Controversies in Cavernous Malformation Management: A Comprehensive Review of Current Literature
Abstract
1. Introduction
2. Materials and Methods
3. Relevant Sections and Discussion
3.1. The Risk of Bleeding in CMs
3.2. Cavernous Malformation and Stereotactic Radiosurgery
3.2.1. Radiobiology of SRS Treatment for CMs
3.2.2. Treatment of Brainstem and Basal Ganglia CMs vs. Lobar Non-Eloquent CMs
3.2.3. Review of Recent Meta-Analysis
3.3. Cavernous Malformation and Epilepsy
3.4. Cavernous Malformation and Pregnancy
3.5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CM | Cavernous Malformation |
| CNS | Central Nervous System |
| ISSVA | International Society for the Study of Vascular Anomalies (ISSVA) |
| DVA | Venous Developmental Abnormality |
| SRS | Stereotactic Radiosurgery |
| ICH | Intracerebral Hemorrhage |
| RCTs | Randomized Controlled Trials |
| AREs | Adverse Radiation Effects |
References
- Kunimoto, K.; Yamamoto, Y.; Jinnin, M. ISSVA Classification of Vascular Anomalies and Molecular Biology. Int. J. Mol. Sci. 2022, 23, 2358. [Google Scholar] [CrossRef] [PubMed]
- Dulamea, A.O.; Lupescu, I.C. Cerebral Cavernous Malformations—An Overview on Genetics, Clinical Aspects and Therapeutic Strategies. J. Neurol. Sci. 2024, 461, 123044. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, H.E.; Solomon, R.A. Epidemiology of Cavernous Malformations. Handb. Clin. Neurol. 2017, 143, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Flemming, K.D.; Graff-Radford, J.; Aakre, J.; Kantarci, K.; Lanzino, G.; Brown, R.D.; Mielke, M.M.; Roberts, R.O.; Kremers, W.; Knopman, D.S.; et al. Population-Based Prevalence of Cerebral Cavernous Malformations in Older Adults: Mayo Clinic Study of Aging. JAMA Neurol. 2017, 74, 801–805. [Google Scholar] [CrossRef]
- Dammann, P.; Wrede, K.; Zhu, Y.; Matsushige, T.; Maderwald, S.; Umutlu, L.; Quick, H.H.; Hehr, U.; Rath, M.; Ladd, M.E.; et al. Correlation of the Venous Angioarchitecture of Multiple Cerebral Cavernous Malformations with Familial or Sporadic Disease: A Susceptibility-Weighted Imaging Study with 7-Tesla MRI. J. Neurosurg. 2017, 126, 570–577. [Google Scholar] [CrossRef]
- Hirota, K.; Akagawa, H.; Kikuchi, A.; Oka, H.; Hino, A.; Mitsuyama, T.; Sasaki, T.; Onda, H.; Kawamata, T.; Kasuya, H. KRIT1 Mutations in Three Japanese Pedigrees with Hereditary Cavernous Malformation. Hum. Genome Var. 2016, 3, 16032. [Google Scholar] [CrossRef]
- Brunereau, L.; Levy, C.; Laberge, S.; Houtteville, J.; Labauge, P. De Novo Lesions in Familial Form of Cerebral Cavernous Malformations: Clinical and MR Features in 29 Non-Hispanic Families. Surg. Neurol. 2000, 53, 475–482; discussion 482–483. [Google Scholar] [CrossRef]
- Abla, A.; Wait, S.D.; Uschold, T.; Lekovic, G.P.; Spetzler, R.F. Developmental Venous Anomaly, Cavernous Malformation, and Capillary Telangiectasia: Spectrum of a Single Disease. Acta Neurochir. 2008, 150, 487–489; discussion 489. [Google Scholar] [CrossRef]
- Zabramski, J.M.; Wascher, T.M.; Spetzler, R.F.; Johnson, B.; Golfinos, J.; Drayer, B.P.; Brown, B.; Rigamonti, D.; Brown, G. The natural history of familial cavernous malformations: Results of an ongoing study. J. Neurosurg. 1994, 80, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Nikoubashman, O.; Di Rocco, F.; Davagnanam, I.; Mankad, K.; Zerah, M.; Wiesmann, M. Prospective Hemorrhage Rates of Cerebral Cavernous Malformations in Children and Adolescents Based on MRI Appearance. AJNR Am. J. Neuroradiol. 2015, 36, 2177–2183. [Google Scholar] [CrossRef]
- Daglioglu, E.; Ergungor, F.; Polat, E.; Nacar, O. Microsurgical Resection of Supratentorial Cerebral Cavernomas. Turk. Neurosurg. 2010, 20, 348–352. [Google Scholar] [CrossRef]
- Rosenow, F.; Alonso-Vanegas, M.A.; Baumgartner, C.; Blümcke, I.; Carreño, M.; Gizewski, E.R.; Hamer, H.M.; Knake, S.; Kahane, P.; Lüders, H.O.; et al. Cavernoma-related Epilepsy: Review and Recommendations for Management—Report of the Surgical Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2013, 54, 2025–2035. [Google Scholar] [CrossRef] [PubMed]
- Bertalanffy, H.; Gilsbach, J.M.; Eggert, H.R.; Seeger, W. Microsurgery of Deep-Seated Cavernous Angiomas: Report of 26 Cases. Acta Neurochir. 1991, 108, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Kivelev, J.; Niemelä, M.; Hernesniemi, J. Treatment Strategies in Cavernomas of the Brain and Spine. J. Clin. Neurosci. 2012, 19, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Al-Shahi Salman, R.; Berg, M.J.; Morrison, L.; Awad, I.A. Angioma Alliance Scientific Advisory Board Hemorrhage from Cavernous Malformations of the Brain: Definition and Reporting Standards. Angioma Alliance Scientific Advisory Board. Stroke 2008, 39, 3222–3230. [Google Scholar] [CrossRef]
- Akers, A.L.; Albanese, J.; Alcazar-Felix, R.J.; Al-Shahi Salman, R.; Awad, I.A.; Connolly, E.S.; Danehy, A.; Flemming, K.D.; Gordon, E.; Hage, S.; et al. Guidelines for the Diagnosis and Clinical Management of Cavernous Malformations of the Brain and Spinal Cord: Consensus Recommendations Based on a Systematic Literature Review by the Alliance to Cure Cavernous Malformation Clinical Advisory Board Experts Panel. Neurosurgery 2025. [Google Scholar] [CrossRef]
