The Impact of High-Intensity Interval Training on Cardiometabolic, Neurologic, Oncologic, and Pain-Related Outcomes: A Comprehensive Review of Systematic Reviews
Abstract
1. Introduction
2. Materials and Methods
2.1. Criteria for Inclusion
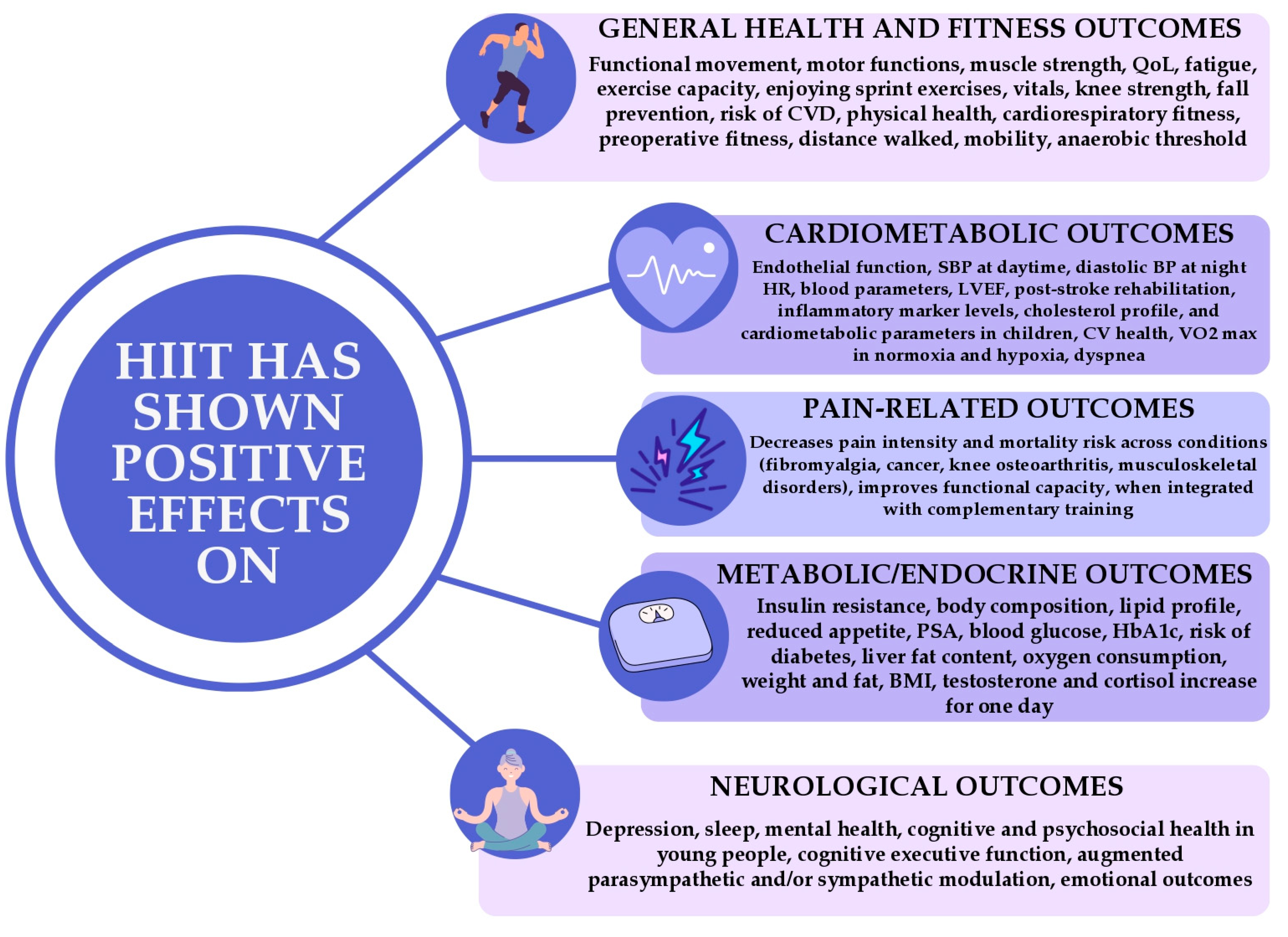
- Cardiometabolic outcomes;
- Neurological outcomes;
- Metabolic/endocrine outcomes;
- Oncologic outcomes;
- Pain-related outcomes.
2.2. Criteria for Exclusion
2.3. Search Strategy
2.4. Data Synthesis and Analysis
2.5. Methodological Quality Assessment
- High: 0–1 non-critical weakness;
- Moderate: more than one non-critical weakness;
- Low: 1 critical flaw (with/without other weaknesses);
- Critically low: more than 1 critical flaw (with/without other weaknesses).
3. Results
3.1. Included Studies
3.1.1. Patient Population and Objectives of the Meta-Analyses
3.1.2. Reported Diagnoses
3.2. Findings
3.2.1. HIIT Exercise-Induced Physiological Potential to Influence Metabolic Syndrome
3.2.2. Effects of HIIT on Blood Pressure and Vascular Function
3.2.3. HIIT in PCOS
3.2.4. HIIT for Cardiometabolic Correction in Children
3.2.5. HIIT After Myocardial Infarction
3.2.6. HIIT in HF
3.2.7. Neurological and Psychological Outcomes
3.2.8. HIIT in Persons with Spinal Cord Injury
3.2.9. Oncological Outcomes
3.2.10. The Impact of HIIT on Pain-Related Disorders
3.3. Quality Assessment Results
3.4. Consistency and Discrepancies and Reported Mechanisms
4. Discussion
4.1. Implications for Future Research
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HIIT | high-intensity interval training |
| VO2max | maximal oxygen uptake |
| HR | heart rate |
| BP | blood pressure |
| AE(s) | adverse event(s) |
| QoL | quality of life |
| CAD | coronary artery disease |
| HF | heart failure |
| MI | myocardial infarction |
| BMI | body mass index |
| HTN | hypertension |
| T2DM | type 2 diabetes mellitus |
| SBP | systolic blood pressure |
| DBP | diastolic blood pressure |
| BG | blood glucose |
| GLUT-4 | glucose transporter type 4 |
| WC | waist circumference |
| EPOC | excess post-exercise oxygen consumption |
| eNOS | endothelial nitric oxide synthase |
| NO | nitric oxide |
| ROS | reactive oxygen species |
| LVEF | left ventricular ejection fraction |
References
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010; Available online: www.who.int/publications-detail-redirect/9789241599979 (accessed on 10 March 2023).
- Batacan, R.B.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of High-Intensity Interval Training on Cardiometabolic Health: A Systematic Review and Meta-Analysis of Intervention Studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Kessler, H.S.; Sisson, S.B.; Short, K.R. The Potential for High-Intensity Interval Training to Reduce Cardiometabolic Disease Risk. Sports Med. 2012, 42, 489–509. [Google Scholar] [CrossRef]
- Hwang, C.-L.; Wu, Y.-T.; Chou, C.-H. Effect of Aerobic Interval Training on Exercise Capacity and Metabolic Risk Factors in People with Cardiometabolic Disorders: A Meta-Analysis. J. Cardiopulm. Rehabil. Prev. 2011, 31, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.S.; Wisløff, U.; Coombes, J.S. High-Intensity Interval Training in Patients with Lifestyle-Induced Cardiometabolic Disease: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2014, 48, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Sultana, R.N.; Sabag, A.; Keating, S.E.; Johnson, N.A. The Effect of Low-Volume High-Intensity Interval Training on Body Composition and Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 1687–1721. [Google Scholar] [CrossRef]
- Serrablo-Torrejon, I.; Lopez-Valenciano, A.; Ayuso, M.; Horton, E.; Mayo, X.; Medina-Gomez, G.; Liguori, G.; Jimenez, A. High Intensity Interval Training Exercise-Induced Physiological Changes and Their Potential Influence on Metabolic Syndrome Clinical Biomarkers: A Meta-Analysis. BMC Endocr. Disord. 2020, 20, 167. [Google Scholar] [CrossRef]
- Santos, I.K.D.; Nunes, F.A.S.D.S.; Queiros, V.S.; Cobucci, R.N.; Dantas, P.B.; Soares, G.M.; Cabral, B.G.d.A.T.; Maranhão, T.M.d.O.; Dantas, P.M.S. Effect of High-Intensity Interval Training on Metabolic Parameters in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2021, 16, e0245023. [Google Scholar] [CrossRef]
- Ramos, J.S.; Dalleck, L.C.; Tjonna, A.E.; Beetham, K.S.; Coombes, J.S. The Impact of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Vascular Function: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 679–692. [Google Scholar] [CrossRef]
- Solera-Martínez, M.; Herraiz-Adillo, Á.; Manzanares-Domínguez, I.; De La Cruz, L.L.; Martínez-Vizcaíno, V.; Pozuelo-Carrascosa, D.P. High-Intensity Interval Training and Cardiometabolic Risk Factors in Children: A Meta-Analysis. Pediatrics 2021, 148, e2021050810. [Google Scholar] [CrossRef]
- Qin, Y.; Kumar Bundhun, P.; Yuan, Z.-L.; Chen, M.-H. The Effect of High-Intensity Interval Training on Exercise Capacity in Post-Myocardial Infarction Patients: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2022, 29, 475–484. [Google Scholar] [CrossRef]
- Poon, E.T.-C.; Wongpipit, W.; Ho, R.S.-T.; Wong, S.H.-S. Interval Training versus Moderate-Intensity Continuous Training for Cardiorespiratory Fitness Improvements in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis. J. Sports Sci. 2021, 39, 1996–2005. [Google Scholar] [CrossRef] [PubMed]
- Rugbeer, N.; Constantinou, D.; Torres, G. Comparison of High-Intensity Training versus Moderate-Intensity Continuous Training on Cardiorespiratory Fitness and Body Fat Percentage in Persons with Overweight or Obesity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Phys. Act. Health 2021, 18, 610–623. [Google Scholar] [CrossRef]
- Araújo, B.T.S.; Leite, J.C.; Fuzari, H.K.B.; Pereira de Souza, R.J.; Remígio, M.I.; Dornelas de Andrade, A.; Lima Campos, S.; Cunha Brandão, D. Influence of High-Intensity Interval Training versus Continuous Training on Functional Capacity in Individuals with Heart Failure: A Systematic Review and Meta-Analysis. J. Cardiopulm. Rehabil. Prev. 2019, 39, 293–298. [Google Scholar] [CrossRef]
- García, I.B.; Arias, J.Á.R.; Campo, D.J.R.; González-Moro, I.M.; Poyatos, M.C. High-Intensity Interval Training Dosage for Heart Failure and Coronary Artery Disease Cardiac Rehabilitation. Syst. Rev. Meta Anal. Rev. Esp. Cardiol. 2019, 72, 233–243. [Google Scholar]
- Min, L.; Wang, D.; You, Y.; Fu, Y.; Ma, X. Effects of High-Intensity Interval Training on Sleep: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 10973. [Google Scholar] [CrossRef]
- Martland, R.; Korman, N.; Firth, J.; Vancampfort, D.; Thompson, T.; Stubbs, B. Can High-Intensity Interval Training Improve Mental Health Outcomes in the General Population and Those with Physical Illnesses? A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2022, 56, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Leahy, A.A.; Mavilidi, M.F.; Smith, J.J.; Hillman, C.H.; Eather, N.; Barker, D.; Lubans, D.R. Review of High-Intensity Interval Training for Cognitive and Mental Health in Youth. Med. Sci. Sports Exerc. 2020, 52, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Korman, N.; Armour, M.; Chapman, J.; Rosenbaum, S.; Kisely, S.; Suetani, S.; Firth, J.; Siskind, D. High Intensity Interval Training (HIIT) for People with Severe Mental Illness: A Systematic Review & Meta-Analysis of Intervention Studies—Considering Diverse Approaches for Mental and Physical Recovery. Psychiatry Res. 2020, 284, 112601. [Google Scholar]
- Alves, A.R.; Dias, R.; Neiva, H.P.; Marinho, D.A.; Marques, M.C.; Sousa, A.C.; Loureiro, V.; Loureiro, N. High-Intensity Interval Training Upon Cognitive and Psychological Outcomes in Youth: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 5344. [Google Scholar] [CrossRef]
- Peters, J.; Abou, L.; Rice, L.A.; Dandeneau, K.; Alluri, A.; Salvador, A.F.; Rice, I. The Effectiveness of Vigorous Training on Cardiorespiratory Fitness in Persons with Spinal Cord Injury: A Systematic Review and Meta-Analysis. Spinal Cord 2021, 59, 1035–1044. [Google Scholar] [CrossRef]
- Smyth, E.; O’Connor, L.; Mockler, D.; Reynolds, J.V.; Hussey, J.; Guinan, E. Preoperative High Intensity Interval Training for Oncological Resections: A Systematic Review and Meta-Analysis. Surg. Oncol. 2021, 38, 101620. [Google Scholar] [CrossRef]
- Mugele, H.; Freitag, N.; Wilhelmi, J.; Yang, Y.; Cheng, S.; Bloch, W.; Schumann, M. High-Intensity Interval Training in the Therapy and Aftercare of Cancer Patients: A Systematic Review with Meta-Analysis. J. Cancer Surviv. 2019, 13, 205–223. [Google Scholar] [CrossRef]
- Peng, Y.; Ou, Y.; Wang, K.; Wang, Z.; Zheng, X. The Effect of Low Volume High-Intensity Interval Training on Metabolic and Cardiorespiratory Outcomes in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2023, 13, 1098325. [Google Scholar] [CrossRef]
- Sabouri, M.; Amirshaghaghi, F.; Hesari, M.M. High-Intensity Interval Training Improves the Vascular Endothelial Function Comparing Moderate-Intensity Interval Training in Overweight or Obese Adults: A Meta-Analysis. Clin. Nutr. ESPEN 2023, 53, 100–106. [Google Scholar] [CrossRef]
- Stern, G.; Psycharakis, S.G.; Phillips, S.M. Effect of High-Intensity Interval Training on Functional Movement in Older Adults: A Systematic Review and Meta-Analysis. Sports Med. Open 2023, 9, 5. [Google Scholar] [CrossRef]
- Harpham, C.; Gunn, H.; Marsden, J.; Connolly, L. The Feasibility, Safety, Physiological and Clinical Effects of High-Intensity Interval Training for People with Parkinson’s: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2023, 35, 497–523. [Google Scholar] [CrossRef]
