Arthroscopic Discopexy Techniques for Articular Disc Displacement: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim and Objectives
2.2. Research Question
2.3. Eligibility Criteria and Search Strategy
2.4. Data Extraction and Management
2.5. Assessment of Research Quality
2.6. Data Synthesis and Statistical Analysis
3. Results
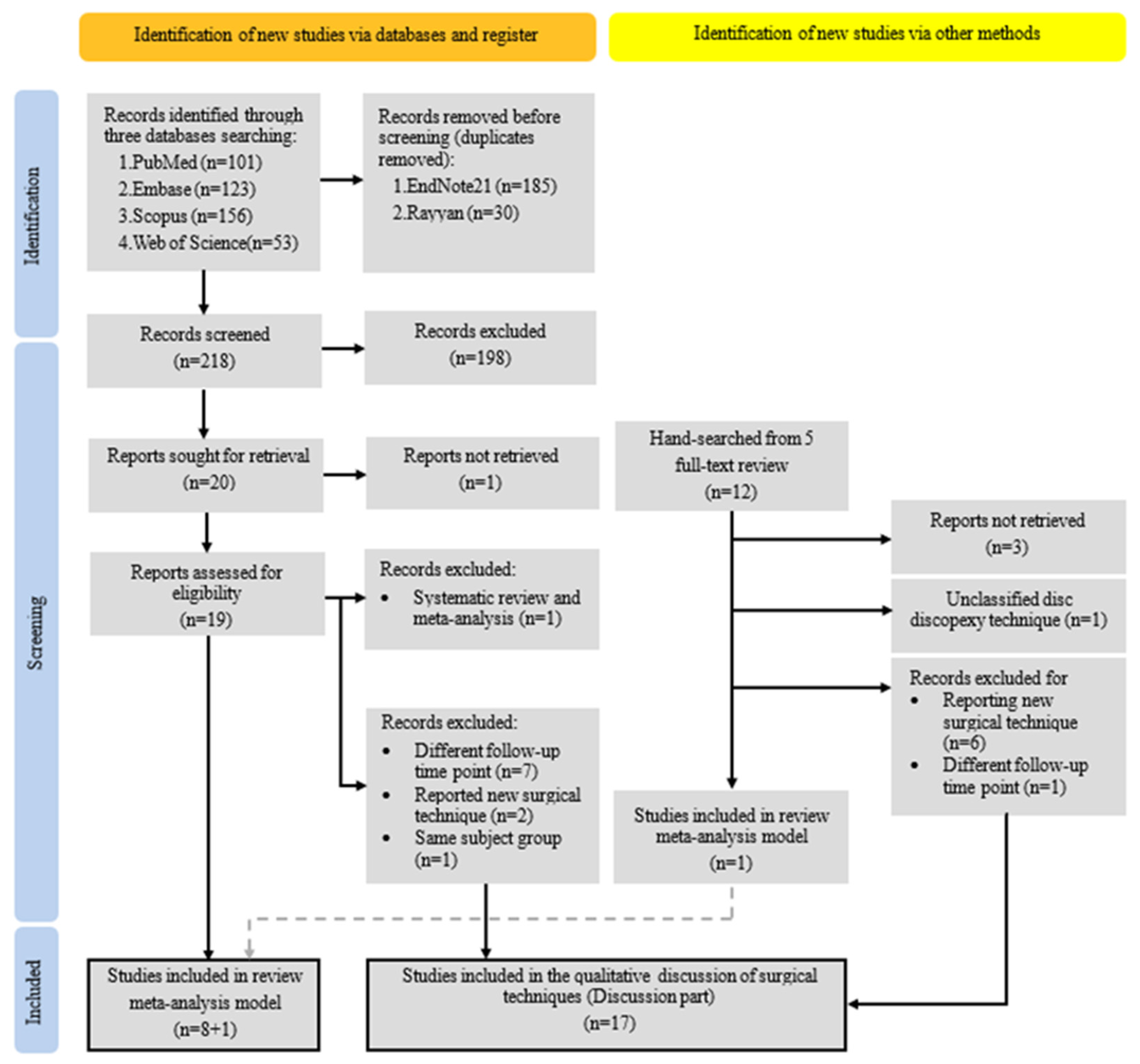
3.1. Study Selection
3.2. Characteristics and Quality of the Included Studies
3.3. Research Quality Assessment
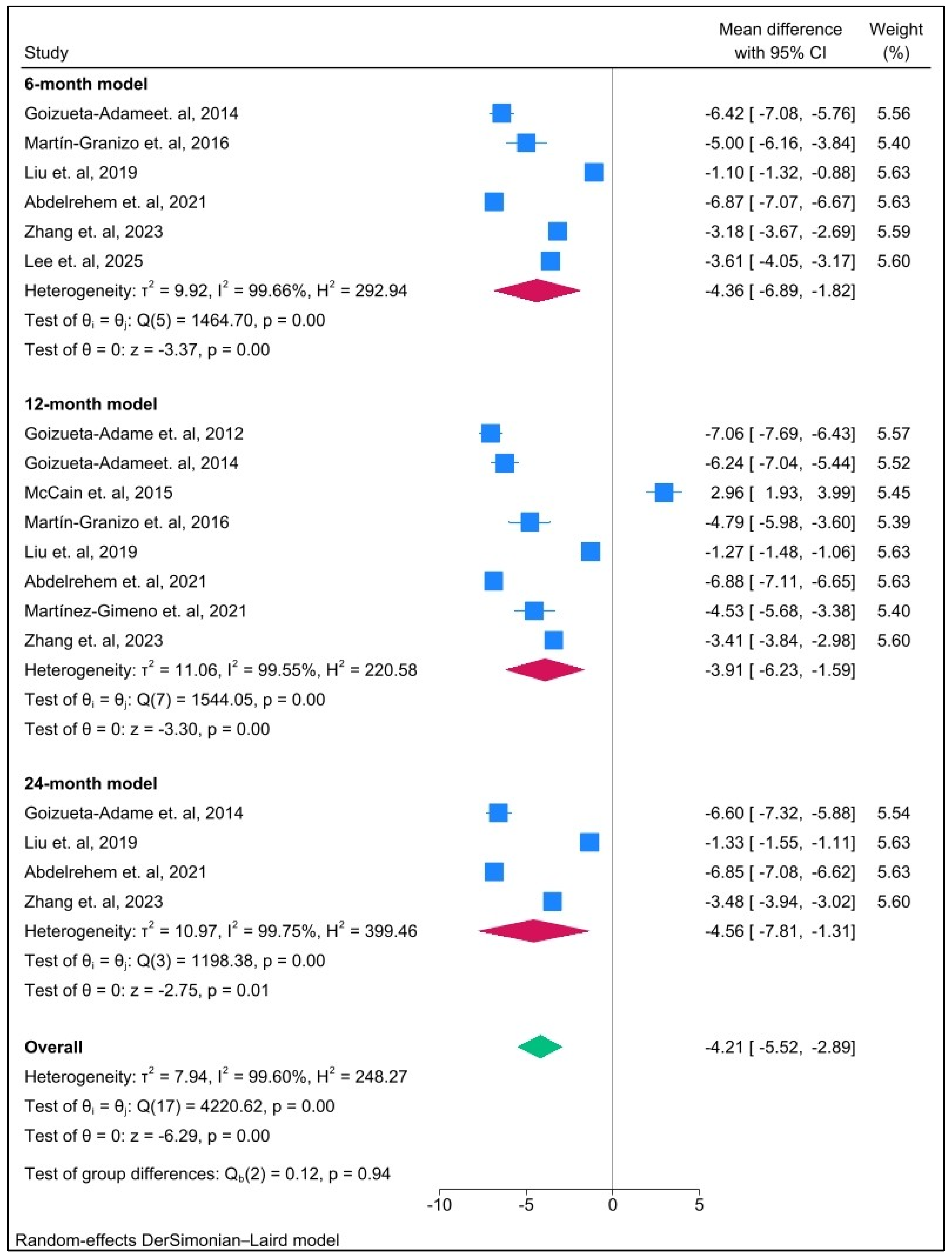
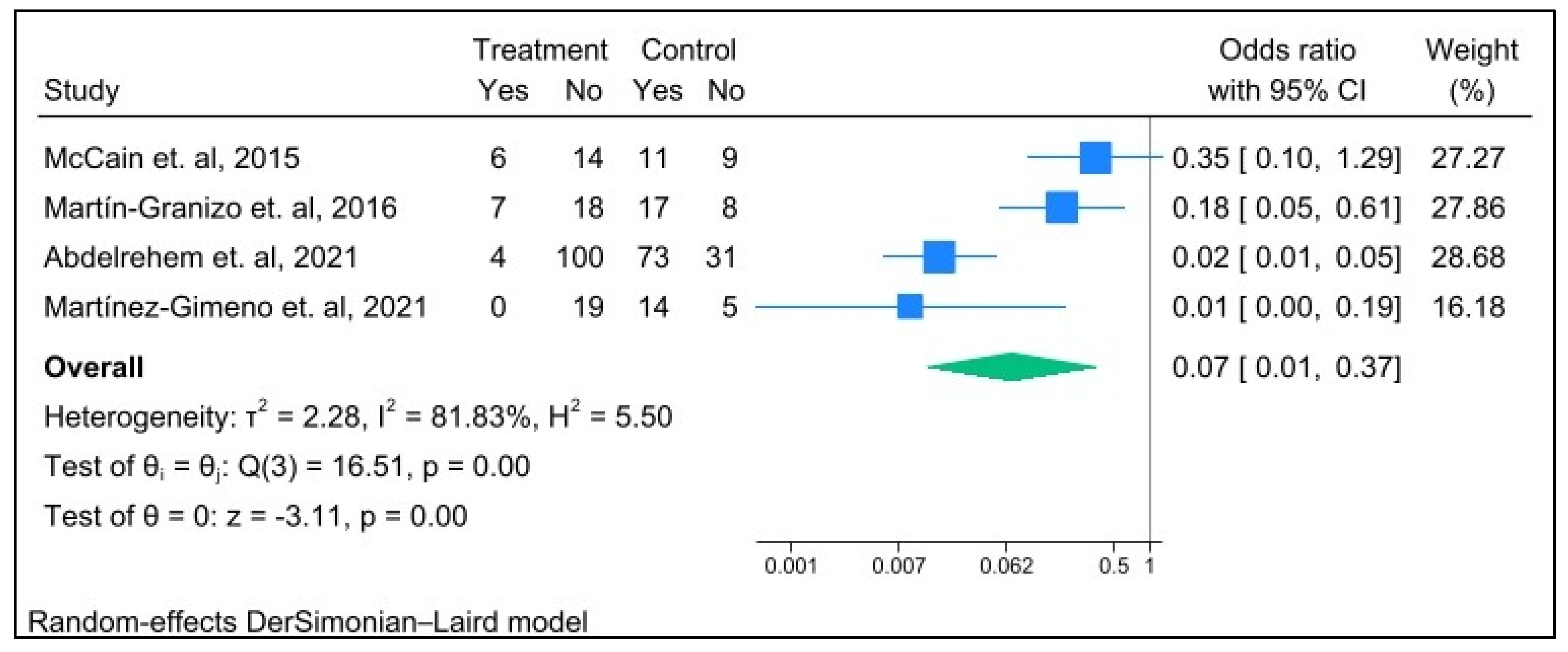
3.4. Synthesis of Results
3.5. Assessment of the Quality of Evidence
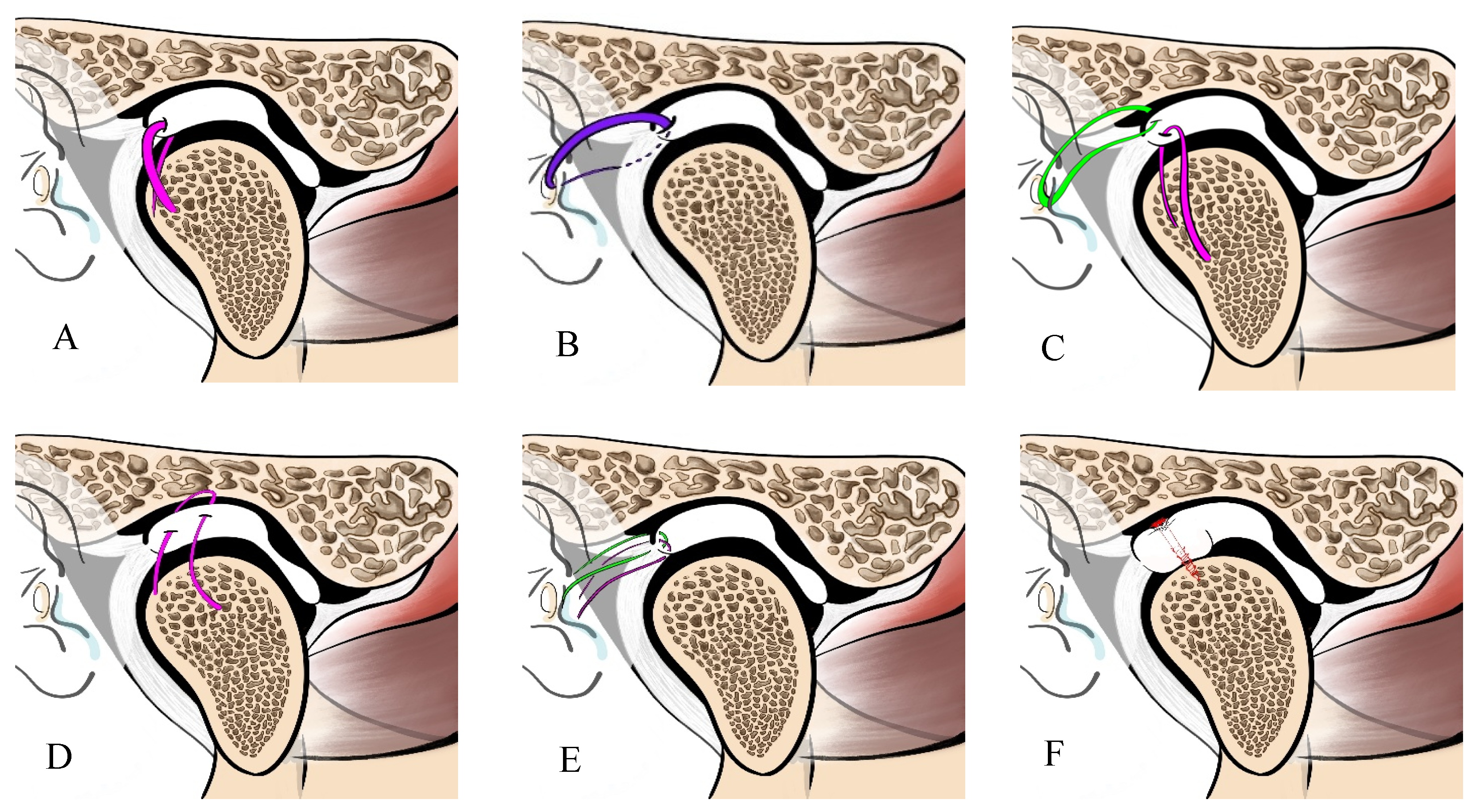
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zieliński, G.; Pająk-Zielińska, B.; Ginszt, M. A meta-analysis of the global prevalence of temporomandibular disorders. J. Clin. Med. 2024, 13, 1365. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6. [Google Scholar] [CrossRef]
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. 2013, 57, 465–479. [Google Scholar] [CrossRef]
- Wolford, L.M.; Gonçalves, J.R. Condylar resorption of the temporomandibular joint: How do we treat it? Oral Maxillofac. Surg. Clin. 2015, 27, 47–67. [Google Scholar] [CrossRef]
- Wolford, L.M.; Cardenas, L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Mercuri, L.G. Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review. J. Clin. Med. 2024, 13, 3951. [Google Scholar] [CrossRef]
- Arnett, G.; Milam, S.; Gottesman, L. Progressive mandibular retrusion—Idiopathic condylar resorption. Part I Am. J. Orthod. Dentofac. Orthop. 1996, 110, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E. Etiology and Diagnosis for Idiopathic Condylar Resorption in Growing Adolescents. J. Clin. Med. 2023, 12, 6607. [Google Scholar] [CrossRef] [PubMed]
