Variations in Root and Canal Morphology of Mandibular First Molars: A Retrospective Cone-Beam Computed Tomography Study in a Saudi Subpopulation
Abstract
1. Introduction
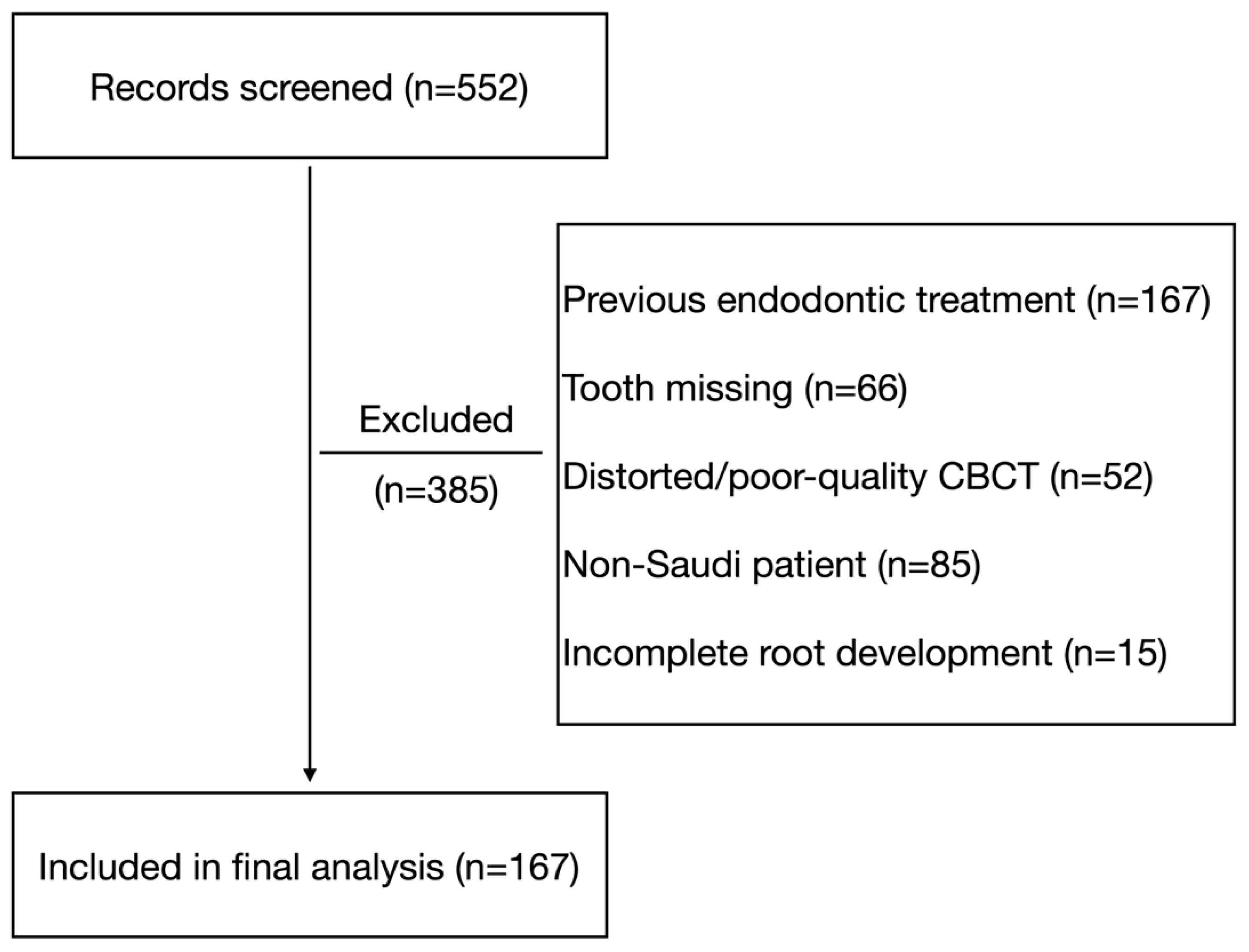
2. Materials and Methods
Study Design and Ethical Approval
3. Eligibility Criteria
- Inclusion criteria
- Saudi patients aged ≥ 10 years.
- Fully erupted mandibular first molars.
- Completely formed root apices.
- CBCT scans with diagnostic image quality.