- Hu, M.; Nie, J.; Lei, O.K.; Shi, Q.; Kong, Z. Acute Effect of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Appetite Perception: A Systematic Review and Meta-Analysis. Appetite 2023, 182, 106427. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Liu, X.; Shen, F.; Xu, N.B.; Li, Y.B.; Xu, K.; Li, J.; Liu, Y. Effects of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Blood Pressure in Patients with Hypertension: A Meta-Analysis. Medicine 2022, 101, e32246. [Google Scholar] [CrossRef] [PubMed]
- McClure, R.D.; Alcántara-Cordero, F.J.; Weseen, E.; Maldaner, M.; Hart, S.; Nitz, C.; Boulé, N.G.; Yardley, J.E. Systematic Review and Meta-Analysis of Blood Glucose Response to High-Intensity Interval Exercise in Adults with Type 1 Diabetes. Can. J. Diabetes 2023, 47, 171–179. [Google Scholar] [PubMed]
- Mesquita, F.O.D.S.; Gambassi, B.B.; Silva, M.D.O.; Moreira, S.R.; Neves, V.R.; Gomes-Neto, M.; Schwingel, P.A. Effect of High-Intensity Interval Training on Exercise Capacity, Blood Pressure, and Autonomic Responses in Patients with Hypertension: A Systematic Review and Meta-Analysis. Sports Health 2023, 15, 571–578. [Google Scholar] [CrossRef]
- Casaña, J.; Varangot-Reille, C.; Calatayud, J.; Suso-Martí, L.; Sanchís-Sánchez, E.; Aiguadé, R.; López-Bueno, R.; Gargallo, P.; Cuenca-Martínez, F.; Blanco-Díaz, M. High-Intensity Interval Training (HIIT) on Biological and Body Composition Variables in Patients with Musculoskeletal Disorders: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 6937. [Google Scholar] [CrossRef] [PubMed]
- Khalafi, M.; Sakhaei, M.H.; Kazeminasab, F.; Symonds, M.E.; Rosenkranz, S.K. The Impact of High-Intensity Interval Training on Vascular Function in Adults: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 1046560. [Google Scholar] [CrossRef]
- Westmacott, A.; Sanal-Hayes, N.E.M.; McLaughlin, M.; Mair, J.L.; Hayes, L.D. High-Intensity Interval Training (HIIT) in Hypoxia Improves Maximal Aerobic Capacity More Than HIIT in Normoxia: A Systematic Review, Meta-Analysis, and Meta-Regression. Int. J. Environ. Res. Public Health 2022, 19, 14261. [Google Scholar] [CrossRef]
- García-Pérez-de-Sevilla, G.; Yvert, T.; Blanco, Á.; Sosa Pedreschi, A.I.; Thuissard, I.J.; Pérez-Ruiz, M. Effectiveness of Physical Exercise Interventions on Pulmonary Function and Physical Fitness in Children and Adults with Cystic Fibrosis: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 2205. [Google Scholar] [CrossRef]
- Cuenca-Martínez, F.; Sempere-Rubio, N.; Varangot-Reille, C.; Fernández-Carnero, J.; Suso-Martí, L.; Alba-Quesada, P.; La Touche, R. Effects of High-Intensity Interval Training (HIIT) on Patients with Musculoskeletal Disorders: A Systematic Review and Meta-Analysis with a Meta-Regression and Mapping Report. Diagnostics 2022, 12, 2532. [Google Scholar] [CrossRef]
- Schulté, B.; Nieborak, L.; Leclercq, F.; Villafañe, J.H.; Sánchez Romero, E.A.; Corbellini, C. The Comparison of High-Intensity Interval Training versus Moderate-Intensity Continuous Training after Coronary Artery Bypass Graft: A Systematic Review of Recent Studies. J. Cardiovasc. Dev. Dis. 2022, 9, 328. [Google Scholar] [CrossRef]
- Chang, M.; Wang, J.; Hashim, H.A.; Xie, S.; Malik, A.A. Effect of High-Intensity Interval Training on Aerobic Capacity and Fatigue Among Patients with Prostate Cancer: A Meta-Analysis. World J. Surg. Oncol. 2022, 20, 348. [Google Scholar] [CrossRef]
- Alzar-Teruel, M.; Aibar-Almazán, A.; Hita-Contreras, F.; Carcelén-Fraile, M.d.C.; Martínez-Amat, A.; Jiménez-García, J.D.; Fábrega-Cuadros, R.; Castellote-Caballero, Y. High-Intensity Interval Training Among Middle-Aged and Older Adults for Body Composition and Muscle Strength: A Systematic Review. Front. Public Health 2022, 10, 992706. [Google Scholar] [CrossRef] [PubMed]
- Gu, T.; Hao, P.; Chen, P.; Wu, Y. A Systematic Review and Meta-Analysis of the Effectiveness of High-Intensity Interval Training in People with Cardiovascular Disease at Improving Depression and Anxiety. Evid. Based Complement. Alternat. Med. 2022, 2022, 8322484. [Google Scholar] [CrossRef] [PubMed]
- Chua, M.T.; Sim, A.; Burns, S.F. Acute and Chronic Effects of Blood Flow Restricted High-Intensity Interval Training: A Systematic Review. Sports Med. Open 2022, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.J.; Aspe, R.R.; Craig, T.P.; Kavaliauskas, M.; Babraj, J.; Swinton, P.A. The Effects of Sprint Interval Training on Physical Performance: A Systematic Review and Meta-Analysis. J. Strength Cond. Res. 2023, 37, 457–481. [Google Scholar] [CrossRef] [PubMed]
- Scoubeau, C.; Bonnechère, B.; Cnop, M.; Faoro, V.; Klass, M. Effectiveness of Whole-Body High-Intensity Interval Training on Health-Related Fitness: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 9559. [Google Scholar] [CrossRef]
- Astorino, T.A.; Causer, E.; Hazell, T.J.; Arhen, B.B.; Gurd, B.J. Change in Central Cardiovascular Function in Response to Intense Interval Training: A Systematic Review and Meta-Analysis. Med. Sci. Sports Exerc. 2022, 54, 1991–2004. [Google Scholar] [CrossRef]
- Wang, C.; Xing, J.; Zhao, B.; Wang, Y.; Zhang, L.; Wang, Y.; Zheng, M.; Liu, G. The Effects of High-Intensity Interval Training on Exercise Capacity and Prognosis in Heart Failure and Coronary Artery Disease: A Systematic Review and Meta-Analysis. Cardiovasc. Ther. 2022, 2022, 4273809. [Google Scholar] [CrossRef]
- Mateo-Gallego, R.; Madinaveitia-Nisarre, L.; Giné-Gonzalez, J.; Bea, A.M.; Guerra-Torrecilla, L.; Baila-Rueda, L.; Perez-Calahorra, S.; Civeira, F.; Lamiquiz-Moneo, I. The Effects of High-Intensity Interval Training on Glucose Metabolism, Cardiorespiratory Fitness and Weight Control in Subjects with Diabetes: Systematic Review a Meta-Analysis. Diabetes Res. Clin. Pract. 2022, 190, 109979. [Google Scholar] [CrossRef]
- De Oliveira Teles, G.; Da Silva, C.S.; Rezende, V.R.; Rebelo, A.C.S. Acute Effects of High-Intensity Interval Training on Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7049. [Google Scholar] [CrossRef]
- Cao, M.; Li, S.; Tang, Y.; Zou, Y. A Meta-Analysis of High-Intensity Interval Training on Glycolipid Metabolism in Children with Metabolic Disorders. Front. Pediatr. 2022, 10, 887852. [Google Scholar] [CrossRef]
- Khalafi, M.; Mojtahedi, S.; Ostovar, A.; Rosenkranz, S.K.; Korivi, M. High-Intensity Interval Exercise versus Moderate-Intensity Continuous Exercise on Postprandial Glucose and Insulin Responses: A Systematic Review and Meta-Analysis. Obes. Rev. 2022, 23, e13459. [Google Scholar] [CrossRef]
- Guo, Z.; Cai, J.; Wu, Z.; Gong, W. Effect of High-Intensity Interval Training Combined with Fasting in the Treatment of Overweight and Obese Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4638. [Google Scholar] [CrossRef] [PubMed]
- Bauer, N.; Sperlich, B.; Holmberg, H.-C.; Engel, F.A. Effects of High-Intensity Interval Training in School on the Physical Performance and Health of Children and Adolescents: A Systematic Review with Meta-Analysis. Sports Med. Open 2022, 8, 50. [Google Scholar] [CrossRef]
- Hu, M.; Jung, M.E.; Nie, J.; Kong, Z. Affective and Enjoyment Responses to Sprint Interval Training in Healthy Individuals: A Systematic Review and Meta-Analysis. Front. Psychol. 2022, 13, 820228. [Google Scholar] [CrossRef]
- Anjos, J.M.; Neto, M.G.; Dos Santos, F.S.; Almeida, K.d.O.; Bocchi, E.A.; Bitar, Y.d.S.L.; Duraes, A.R. The Impact of High-Intensity Interval Training on Functioning and Health-Related Quality of Life in Post-Stroke Patients: A Systematic Review with Meta-Analysis. Clin. Rehabil. 2022, 36, 726–739. [Google Scholar] [CrossRef]
- Yue, T.; Wang, Y.; Liu, H.; Kong, Z.; Qi, F. Effects of High-Intensity Interval vs. Moderate-Intensity Continuous Training on Cardiac Rehabilitation in Patients with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 845225. [Google Scholar] [CrossRef] [PubMed]
- Khalafi, M.; Ravasi, A.A.; Malandish, A.; Rosenkranz, S.K. The Impact of High-Intensity Interval Training on Postprandial Glucose and Insulin: A Systematic Review and Meta-Analysis. Diabetes Res. Clin. Pract. 2022, 186, 109815. [Google Scholar] [CrossRef] [PubMed]
- Kwok, M.M.Y.; Ng, S.S.M.; Man, S.S.; So, B.C.L. The Effect of Aquatic High Intensity Interval Training on Cardiometabolic and Physical Health Markers in Women: A Systematic Review and Meta-Analysis. J. Exerc. Sci. Fit. 2022, 20, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.K.D.; Kilic, F.; Dhawan, R.; Sidhu, R.; Elazrag, S.E.; Bijoora, M.; Sekhar, S.; Ravinarayan, S.M.; Mohammed, L. High-Intensity Interval Training among Heart Failure Patients and Heart Transplant Recipients: A Systematic Review. Cureus 2022, 14, e21333. [Google Scholar] [CrossRef]
- Lu, Z.; Song, Y.; Chen, H.; Li, S.; Teo, E.-C.; Gu, Y. A Mixed Comparisons of Aerobic Training with Different Volumes and Intensities of Physical Exercise in Patients with Hypertension: A Systematic Review and Network Meta-Analysis. Front. Cardiovasc. Med. 2022, 8, 770975. [Google Scholar] [CrossRef]
- You, Q.; Yu, L.; Li, G.; He, H.; Lv, Y. Effects of Different Intensities and Durations of Aerobic Exercise on Vascular Endothelial Function in Middle-Aged and Elderly People: A Meta-Analysis. Front. Physiol. 2022, 12, 803102. [Google Scholar] [CrossRef]
- Boullosa, D.; Dragutinovic, B.; Feuerbacher, J.F.; Benítez-Flores, S.; Coyle, E.F.; Schumann, M. Effects of Short Sprint Interval Training on Aerobic and Anaerobic Indices: A Systematic Review and Meta-Analysis. Scand. Med. Sci. Sports 2022, 32, 810–820. [Google Scholar] [CrossRef]
- Carpes, L.; Costa, R.; Schaarschmidt, B.; Reichert, T.; Ferrari, R. High-Intensity Interval Training Reduces Blood Pressure in Older Adults: A Systematic Review and Meta-Analysis. Exp. Gerontol. 2022, 158, 111657. [Google Scholar] [CrossRef]