- Nicolielo, L.; Jacobs, R.; Albdour, E.A.; Hoste, X.; Abeloos, J.; Politis, C.; Swennen, G. Is oestrogen associated with mandibular condylar resorption? A systematic review. Int. J. Oral Maxillofac. Surg. 2017, 46, 1394–1402. [Google Scholar] [CrossRef]
- Gunson, M.J.; Arnett, G.W.; Formby, B.; Falzone, C.; Mathur, R.; Alexander, C. Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: A case for low serum 17β-estradiol as a major factor in progressive condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 772–779. [Google Scholar] [CrossRef]
- Nogami, S.; Yamauchi, K.; Shimizu, Y.; Hirayama, B.; Kumasaka, A.; Iikubo, M.; Kumamoto, H.; Takahashi, T. Experimental comparison between tractional and compressive stress on temporomandibular joint. Oral Dis. 2017, 23, 644–652. [Google Scholar] [CrossRef]
- Nogami, S.; Yamauchi, K.; Odashima, K.; Ito, K.; Iikubo, M.; Kumasaka, A.; Martinez-de la Cruz, G.; Gaggl, A.; Kumamoto, H.; Takahashi, T. Influence of oestrogen deficiency and excessive mechanical stress on condylar head of mandible. Oral Dis. 2020, 26, 1718–1726. [Google Scholar] [CrossRef]
- Nogami, S.; Kajita, T.; Yanagisawa, Y.; Suzuki, H.; Takeda, Y.; Ito, K.; Kumasaka, A.; Steiner, C.; Gaggl, A.; Iikubo, M. Effects of antigen-induced arthritis and compressive mechanical stress on condylar head of mandible. J. Oral Biosci. 2025, 67, 100654. [Google Scholar] [CrossRef]
- Nogami, S.; Yamauchi, K.; Satomi, N.; Yamaguchi, Y.; Yokota, S.; Abe, Y.; Takahashi, T. Risk factors related to aggressive condylar resorption after orthognathic surgery for females: Retrospective study. Cranio 2017, 35, 250–258. [Google Scholar] [CrossRef]