- Exclusion criteria
- Previous root canal treatment.
- Large metallic restorations or crowns causing scatter.
- Calcified canals or internal/external resorption.
- Incomplete root formation.
- Motion artifacts or distorted CBCT images.
3.1. CBCT Acquisition Parameters
3.2. CBCT Image Processing and Root Alignment Protocol
3.3. Definitions and Criteria
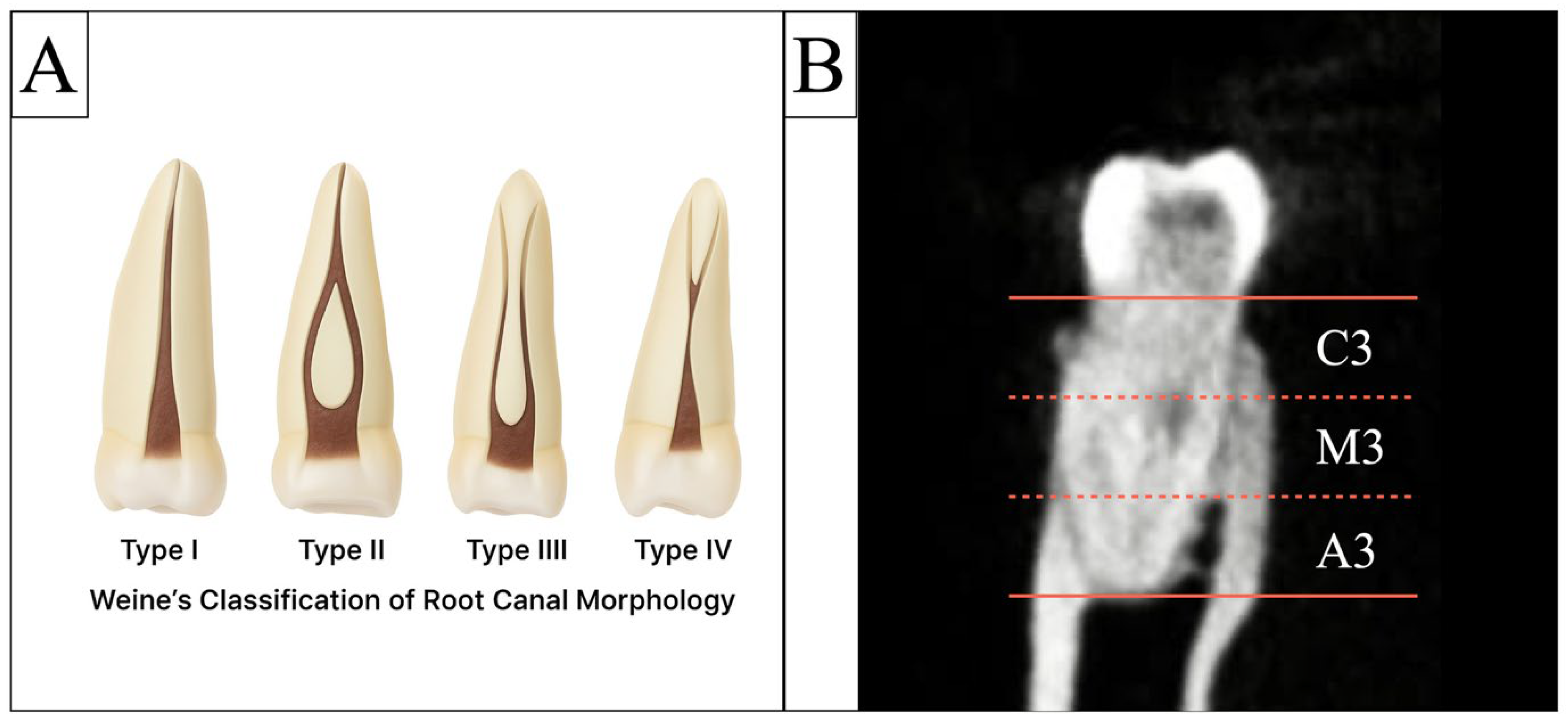
3.3.1. Canal Configuration
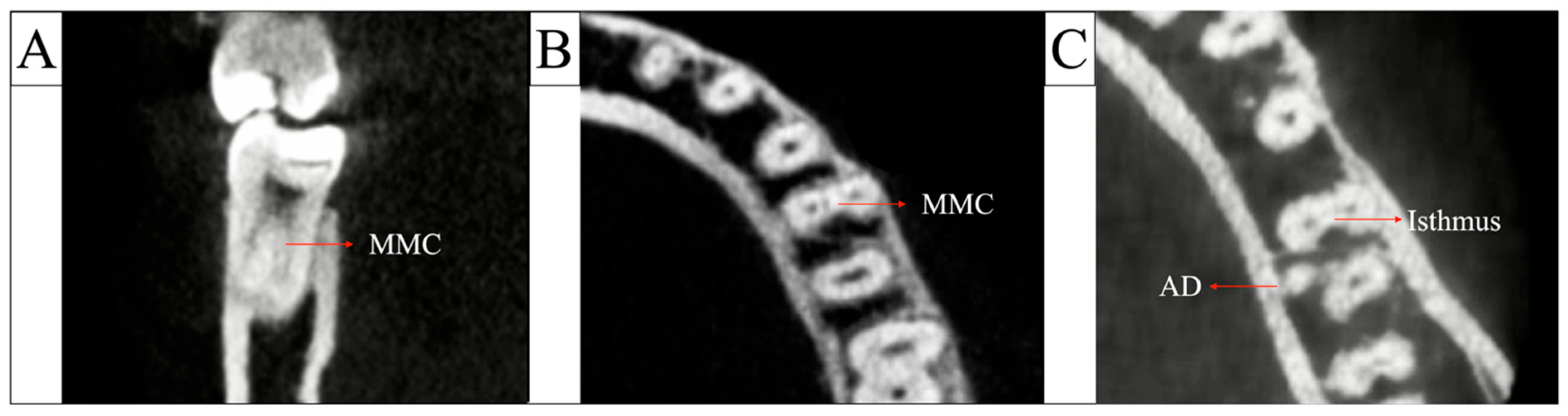
3.3.2. Middle Mesial Canal (MMC)
3.3.3. Isthmus Classification
- C3: coronal third;
- M3: middle third;
- A3: apical third.
3.3.4. Intercanal Distance
3.4. Examiner Calibration and Reliability Analysis
3.5. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Clinical Significance
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Society of Endodontology. Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology. Int. Endod. J. 2006, 39, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.N. Apical periodontitis: A dynamic encounter between root canal infection and host response. Periodontol. 2000 1997, 13, 121–148. [Google Scholar] [CrossRef] [PubMed]
- Berkovitz, B.K.; Holland, G.; Muxham, B.J. Tooth morphology. In Oral Anatomy Histology and Embryology, 1st ed.; Wolf: London, UK, 1992; pp. 24–43. [Google Scholar]
- Azim, A.A.; Griggs, J.A.; Huang, G.T. The Tennessee study: Factors affecting treatment outcome and healing time following nonsurgical root canal treatment. Int. Endod. J. 2016, 49, 6–16. [Google Scholar] [CrossRef]
- Smith, C.S.; Setchell, D.J.; Harty, F.J. Factors influencing the success of conventional root canal therapy--a five-year retrospective study. Int. Endod. J. 1993, 26, 321–333. [Google Scholar] [CrossRef]
- Swartz, D.B.; Skidmore, A.E.; Griffin, J.A., Jr. Twenty years of endodontic success and failure. J. Endod. 1983, 9, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Gu, L.; Wei, X.; Ling, J.; Huang, X. A microcomputed tomographic study of canal isthmuses in the mesial root of mandibular first molars in a Chinese population. J. Endod. 2009, 35, 353–356. [Google Scholar] [CrossRef]
- Weine, F.S.; Hayami, S.; Hata, G.; Toda, T. Canal configuration of the mesiobuccal root of the maxillary first molar of a Japanese sub-population. Int. Endod. J. 1999, 32, 79–87. [Google Scholar] [CrossRef]
- Pattanshetti, N.; Gaidhane, M.; Al Kandari, A.M. Root and canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait population—A clinical study. Int. Endod. J. 2008, 41, 755–762. [Google Scholar] [CrossRef]
- Kim, S.Y.; Yang, S.E. Cone-beam computed tomography study of incidence of distolingual root and distance from distolingual canal to buccal cortical bone of mandibular first molars in a Korean population. J. Endod. 2012, 38, 301–304. [Google Scholar] [CrossRef]