- Edwards, J.; De Caux, A.; Donaldson, J.; Wiles, J.; O’Driscoll, J. Isometric Exercise versus High-Intensity Interval Training for the Management of Blood Pressure: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2022, 56, 506–514. [Google Scholar] [CrossRef]
- Leiva-Valderrama, J.M.; Montes-de-Oca-Garcia, A.; Opazo-Diaz, E.; Ponce-Gonzalez, J.G.; Molina-Torres, G.; Velázquez-Díaz, D.; Galán-Mercant, A. Effects of High-Intensity Interval Training on Inflammatory Biomarkers in Patients with Type 2 Diabetes. A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12644. [Google Scholar] [CrossRef]
- Li, J.; Li, Y.; Gong, F.; Huang, R.; Zhang, Q.; Liu, Z.; Lin, J.; Li, A.; Lv, Y.; Cheng, Y. Effect of Cardiac Rehabilitation Training on Patients with Coronary Heart Disease: A Systematic Review and Meta-Analysis. Ann. Palliat. Med. 2021, 10, 11901–11909. [Google Scholar] [CrossRef] [PubMed]
- Boulmpou, A.; Theodorakopoulou, M.P.; Boutou, A.K.; Alexandrou, M.-E.; Papadopoulos, C.E.; Bakaloudi, D.R.; Pella, E.; Sarafidis, P.; Vassilikos, V. Effects of Different Exercise Programs on the Cardiorespiratory Reserve in Hfpef Patients: A Systematic Review and Meta-Analysis. Hell. J. Cardiol. 2022, 64, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Tang, Y.; Li, S.; Zou, Y. Effects of High-Intensity Interval Training and Moderate-Intensity Continuous Training on Cardiometabolic Risk Factors in Overweight and Obesity Children and Adolescents: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2021, 18, 11905. [Google Scholar] [CrossRef]
- Elboim-Gabyzon, M.; Buxbaum, R.; Klein, R. The Effects of High-Intensity Interval Training (HIIT) on Fall Risk Factors in Healthy Older Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11809. [Google Scholar] [CrossRef]
- Li, D.; Chen, P. The Effects of Different Exercise Modalities in the Treatment of Cardiometabolic Risk Factors in Obese Adolescents with Sedentary Behavior—A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Children 2021, 8, 1062. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Huang, Y.; Wang, Q.; Liu, K.; Sun, G. Effects of High-Intensity Interval Training on Pulmonary Function and Exercise Capacity in Individuals with Chronic Obstructive Pulmonary Disease: A Meta-Analysis and Systematic Review. Adv. Ther. 2022, 39, 94–116. [Google Scholar] [CrossRef]
- Sabag, A.; Barr, L.; Armour, M.; Armstrong, A.; Baker, C.J.; Twigg, S.M.; Chang, D.; A Hackett, D.; E Keating, S.; George, J.; et al. The Effect of High-Intensity Interval Training vs Moderate-Intensity Continuous Training on Liver Fat: A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metabol. 2022, 107, 862–881. [Google Scholar] [CrossRef]
- Heredia-Ciuró, A.; Fernández-Sánchez, M.; Martín-Núñez, J.; Calvache-Mateo, A.; Rodríguez-Torres, J.; López-López, L.; Valenza, M.C. High-Intensity Interval Training Effects in Cardiorespiratory Fitness of Lung Cancer Survivors: A Systematic Review and Meta-Analysis. Support. Care Cancer. 2022, 30, 3017–3027. [Google Scholar] [CrossRef] [PubMed]
- Ertürk, G.; Günday, Ç.; Evrendilek, H.; Sağır, K.; Aslan, G.K. Effects of High Intensity Interval Training and Sprint Interval Training in Patients with Asthma: A Systematic Review. J. Asthma 2022, 59, 2292–2304. [Google Scholar] [CrossRef]
- Hu, J.; Wang, Z.; Lei, B.; Li, J.; Wang, R. Effects of a Low-Carbohydrate High-Fat Diet Combined with High-Intensity Interval Training on Body Composition and Maximal Oxygen Uptake: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 10740. [Google Scholar] [CrossRef]
- Fassora, M.; Calanca, L.; Jaques, C.; Mazzolai, L.; Kayser, B.; Lanzi, S. Intensity-Dependent Effects of Exercise Therapy on Walking Performance and Aerobic Fitness in Symptomatic Patients with Lower-Extremity Peripheral Artery Disease: A Systematic Review and Meta-Analysis. Vasc. Med. 2022, 27, 158–170. [Google Scholar] [CrossRef]
- Wang, K.; Zhu, Y.; Wong, S.H.-S.; Chen, Y.; Siu, P.M.-F.; Baker, J.S.; Sun, F. Effects and Dose–Response Relationship of High-Intensity Interval Training on Cardiorespiratory Fitness in Overweight and Obese Adults: A Systematic Review and Meta-Analysis. J. Sports Sci. 2021, 39, 2829–2846. [Google Scholar] [CrossRef]
- Zhu, Y.; Nan, N.; Wei, L.; Li, T.; Gao, X.; Lu, D. The Effect and Safety of High-Intensity Interval Training in the Treatment of Adolescent Obesity: A Meta-Analysis. Ann. Palliat. Med. 2021, 10, 8596–8606. [Google Scholar] [CrossRef]
- McLeod, K.A.; Jones, M.D.; Thom, J.M.; Parmenter, B.J. Resistance Training and High-Intensity Interval Training Improve Cardiometabolic Health in High Risk Older Adults: A Systematic Review and Meta-Anaylsis. Int. J. Sports Med. 2022, 43, 206–218. [Google Scholar] [CrossRef]
- Dote-Montero, M.; Carneiro-Barrera, A.; Martinez-Vizcaino, V.; Ruiz, J.R.; Amaro-Gahete, F.J. Acute Effect of HIIT on Testosterone and Cortisol Levels in Healthy Individuals: A Systematic Review and Meta-Analysis. Scand. Med. Sci. Sports 2021, 31, 1722–1744. [Google Scholar] [CrossRef] [PubMed]
- Picard, M.; Tauveron, I.; Magdasy, S.; Benichou, T.; Bagheri, R.; Ugbolue, U.C.; Navel, V.; Dutheil, F. Effect of Exercise Training on Heart Rate Variability in Type 2 Diabetes Mellitus Patients: A Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0251863. [Google Scholar] [CrossRef]
- Battista, F.; Ermolao, A.; Van Baak, M.A.; Beaulieu, K.; Blundell, J.E.; Busetto, L.; Carraça, E.V.; Encantado, J.; Dicker, D.; Farpour-Lambert, N.; et al. Effect of Exercise on Cardiometabolic Health of Adults with Overweight or Obesity: Focus on Blood Pressure, Insulin Resistance, and Intrahepatic Fat—A Systematic Review and Meta-Analysis. Obes. Rev. 2021, 22, e13269. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.-J.; Wang, Z.-Y.; Gao, H.-E.; Zhou, X.-F.; Li, F.-H. Impact of High-Intensity Interval Training on Cardiorespiratory Fitness, Body Composition, Physical Fitness, and Metabolic Parameters in Older Adults: A Meta-Analysis of Randomized Controlled Trials. Exp. Gerontol. 2021, 150, 111345. [Google Scholar] [CrossRef]
- Khalafi, M.; Symonds, M.E. The Impact of High Intensity Interval Training on Liver Fat Content in Overweight or Obese Adults: A Meta-Analysis. Physiol. Behav. 2021, 236, 113416. [Google Scholar] [CrossRef]
- Ai, J.-Y.; Chen, F.-T.; Hsieh, S.-S.; Kao, S.-C.; Chen, A.-G.; Hung, T.-M.; Chang, Y.-K. The Effect of Acute High-Intensity Interval Training on Executive Function: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3593. [Google Scholar] [CrossRef] [PubMed]
- Morze, J.; Rücker, G.; Danielewicz, A.; Przybyłowicz, K.; Neuenschwander, M.; Schlesinger, S.; Schwingshackl, L. Impact of Different Training Modalities on Anthropometric Outcomes in Patients with Obesity: A Systematic Review and Network Meta-Analysis. Obes. Rev. 2021, 22, e13218. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, K.; Matsuoka, Y.J.; Ochi, E. High-Intensity Interval Training in Breast Cancer Survivors: A Systematic Review. BMC Cancer 2021, 21, 184. [Google Scholar] [CrossRef]
- Zhang, X.; Xu, D.; Sun, G.; Jiang, Z.; Tian, J.; Shan, Q. Effects of High-Intensity Interval Training in Patients with Coronary Artery Disease after Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. Nurs. Open 2021, 8, 1424–1435. [Google Scholar] [CrossRef]
- Conceição, L.S.R.; Gois, C.O.; Fernandes, R.E.S.; Martins-Filho, P.R.S.; Neto, M.G.; Neves, V.R.; Carvalho, V.O. Effect of High-Intensity Interval Training on Aerobic Capacity and Heart Rate Control of Heart Transplant Recipients: A Systematic Review with Meta-Analysis. Braz. J. Cardiovasc. Surg. 2021, 36, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Palma, S.; Hasenoehrl, T.; Jordakieva, G.; Ramazanova, D.; Crevenna, R. High-Intensity Interval Training in the Prehabilitation of Cancer Patients—A Systematic Review and Meta-Analysis. Support. Care Cancer 2021, 29, 1781–1794. [Google Scholar] [CrossRef]
- Manresa-Rocamora, A.; Sarabia, J.M.; Sánchez-Meca, J.; Oliveira, J.; Vera-Garcia, F.J.; Moya-Ramón, M. Are the Current Cardiac Rehabilitation Programs Optimized to Improve Cardiorespiratory Fitness in Patients? A Meta-Analysis. J. Aging Phys. Act. 2021, 29, 327–342. [Google Scholar] [CrossRef]
- Hsieh, S.-S.; Chueh, T.-Y.; Huang, C.-J.; Kao, S.-C.; Hillman, C.H.; Chang, Y.-K.; Hung, T.-M. Systematic Review of the Acute and Chronic Effects of High-Intensity Interval Training on Executive Function across the Lifespan. J. Sports Sci. 2021, 39, 10–22. [Google Scholar] [CrossRef]
- Perrier-Melo, R.J.; D’Amorim, I.; Santos, T.M.; Costa, E.C.; Barbosa, R.R.; Costa, M.D.C. Effect of Active Versus Passive Recovery on Performance-Related Outcome During High-Intensity Interval Exercise. J. Sports Med. Phys. Fit. 2021, 61, 562–570. [Google Scholar] [CrossRef]
- Dupuit, M.; Maillard, F.; Pereira, B.; Marquezi, M.L.; Lancha, A.H.; Boisseau, N. Effect of High Intensity Interval Training on Body Composition in Women Before and After Menopause: A Meta-Analysis. Exp. Physiol. 2020, 105, 1470–1490. [Google Scholar] [CrossRef]
- Khalafi, M.; Symonds, M.E. The Impact of High-Intensity Interval Training on Inflammatory Markers in Metabolic Disorders: A Meta-Analysis. Scand. Med. Sci. Sports 2020, 30, 2020–2036. [Google Scholar] [CrossRef]
- Wallen, M.P.; Hennessy, D.; Brown, S.; Evans, L.; Rawstorn, J.C.; Shee, A.W.; Hall, A. High-Intensity Interval Training Improves Cardiorespiratory Fitness in Cancer Patients and Survivors: A Meta-Analysis. Eur. J. Cancer Care 2020, 29, e13267. [Google Scholar] [CrossRef] [PubMed]