- Lee, L.M.; Zhu, Y.M.; Yang, R.; Li, S.Y.; Liang, X.; Wang, Y.M. Early management of anterior disc displacement without reduction: Evaluating the effectiveness of modified arthroscopy discopexy with anterior disc repositioning splint. J. Craniomaxillofac. Surg. 2025, 53, 97–103. [Google Scholar] [CrossRef] [PubMed]
- McCain, J.P.; Hossameldin, R.H.; Srouji, S.; Maher, A. Arthroscopic discopexy is effective in managing temporomandibular joint internal derangement in patients with wilkes stage II and III. J. Oral Maxillofac. Surg. 2015, 73, 391–401. [Google Scholar] [CrossRef]
- Zhang, W.; Luo, Y.; Abdelrehem, A.; Liu, X.; Chen, M.; Yang, C.; Yu, C.; Wang, F. Arthroscopic Disk Repositioning After Failed Open Disk Repositioning. J. Craniofac. Surg. 2023, 34, e129–e134. [Google Scholar] [CrossRef]
- Ward, C.K.B.; Cheung, J.; Troost, J.P.; Aronovich, S.; Hakim, M.A. Does Postoperative Disc Position Following Double Suture Arthroscopic Discopexy Correlate with Improvements in Pain and Quality of Life? J. Oral Maxillofac. Surg. 2025, 83, 510–527. [Google Scholar] [CrossRef]
- Tang, Y.H.; van Bakelen, N.B.; Gareb, B.; Spijkervet, F.K.L. Arthroscopy versus arthrocentesis and versus conservative treatments for temporomandibular joint disorders: A systematic review with meta-analysis and trial sequential analysis. Int. J. Oral Maxillofac. Surg. 2024, 53, 503–520. [Google Scholar] [CrossRef] [PubMed]
- Hakim, M.A.; McCain, J.P.; Ahn, D.Y.; Troulis, M.J. Minimally Invasive Endoscopic Oral and Maxillofacial Surgery. Oral Maxillofac. Surg. Clin. 2019, 31, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Xu, J.; Zhang, J.; Wan, Y.; He, Y.; Lei, J.; Zhang, Y.; Yang, C.; Yang, Y. Exercise therapy in postoperative patients with temporomandibular joint internal derangement: A systematic review. J. Oral Rehabil. 2024, 51, 2158–2168. [Google Scholar] [CrossRef] [PubMed]