- Chandra, S.S.; Chandra, S.; Shankar, P.; Indira, R. Prevalence of radix entomolaris in mandibular permanent first molars: A study in a South Indian population. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, e77–e82. [Google Scholar] [CrossRef]
- Alavi, A.M.; Opasanon, A.; Ng, Y.L.; Gulabivala, K. Root and canal morphology of Thai maxillary molars. Int. Endod. J. 2002, 35, 478–485. [Google Scholar] [CrossRef]
- Awawdeh, L.; Abdullah, H.; Al-Qudah, A. Root form and canal morphology of Jordanian maxillary first premolars. J. Endod. 2008, 34, 956–961. [Google Scholar] [CrossRef]
- Silva, E.J.N.L.; Nejaim, Y.; Silva, A.V.; Haiter-Neto, F.; Cohenca, N. Evaluation of root canal configuration of mandibular molars in a Brazilian population by using cone-beam computed tomography: An in vivo study. J. Endod. 2013, 39, 849–852. [Google Scholar] [CrossRef]
- Valencia de Pablo, Ó.; Estevez, R.; Peix, M.; Heilborn, C.; Cohenca, N. Root anatomy and canal configuration of the permanent mandibular first molar: A systematic review. J. Endod. 2010, 36, 1919–1931. [Google Scholar] [CrossRef]
- Naoum, H.; Love, R.; Chandler, N.; Herbison, P. Effect of X-ray beam angulation and intraradicular contrast medium on radiographic interpretation of lower first molar root canal anatomy. Int. Endod. J. 2003, 36, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Cotton, T.P.; Geisler, T.M.; Holden, D.T.; Schwartz, S.A.; Schindler, W.G. Endodontic applications of cone-beam volumetric tomography. J. Endod. 2007, 33, 1121–1132. [Google Scholar] [CrossRef]
- Bansal, R.; Hegde, S.; Astekar, M. Morphology and prevalence of middle canals in the mandibular molars: A systematic review. J. Oral Maxillofac. Pathol. 2018, 22, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Azim, A.A.; Deutsch, A.S.; Solomon, C.S. Prevalence of middle mesial canals in mandibular molars after guided troughing under high magnification: An in vivo investigation. J. Endod. 2015, 41, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, R.; Xu, H.; Zhang, Q.; Guo, Y. Prevalence and morphology of middle mesial canals in mandibular first molars and their relationship with anatomical aspects of the mesial root: A CBCT analysis. BMC Oral Health 2025, 25, 147. [Google Scholar] [CrossRef]
- Al Shehadat, S.; Waheb, S.; Al Bayatti, S.W.; Kheder, W.; Khalaf, K.; Murray, C.A. Cone beam computed tomography analysis of root and root canal morphology of first permanent lower molars in a Middle East subpopulation. J. Int. Soc. Prev. Community Dent. 2019, 9, 458. [Google Scholar] [CrossRef]