- Idiculla, P.S.; Gurala, D.; Philipose, J.; Rajdev, K.; Patibandla, P. Cerebral Cavernous Malformations, Developmental Venous Anomaly, and Its Coexistence: A Review. Eur. Neurol. 2020, 83, 360–368. [Google Scholar] [CrossRef]
- Moriarity, J.L.; Clatterbuck, R.E.; Rigamonti, D. The Natural History of Cavernous Malformations. Neurosurg. Clin. N. Am. 1999, 10, 411–417. [Google Scholar] [CrossRef]
- Chen, B.; Herten, A.; Saban, D.; Rauscher, S.; Radbruch, A.; Schmidt, B.; Zhu, Y.; Jabbarli, R.; Wrede, K.H.; Kleinschnitz, C.; et al. Hemorrhage from Cerebral Cavernous Malformations: The Role of Associated Developmental Venous Anomalies. Neurology 2020, 95, e89–e96. [Google Scholar] [CrossRef]
- Aboian, M.S.; Daniels, D.J.; Rammos, S.K.; Pozzati, E.; Lanzino, G. The Putative Role of the Venous System in the Genesis of Vascular Malformations. Neurosurg. Focus 2009, 27, E9. [Google Scholar] [CrossRef]
- Karaaslan, B.; Gülsuna, B.; Erol, G.; Dağli, Ö.; Emmez, H.; Kurt, G.; Çeltikçi, E.; Börcek, A.Ö. Stereotactic Radiosurgery for Cerebral Cavernous Malformation: Comparison of Hemorrhage Rates before and after Stereotactic Radiosurgery. J. Neurosurg. 2022, 136, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Brinjikji, W.; El-Masri, A.E.-R.; Wald, J.T.; Flemming, K.D.; Lanzino, G. Prevalence of Cerebral Cavernous Malformations Associated with Developmental Venous Anomalies Increases with Age. Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg. 2017, 33, 1539–1543. [Google Scholar] [CrossRef] [PubMed]
- Mooney, M.A.; Zabramski, J.M. Developmental Venous Anomalies. Handb. Clin. Neurol. 2017, 143, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Tasiou, A.; Brotis, A.G.; Kalogeras, A.; Tzerefos, C.; Alleyne, C.H.; Andreou, A.; Demetriades, A.K.; Foroglou, N.; Friedlander, R.M.; Karlsson, B.; et al. Cavernous Malformations of the Central Nervous System: An International Consensus Statement. Brain Spine 2023, 3, 102707. [Google Scholar] [CrossRef]
- Tos, S.M.; Shaaban, A.; Mantziaris, G.; Dumot, C.; Kotecha, R.; Fariselli, L.; Gorgulho, A.; Levivier, M.; Ma, L.; Paddick, I.; et al. Stereotactic Radiosurgery for Intracranial Cavernous Malformations: International Stereotactic Radiosurgery Society, Systematic Review, Meta-Analysis, and Practice Guidelines. World Neurosurg. 2024, 192, e366–e401. [Google Scholar] [CrossRef]
- Nagy, G.; Kemeny, A.A. Radiosurgery for Cerebral Cavernomas. J. Neurosurg. Sci. 2015, 59, 295–306. [Google Scholar]
- Taslimi, S.; Modabbernia, A.; Amin-Hanjani, S.; Barker, F.G.; Macdonald, R.L. Natural History of Cavernous Malformation: Systematic Review and Meta-Analysis of 25 Studies. Neurology 2016, 86, 1984–1991. [Google Scholar] [CrossRef]
- Horne, M.A.; Flemming, K.D.; Su, I.-C.; Stapf, C.; Jeon, J.P.; Li, D.; Maxwell, S.S.; White, P.; Christianson, T.J.; Agid, R.; et al. Angioma Alliance Scientific Advisory Board. Clinical course of untreated cerebral cavernous malformations: A meta-analysis of individual patient data. Lancet Neurol. 2016, 15, 166–173. [Google Scholar] [CrossRef]
- Lee, C.-C.; Wang, W.-H.; Yang, H.-C.; Lin, C.-J.; Wu, H.-M.; Lin, Y.-Y.; Hu, Y.-S.; Chen, C.-J.; Chen, Y.-W.; Chou, C.-C.; et al. Gamma Knife Radiosurgery for Cerebral Cavernous Malformation. Sci. Rep. 2019, 9, 19743. [Google Scholar] [CrossRef]
- Bubenikova, A.; Skalicky, P.; Benes, V.; Benes, V.; Bradac, O. Overview of Cerebral Cavernous Malformations: Comparison of Treatment Approaches. J. Neurol. Neurosurg. Psychiatry 2022, 93, 475–480. [Google Scholar] [CrossRef]
- Mouchtouris, N.; Chalouhi, N.; Chitale, A.; Starke, R.M.; Tjoumakaris, S.I.; Rosenwasser, R.H.; Jabbour, P.M. Management of Cerebral Cavernous Malformations: From Diagnosis to Treatment. Sci. World J. 2015, 2015, 808314. [Google Scholar] [CrossRef] [PubMed]
- 32 Moultrie, F.; Horne, M.A.; Josephson, C.B.; Hall, J.M.; Counsell, C.E.; Bhattacharya, J.J.; Papanastassiou, V.; Sellar, R.J.; Warlow, C.P.; Murray, G.D.; et al. Outcome after Surgical or Conservative Management of Cerebral Cavernous Malformations. Neurology 2014, 83, 582–589. [Google Scholar] [CrossRef] [PubMed]
- 33 Kondziolka, D.; Lunsford, L.D.; Flickinger, J.C.; Kestle, J.R. Reduction of Hemorrhage Risk after Stereotactic Radiosurgery for Cavernous Malformations. J. Neurosurg. 1995, 83, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Al-Shahi Salman, R.; Hall, J.M.; Horne, M.A.; Moultrie, F.; Josephson, C.B.; Bhattacharya, J.J.; Counsell, C.E.; Murray, G.D.; Papanastassiou, V.; Ritchie, V.; et al. Untreated Clinical Course of Cerebral Cavernous Malformations: A Prospective, Population-Based Cohort Study. Lancet Neurol. 2012, 11, 217–224. [Google Scholar] [CrossRef]
- Barker, F.G.; Amin-Hanjani, S.; Butler, W.E.; Lyons, S.; Ojemann, R.G.; Chapman, P.H.; Ogilvy, C.S. Temporal Clustering of Hemorrhages from Untreated Cavernous Malformations of the Central Nervous System. Neurosurgery 2001, 49, 15–24; discussion 24–25. [Google Scholar] [CrossRef]
- Poorthuis, M.H.F.; Klijn, C.J.M.; Algra, A.; Rinkel, G.J.E.; Al-Shahi Salman, R. Treatment of Cerebral Cavernous Malformations: A Systematic Review and Meta-Regression Analysis. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1319–1323. [Google Scholar] [CrossRef]