- Heo, H.-A.; Park, S.; Pyo, S.-W.; Yoon, H.-J. Clinical outcomes of patients with unilateral internal derangement of the temporomandibular joint following arthrocentesis and stabilization splint therapy. Maxillofac. Plast. Reconstr. Surg. 2024, 46, 24. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions of Site. Available online: https://training.cochrane.org/handbook/current/chapter-14 (accessed on 15 September 2023).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 10 November 2025).
- Schünemann, H.J.; Brennan, S.; Akl, E.A.; Hultcrantz, M.; Alonso-Coello, P.; Xia, J.; Davoli, M.; Rojas, M.X.; Meerpohl, J.J.; Flottorp, S.; et al. The development methods of official GRADE articles and requirements for claiming the use of GRADE—A statement by the GRADE guidance group. J. Clin. Epidemiol. 2023, 159, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Goizueta-Adame, C.C.; Pastor-Zuazaga, D.; Orts Bañón, J.E. Arthroscopic disc fixation to the condylar head. Use of resorbable pins for internal derangement of the temporomandibular joint (stage II–IV). Preliminary report of 34 joints. J. Craniomaxillofac. Surg. 2014, 42, 340–346. [Google Scholar] [CrossRef]
- Liu, X.; Zheng, J.; Cai, X.; Abdelrehem, A.; Yang, C. Techniques of Yang’s arthroscopic discopexy for temporomandibular joint rotational anterior disc displacement. Int. J. Oral Maxillofac. Surg. 2019, 48, 769–778. [Google Scholar] [CrossRef]
- Abdelrehem, A.; Hu, Y.K.; Yang, C.; Zheng, J.S.; Shen, P.; Shen, Q.C. Arthroscopic versus open disc repositioning and suturing techniques for the treatment of temporomandibular joint anterior disc displacement: 3-year follow-up study. Int. J. Oral Maxillofac. Surg. 2021, 50, 1351–1360. [Google Scholar] [CrossRef]