- Zouhal, H.; Ben Abderrahman, A.; Khodamoradi, A.; Saeidi, A.; Jayavel, A.; Hackney, A.C.; Laher, I.; Algotar, A.M.; Jabbour, G. Effects of Physical Training on Anthropometrics, Physical and Physiological Capacities in Individuals with Obesity: A Systematic Review. Obes. Rev. 2020, 21, e13039. [Google Scholar] [CrossRef] [PubMed]
- Martin-Smith, R.; Cox, A.; Buchan, D.S.; Baker, J.S.; Grace, F.; Sculthorpe, N. High Intensity Interval Training (HIIT) Improves Cardiorespiratory Fitness (CRF) in Healthy, Overweight and Obese Adolescents: A Systematic Review and Meta-Analysis of Controlled Studies. Int. J. Environ. Res. Public Health 2020, 17, 2955. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, L.; Su, Y. Comparative Effectiveness of High-Intensity Interval Training and Moderate-Intensity Continuous Training for Cardiometabolic Risk Factors and Cardiorespiratory Fitness in Childhood Obesity: A Meta-Analysis of Randomized Controlled Trials. Front. Physiol. 2020, 11, 214. [Google Scholar] [CrossRef] [PubMed]
- Keating, C.J.; Montilla, J.Á.P.; Román, P.Á.L.; del Castillo, R.M. Comparison of High-Intensity Interval Training to Moderate-Intensity Continuous Training in Older Adults: A Systematic Review. J. Aging Phys. Act. 2020, 28, 798–807. [Google Scholar] [CrossRef]
- Leal, J.M.; Galliano, L.M.; Del Vecchio, F.B. Effectiveness of High-Intensity Interval Training versus Moderate-Intensity Continuous Training in Hypertensive Patients: A Systematic Review and Meta-Analysis. Curr. Hypertens. Rep. 2020, 22, 26. [Google Scholar] [CrossRef]
- Bouaziz, W.; Malgoyre, A.; Schmitt, E.; Lang, P.; Vogel, T.; Kanagaratnam, L. Effect of High-Intensity Interval Training and Continuous Endurance Training on Peak Oxygen Uptake Among Seniors Aged 65 or Older: A Meta-Analysis of Randomized Controlled Trials. Int. J. Clin. Pract. 2020, 74, e13490. [Google Scholar] [CrossRef]
- Wood, G.; Murrell, A.; Van Der Touw, T.; Smart, N. HIIT Is Not Superior to MICT in Altering Blood Lipids: A Systematic Review and Meta-Analysis. BMJ Open Sport Exerc. Med. 2019, 5, e000647. [Google Scholar] [CrossRef]
- Martland, R.; Mondelli, V.; Gaughran, F.; Stubbs, B. Can High-Intensity Interval Training Improve Physical and Mental Health Outcomes? A Meta-Review of 33 Systematic Reviews Across the Lifespan. J. Sports Sci. 2020, 38, 430–469. [Google Scholar] [CrossRef] [PubMed]
- Martland, R.; Mondelli, V.; Gaughran, F.; Stubbs, B. Can High Intensity Interval Training Improve Health Outcomes Among People with Mental Illness? A Systematic Review and Preliminary Meta-Analysis of Intervention Studies Across a Range of Mental Illnesses. J. Affect. Dis. 2020, 263, 629–660. [Google Scholar] [CrossRef] [PubMed]
- Lora-Pozo, I.; Lucena-Anton, D.; Salazar, A.; Galán-Mercant, A.; Moral-Munoz, J.A. Anthropometric, Cardiopulmonary and Metabolic Benefits of the High-Intensity Interval Training Versus Moderate, Low-Intensity or Control for Type 2 Diabetes: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4524. [Google Scholar] [CrossRef] [PubMed]
- Adolfo, J.R.; Dhein, W.; Sbruzzi, G. Intensity of Physical Exercise and Its Effect on Functional Capacity in COPD: Systematic Review and Meta-Analysis. J. Bras. Pneumol. 2019, 45, e20180011. [Google Scholar] [CrossRef]
- Pymer, S.; Palmer, J.; Harwood, A.E.; Ingle, L.; Smith, G.E.; Chetter, I.C. A Systematic Review of High-Intensity Interval Training as an Exercise Intervention for Intermittent Claudication. J. Vasc. Surg. 2019, 70, 2076–2087. [Google Scholar] [CrossRef]
- Campbell, W.W.; Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; et al. High-Intensity Interval Training for Cardiometabolic Disease Prevention. Med. Sci. Sports Exerc. 2019, 51, 1220–1226. [Google Scholar] [CrossRef]
- Cao, M.; Quan, M.; Zhuang, J. Effect of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Cardiorespiratory Fitness in Children and Adolescents: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1533. [Google Scholar] [CrossRef]
- Wiener, J.; McIntyre, A.; Janssen, S.; Chow, J.T.; Batey, C.; Teasell, R. Effectiveness of High-Intensity Interval Training for Fitness and Mobility Post Stroke: A Systematic Review. PM&R 2019, 11, 868–878. [Google Scholar]
- Way, K.L.; Sultana, R.N.; Sabag, A.; Baker, M.K.; Johnson, N.A. The Effect of High Intensity Interval Training Versus Moderate Intensity Continuous Training on Arterial Stiffness and 24 H Blood Pressure Responses: A Systematic Review and Meta-Analysis. J. Sci. Med. Sport 2019, 22, 385–391. [Google Scholar] [CrossRef]
- Delgado-Floody, P.; Latorre-Román, P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; García-Pinillos, F. Feasibility of Incorporating High-Intensity Interval Training into Physical Education Programs to Improve Body Composition and Cardiorespiratory Capacity of Overweight and Obese Children: A Systematic Review. J. Exerc. Sci. Fit. 2019, 17, 35–40. [Google Scholar] [CrossRef]
- Da Silva, D.E.; Grande, A.J.; Roever, L.; Tse, G.; Liu, T.; Biondi-Zoccai, G.; de Farias, J.M. High-Intensity Interval Training in Patients with Type 2 Diabetes Mellitus: A Systematic Review. Curr. Atheroscler. Rep. 2019, 21, 8. [Google Scholar] [CrossRef]
- Su, L.; Fu, J.; Sun, S.; Zhao, G.; Cheng, W.; Dou, C.; Quan, M. Effects of HIIT and MICT on Cardiovascular Risk Factors in Adults with Overweight and/or Obesity: A Meta-Analysis. PLoS ONE 2019, 14, e0210644. [Google Scholar] [CrossRef]
- Andreato, L.V.; Esteves, J.V.; Coimbra, D.R.; Moraes, A.J.P.; De Carvalho, T. The Influence of High-Intensity Interval Training on Anthropometric Variables of Adults with Overweight or Obesity: A Systematic Review and Network Meta-Analysis. Obes. Rev. 2019, 20, 142–155. [Google Scholar] [CrossRef] [PubMed]
- Wewege, M.A.; Ahn, D.; Yu, J.; Liou, K.; Keech, A. High-Intensity Interval Training for Patients with Cardiovascular Disease—Is It Safe? A Systematic Review. J. Am. Heart Assoc. 2018, 7, e009305. [Google Scholar] [CrossRef]
- Abreu, R.M.D.; Rehder-Santos, P.; Simões, R.P.; Catai, A.M. Can High-Intensity Interval Training Change Cardiac Autonomic Control? A Systematic Review. Braz. J. Phys. Ther. 2019, 23, 279–289. [Google Scholar] [CrossRef]
- Tucker, W.J.; Beaudry, R.I.; Liang, Y.; Clark, A.M.; Tomczak, C.R.; Nelson, M.D.; Ellingsen, O.; Haykowsky, M.J. Meta-Analysis of Exercise Training on Left Ventricular Ejection Fraction in Heart Failure with Reduced Ejection Fraction: A 10-Year Update. Prog. Cardiovasc. Dis. 2019, 62, 163–171. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, L.; Li, P.; Li, N.; Xu, Y. Effectiveness of High-Intensity Interval Training on Glycemic Control and Cardiorespiratory Fitness in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2019, 31, 575–593. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.C.; Hay, J.L.; Kehler, D.S.; Boreskie, K.F.; Arora, R.C.; Umpierre, D.; Szwajcer, A.; Duhamel, T.A. Effects of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Blood Pressure in Adults with Pre- to Established Hypertension: A Systematic Review and Meta-Analysis of Randomized Trials. Sports Med. 2018, 48, 2127–2142. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, B.R.R.; Santos, T.M.; Kilpatrick, M.; Pires, F.O.; Deslandes, A.C. Affective and Enjoyment Responses in High Intensity Interval Training and Continuous Training: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0197124. [Google Scholar] [CrossRef]
- Gomes Neto, M.; Durães, A.R.; Conceição, L.S.R.; Saquetto, M.B.; Ellingsen, Ø.; Carvalho, V.O. High Intensity Interval Training Versus Moderate Intensity Continuous Training on Exercise Capacity and Quality of Life in Patients with Heart Failure with Reduced Ejection Fraction: A Systematic Review and Meta-Analysis. Int. J. Cardiol. 2018, 261, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Perrier-Melo, R.J.; Figueira, F.A.M.D.S.; Guimarães, G.V.; Costa, M.D.C. High-Intensity Interval Training in Heart Transplant Recipients: A Systematic Review with Meta-Analysis. Arq. Bras. Cardiol. 2018, 110, 188–194. [Google Scholar] [CrossRef]
- Hannan, A.; Hing, W.; Simas, V.; Climstein, M.; Coombes, J.S.; Jayasinghe, R.; Byrnes, J.; Furness, J. High-Intensity Interval Training Versus Moderate-Intensity Continuous Training Within Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. Open Access J. Sports Med. 2018, 9, 1–17. [Google Scholar] [CrossRef] [PubMed]
- De Nardi, A.T.; Tolves, T.; Lenzi, T.L.; Signori, L.U.; Silva, A.M.V.D. High-Intensity Interval Training Versus Continuous Training on Physiological and Metabolic Variables in Prediabetes and Type 2 Diabetes: A Meta-Analysis. Diabetes Res. Clin. Pract. 2018, 137, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Maillard, F.; Pereira, B.; Boisseau, N. Effect of High-Intensity Interval Training on Total, Abdominal and Visceral Fat Mass: A Meta-Analysis. Sports Med. 2018, 48, 269–288. [Google Scholar] [CrossRef]
- Gomes-Neto, M.; Durães, A.R.; Reis, H.F.C.D.; Neves, V.R.; Martinez, B.P.; Carvalho, V.O. High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Exercise Capacity and Quality of Life in Patients with Coronary Artery Disease: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiolog. 2017, 24, 1696–1707. [Google Scholar] [CrossRef]
- Wewege, M.; Van Den Berg, R.; Ward, R.E.; Keech, A. The Effects of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Body Composition in Overweight and Obese Adults: A Systematic Review and Meta-Analysis. Obes. Rev. 2017, 18, 635–646. [Google Scholar] [CrossRef]