- Lee, C.-C.; Pan, D.H.-C.; Chung, W.-Y.; Liu, K.-D.; Yang, H.-C.; Wu, H.-M.; Guo, W.-Y.; Shih, Y.-H. Brainstem Cavernous Malformations: The Role of Gamma Knife Surgery. J. Neurosurg. 2012, 117, 164–169. [Google Scholar] [CrossRef]
- Wen, R.; Shi, Y.; Gao, Y.; Xu, Y.; Xiong, B.; Li, D.; Gong, F.; Wang, W. The Efficacy of Gamma Knife Radiosurgery for Cavernous Malformations: A Meta-Analysis and Review. World Neurosurg. 2019, 123, 371–377. [Google Scholar] [CrossRef]
- Pollock, B.E.; Garces, Y.I.; Stafford, S.L.; Foote, R.L.; Schomberg, P.J.; Link, M.J. Stereotactic Radiosurgery for Cavernous Malformations. J. Neurosurg. 2000, 93, 987–991. [Google Scholar] [CrossRef]
- Pollock, B.E. Radiosurgery for Cavernous Malformations: Theory and Practice. Clin. Neurosurg. 2008, 55, 97–100. [Google Scholar]
- Fuetsch, M.; El Majdoub, F.; Hoevels, M.; Müller, R.P.; Sturm, V.; Maarouf, M. Stereotactic LINAC Radiosurgery for the Treatment of Brainstem Cavernomas. Strahlenther. Onkol. 2012, 188, 311–316. [Google Scholar] [CrossRef]
- Bertalanffy, H.; Benes, L.; Miyazawa, T.; Alberti, O.; Siegel, A.M.; Sure, U. Cerebral Cavernomas in the Adult. Review of the Literature and Analysis of 72 Surgically Treated Patients. Neurosurg. Rev. 2002, 25, 1–53; discussion 54–55. [Google Scholar] [CrossRef] [PubMed]
- Bertalanffy, H.; Gerganov, V.M. Microsurgical or Radiosurgical Management of Intracranial Cavernomas. Acta Neurochir. Suppl. 2013, 116, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.; Hodgson, T.J.; Seaman, S.; Kemeny, A.A.; Forster, D.M. Stereotactic Radiosurgery and the Risk of Haemorrhage from Cavernous Malformations. Br. J. Neurosurg. 2000, 14, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Liscák, R.; Vladyka, V.; Simonová, G.; Vymazal, J.; Novotny, J. Gamma Knife Radiosurgery of the Brain Stem Cavernomas. Minim. Invasive Neurosurg. 2000, 43, 201–207. [Google Scholar] [CrossRef]
- Dumot, C.; Mantziaris, G.; Pikis, S.; Dayawansa, S.; Xu, Z.; Samanci, Y.; Ardor, G.D.; Peker, S.; Nabeel, A.M.; Reda, W.A.; et al. Epilepsy Associated with Cerebral Cavernous Malformations Managed with Stereotactic Radiosurgery: An International, Multicenter Study. J. Neurol. 2023, 270, 5048–5056. [Google Scholar] [CrossRef]
- Chalouhi, N.; Jabbour, P.; Andrews, D.W. Stereotactic Radiosurgery for Cavernous Malformations: Is It Effective? World Neurosurg. 2013, 80, e185–e186. [Google Scholar] [CrossRef]
- Sager, O.; Beyzadeoglu, M.; Dincoglan, F.; Gamsiz, H.; Demiral, S.; Uysal, B.; Oysul, K.; Dirican, B.; Sirin, S. Evaluation of Linear Accelerator-Based Stereotactic Radiosurgery in the Management of Glomus Jugulare Tumors. Tumori 2014, 100, 184–188. [Google Scholar] [CrossRef]
- Lindquist, C.; Guo, W.Y.; Karlsson, B.; Steiner, L. Radiosurgery for Venous Angiomas. J. Neurosurg. 1993, 78, 531–536. [Google Scholar] [CrossRef]
- Chung, M.-W.; Chuang, C.-C.; Wang, C.-C.; Chen, H.-C.; Hsu, P.-W. Prognostic Factors Analysis for Intracranial Cavernous Malformations Treated with Linear Accelerator Stereotactic Radiosurgery. Life 2022, 12, 1363. [Google Scholar] [CrossRef]
- Lunsford, L.D.; Khan, A.A.; Niranjan, A.; Kano, H.; Flickinger, J.C.; Kondziolka, D. Stereotactic Radiosurgery for Symptomatic Solitary Cerebral Cavernous Malformations Considered High Risk for Resection. J. Neurosurg. 2010, 113, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Monaco, E.A.; Khan, A.A.; Niranjan, A.; Kano, H.; Grandhi, R.; Kondziolka, D.; Flickinger, J.C.; Lunsford, L.D. Stereotactic Radiosurgery for the Treatment of Symptomatic Brainstem Cavernous Malformations. Neurosurg. Focus 2010, 29, E11. [Google Scholar] [CrossRef] [PubMed]
- Niranjan, A.; Lunsford, L.D. Stereotactic Radiosurgery Guidelines for the Management of Patients with Intracranial Cavernous Malformations. Prog. Neurol. Surg. 2013, 27, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Nagy, G.; Kemeny, A.A. Stereotactic Radiosurgery of Intracranial Cavernous Malformations. Neurosurg. Clin. N. Am. 2013, 24, 575–589. [Google Scholar] [CrossRef]
- Akers, A.; Al-Shahi Salman, R.; A Awad, I.; Dahlem, K.; Flemming, K.; Hart, B.; Kim, H.; Jusue-Torres, I.; Kondziolka, D.; Lee, C.; et al. Synopsis of Guidelines for the Clinical Management of Cerebral Cavernous Malformations: Consensus Recommendations Based on Systematic Literature Review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel. Neurosurgery 2017, 80, 665–680. [Google Scholar] [CrossRef]
- Sandmann, A.C.A.; Kempeneers, M.A.; van den Berg, R.; Verbaan, D.; Vandertop, W.P.; Coutinho, J.M. Clinical Course of Patients with Conservatively Managed Cerebral Cavernous Malformations. Eur. Stroke J. 2024, 9, 667–675. [Google Scholar] [CrossRef]
- Flemming, K.D.; Link, M.J.; Christianson, T.J.H.; Brown, R.D. Prospective Hemorrhage Risk of Intracerebral Cavernous Malformations. Neurology 2012, 78, 632–636. [Google Scholar] [CrossRef]
- Dammann, P.; Jabbarli, R.; Wittek, P.; Oppong, M.D.; Kneist, A.; Zhu, Y.; Wrede, K.; Müller, O.; Forsting, M.; Sure, U. Solitary Sporadic Cerebral Cavernous Malformations: Risk Factors of First or Recurrent Symptomatic Hemorrhage and Associated Functional Impairment. World Neurosurg. 2016, 91, 73–80. [Google Scholar] [CrossRef]