- Yang, C.; Cai, X.Y.; Chen, M.J.; Zhang, S.Y. New arthroscopic disc repositioning and suturing technique for treating an anteriorly displaced disc of the temporomandibular joint: Part I—Technique introduction. Int. J. Oral Maxillofac. Surg. 2012, 41, 1058–1063. [Google Scholar] [CrossRef]
- Goizueta-Adame, C.C.; Muñoz-Guerra, M.F. The posterior double pass suture in repositioning of the temporomandibular disc during arthroscopic surgery: A report of 16 cases. J. Craniomaxillofac. Surg. 2012, 40, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Martín-Granizo, R.; Millón-Cruz, A. Discopexy using resorbable pins in temporomandibular joint arthroscopy: Clinical and magnetic resonance imaging medium-term results. J. Craniomaxillofac. Surg. 2016, 44, 479–486. [Google Scholar] [CrossRef]
- Martínez-Gimeno, C.; García-Hernández, A.; Martínez-Martínez, R. Single portal arthroscopic temporomandibular joint discopexy: Technique and results. J. Craniomaxillofac. Surg. 2021, 49, 171–176. [Google Scholar] [CrossRef]
- Israel, H.A. Technique for placement of a discal traction suture during temporomandibular joint arthroscopy. J. Oral Maxillofac. Surg. 1989, 47, 311–313. [Google Scholar] [CrossRef]
- Tarro, A.W. Arthroscopic treatment of anterior disc displacement: A preliminary report. J. Oral Maxillofac. Surg. 1989, 47, 353–358. [Google Scholar] [CrossRef] [PubMed]