- Xie, B.; Yan, X.; Cai, X.; Li, J. Effects of High-Intensity Interval Training on Aerobic Capacity in Cardiac Patients: A Systematic Review with Meta-Analysis. BioMed Res. Int. 2017, 2017, 5420840. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Cerrillo-Urbina, A.J.; Herrera-Valenzuela, T.; Cristi-Montero, C.; Saavedra, J.M.; Martínez-Vizcaíno, V. Is High-Intensity Interval Training More Effective on Improving Cardiometabolic Risk and Aerobic Capacity Than Other Forms of Exercise in Overweight and Obese Youth? A Meta-Analysis. Obes. Rev. 2016, 17, 531–540. [Google Scholar] [CrossRef]
- Jelleyman, C.; Yates, T.; O’Donovan, G.; Gray, L.J.; King, J.A.; Khunti, K.; Davies, M.J. The Effects of High-Intensity Interval Training on Glucose Regulation and Insulin Resistance: A Meta-Analysis. Obes. Rev. 2015, 16, 942–961. [Google Scholar] [CrossRef]
- Liou, K.; Ho, S.; Fildes, J.; Ooi, S.-Y. High Intensity Interval Versus Moderate Intensity Continuous Training in Patients with Coronary Artery Disease: A Meta-Analysis of Physiological and Clinical Parameters. Heart Lung Circ. 2016, 25, 166–174. [Google Scholar] [CrossRef]
- Milanović, Z.; Sporiš, G.; Weston, M. Effectiveness of High-Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta-Analysis of Controlled Trials. Sports Med. 2015, 45, 1469–1481. [Google Scholar] [CrossRef] [PubMed]
- Elliott, A.D.; Rajopadhyaya, K.; Bentley, D.J.; Beltrame, J.F.; Aromataris, E.C. Interval Training Versus Continuous Exercise in Patients with Coronary Artery Disease: A Meta-Analysis. Heart Lung Circ. 2015, 24, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Haykowsky, M.J.; Timmons, M.P.; Kruger, C.; McNeely, M.; Taylor, D.A.; Clark, A.M. Meta-Analysis of Aerobic Interval Training on Exercise Capacity and Systolic Function in Patients with Heart Failure and Reduced Ejection Fractions. Am. J. Cardiol. 2013, 111, 1466–1469. [Google Scholar] [CrossRef] [PubMed]
- Sousa, M.; Oliveira, R.; Brito, J.P.; Martins, A.D.; Moutão, J.; Alves, S. Effects of Combined Training Programs in Individuals with Fibromyalgia: A Systematic Review. Healthcare 2023, 11, 1708. [Google Scholar] [CrossRef]
- Wang, L.; Quan, M.; Nieman, D.C.; Li, F.; Shi, H.; Bai, X.; Xiong, T.; Wei, X.; Chen, P.; Shi, Y. Effects of High-Intensity Interval Training and Combined High-Intensity Interval Training Programs on Cancer-Related Fatigue and Cancer Pain: A Systematic Review and Meta-Analysis. Med. Sci. Sports Exerc. 2023, 55, 1620–1631. [Google Scholar] [CrossRef]
- Hua, J.; Sun, L.; Teng, Y. Effects of High-Intensity Strength Training in Adults with Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2023, 102, 292–299. [Google Scholar] [CrossRef]
| Author, Citation | Study Design | Study Goals | N of Patients Included in the Analysis | Total Number of Studies Included in the Meta-Analysis | Diagnosis | Comorbidities | Study Conclusions |
|---|---|---|---|---|---|---|---|
| [117] | SR | Cardiac autonomic responses | 193 | 6 | Healthy, CAD, CHD, MetS | - | Augmented parasympathetic and/or sympathetic modulation |
| [106] | SR + MA | VO2max | 295 | 6 | COPD | - | HIIT is similar in improving VO2max in comparison with traditional exercises |
| [84] | SR | Executive function | 720 | 24 | Healthy | - | HIIT improves executive function |
| [21] | SR | Cognitive and psychological outcomes | 652 | 8 | Healthy teenagers | - | HIIT improves cognitive and psychological health in young people |
| [40] | SR | Body composition, muscle strength, physical function | 615 | 8 | Healthy | - | HIIT improves body composition and muscle strength |
| [115] | MA | Anthropometric outcomes | 1222 | 48 | Overweight, obese, healthy | - | Comparable results between HIIT and MIIT |
| [54] | SR + MA | QoL, VO2max | 375 | 9 | Stroke | - | HIIT enhanced post-stroke rehabilitation and VO2max |
| [15] | SR + MA | VO2max, QoL | 129 | 7 in qualitative review, 5 in meta-analysis | Heart failure (HF) | - | Comparable advantages of HIIT inVO2 peak, QoL, LVEF |
| [45] | SR + MA | SV, blood volume, hematocrit, VO2max | 946 | 45 | Overweight, obesity, COPD, schizophrenia, HF, CAD, MetS, T2DM | - | HIIT improves VO2max, and consequently blood parameters |
| [16] | SR + MA | VO2max | 404 | 19 | CAD, HF | - | More effective results of HIT in HF than CAD patients |
| [2] | SR + MA | Cardio- and metabolic outcomes | 2164 | 65 | Overweight, obese, healthy patients | - | Improvement of short-term and long-term HIIT on VO2max in healthy adults |
| [81] | SR + MA | BP, insulin resistance, intrahepatic fat | 3033 | 54 | Overweight or obesity | HTN, T2DM, Metabolic syndrome, NAFLD, Dyslipidaemia, NASH | HIIT improves cardiometabolic outcomes |
| [52] | SR + MA | HR, VO2max, glucose, BP, insulin, insulin resistance | 707 | 11 | Healthy children | - | HIIT improved exercise capacity and glucose levels |
| [101] | SR + MA | VO2max | 480 | 15 | Health and unhealthy | - | HIIT improves VO2max |
| [61] | SR + MA | VO2max | 438 | 18 | Healthy | - | Sprint interval exercise improves VO2max |
| [66] | SR + MA | VO2max, QoL, exercise capacity, cardiac parameters | 515 | 11 | HF | - | HIIT improves VO2max and exercise capacity |
| [108] | SR + MA | Efficacy, safety | 228 | 11 articles describing 7 studies | MS | - | Safety and efficacy of HIIT |
| [109] | MA | CRF | 563 | 17 | Healthy minors aged < 18 | - | Favorable outcome for CRF in HIIT than MICT |
| [67] | SR + MA | VO2max, BP, body composition, glucose, insulin, insulin resistance, lipid profile | 325 | 12 | Children with overweight, obesity | - | HIIT improves VO2max, and SBP |
| [49] | SR + MA | Lipid profile, blood glucose, insulin, insulin resistance | 538 | 18 | Children with MetS | Obesity, overweight, asthma, NAFLD | HIIT improves lipid profile and blood glucose |
| [62] | SR + MA | BP | 266 | 10 | HTN | Parkinson, urology, HF | HIIT decreases BP |
| [33] | SR + MA | Body composition, HR, BP, CRP | 380 | 8 | MSK disorders | - | HIIT affected only heart rate |
| [39] | SR + MA | VO2max, fatigue, inflammatory markers | 215 | 6 | Prostate cancer | - | HIIT improves VO2max, fatigue, PSA, but not inflammatory markers |
| [42] | SR | VO2max, blood lactate, creatine kinase | 244 | 18 | Healthy | - | HIIT improves exercise capacity |
| [88] | SR + MA | VO2max, heart rate | 212 | 5 | Heart transplantation | - | HIIT improves VO2max and heart rate |
| [120] | SR + MA | BP, VO2max | 143 | 9 in qualitative review, meta-analysis: 9 for VO2max, 7 for BP | Pre-HTN, HTN | CHF, CHD, MetS, abdominal obesity, pre-T2DM | No difference in BP at rest, improved VO2max |
| [37] | SR + MA | Pain, VO2max, QoL | 530 | 13 | MSK disorders | - | HIIT decreases pain, improves VO2max, but not QoL |
| [113] | SR | BG | 325 (drop-out 182) | 5 | T2DM | - | No sufficient evidence |
| [125] | SR + MA | Functional capacity and cardiometabolic outcomes | 184 | 7 in qualitative review, 5 in meta-analysis | Pre- and T2DM | - | More favorable functional capacity of HIIT but comparable cardiometabolic outcomes of HIIT and MICT |
| [48] | SR | Glucose, inflammatory markers, lipid profile | 168 | 14 | T2DM, T1DM | - | HIIT improves glycemic control |
| [32] | SR + MA | Exercise capacity, BP, VO2max | 569 | 9 | HTN | - | HIIT is superior to moderate intensity exercise in improving VO2max |
| [112] | SR | Body composition, CRF | 136 | 6 | Overweight | - | Favorable effect of HIIT on body composition |
| [79] | SR + MA | Testosterone and cortisol | 890 | 60 | Healthy | - | Testosterone and cortisol increase immediately and return to baseline in one day |
| [93] | SR + MA | Body composition | 959 | 38 | Females | Overweight, obesity, T2DM, PCOS, dislipidemia, rheumatic disease, metabolic syndrome | HIIT helps reducing weight and fat |
| [63] | SR + MA | BP, HR | 1583 | 38 | HTN | - | HIIT decreases BP worse than isometric exercise training, but better reduces HR |
| [68] | SR | Fall risk factors, physical activity, QoL | 328 | 11 | Healthy | - | HIIT is safe and effective in fall prevention |
| [134] | MA | VO2 peak | 229 | 6 | CAD (CABG, AP, MI, PCI) | - | More favorable outcome for VO2max and anaerobic threshold in HIIT |
| [73] | SR | Anthropometric and CVS parameters, lung function, cardiorespiratory fitness, asthma symptoms and control, QoL | 841 | 7 | Asthma | - | HIIT improved FEV1 and oxygen consumption |
| [75] | SR + MA | Pain-free walking distance and oxygen consumption | 1132 | 19 | Lower extremity PAD | - | HIIT was less effective in walking distance than light-to-moderate PA, but more effective in maximal oxygen consumption |
| [70] | SR + MA | Pulmonary function, dyspnea, QoL, adverse events, VO2max | 689 | 12 | COPD | - | HIIT improves pulmonary function, QoL, dyspnea, VO2max |
| [130] | SR + MA | Cardiometabolic outcomes and VO2max | 274 | 9 | Overweight and obese children < 18 | - | More favorable outcome in BP and VO2max for HIIT |
| [36] | SR + MA | Pulmonary function, VO2max, muscle strength | 399 | 12 | CF | - | HIIT improves VO2max, muscle strength, but not lung function |
| [127] | SR + MA | VO2max, QoL | 609 | 12 | CAD | - | Improved VO2max for HIIT, but no difference in QoL |
| [122] | SR + MA | VO2max | 411 | 13 | HFREF | - | Superiority of HIIT over MICT in VO2max |
| [41] | SR + MA | Severity of depression and anxiety | 515 | 12 | CAD, angina, arrhythmias, HF, HTN, stroke, MI, atherosclerosis, CMP, Parkinson | - | HIIT improves depression, but not anxiety |
| [51] | SR + MA | Body composition, VO2max, glucose, insulin | 230 | 9 | Overweight, obesity | - | HIIT and fasting improve glucose |
| [43] | SR + MA | VO2max, exercise capacity | 846 | 55 | Healthy | - | HIIT improves exercise capacity |
| [124] | SR + MA | CRF, AE | 953 | 17 | CAD (MI, PCI, CABG, PTCA) | - | Improved CRF in HIIT group. No difference in AE |
| [28] | SR + MA | Safety, VO2max | 117 | 11 | Parkinson | - | HIIT is safe, improves VO2max and motor functions |