- Loan, J.J.M.; Bacon, A.; van Beijnum, J.; Bhatt, P.; Bjornson, A.; Broomes, N.; Bullen, A.; Bulters, D.; Cahill, J.; Chavredakis, E.; et al. Cavernomas A Randomised Effectiveness (CARE) pilot trial collaborators. Feasibility of comparing medical management and surgery (with neurosurgery or stereotactic radiosurgery) with medical management alone in people with symptomatic brain cavernoma—Protocol for the Cavernomas: A Randomised Effectiveness (CARE) pilot trial. BMJ Open. 2023, 13, e075187. [Google Scholar] [CrossRef] [PubMed]
- Nyáry, I.; Major, O.; Hanzély, Z.; Szeifert, G.T. Histopathological Findings in a Surgically Resected Thalamic Cavernous Hemangioma 1 Year after 40-Gy Irradiation. J. Neurosurg. 2005, 102, 56–58. [Google Scholar] [CrossRef]
- Szeifert, G.T.; Levivier, M.; Lorenzoni, J.; Nyáry, I.; Major, O.; Kemeny, A.A. Morphological Observations in Brain Arteriovenous Malformations after Gamma Knife Radiosurgery. Prog. Neurol. Surg. 2013, 27, 119–129. [Google Scholar] [CrossRef]
- Shin, S.S.; Murdoch, G.; Hamilton, R.L.; Faraji, A.H.; Kano, H.; Zwagerman, N.T.; Gardner, P.A.; Lunsford, L.D.; Friedlander, R.M. Pathological Response of Cavernous Malformations Following Radiosurgery. J. Neurosurg. 2015, 123, 938–944. [Google Scholar] [CrossRef]
- Moeller, B.J.; Cao, Y.; Li, C.Y.; Dewhirst, M.W. Radiation Activates HIF-1 to Regulate Vascular Radiosensitivity in Tumors: Role of Reoxygenation, Free Radicals, and Stress Granules. Cancer Cell 2004, 5, 429–441. [Google Scholar] [CrossRef] [PubMed]
- Park, C.-M.; Park, M.-J.; Kwak, H.-J.; Lee, H.-C.; Kim, M.-S.; Lee, S.-H.; Park, I.-C.; Rhee, C.H.; Hong, S.-I. Ionizing Radiation Enhances Matrix Metalloproteinase-2 Secretion and Invasion of Glioma Cells through Src/Epidermal Growth Factor Receptor-Mediated P38/Akt and Phosphatidylinositol 3-Kinase/Akt Signaling Pathways. Cancer Res. 2006, 66, 8511–8519. [Google Scholar] [CrossRef] [PubMed]
- Harat, M.; Lebioda, A.; Lasota, J.; Makarewicz, R. Evaluation of Brain Edema Formation Defined By MRI After LINAC-Based Stereotactic Radiosurgery. Radiol. Oncol. 2017, 51, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Nagy, G.; Yianni, J.; Bhattacharyya, D.; Rowe, J.G.; Kemeny, A.A.; Radatz, M.W.R. Repeat Radiosurgery Treatment After Cavernous Malformation Radiosurgery. World Neurosurg. 2018, 118, e296–e303. [Google Scholar] [CrossRef]
- Campbell, P.G.; Jabbour, P.; Yadla, S.; Awad, I.A. Emerging Clinical Imaging Techniques for Cerebral Cavernous Malformations: A Systematic Review. Neurosurg. Focus 2010, 29, E6. [Google Scholar] [CrossRef]
- Lunsford, L.D.; Niranjan, A.; Kano, H.; Kondziolka, D. The Technical Evolution of Gamma Knife Radiosurgery for Arteriovenous Malformations. Prog. Neurol. Surg. 2013, 27, 22–34. [Google Scholar] [CrossRef]
- Shanker, M.D.; Webber, R.; Pinkham, M.B.; Huo, M.; Olson, S.; Hall, B.; Jayalath, R.; Watkins, T.; Foote, M.C. Gamma Knife® Stereotactic Radiosurgery for Intracranial Cavernous Malformations. J. Clin. Neurosci. 2022, 106, 96–102. [Google Scholar] [CrossRef]
- Pandey, P.; Westbroek, E.M.; Gooderham, P.A.; Steinberg, G.K. Cavernous Malformation of Brainstem, Thalamus, and Basal Ganglia: A Series of 176 Patients. Neurosurgery 2013, 72, 573–589; discussion 588–589. [Google Scholar] [CrossRef]
- Gross, B.A.; Batjer, H.H.; Awad, I.A.; Bendok, B.R.; Du, R. Brainstem Cavernous Malformations: 1390 Surgical Cases from the Literature. World Neurosurg. 2013, 80, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Almefty, K.K.; Spetzler, R.F. Management of Brainstem Cavernous Malformations. World Neurosurg. 2015, 83, 317–319. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.-Y.; Li, D.; Song, L.-R.; Liu, P.-P.; Wu, Z.-Y.; Wang, L.; Zhang, L.-W.; Zhang, J.-T.; Wu, Z. Nomogram for Predicting an Individual Prospective Hemorrhage Risk in Untreated Brainstem Cavernous Malformations. J. Neurosurg. 2023, 138, 910–921. [Google Scholar] [CrossRef] [PubMed]
- Gross, B.A.; Batjer, H.H.; Awad, I.A.; Bendok, B.R. Cavernous Malformations of the Basal Ganglia and Thalamus. Neurosurgery 2009, 65, 7–18; discussion 18–19. [Google Scholar] [CrossRef]
- Walcott, B.P.; Choudhri, O.; Lawton, M.T. Brainstem Cavernous Malformations: Natural History versus Surgical Management. J. Clin. Neurosci. 2016, 32, 164–165. [Google Scholar] [CrossRef]
- Kearns, K.N.; Chen, C.-J.; Tvrdik, P.; Park, M.S.; Kalani, M.Y.S. Outcomes of Basal Ganglia and Thalamic Cavernous Malformation Surgery: A Meta-Analysis. J. Clin. Neurosci. 2020, 73, 209–214. [Google Scholar] [CrossRef]
- Hori, T.; Chernov, M.; Alshebib, Y.A.; Kubota, Y.; Matsuo, S.; Shiramizu, H.; Okada, Y. Long-Term Outcomes after Surgery for Brainstem Cavernous Malformations: Analysis of 46 Consecutive Cases. J. Neurosurg. 2023, 138, 900–909. [Google Scholar] [CrossRef]
- Gao, X.; Yue, K.; Sun, J.; Cao, Y.; Zhao, B.; Zhang, H.; Dai, S.; Zhang, L.; Luo, P.; Jiang, X. Microsurgery vs. Gamma Knife Radiosurgery for the Treatment of Brainstem Cavernous Malformations: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 600461. [Google Scholar] [CrossRef]
- Nagy, G.; Razak, A.; Rowe, J.G.; Hodgson, T.J.; Coley, S.C.; Radatz, M.W.R.; Patel, U.J.; Kemeny, A.A. Stereotactic Radiosurgery for Deep-Seated Cavernous Malformations: A Move toward More Active, Early Intervention. Clinical Article. J. Neurosurg. 2010, 113, 691–699. [Google Scholar] [CrossRef]