- Qiao, X.; Zhu, H.; Yan, Y.; Li, J.; Ren, J.; Gao, Y.; Zou, L. Prevalence of middle mesial canal and radix entomolaris of mandibular first permanent molars in a western Chinese population: An in vivo cone-beam computed tomographic study. BMC Oral Health 2020, 20, 224. [Google Scholar] [CrossRef]
- Aldosimani, M.A.; Althumairy, R.I.; Alzahrani, A.; Aljarbou, F.A.; Alkatheeri, M.S.; AlGhizzi, M.A.; Abughosh, T.K. The mid-mesial canal prevalence in mandibular molars of a Saudi population: A cone-beam computed tomography study. Saudi Dent. J. 2021, 33, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Mashyakhy, M.; AlTuwaijri, N.; Alessa, R.; Alazzam, N.; Alotaibi, B.; Almutairi, R.; Alroomy, R.; Thota, G.; Melha, A.A.; Alkahtany, M.F.; et al. Anatomical Evaluation of Root and Root Canal Morphology of Permanent Mandibular Dentition among the Saudi Arabian Population: A Systematic Review. BioMed Res. Int. 2022, 2022, 2400314. [Google Scholar] [CrossRef]
- Srivastava, S.; Alrogaibah, N.A.; Aljarbou, G. Cone-beam computed tomographic analysis of middle mesial canals and isthmus in mesial roots of mandibular first molars-prevalence and related factors. J. Conserv. Dent. Endod. 2018, 21, 526–530. [Google Scholar] [CrossRef]
- Weine, F.S.; Healey, H.J.; Gerstein, H.; Evanson, L. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surg. Oral Med. Oral Pathol. 1969, 28, 419–425. [Google Scholar] [CrossRef]
- Vertucci, F.J. Root canal anatomy of the human permanent teeth. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 589–599. [Google Scholar] [CrossRef]
- Chen, G.; Yao, H.; Tong, C. Investigation of the root canal configuration of mandibular first molars in a Taiwan Chinese population. Int. Endod. J. 2009, 42, 1044–1049. [Google Scholar] [CrossRef] [PubMed]
- Madfa, A.A.; Alshammari, A.F.; Almagadawyi, E.; Al-Haddad, A.; Aledaili, E.A. Prevalence of radix entomolaris and distolingual canals and their association with the incidence of middle mesial canals in mandibular first molars of a Saudi subpopulation. Sci. Rep. 2025, 15, 37384. [Google Scholar] [CrossRef] [PubMed]
- Şendişçi Gök, R.; Tercanlı, H.; Ekinci, A. Evaluation of root and canal morphology of mandibular molar teeth by cone beam computed tomography: Cross-sectional study. BMC Oral Health 2025, 25, 798. [Google Scholar] [CrossRef]
- Bhatti, U.A.; Muhammad, M.; Javed, M.Q.; Sajid, M. Frequency of middle mesial canal in mandibular first molars and its association with various anatomic variables. Aust. Endod. J. 2022, 48, 494–500. [Google Scholar] [CrossRef]
- Huang, C.-C.; Chang, Y.-C.; Chuang, M.-C.; Lai, T.-M.; Lai, J.-Y.; Lee, B.-S.; Lin, C.-P. Evaluation of root and canal systems of mandibular first molars in Taiwanese individuals using cone-beam computed tomography. J. Formos. Med. Assoc. 2010, 109, 303–308. [Google Scholar] [CrossRef]