| [135] | SR + MA | VO2 peak, LVEF | 168 | 7 | HFREF | - | Higher effectiveness of HIIT than MICT on VO2max improvement |
| [72] | SR + MA | VO2max | 305 | 8 | Lung cancer | - | Favorable effects of HIIT on oxygen consumption |
| [91] | SR | Executive function, heart rate, VO2max | 1223 | 23 | Healthy children and adults | - | HIIT improves cognitive executive functions |
| [74] | SR + MA | Weight, BMI, fat percentage, oxygen consumption | 129 | 10 | All adults | Diabetes, overweight, obese | Diet and HIIT reduce weight and fat |
| [53] | SR + MA | Exercise enjoyment | 675 | 25 | Healthy | - | Participants enjoyed sprint exercises comparable to HIIT |
| [29] | SR + MA | Appetite | 169 | 13 | Healthy | - | Both HIIT and moderate exercise reduced appetite |
| [131] | MA | T2DM-related outcomes, weight, CRF | 2035 | 50 (36 controlled, 14 one-group) | Healthy, sedentary, overweight, obese | T2DM, MetS, HF, CAD, MI, angina, schizophrenia, cancer | Favorable effects of HIIT on insulin resistance, fasting glucose and HbA1c levels, body weight, and CRF |
| [99] | SR | VO2max | 259 | 15 | HF, COPD, T2DM, CAD, cancer | - | HIIT can improve VO2max similar to moderate-intensity exercise |
| [94] | SR + MA | Inflammatory markers | 841 | 29 | Overweight, obesity, T2DM, PCOS, metabolic syndrome, NAFLD | - | HIIT decreases inflammatory markers |
| [83] | SR + MA | Liver fat percentage | 333 | 10 | Overweight or obesity | CAD, NAFLD, T2DM | HIIT improves liver fat content |
| [34] | SR + MA | Vascular function | 1437 | 36 | Overweight, obesity, MetS, T2DM, T1DM, PCOS, HTN, HF, CAD, MI, heart transplant, ToF, cancer | - | HIIT improves vascular function |
| [50] | SR + MA | Blood glucose, insulin | 467 | 30 | MetS | Overweight, obesity, T2DM | HIIT improves insulin and glucose responses |
| [56] | SR + MA | Glucose, insulin | 870 | 25 | T2DM, HTN, obesity, NAFLD, overweight | - | HIIT improves glucose and insulin levels |
| [20] | SR + MA | Safety, VO2max, body composition, psychological health, QoL | 366 | 9 | Severe mental illness | - | HIIT shows adherence, is safe, decreases depression, improves VO2max |
| [57] | SR + MA | VO2max, BP, body composition, knee strength, HR, lipid profile | 476 | 13 | Healthy | - | Aquatic HIIT improves body composition, lipid profile, vitals, knee strength, and VO2max |
| [19] | SR + MA | Cognitive and mental health | 2092 | 22 | Children | - | HIIT can improve cognitive and mental health |
| [100] | SR + MA | Blood pressure, VO2max | 269 | 15 | HTN | HF, obesity, overweight, CAD, metabolic syndrome | HIIT decreases blood pressure. It is superior to moderate intensity exercise in improving VO2max |
| [64] | SR | Body composition, inflammatory markers | 258 | 7 | T2DM | - | HIIT decreases inflammatory marker levels |
| [65] | SR + MA | VO2max, lipid profile, QoL, cardiac parameters | 465 | 8 | HF, MI, ToF | - | HIIT and moderate intensity exercises improve VO2max |
| [69] | SR + MA | Lipid profile, body composition, insulin resistance, VO2max, | 704 | 19 | Obese children | - | Aerobic exercises reduce the risk of CVD, mixed exercises reduces the risk of diabetes |
| [30] | SR + MA | BP, HR, VO2max | 442 | 13 | HTN | - | HIIT better decreases SBP at daytime than moderate exercise |
| [132] | MA | VO2max and CV outcomes | 472 | 10 | CAD | - | Improved mean VO2max in HIIT group |
| [119] | SR + MA | T2DM control, CRF | 345 | 13 | T2DM | - | Superiority of HIIT over MICT or no training on body composition, VO2peak, and HbA1c level |
| [98] | SR + MA | VO2max, body composition, blood pressure, lipid profile, blood glucose | 309 | 9 | Childhood obesity | - | HIIT improves VO2max, body composition, and blood pressure |
| [105] | SR + MA | Body composition, cardiopulmonary parameters | 548 | 10 | T2DM | HTN, obesity, renal diseases, cardiovascular diseases | HIIT improves body composition and cardiopulmonary outcomes |
| [59] | SR + Network MA | BP, BMI, HR | 846 | 12 | HTN | - | Moderate intensity exercise lowers BP better than HIIT. HIIT better improves exercise capacity |
| [126] | MA | Body adiposity | 617 | 39 | Healthy, overweight, obese, sedentary adults, | Pre- and T2DM, MetS, PMW, NAFLD, PCOS, rheumatic disease | Reduction in HIIT of visceral, abdominal, and total fat |
| [90] | SR + MA | VO2max | 1417 | 29 | MI | - | HIIT improves VO2max |
| [97] | SR + MA | VO2max | 1201 | 18 | Overweight, obesity teenagers | - | HIIT improves VO2max |
| [103] | Meta-review | VO2max, body composition, blood glucose, blood pressure, inflammatory markers, exercise capacity, cognitive and mental health, QoL, safety, adherence | 19566 | 33 | DM, metabolic syndrome, HF, CAD, COPD | - | HIIT is beneficial for physical and mental health, its adherence is high, and it is safe |
| [104] | SR + MA | VO2max, mental health, body composition, inflammatory markers, QoL, adverse events | 360 | 12 | Mental illness: anxiety, eating, stress disorders | - | HIIT improves physical and mental health |
| [17] | SR + MA | Effects of HIIT on psychological and physical illness, including sleep | 2901 | 53 | General population | Cardiometabolic disorders COPD, Cancer, stroke, Crohn’s disease, Cutaneous systemic sclerosis, and liver resection. | Beneficial effects of HIIT on physical and mental health |
| [47] | SR + MA | VO2max, glucose, weight, glycemic control, insulin, insulin resistance | 708 | 19 | T2DM | Metabolic syndrome, obesity, NAFLD | HIIT improves glycemic control and insulin resistance |
| [31] | SR + MA | Blood glucose | 155 | 15 | T1DM | - | Inconsistent effects on blood glucose |
| [78] | SR + MA | Body composition, lipid profile, blood glucose | 422 | 9 | Overweight or obesity, HTN, dyslipidemia, hyperglycemia, insulin resistance | - | HIIT improves body composition, lab analyses, and exercise capacity |
| [133] | SR + MA | VO2max | 723 | 28 | Healthy | - | Higher improvement in VO2max in after HIIT than endurance training |
| [17] | SR + MA | Primary: sleep quality Secondary: anxiety, depression and health-related QoL | 755 | 21 | All adults | RA, CKD, testicular cancer, prostate cancer, overweight, obesity, sleep apnea, depression, insomnia, Parkinson, axial spinal arthritis, drug use disorders | HIIT improves sleep |
| [85] | SR + network MA | Body composition, fat percentage | 4774 | 32 | Obesity | - | Aerobic with resistance training can improve body composition |
| [24] | SR + MA | Physical well-being and health outcomes | 448 | 12 | Cancer | Various cancer types | Comparably favorable effect of HIIT and MIE; superiority of HIIT over UC for VO2max |
| [121] | SR + MA | Emotional outcomes | 156 | 8 | Active, sedentary | - | Favorable emotional outcomes of HIIT |
| [89] | SR + MA | Safety, VO2max | 896 | 8 | Cancer: lung, breast, bladder, rectal, liver | - | HIIT is beneficial and safe |
| [25] | SR + MA | Fasting glucose, glycemic control, insulin resistance, body composition, lipid profile, BP, VO2max | 69 | 5 | T2DM | - | HIIT improves glycemic control, insulin resistance, body composition, VO2max, and lipid profile |
| [123] | SR + MA | VO2peak, hemodynamic outcomes | 118 | 3 | Heart transplant recipients | - | Increased peak HR and VO2max following 8–12 week HIIT |
| [92] | |||||||
| [22] | SR + MA | Peak VO2max | 145 | 16 | spinal cord injury | - | HIIT is beneficial for CVS health, but not superior to other exercises |
| [80] | SR + MA | Cardiorespiratory parameters | 523 | 21 | T2DM | - | HIIT improves cardiorespiratory parameters |
| [13] | SR + MA | VO2max | 429 | 14 | Healthy | - | HIIT improves fitness |
| [107] | SR + MA | Intermittent claudication, VO2max | 350 | 9 articles describing 8 studies | Peripheral arterial disease | - | Improvement in distance walked and VO2max |
| [12] | SR + MA | QoL, AEs, vitals, peak VO2max, LVEF, LVEDV | 387 | 8 | Post-MI | - | HIIT is safe and improves exercise capacity |
| [10] | SR + MA | Vascular outcomes | 182 | 7 | HF, MetS, HTN, T2DM, PMW, obese | - | Enhanced function of BAVF following 12 week or longer HIIT |
| [14] | SR + MA | Body fat, VO2max | 784 | 26 | Overweight or obesity | - | HIIT was less effective than moderate exercise in increasing VO2max |
| [71] | SR + MA | Liver fat | 745 | 19 | T2DM, NAFLD, obesity, liver steatosis | - | HIIT improves liver fat content similar to moderate intensity exercise |
| [26] | SR + MA | Endothelial function | 208 | 8 | Overweight, obesity | - | HIIT improves endothelial function |
| [9] | SR + MA | Insulin resistance, BMI | 423 | 7 | PCOS | - | HIIT improve insulin resistance and BMI |
| [38] | SR | QoL, VO2max | 379 | 5 | CABG patients | CAD, MI | HIIT improves QoL and VO2max |
| [44] | SR + MA | Body composition, VO2max, lipid profile, blood glucose | 657 | 22 | Healthy | Obesity, sarcopenia | HIIT improves body composition, but is less effective in improving VO2max in comparison with traditional exercise |
| [8] | SR + MA | Body composition parameters, lipid profile, fasting glucose, blood pressure | 414 | 10 | Metabolic syndrome | - | HIIT improves blood pressure, blood glucose levels, and body composition |
| [23] | SR + MA | Peak VO2max | 384 | 5 | oncological resections | - | HIIT improves preop fitness |
| [11] | SR + MA | Changes in BMI, fat percentage, cardiometabolic risk factors, heart rate, oxygen consumption | 512 | 11 | Children | Overweight, obesity | HIIT improves cholesterol profile and cardiometabolic parameters in children |
| [27] | SR + MA | Functional movement | 851 | 18 | HTN, obesity, Alzheimer, COPD, CAD, HF, CAD | - | HIIT improves functional movement |
| [114] | MA | CVD outcomes | 620 | 22 | Overweight/obese | - | Improved body composition, TC, VO2max in HIIT group |