- Park, S.-H.; Hwang, S.-K. Gamma Knife Radiosurgery for Symptomatic Brainstem Intra-Axial Cavernous Malformations. World Neurosurg. 2013, 80, e261–e266. [Google Scholar] [CrossRef]
- Lee, S.H.; Choi, H.J.; Shin, H.S.; Choi, S.K.; Oh, I.H.; Lim, Y.J. Gamma Knife Radiosurgery for Brainstem Cavernous Malformations: Should a Patient Wait for the Rebleed? Acta Neurochir. 2014, 156, 1937–1946. [Google Scholar] [CrossRef] [PubMed]
- Aboukais, R.; Estrade, L.; Devos, P.; Blond, S.; Lejeune, J.-P.; Reyns, N. Gamma Knife Radiosurgery of Brainstem Cavernous Malformations. Stereotact. Funct. Neurosurg. 2016, 94, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lim, Y.J. Stereotactic Radiosurgery for Cavernous Malformations: Prejudice from Ignorance. Acta Neurochir. 2015, 157, 51–52. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Flemming, K.D.; Nelson, J.A.; Lui, A.; Majersik, J.J.; Cruz, M.D.; Zabramski, J.; Trevizo, O.; Lanzino, G.; Zafar, A.; et al. Baseline Characteristics of Patients With Cavernous Angiomas With Symptomatic Hemorrhage in Multisite Trial Readiness Project. Stroke 2021, 52, 3829–3838. [Google Scholar] [CrossRef]
- Dayawansa, S.; Dumot, C.; Mantziaris, G.; Xu, Z.; Pikis, S.; Peker, S.; Samanci, Y.; Ardor, G.D.; Nabeel, A.M.; Reda, W.A.; et al. Stereotactic Radiosurgery (SRS) for Patients with Brainstem Cerebral Cavernous Malformations (CCMs): An International, Multicentric Study. Sci. Rep. 2024, 14, 25933. [Google Scholar] [CrossRef]
- Fotakopoulos, G.; Andrade-Barazarte, H.; Kivelev, J.; Tjahjadi, M.; Goehre, F.; Hernesniemi, J. Brainstem Cavernous Malformations Management: Microsurgery vs. Radiosurgery, a Meta-Analysis. Front. Surg. 2021, 8, 630134. [Google Scholar] [CrossRef]
- Al-Shalchy, A.K.; Al-Taie, R.H.; Al-Rubaye, A.H.; Patel, S.; Algabri, M.H.; Ismail, M. Brainstem Cavernous Malformations: A Systematic Review and Meta-Analysis. World Neurosurg. 2025, 203, 124452. [Google Scholar] [CrossRef] [PubMed]
- Nagy, G.; Stokes, S.S.; Erőss, L.G.; Bhattacharyya, D.; Yianni, J.; Rowe, J.G.; Kemeny, A.A.; Radatz, M.W.R. Contemporary Radiosurgery of Cerebral Cavernous Malformations: Part 2. Treatment Outcome for Hemispheric Lesions. J. Neurosurg. 2019, 130, 1826–1834. [Google Scholar] [CrossRef]
- Poorthuis, M.H.F.; Rinkel, L.A.; Lammy, S.; Al-Shahi Salman, R. Stereotactic Radiosurgery for Cerebral Cavernous Malformations: A Systematic Review. Neurology 2019, 93, e1971–e1979. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, K.H.; Lee, M.H.; Lee, J.-I. Stereotactic Radiosurgery for Brainstem Cavernous Malformations: An Updated Systematic Review and Meta-Analysis. World Neurosurg. 2019, 130, e648–e659. [Google Scholar] [CrossRef]
- Li, D.; Jiao, Y.-M.; Wang, L.; Lin, F.-X.; Wu, J.; Tong, X.-Z.; Wang, S.; Cao, Y. Surgical Outcome of Motor Deficits and Neurological Status in Brainstem Cavernous Malformations Based on Preoperative Diffusion Tensor Imaging: A Prospective Randomized Clinical Trial. J. Neurosurg. 2019, 130, 286–301. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Park, S.-H. Systemic Expression of Vascular Endothelial Growth Factor in Patients with Cerebral Cavernous Malformation Treated by Stereotactic Radiosurgery. J. Korean Neurosurg. Soc. 2016, 59, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Harris, L.; Poorthuis, M.H.F.; Grover, P.; Kitchen, N.; Al-Shahi Salman, R. Surgery for Cerebral Cavernous Malformations: A Systematic Review and Meta-Analysis. Neurosurg. Rev. 2022, 45, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Washington, C.W.; McCoy, K.E.; Zipfel, G.J. Update on the Natural History of Cavernous Malformations and Factors Predicting Aggressive Clinical Presentation. Neurosurg. Focus 2010, 29, E7. [Google Scholar] [CrossRef]
- Klostranec, J.M.; Krings, T. Neuroimaging of Cerebral Cavernous Malformations. J. Neurosurg. Sci. 2015, 59, 221–235. [Google Scholar]
- Ruan, D.; Yu, X.-B.; Shrestha, S.; Wang, L.; Chen, G. The Role of Hemosiderin Excision in Seizure Outcome in Cerebral Cavernous Malformation Surgery: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0136619. [Google Scholar] [CrossRef]
- Dziedzic, T.A.; Koczyk, K.; Nowak, A.; Maj, E.; Marchel, A. Long-Term Management of Seizures after Surgical Treatment of Supratentorial Cavernous Malformations: A Retrospective Single Centre Study. J. Korean Neurosurg. Soc. 2022, 65, 415–421. [Google Scholar] [CrossRef]
- Kraemer, D.L.; Awad, I.A. Vascular Malformations and Epilepsy: Clinical Considerations and Basic Mechanisms. Epilepsia 1994, 35, S30–S43. [Google Scholar] [CrossRef]
- Englot, D.J.; Chang, E.F. Rates and Predictors of Seizure Freedom in Resective Epilepsy Surgery: An Update. Neurosurg. Rev. 2014, 37, 389–404; discussion 404–405. [Google Scholar] [CrossRef]
- Shang-Guan, H.-C.; Wu, Z.-Y.; Yao, P.-S.; Chen, G.-R.; Zheng, S.-F.; Kang, D.-Z. Is Extended Lesionectomy Needed for Patients with Cerebral Cavernous Malformations Presenting with Epilepsy? A Meta-Analysis. World Neurosurg. 2018, 120, e984–e990. [Google Scholar] [CrossRef]