- McCain, J.P.; Podrasky, A.E.; Zabiegalski, N.A. Arthroscopic disc repositioning and suturing: A preliminary report. J. Oral Maxillofac. Surg. 1992, 50, 568–579; discussion 579–580. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Huang, D.; Liu, X.; Yang, C.; Undt, G.; Haddad, S.M.; Chen, Z. Arthroscopic treatment for intra-articular adhesions of the temporomandibular joint. J. Oral Maxillofac. Surg. 2011, 69, 2120–2127. [Google Scholar] [CrossRef]
- McNamara, D.C.; Rosenberg, I.; Jackson, P.A.; Hogben, J. Efficacy of arthroscopic surgery and midlaser treatments for chronic temporomandibular joint articular disc derangement following motor vehicle accident. Aust. Dent. J. 1996, 41, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Rosenbrg, I.; Goss, A. A modified technique of temporomandibular joint arthroscopic operative surgery of the superior and inferior joint spaces. J. Maxillofac. Oral Surg. 2020, 19, 561–570. [Google Scholar] [CrossRef]
- Del Santo, L.; Macedo, D.V.; de Souza, C.; Monje Gil, F. Arthroscopic Disc Suturing and Repositioning Technique for Treating Anteriorly Displaced Disc in Temporomandibular Joint Disorders: A Posterior Anchorage Technique. J. Oral Maxillofac. Surg. 2023, 81, 698–707. [Google Scholar] [CrossRef]
- Zhang, S.Y.; Liu, X.M.; Yang, C.; Cai, X.Y.; Chen, M.J.; Haddad, M.S.; Yun, B.; Chen, Z.Z. New arthroscopic disc repositioning and suturing technique for treating internal derangement of the temporomandibular joint: Part II—Magnetic resonance imaging evaluation. J. Oral Maxillofac. Surg. 2010, 68, 1813–1817. [Google Scholar] [CrossRef]
- Wang, B.L.; Yang, C.; Cai, X.Y.; Chen, M.J.; Zhang, S.Y.; Fang, B.; Yun, B. Malocclusion as a common occurrence in temporomandibular joint arthroscopic disc repositioning: Outcomes at 49 days after surgery. J. Oral Maxillofac. Surg. 2011, 69, 1587–1593. [Google Scholar] [CrossRef]