| [7] | SR + MA | Body composition, VO2max | 1422 | 47 | Overweight, obesity | T2DM, Down syndrome, MetS, NAFLD, cancer | Improvement in VO2max, but not body composition |
| [86] | SR | VO2max | 639 | 12 | Breast cancer | - | HIIT improves cardiorespiratory fitness |
| [118] | SR + MA | LVEF | 1078 | 18 | HFREF | - | Superiority of 2- 3-month HIIT on improving LVEF |
| [95] | SR + MA | VO2max, safety | 516 | 12 | Cancer: liver, lung, rectal, bladder, breast, testicular | - | HIIT improves VO2max |
| [76] | SR + MA | Peak VO2max | 543 | 19 | Overweight, obesity | NAFLD, T2DM | HIIT improves cardiorespiratory fitness |
| [46] | SR + MA | VO2max, LVEF | 664 | 15 | CAD, HF | - | HIIT improves VO2max and LVEF |
| [111] | SR + MA | Central arterial stiffness, 24 h BP | 491 | 16 | Any health status | - | Reduction in diastolic BP at night in HIIT versus MICT |
| [35] | SR + MA | VO2max | 194 | 9 | Healthy | - | HIIT improved VO2max in normoxia and hypoxia |
| [128] | SR + MA | Body composition | 424 | 13 | Overweight/obese adults aged 18–45 | - | Comparable slight improvement in body composition (but not weight) |
| [116] | SR | CV outcomes | 1117 | 23 | CAD (MI, PCI, CABG) | - | Low risk of CV AE following HIIT |
| [11] | SR | VO2max, mobility | 140 | 6 | Stroke | - | Improved VO2max and mobility compared to baseline but not to MICT |
| [102] | SR + MA | Lipid profile, heart rate, VO2max | 791 | 26 | HTN, overweight, obesity | - | HIIT and moderate exercise are similar in improving lipid profile. HIIT is superior to moderate exercise in improving HDL |
| [82] | SR + MA | VO2max, body composition, metabolic parameters | 1156 | 29 | Older patients | - | HIIT was beneficial at improving fitness |
| [129] | SR + MA | VO2max | 736 | 21 | Cardiac patients | - | Improved VO2 peak |
| [60] | SR + MA | Endothelial function | 221 | 9 | Healthy | - | Aerobic function improves endothelial function |
| [58] | SR and MA | VO2max | 520 | 10 | CHD, HF | - | HIIT improves VO2max and QoL |
| [55] | SR + MA | VO2max | 949 | 22 | CAD, HF, MI, heart transplant | - | HIIT improves VO2max |
| [87] | SR + MA | Lipid profile, restenosis, cardiopulmonary parameters | 247 | 6 | CAD | - | HIIT improves cardiopulmonary parameters, but not heart rate |
| [77] | SR + MA | Peak VO2max, HR, body composition | 488 | 11 | Obesity | - | HIIT reduces fat and BMI |
| [96] | SR | VO2max, body composition, exercise performance | 6768 | 116 | Obesity | HF, T2DM | HIIT improves VO2max and body composition |
| [136] | SR | Physical fitness and functional capacity | 834 | 13 | Fibromyalgia | - | Combined training programs are the most effective for patients with fibromyalgia |
| [137] | SR + MA | VO2max, AE, pain, and QoL | 938 | 12 | Cancer-related fatigue | Pain related to cancer | HIIT and combined HIIT can reduce pain and cancer-related fatigue |
| [138] | SR + MA | VO2max, AE, pain, and QoL | 892 | 10 | Knee osteoarthritis | - | HIIT have comparable effects with low-intensity training |
| Included Study | Category | Reported Mechanism and Frequency (If Reported) | Direction |
|---|---|---|---|
| [117] | Cardiometabolic | Parasympathetic and/or sympathetic modulation. | Positive |
| [106] | Cardiometabolic | Physiological mimicry and lower dynamic hyperinflation. | Comparable |
| [84] | Neurologic | Raising of H2O2 and TNF-α activates PGC-1α, which promotes brain-derived neurotrophic factor (BDNF) synthesis. Prefrontal cortex activation. Alterations in lactate and catecholamine levels. | Positive |
| [21] | Neurologic | Reported best intervals: 4–16 weeks, for 8–30 min/session, psychosocial mechanism: ability to improve self-concept, self-esteem, cognitive ability, and self-perception in youth. | Positive |
| [40] | Cardiometabolic | Reported no differences between training 1, 2, or 3 days per week. The mechanism involves axonal regeneration for muscle growth promotion. | Comparable |
| [115] | Metabolic | Decreases body mass. | Comparable |
| [54] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [15] | Cardiometabolic | Increased oxygen uptake. | Comparable |
| [45] | Cardiometabolic | Adaptations in central oxygen transport and/or peripheral oxygen extraction. | Positive |
| [16] | Cardiometabolic | The maximum benefits are between weeks 6 and 12. The mechanism involves increased oxygen uptake. | Positive |
| [2] | Cardiometabolic | Duration for at least 12 weeks. Increased baroreflex-mediated modulation of the sinoatrial node. | Positive |
| [81] | Cardiometabolic | Improvement in insulin sensitivity, glucose uptake, mitochondrial lipid oxidation, and arterial flexibility. | Positive |
| [52] | Cardiometabolic | At least 5 days duration (for children). Neuromuscular exercises (sit-ups and push-ups) are the most effective for adolescents. | Positive |
| [101] | Cardiometabolic | Peripheral muscle and central cardiorespiratory adaptation | Positive |
| [61] | Cardiometabolic | Duration is more than 2 weeks. Increased oxygen uptake. | Positive |
| [66] | Cardiometabolic | Peripheral mechanisms that lead to ameliorated oxygen utilization by skeletal muscles. | Positive |
| [108] | Cardiometabolic | Can improve insulin sensitivity and blood pressure. | Positive |
| [109] | Cardiometabolic | Mitochondrial adaptations, increases in citrate synthase maximal activity, type Ⅱ fiber activation, adenosine monophosphate-activated protein kinase activity, and central adaptation | Positive |
| [67] | Cardiometabolic | The increased translocation of GLUT-4 to the plasma membrane and the activation of AMP-activated kinase (AMPK). Increased blood flow velocity, elevated nitric oxide (NO) level in endothelial cells, and increased nitric oxide are dependent on peripheral vascular compliance. | Positive |
| [49] | Metabolic | Glycolipid metabolism promotion. | Positive |
| [62] | Cardiometabolic | Blood pressure reduction. | Comparable |
| [33] | Metabolic | Increased oxygen uptake. | Comparable |
| [39] | Oncologic | Middle- to long-term physiological adaptation, adaptation to high physiological load, increased oxidative enzyme activities, mitochondrial biogenesis, and angiogenesis, activation of AMPK-PGC1α than CAMK-PGC1α (cell stimuli), stimulation of glycogen synthesis | Positive (but is not considered novel) |
| [42] | Cardiometabolic | Under partial Blood flow restriction occlusion, different haemodynamic and vascular responses are elicited to control the changes in blood flow and alterations in oxygen delivery | Positive |
| [88] | Cardiometabolic | Recommended 4 min at high intensity. The mechanism involves increased oxygen uptake. | Positive |
| [120] | Cardiometabolic | Increased oxygen uptake. | Comparable |
| [37] | Pain-related outcome | Muscular adaptations (mitochondrial biogenesis and increased intramuscular capillarisation), vascular adaptations (increased blood cell volume), and cardiac adaptations (increased cardiac output and contractility). | Comparable |
| [113] | Metabolic | Increase insulin sensitivity. | Not concluded |
| [125] | Metabolic | Improves functional capacity. | Comparable |
| [48] | Metabolic | Increased GLUT-4 in the plasma membrane, improved uptake of muscle glucose, and an increase in the activity of glycolytic and oxidative enzymes. | Positive |
| [32] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [112] | Cardiometabolic | The reported duration is 6–24 weeks with 2–3 sessions per week. Increased metabolic and cardiorespiratory stress. | Positive |
| [79] | Metabolic | Testosterone and cortisol increase immediately after a single HIIT session, then drop below baseline levels, and finally return to baseline values after 24 h. Genomic and non-genomic androgen action. Hypothalamic–pituitary–adrenal axis activation. | Not applicable. The study tested how HIIT increases levels of hormones. |
| [93] | Metabolic | Increased catecholamine production, leading to significant lipolysis during exercise, followed by higher post-exercise fat oxidation. | Positive |
| [63] | Cardiometabolic | Decreased resting blood pressure | Positive |
| [68] | Neurologic | Optimal periods are 12 weeks, 2 sessions a week. | Positive |
| [134] | Cardiometabolic | Improvement in anaerobic threshold. | Positive |
| [73] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [75] | Cardiometabolic | A personalized approach may lead to greater improvements in cardiorespiratory fitness. | Depends on a personalized approach |
| [70] | Cardiometabolic | Can improve pulmonary function | Positive |
| [130] | Cardiometabolic | Adaptations in muscles’ mitochondrial enzymes, improved ability to extract and use available oxygen. | Positive |
| [36] | Cardiometabolic | Improving respiratory muscle function, but not the lung function. | Positive |
| [127] | Cardiometabolic | Increased oxygen uptake. | Comparable |
| [122] | Cardiometabolic | Increased oxygen uptake. | Comparable |
| [41] | Cardiometabolic | Reduces inflammation, enhances neurogenesis via increased BDNF, improves hormonal balance by elevating monoamines and regulating the HPA axis, and decreases oxidative stress by boosting antioxidant defenses. | Positive |
| [51] | Metabolic | Increased aerobic capacity. | Positive |
| [43] | Cardiometabolic | Increase in cross-bridge cycling and Ca2+ movement, elevation of adenosine monophosphate and activation of adenosine monophosphate kinase, which boosts proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) expression, leading to enhanced mitochondrial adaptations. | Positive |
| [124] | Cardiometabolic | Improves cardiorespiratory fitness. | Comparable |
| [28] | Neurologic | Recommended up to 12 weeks duration. May increase BDNF and cardiorespiratory fitness. | Positive |