- Baumann, C.R.; Schuknecht, B.; Lo Russo, G.; Cossu, M.; Citterio, A.; Andermann, F.; Siegel, A.M. Seizure Outcome after Resection of Cavernous Malformations Is Better When Surrounding Hemosiderin-Stained Brain Also Is Removed. Epilepsia 2006, 47, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Tao, Z.; You, C.; Li, Q.; Liu, Y. Extended Resection of Hemosiderin Fringe Is Better for Seizure Outcome: A Study in Patients with Cavernous Malformation Associated with Refractory Epilepsy. Neurol. India 2013, 61, 288–292. [Google Scholar] [CrossRef] [PubMed]
- von der Brelie, C.; Malter, M.P.; Niehusmann, P.; Elger, C.E.; von Lehe, M.; Schramm, J. Surgical Management and Long-Term Seizure Outcome after Epilepsy Surgery for Different Types of Epilepsy Associated with Cerebral Cavernous Malformations. Epilepsia 2013, 54, 1699–1706. [Google Scholar] [CrossRef] [PubMed]
- Zevgaridis, D.; van Velthoven, V.; Ebeling, U.; Reulen, H.J. Seizure Control Following Surgery in Supratentorial Cavernous Malformations: A Retrospective Study in 77 Patients. Acta Neurochir. 1996, 138, 672–677. [Google Scholar] [CrossRef]
- Cappabianca, P.; Alfieri, A.; Maiuri, F.; Mariniello, G.; Cirillo, S.; de Divitiis, E. Supratentorial Cavernous Malformations and Epilepsy: Seizure Outcome after Lesionectomy on a Series of 35 Patients. Clin. Neurol. Neurosurg. 1997, 99, 179–183. [Google Scholar] [CrossRef]
- Yeon, J.Y.; Kim, J.-S.; Choi, S.J.; Seo, D.-W.; Hong, S.B.; Hong, S.-C. Supratentorial Cavernous Angiomas Presenting with Seizures: Surgical Outcomes in 60 Consecutive Patients. Seizure 2009, 18, 14–20. [Google Scholar] [CrossRef]
- Huang, C.; Chen, M.-W.; Si, Y.; Li, J.-M.; Zhou, D. Factors Associated with Epileptic Seizure of Cavernous Malformations in the Central Nervous System in West China. Pak. J. Med. Sci. 2013, 29, 1116–1121. [Google Scholar] [CrossRef]
- Kwon, C.-S.; Sheth, S.A.; Walcott, B.P.; Neal, J.; Eskandar, E.N.; Ogilvy, C.S. Long-Term Seizure Outcomes Following Resection of Supratentorial Cavernous Malformations. Clin. Neurol. Neurosurg. 2013, 115, 2377–2381. [Google Scholar] [CrossRef]
- Hammen, T.; Romstöck, J.; Dörfler, A.; Kerling, F.; Buchfelder, M.; Stefan, H. Prediction of Postoperative Outcome with Special Respect to Removal of Hemosiderin Fringe: A Study in Patients with Cavernous Haemangiomas Associated with Symptomatic Epilepsy. Seizure 2007, 16, 248–253. [Google Scholar] [CrossRef]
- Jin, Y.; Zhao, C.; Zhang, S.; Zhang, X.; Qiu, Y.; Jiang, J. Seizure Outcome after Surgical Resection of Supratentorial Cavernous Malformations plus Hemosiderin Rim in Patients with Short Duration of Epilepsy. Clin. Neurol. Neurosurg. 2014, 119, 59–63. [Google Scholar] [CrossRef]
- Englot, D.J.; Han, S.J.; Lawton, M.T.; Chang, E.F. Predictors of Seizure Freedom in the Surgical Treatment of Supratentorial Cavernous Malformations: Clinical Article. J. Neurosurg. 2011, 115, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- Dammann, P.; Schaller, C.; Sure, U. Should We Resect Peri-Lesional Hemosiderin Deposits When Performing Lesionectomy in Patients with Cavernoma-Related Epilepsy (CRE)? Neurosurg. Rev. 2017, 40, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Van Gompel, J.J.; Rubio, J.; Cascino, G.D.; Worrell, G.A.; Meyer, F.B. Electrocorticography-Guided Resection of Temporal Cavernoma: Is Electrocorticography Warranted and Does It Alter the Surgical Approach?: Clinical Article. J. Neurosurg. 2009, 110, 1179–1185. [Google Scholar] [CrossRef]
- Régis, J.; Bartolomei, F.; Kida, Y.; Kobayashi, T.; Vladyka, V.; Liscàk, R.; Forster, D.; Kemeny, A.; Schröttner, O.; Pendl, G. Radiosurgery for Epilepsy Associated with Cavernous Malformation: Retrospective Study in 49 Patients. Neurosurgery 2000, 47, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Yamada, S.; Nakase, H.; Nakagawa, I.; Nishimura, F.; Motoyama, Y.; Park, Y.-S. Cavernous Malformations in Pregnancy. Neurol. Med. Chir. 2013, 53, 555–560. [Google Scholar] [CrossRef]
- Aiba, T.; Tanaka, R.; Koike, T.; Kameyama, S.; Takeda, N.; Komata, T. Natural History of Intracranial Cavernous Malformations. J. Neurosurg. 1995, 83, 56–59. [Google Scholar] [CrossRef]
- Kaya, A.H.; Ulus, A.; Bayri, Y.; Topal, A.; Gun, S.; Kandemir, B.; Dagcinar, A.; Senel, A.; Iyigun, O. There Are No Estrogen and Progesterone Receptors in Cerebral Cavernomas. Surg. Neurol. 2009, 72, 263–265. [Google Scholar] [CrossRef]
- Kalani, M.Y.S.; Zabramski, J.M. Risk for Symptomatic Hemorrhage of Cerebral Cavernous Malformations during Pregnancy: Clinical Article. J. Neurosurg. 2013, 118, 50–55. [Google Scholar] [CrossRef]
- Witiw, C.D.; Abou-Hamden, A.; Kulkarni, A.V.; Silvaggio, J.A.; Schneider, C.; Wallace, M.C. Cerebral Cavernous Malformations and Pregnancy: Hemorrhage Risk and Influence on Obstetrical Management. Neurosurgery 2012, 71, 626–631. [Google Scholar] [CrossRef]
- Joseph, N.K.; Kumar, S.; Brown, R.D.; Lanzino, G.; Flemming, K.D. Influence of Pregnancy on Hemorrhage Risk in Women With Cerebral and Spinal Cavernous Malformations. Stroke 2021, 52, 434–441. [Google Scholar] [CrossRef]
- Bektas, D.; Lanzino, G.; Smith, K.M.; Flemming, K.D. Tailored management of cavernous malformations in women: Considerations and strategies-a review. Front. Neurol. 2024, 15, 1487808. [Google Scholar] [CrossRef]