- Vertucci, F.; Williams, R. Root canal anatomy of the mandibular first molar. J. N. J. Dent. Assoc. 1974, 45, 27. [Google Scholar]
- Al-Habib, M.A.; Almarzouki, S.; Alsulaiman, M.; Alsofi, L. Comprehensive Analysis of Mandibular First Molar Root and Canal Morphology in Saudi Patients Using Cone Beam Computed Tomography (CBCT). Med. Sci. Monit. 2024, 30, e945364. [Google Scholar] [CrossRef]
- Kim, Y.; Perinpanayagam, H.; Lee, J.K.; Yoo, Y.J.; Oh, S.; Gu, Y.; Lee, S.P.; Chang, S.W.; Lee, W.; Baek, S.H.; et al. Comparison of mandibular first molar mesial root canal morphology using micro-computed tomography and clearing technique. Acta Odontol. Scand. 2015, 73, 427–432. [Google Scholar] [CrossRef]
- Mannocci, F.; Peru, M.; Sherriff, M.; Cook, R.; Pitt Ford, T.R. The isthmuses of the mesial root of mandibular molars: A micro-computed tomographic study. Int. Endod. J. 2005, 38, 558–563. [Google Scholar] [CrossRef]
- Fan, B.; Pan, Y.; Gao, Y.; Fang, F.; Wu, Q.; Gutmann, J.L. Three-dimensional morphologic analysis of isthmuses in the mesial roots of mandibular molars. J. Endod. 2010, 36, 1866–1869. [Google Scholar] [CrossRef]
- Keles, A.; Keskin, C. Deviations of mesial root canals of mandibular first molar teeth at the apical third: A micro–computed tomographic study. J. Endod. 2018, 44, 1030–1032. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, F.B.; Sano, C.L.; Gomes, B.P.F.A.; Zaia, A.A.; Ferraz, C.C.R.; Souza-Filho, F.J. A preliminary in vitro study of the incidence and position of the root canal isthmus in maxillary and mandibular first molars. Int. Endod. J. 2003, 36, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Dao, J.; Liu, Z.; Zhang, Z.; Lu, Y.; Zeng, X. Cone-beam computed tomography investigation of middle mesial canals and isthmuses in mandibular first molars in a Chinese population. BMC Oral Health 2020, 20, 135. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.N.; Henry, S.; Cano, V.; Vera, J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg. Oral Med. Oral Pathol. 2005, 99, 231–252. [Google Scholar] [CrossRef]
- Siqueira, J.F.; Rôças, I.N.; Ricucci, D. Biofilms in endodontic infection. Endod. Top. 2010, 22, 33–49. [Google Scholar] [CrossRef]
- Gutarts, R.; Nusstein, J.; Reader, A.; Beck, M. In vivo debridement efficacy of ultrasonic irrigation following hand-rotary instrumentation in human mandibular molars. J. Endod. 2005, 31, 166–170. [Google Scholar] [CrossRef]
