., Gül, İ., Aytemiz, F., Kibar, M., Süleymaoğlu, C., Fedai, H., Çatakoğlu, A. B., Çetin, Ş., Yöndem, S., Yazıcıoğlu, M. V., Köprülü, D., Çetin, M., Yildiz, S. S., Çakal, B., Yayla, Ç., & Korkmaz, S. (2025). Use of Cangrelor in Türkiye: A Multicenter Real-Life Study. Journal of Clinical Medicine, 14(24), 8728. https://doi.org/10.3390/jcm14248728