- Simonazzi, G.; Curti, A.; Rapacchia, G.; Gabrielli, S.; Pilu, G.; Rizzo, N.; Pozzati, E. Symptomatic Cerebral Cavernomas in Pregnancy: A Series of 6 Cases and Review of the Literature. J. Matern.-Fetal Neonatal Med. 2014, 27, 261–264. [Google Scholar] [CrossRef]
- Maor, G.S.; Faden, M.S.; Brown, R. Prevalence, Risk Factors and Pregnancy Outcomes of Women with Vascular Brain Lesions in Pregnancy. Arch. Gynecol. Obstet. 2020, 301, 665–670. [Google Scholar] [CrossRef]
- Merlino, L.; Del Prete, F.; Titi, L.; Piccioni, M.G. Cerebral Cavernous Malformation: Management and Outcome during Pregnancy and Puerperium. A Systematic Review of Literature. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 101927. [Google Scholar] [CrossRef]
- Zuurbier, S.M.; Santos, A.N.; Flemming, K.D.; Schmidt, B.; Jabbarli, R.; Lanzino, G.; Sure, U.; Dammann, P. Female Hormone Therapy and Risk of Intracranial Hemorrhage from Cerebral Cavernous Malformations: A Multicenter Observational Cohort Study. Neurology 2023, 100, e1673–e1679. [Google Scholar] [CrossRef]
- Abe, M.; Fukudome, K.; Sugita, Y.; Oishi, T.; Tabuchi, K.; Kawano, T. Thrombus and encapsulated hematoma in cerebral cavernous malformations. Acta Neuropathol. 2005, 109, 503–509. [Google Scholar] [CrossRef]



| Lesion Type | MRI Signal | Pathologic Features | Images |
|---|---|---|---|
| Type I | T1: hyperintense core T2: hyper- or hypointense core with surrounding hypointense rim | Subacute hemorrhage surrounded by a rim of hemosiderin-stained macrophages and gliotic brain | 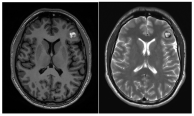 |
| Type II | T1: reticulated mixed signal core T2: reticulated mixed signal core with surrounding hypointense rim resulting in the “popcorn” appearance GE: low signal rim with blooming | Loculated area of hemorrhage and thrombosis of varying age, surrounded by gliotic, hemosiderin-stained brain; in large lesions, areas of calcification may be seen |  |
| Type III | T1: iso- or hypointense T2: hypointense with a hypointense rim that magnifies the size of the lesion GE: hypointense with greater magnification than T2 | Chronic resolved hemorrhage, with hemosiderin staining within and around the lesion |  |
| Type IV | T1: poorly seen or not visualized at all T2: poorly seen or not visualized at all GE: punctate hypointense lesions | Thought to be capillary telangiectasias | 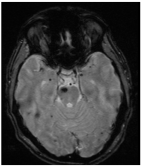 |
| Authors | N° of Studies/Time Limit | Type of Studies | N° of Patients | Mean Age Years | Anatomic Location | Presenting Symptoms | Follow-Up | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| Gao, 2021 [78] | Systematic Review and Meta-Analysis (1990–2019) Microsurgery vs. SRS | 42 retrospective studies | 2492 patients: 2122 microsurgery vs. 370 SRS | Microsurgery 37.2 (12–43) SRS 41.6 (37–44) | Brainstem (100%) | Cranial nerve dysfunction, Sensory disturbances, Motor palsy, hemiparesis, and headache | 36 months (8–110) | Surgery was more commonly performed in symptomatic larger lesions located in the midbrain and pons, while SRS was preferentially selected in medulla CMs and in older patients. Mortality attributed to treatments, symptomatic ICH, and persistent disability did not differ between the microsurgery and SRS. PND was significantly higher in the surgical group than in the SRS group. On the contrary, the number of patients with symptomatic ICH was significantly higher in the SRS group than in the surgical group | Both microsurgery and SRS demonstrated great efficacy in reducing the rebleeding rate after treatment for brainstem CMs. Surgical removal of the symptomatic brain is generally favored. However, in specific cases, SRS is a valid alternative. Randomized trials are needed |
| Fotakopoulos, 2021 [86] | Systematic Review and Meta-Analysis (last search 2020) comparing Microsurgery vs. SRS | 6 retrospective studies | 396 patients: 168 microsurgery vs. 228 SRS | range 33.3–43.7 | Brainstem (100%) | - | - | No statistically significant difference or superiority between microsurgery and SRS of symptomatic brainstem CMs regarding PND after treatment, mortality rates, and reintervention | SRS for brainstem CMs seems to result in a marked reduction in the risk of rebleeding 2 years after treatment, but when compared with microsurgery, there was no remarkable difference. Microsurgery should be considered as the first-line management, particularly for lesions with progressive neurologic deficits, hemorrhage with mass effect, and small lesions. However, conservative management or SRS strategy may be considered for asymptomatic deep CMs and patients with severe comorbidities |
| Al-Schalchy, 2025 [87] | Systematic Review and Meta-Analysis (2001–2024) comparing Microsurgery vs. SRS vs. Conservative management | 45 studies (44 retrospective cohort; 1 RCT) | 3015 adult and pediatric patients: 83.9% microsurgery 10.7% RT or SRS 5.1% conservative management | 10–58 | Brainstem (100%) pons 62.4% midbrain 21% medulla oblongata 16.6% | Previous hemorrhage 82% Cranial nerve deficits 58.9% Hemiparesis 31.7% Ataxia 27.1% Incidental finding 0.7% | 3–97 months (range) | No statistically significant reduction in rebleeding rate and mortality between conservative management and SRS. Significant reduction in rebleeding risk and mortality between microsurgery and conservative management Microsurgery was significantly associated with lower recurrence and mortality compared to SRS. Patients managed conservatively had the highest rebleeding rate and the lowest functional outcome rate | In patients with hemorrhagic or symptomatic brainstem CMs, microsurgical resection resulted in lower recurrence, rebleeding, retreatment, and mortality compared to SRS and conservative management. Radiosurgery may be suitable for selected patients with inaccessible or high-risk lesions. Randomized trials are needed |