| [135] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [72] | Oncologic | Improves cardiorespiratory fitness. | Positive |
| [91] | Neurologic | Improves cerebral oxygenation, arousal, and neuroendocrine responses. | Positive |
| [74] | Cardiometabolic | Decreases insulin in combination with a ketogenic diet. | Positive |
| [53] | Cardiometabolic | Psychological changes, motivation. | Comparable |
| [29] | Metabolic | Can decrease acylated ghrelin and may suppress hunger. | Positive |
| [131] | Metabolic | Reduction in fasting glucose. | Positive |
| [99] | Cardiometabolic | Improves cardiorespiratory fitness. | Positive |
| [94] | Metabolic | Improves circulating TNF-α, leptin and adiponectin | Positive |
| [83] | Metabolic | Reduces liver fat. | Positive |
| [34] | Cardiometabolic | Increased NO bioavailability, antioxidant capacity, anti-inflammatory effects, and increased abundance of endothelial progenitor cells. | Positive |
| [50] | Metabolic | Reduces postprandial glucose. | Positive |
| [56] | Metabolic | Reduces postprandial glucose. | Comparable |
| [20] | Neurologic | Improves mood. | Positive |
| [57] | Cardiometabolic | The hydrostatic pressure in the water created by resistance in movement at high speed promotes muscle action. High speeds promote the recruitment of type II fast-twitch muscle fibers. | Positive |
| [19] | Neurologic | Brain-derived neurotrophic factor and catecholamines induced by exercise may improve cognitive performance. | Positive |
| [100] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [64] | Metabolic | No change in inflammatory biomarkers, reduction in the values of weight and abdominal fat. | Positive |
| [65] | Cardiometabolic | Improves endothelial progenitor cells function, the structure of coronary arteries, and establishes collateral circulation, thereby increasing blood flow and myocardial support. It can regulate vascular tension, improve arterial compliance, and lower the patient’s blood pressure at rest. It can control mood swings, improve negative emotions, maintain the body’s energy balance, and reduce fat accumulation. | Positive |
| [69] | Cardiometabolic | It can promote free fatty acids in the blood to enter the cells. Improves the activities of lipoprotein lipase and hepatic lipase in the muscle and liver. Can decrease leptin, tumor necrosis factor-α, and interleukin-6. Can improve the expression of the uncoupling protein-3 mRNA in the skeletal muscle and the catecholamine level to promote the metabolism level of adipose. | Positive |
| [30] | Cardiometabolic | Promotes nitric oxide production by endothelial cells. | Comparable |
| [132] | Cardiometabolic | Improves resting heart rate and oxygen uptake. | Positive |
| [119] | Cardiometabolic | Changes in hemoglobin A1c and 2 h glucose. | Positive |
| [98] | Cardiometabolic | Favors fat utilization during the recovery period. | Positive |
| [105] | Cardiometabolic | Changes in hemoglobin A1c and average glucose. | Positive |
| [59] | Cardiometabolic | Increased oxygen uptake. | Depends on a personalized approach |
| [126] | Metabolic | Reduces whole body adiposity. | Positive |
| [90] | Cardiometabolic | Improves cardiometabolic fitness | Positive |
| [97] | Cardiometabolic | Long-term and short-term HIIT are similarly effective. Improves cardiorespiratory fitness. | Positive |
| [103] | Neurologic | Improvements in anxiety and depression | Positive |
| [104] | Neurologic | Improvements in motor skills and mental health outcomes. | Positive |
| [18] | Neurologic | Moderate improvements in mental well-being. | Positive |
| [46] | Cardiometabolic | Improvement in glycemic control and insulin resistance. | Positive |
| [31] | Metabolic | Decreases blood glucose. | Inconsistent |
| [78] | Cardiometabolic | Not reported. | Positive |
| [133] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [17] | Neurologic | Small increase in slow-wave sleep (SWS) and total sleep time (TST). | Positive |
| [87] | Metabolic | Post-exercise oxy-gen consumption and fat beta-oxidation. | Positive |
| [24] | Oncologic | Not reported. | Comparable |
| [121] | Neurologic | Not reported. | Positive |
| [89] | Oncologic | Increased oxygen uptake. | Positive |
| [25] | Cardiometabolic | Total cholesterol, high-density lipoprotein, low-density lipoprotein and triglycerides blood lipid metabolism | Positive |
| [123] | Cardiometabolic | Recommended 8–12 weeks. Improved the cardiocirculatory function, stimulating the sinus node faster. | Positive |
| [92] | Cardiometabolic | Passive recovery improves performance. | Positive |
| [22] | Cardiometabolic | Not reported. | Positive |
| [80] | Cardiometabolic | Not reported. | Positive |
| [13] | Cardiometabolic | Improves cardiorespiratory fitness. | Positive |
| [107] | Cardiometabolic | Increased oxygen uptake. | Positive |
| [12] | Cardiometabolic | Lowers blood pressure and increases oxygen uptake. | Positive |
| [10] | Cardiometabolic | Effects on oxidative stress, inflammation, and insulin sensitivity. | Positive |
| [14] | Cardiometabolic | Not reported. | Positive |
| [71] | Metabolic | Enhances cardiorespiratory fitness, mitochondrial function, and fat metabolism. | Comparable |
| [26] | Cardiometabolic | Improves endothelial function. | Positive |
| [9] | Metabolic | Promotes translocation of GLUT-4 receptors inside the cell of the membrane, facilitates the diffusion of plasma glucose into striated muscle tissue and adipocytes without the need for insulin action. | Positive |
| [38] | Cardiometabolic | Not reported | Comparable |
| [44] | Cardiometabolic | Improves stretch-shortening cycles that favor recruitment of type 2 muscle fibers and thereby promote muscle hypertrophy | Comparable |
| [8] | Metabolic | Greater fat oxidation, and changes in appetite and satiety. | Positive |
| [23] | Oncologic | Not reported. | Not significant |
| [11] | Cardiometabolic | Improves total cholesterol, low-density lipoprotein cholesterol, and triglycerides levels in children. | Positive |
| [27] | Neurologic | Adaptations to increased oxygen uptake. | Comparable |
| [114] | Cardiometabolic | Improves cardiorespiratory fitness and increase in skeletal muscle mitochondrial respiration. | Comparable |
| [7] | Cardiometabolic | Improves cardiorespiratory fitness. | Comparable |
| [86] | Oncologic | Increases lower body muscle mass, endothelial function, can reduce interleukin-6 biomarker. | Positive |
| [118] | Cardiometabolic | Not reported. | Comparable |
| [95] | Oncologic | Increased oxygen uptake. | Comparable |
| [76] | Cardiometabolic | Increases stroke volume and ejection fraction of the heart induced by enhanced left ventricular systolic function, increases peroxisome proliferator-activated receptor γ-coactivator-1α (PGC-1α) and glucose transporters following, induces improved mitochondrial function. | Unclear |
| [46] | Cardiometabolic | Improves mitochondrial function at the molecular level. | Positive |
| [111] | Cardiometabolic | Decreases blood pressure. | Positive |
| [35] | Cardiometabolic | Hypoxic stimuli improve HHIT effectiveness. | Positive |
| [128] | Metabolic | Decreases whole body fat. | Comparable |
| [116] | Cardiometabolic | Not reported. | Positive |
| [11] | Cardiometabolic | Not reported. | Positive |
| [102] | Metabolic | Not reported | Comparable |
| [82] | Cardiometabolic | Improves cardiorespiratory fitness. | Positive |
| [129] | Cardiometabolic | Increases oxygen uptake. | Positive |
| [60] | Cardiometabolic | Recommends 8 weeks. Improves endothelial function. | Positive |
| [58] | Cardiometabolic | Increases cardiac pumping function and improves cardiopulmonary exchange function. | Positive |
| [55] | Cardiometabolic | Improves cardiorespiratory fitness. | Positive |
| [87] | Cardiometabolic | Improves cardiopulmonary function. | Comparable |
| [77] | Metabolic | Reduces body fat percentage. | Positive |
| [96] | Metabolic | Increased oxygen uptake. | Positive |
| [136] | Pain-related outcome | Minimum 14 weeks is recommended. Modulation of the HPA axis and increased serotonin, norepinephrine and endogenous opioid activity, enhancing pain-inhibitory pathways. | Positive |
| [137] | Oncologic | Not reported | Positive |
| [138] | Pain-related outcome | Not reported | Comparable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viderman, D.; Rakhmanov, Y.; Aubakirova, M.; Kalikanov, S.; Fredericson, M. The Impact of High-Intensity Interval Training on Cardiometabolic, Neurologic, Oncologic, and Pain-Related Outcomes: A Comprehensive Review of Systematic Reviews. J. Clin. Med. 2025, 14, 8328. https://doi.org/10.3390/jcm14238328
Viderman D, Rakhmanov Y, Aubakirova M, Kalikanov S, Fredericson M. The Impact of High-Intensity Interval Training on Cardiometabolic, Neurologic, Oncologic, and Pain-Related Outcomes: A Comprehensive Review of Systematic Reviews. Journal of Clinical Medicine. 2025; 14(23):8328. https://doi.org/10.3390/jcm14238328
Chicago/Turabian StyleViderman, Dmitriy, Yeltay Rakhmanov, Mina Aubakirova, Sultan Kalikanov, and Michael Fredericson. 2025. "The Impact of High-Intensity Interval Training on Cardiometabolic, Neurologic, Oncologic, and Pain-Related Outcomes: A Comprehensive Review of Systematic Reviews" Journal of Clinical Medicine 14, no. 23: 8328. https://doi.org/10.3390/jcm14238328
APA StyleViderman, D., Rakhmanov, Y., Aubakirova, M., Kalikanov, S., & Fredericson, M. (2025). The Impact of High-Intensity Interval Training on Cardiometabolic, Neurologic, Oncologic, and Pain-Related Outcomes: A Comprehensive Review of Systematic Reviews. Journal of Clinical Medicine, 14(23), 8328. https://doi.org/10.3390/jcm14238328