- Plotino, G.; Özyürek, T.; Gündoğar, M.; Uslu, G.; Pedullà, E.; Careddu, R.; Franco, V. Efficacy of different irrigant activation devices in removing dentin debris from an artificial isthmus connecting curved canals. Aust. Endod. J. 2023, 49, 353–358. [Google Scholar] [CrossRef]
- Rödig, T.; Koberg, C.; Baxter, S.; Konietschke, F.; Wiegand, A.; Rizk, M. Micro-CT evaluation of sonically and ultrasonically activated irrigation on the removal of hard-tissue debris from isthmus-containing mesial root canal systems of mandibular molars. Int. Endod. J. 2019, 52, 1173–1181. [Google Scholar] [CrossRef]
- Malentacca, A.; Uccioli, U.; Mannocci, F.; Bhuva, B.; Zangari, D.; Pulella, C.; Lajolo, C. The comparative effectiveness and safety of three activated irrigation techniques in the isthmus area using a transparent tooth model. Int. Endod. J. 2018, 51, e35–e41. [Google Scholar] [CrossRef] [PubMed]
- Song, J.S.; Choi, H.J.; Jung, I.Y.; Jung, H.S.; Kim, S.O. The prevalence and morphologic classification of distolingual roots in the mandibular molars in a Korean population. J. Endod. 2010, 36, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Pineda, F.; Kuttler, Y. Mesiodistal and buccolingual roentgenographic investigation of 7275 root canals. Oral Surg. Oral Med. Oral Pathol. 1972, 33, 101–110. [Google Scholar] [CrossRef] [PubMed]
| Root Type | Weine’s Canal Configurations | ||||
|---|---|---|---|---|---|
| I | II | III | IV | p-Value * | |
| Mesial Root | 3 | 164 | 155 | 0 | <0.001 |
| n = 322 | (0.9%) | (50.9%) | (48.1%) | (0.0%) | |
| Distal (Main) Root | 223 | 65 | 20 | 14 | |
| n = 322 | (69.3%) | (20.2%) | (6.2%) | (4.3%) | |
| Variable | Category | Mesial Root | Distal Main Root | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | p-Value * | I | II | III | IV | p-Value * | ||
| Gender | Male | 1 (0.7%) | 65 (45.8%) | 76 (53.5%) | 0 (0.0%) | 0.009 | 96 (67.6%) | 28 (19.7%) | 8 (5.6%) | 10 (7.0%) | 0.001 |
| Female | 2 (1.1%) | 99 (55.0%) | 79 (43.9%) | 0 (0.0%) | 127 (70.6%) | 37 (20.6%) | 12 (6.6%) | 4 (2.2%) | |||
| Age | ≤ 20 | 0 (0.0%) | 26 (51.0%) | 25 (49.0%) | 0 (0.0%) | <0.001 | 44 (86.3%) | 4 (7.8%) | 0 (0.0%) | 3 (5.9%) | <0.001 |
| 21–30 | 3 (2.5%) | 62 (51.2%) | 56 (46.3%) | 0 (0.0%) | 80 (66.1%) | 27 (22.3%) | 8 (6.6%) | 6 (5.0%) | |||
| 31–40 | 0 (0.0%) | 48 (50.0%) | 48 (50.0%) | 0 (0.0%) | 62 (64.6%) | 22 (22.9%) | 7 (7.3%) | 5 (5.2%) | |||
| 41–50 | 0 (0.0%) | 14 (43.8%) | 18 (56.3%) | 0 (0.0%) | 24 (75.0%) | 6 (18.8%) | 2 (6.2%) | 0 (0.0%) | |||
| 51–60 | 0 (0.0%) | 10 (71.4%) | 4 (28.6%) | 0 (0.0%) | 11 (78.6%) | 3 (21.4%) | 0 (0.0%) | 0 (0.0%) | |||
| ≥61 | 0 (0.0%) | 4 (50.0%) | 4 (50.0%) | 0 (0.0%) | 2 (25.0%) | 3 (37.5%) | 3 (37.5%) | 0 (0.0%) | |||