| Authors | N° of Studies/ Time Limit | N° of Patients | Mean Age | Mean Size of CMs | Anatomic Location | Mean Marginal Dose | AHR Pre-SRS | AHR Post-SRS | Mean FU | Adverse Effect | Associated Factor to ARE | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wen, 2019 [38] | Meta-analysis 9 cohort studies (1 case–control) (2007–2017) | 747 | 40 yrs | 0.3–14.8 cm3 | brainstem/basal ganglia/thalamus (81%) | 11–15.8 Gy (range among studies) | 7.2–39.5% (not including the first bleeding) | 1.22–12.3% (first 2 yrs post-SRS) 1–3.6% (>2 yrs post-SRS) significant reduction | 48 months (36–68) | 7.1% (headache, FND, edema) | Patients with cerebral CMs, especially if deep-seated and surgically inaccessible, seem to benefit from SRS owing to a significant reduction in annual hemorrhage without differences between the first 2 years and 2 years after | |
| Poorthuis, 2019 [89] | Meta-analysis 30 cohort studies (3 studies compared SRS vs. surgery; 1 study compared SRS vs. surgery vs. observation) (–2018) | 1576 | 40 yrs | 1.37 cm3 (0.6–1.86) | lobar (18%) basal ganglia and thalamus (13%) brainstem (61%) | 15 Gy (13–16) (range among studies) | 2.40% (symptomatic) | 48 months (35–62) | 0.71% (FND) 0.18% (mortality) | After SRS, the annual incidences of death, ICH, and FND are <5% and seem comparable to outcomes without SRS. A randomized trial of SRS for CMs is needed. | ||
| Kim, 2019 [90] | Meta-analysis 14 retrospective studies (2000–2018) | 576 | 40 yrs | 0.014–14.6 cm3 | brainstem (100%) | 11–15.8 Gy (range among studies) | 23.4% | 3.2% | 6–228 months (range) | 7.3% (2.2% permanent) | Marginal dose > 13 Gy | SRS using a relatively low marginal dose is a safe and effective treatment for brainstem CMs. Hemorrhage rate 2 years after SRS was significantly lower than that within 2 years after SRS. |
| Bubenikova, 2022 [30] | Meta-analysis 98 studies (1 single randomized study) (1990–2020) | 8994 | 34.8 yrs | 1.4 cm | lobar (23%) deep-seated (12%) brainstem (50%) cerellum (5%) | 13.8% (symptomatic and asymptomatic) | 50 months (23.6–112) | 9% (long-term FND) 0.6% (mortality) | Deep-seated CMs Initial ICH | The efficacy of preventing hemorrhage was 97% in surgical, 86% in SRS, and 77% in conservative treatment. The lowest mortality (1%) was observed after SRS, and the highest persistent morbidity (22%) was observed in the conservatively treated group. SRS is a method of choice predominantly in poorly accessible CMs or those with a less aggressive nature. | ||
| Shanker, 2022 [69] | Meta-analysis 25 studies (1995–2021) | 1758 | 24.9% | 6.7% (first 2 yrs post SRS) 3.4% (>2 yrs post SRS) significant reduction | 27–111.7 months (range) | 12% (4% permanent) | SRS is effective and associated with a statistically significant eightfold reduction in rebleeding risk, particularly in the first 2 years following treatment. | |||||
| Tos, 2024 [25] | Meta-analysis 32 studies (30 retrospective; 1 case–control; 1 prospective) (1998–2023) | 2672 | 35–44 yrs | 0.28–3.1 cm3 | brainstem (36.9) lobar (30.6%) basal ganglia and thalamus (19.7%) cerebellum (5.1%) | 11.6–25 Gy | Overall risk of AHR decreased by 5.9-fold (3.5-fold in the first 2 years post-SRS; 9.1-fold > 2 years post-SRS) | 22–111 months (range) | 8% (2% permanent) (6% if treated with < 13 Gy 9% if treated with > 13 Gy) | Marginal dose > 13 Gy | SRS is an effective intervention for CMs, significantly reducing hemorrhage rates and improving seizure outcome without differences based on marginal doses. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrassi, E.; Mazzucchi, E.; Raus, L.; Lecce, M.; Marucci, L.; Farneti, A.; Telera, S. Controversies in Cavernous Malformation Management: A Comprehensive Review of Current Literature. J. Clin. Med. 2025, 14, 8614. https://doi.org/10.3390/jcm14238614
Carrassi E, Mazzucchi E, Raus L, Lecce M, Marucci L, Farneti A, Telera S. Controversies in Cavernous Malformation Management: A Comprehensive Review of Current Literature. Journal of Clinical Medicine. 2025; 14(23):8614. https://doi.org/10.3390/jcm14238614
Chicago/Turabian StyleCarrassi, Erika, Edoardo Mazzucchi, Laura Raus, Mario Lecce, Laura Marucci, Alessia Farneti, and Stefano Telera. 2025. "Controversies in Cavernous Malformation Management: A Comprehensive Review of Current Literature" Journal of Clinical Medicine 14, no. 23: 8614. https://doi.org/10.3390/jcm14238614
APA StyleCarrassi, E., Mazzucchi, E., Raus, L., Lecce, M., Marucci, L., Farneti, A., & Telera, S. (2025). Controversies in Cavernous Malformation Management: A Comprehensive Review of Current Literature. Journal of Clinical Medicine, 14(23), 8614. https://doi.org/10.3390/jcm14238614