- Jerez, D.; Laissle, G.; Fuenzalida, C.; Uribe, S. Modification to Yang’s arthroscopic discopexy technique for temporomandibular joint disc displacement: A technical note. J. Oral Maxillofac. Surg. 2022, 80, 989–995. [Google Scholar] [CrossRef]
- de Barros, R.C.M.; Ono, H.Y. Simultaneous arthroscopy of upper and lower compartments of the temporomandibular joint. Int. J. Oral Maxillofac. Surg. 2025, 54, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Lei, J.; Fu, K.; Zhang, Y.; He, Y. Modified arthroscopic disc repositioning and suturing technique for the treatment of TMJ anterior disc displacement without reduction: A technical note. J. Craniomaxillofac. Surg. 2025, 53, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Martín-Granizo, R.; González-García, R. Arthroscopic Disc Repositioning Techniques of the Temporomandibular Joint Part 2: Resorbable Pins. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2022, 30, 185–191. [Google Scholar] [CrossRef]
- Millón-Cruz, A.; Martín-Granizo López, R. Long-term clinical outcomes of arthroscopic discopexy with resorbable pins. J. Craniomaxillofac. Surg. 2020, 48, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- González-García, R.; Rodríguez-Campo, F.J.; Monje, F.; Sastre-Pérez, J.; Gil-Díez Usandizaga, J.L. Operative versus simple arthroscopic surgery for chronic closed lock of the temporomandibular joint: A clinical study of 344 arthroscopic procedures. Int. J. Oral Maxillofac. Surg. 2008, 37, 790–796. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Sanz, D.; Cardoso, H.J. Bilateral arthroscopy of the temporomandibular joint: Clinical outcomes and the role of a second intervention—A prospective study. Clin. Oral Investig. 2023, 27, 6167–6176. [Google Scholar] [CrossRef]