| Weine Type | n (Mesial Roots) | Intercanal Distance in mm (Mean ± SD) | Isthmus Present n (%) | Isthmus Level A3 n (%) | Isthmus Level M3 n (%) | Isthmus Level C3 n (%) |
|---|---|---|---|---|---|---|
| II | 164 | 1.97 ± 0.43 | 124 (75.6%) | 2 (1.2%) | 85 (51.8%) | 90 (54.9%) |
| III | 155 | 1.93 ± 0.51 | 137 (88.4%) | 112 (72.3%) | 90 (58.1%) | 85 (54.8%) |
| p-value | 0.435 * | 0.003 § | <0.001 § | 0.263 § | 0.994 § |
| Weine Type | All Distal Roots (n = 243) | Two-Distal-Root Molars (n = 79, Main Distal Root Only) | p-Value * |
|---|---|---|---|
| I | 220 (90.5%) | 3 (3.8%) | <0.001 |
| II | 16 (6.6%) | 49 (62.0%) | |
| III | 5 (2.1%) | 15 (19.0%) | |
| IV | 2 (0.8%) | 12 (15.2%) | |
| Total | 243 (100%) | 79 (100%) |
| Root Type | Paired (n) | Matching (n) | Agreement | Unweighted Cohen’s κ | p-Value |
|---|---|---|---|---|---|
| Mesial | 152 | 132 | 86.8% | 0.74 | <0.001 * |
| Distal | 155 | 137 | 88.4% | 0.76 | <0.001 § |
| Variable | Category | Total n | Symmetry Present n (%) | p-Value * |
|---|---|---|---|---|
| Overall | All | 155 | 118 (76.1%) | 0.852 |
| Gender | Female | 86 | 66 (76.7%) | |
| Male | 69 | 52 (75.4%) | ||
| Age group | ≤20 | 25 | 17 (68.0%) | 0.325 |
| 21–30 | 58 | 44 (75.9%) | ||
| 31–40 | 46 | 40 (87.0%) | ||
| 41–50 | 16 | 10 (62.5%) | ||
| 51–60 | 6 | 4 (66.7%) | ||
| ≥60 | 4 | 3 (75.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Austah, O.; Ali, W.; Althebaiti, A.; Albati, M.S.; Zahran, S.; Barayan, M.; Bokhary, A.; Alsofi, L. Variations in Root and Canal Morphology of Mandibular First Molars: A Retrospective Cone-Beam Computed Tomography Study in a Saudi Subpopulation. J. Clin. Med. 2025, 14, 8355. https://doi.org/10.3390/jcm14238355
Austah O, Ali W, Althebaiti A, Albati MS, Zahran S, Barayan M, Bokhary A, Alsofi L. Variations in Root and Canal Morphology of Mandibular First Molars: A Retrospective Cone-Beam Computed Tomography Study in a Saudi Subpopulation. Journal of Clinical Medicine. 2025; 14(23):8355. https://doi.org/10.3390/jcm14238355
Chicago/Turabian StyleAustah, Obadah, Waad Ali, Amani Althebaiti, Mohammed Saleh Albati, Shatha Zahran, Mohammed Barayan, Abdullah Bokhary, and Loai Alsofi. 2025. "Variations in Root and Canal Morphology of Mandibular First Molars: A Retrospective Cone-Beam Computed Tomography Study in a Saudi Subpopulation" Journal of Clinical Medicine 14, no. 23: 8355. https://doi.org/10.3390/jcm14238355
APA StyleAustah, O., Ali, W., Althebaiti, A., Albati, M. S., Zahran, S., Barayan, M., Bokhary, A., & Alsofi, L. (2025). Variations in Root and Canal Morphology of Mandibular First Molars: A Retrospective Cone-Beam Computed Tomography Study in a Saudi Subpopulation. Journal of Clinical Medicine, 14(23), 8355. https://doi.org/10.3390/jcm14238355