- McCain, J.; Menis, M. Puncture Techniques and Arthroscopic Anatomy. Principles and Practice of Temporomandibular Joint Arthroscopy; Mosby: St. Louis, MO, USA, 1996; p. 128. [Google Scholar]
- McCain, J.P.; Hossameldin, R.H. Advanced arthroscopy of the temporomandibular joint. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2011, 19, 145–167. [Google Scholar] [CrossRef]
- McCain, J.P.; Sanders, B.; Koslin, M.G.; Quinn, J.H.; Peters, P.B.; Indresano, A.T. Temporomandibular joint arthroscopy: A 6-year multicenter retrospective study of 4831 joints. J. Oral Maxillofac. Surg. 1992, 50, 926–930. [Google Scholar] [CrossRef]
- Carls, F.; Engelke, W.; Locher, M.; Sailer, H. Complications following arthroscopy of the temporomandibular joint: Analysis covering a 10-year period (451 arthroscopies). J. Craniomaxillofac. Surg. 1996, 24, 12–15. [Google Scholar] [CrossRef]
- Jerez-Frederick, D.; Albers, D.; Fuenzalida, C.; Laissle, G.; Ávila-Oliver, C. Is the Complexity of Arthroscopic Temporomandibular Joint Surgery Associated with Short-Term Complication Rates? J. Oral Maxillofac. Surg. 2025, 83, 270–278. [Google Scholar] [CrossRef] [PubMed]
- González, L.V.; López, J.P.; Díaz-Báez, D.; López, R.M.-G. Intraoperative complications in temporomandibular joint arthroscopy: A retrospective observational analysis of 899 arthroscopies. J. Craniomaxillofac. Surg. 2022, 50, 651–656. [Google Scholar] [CrossRef]
- Laskin, D.M. Arthroscopy Versus Arthrocentesis for Treating Internal Derangements of the Temporomandibular Joint. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 325–328. [Google Scholar] [CrossRef]
- Rodhen, R.M.; de Holanda, T.A.; Barbon, F.J.; de Oliveira da Rosa, W.L.; Boscato, N. Invasive surgical procedures for the management of internal derangement of the temporomandibular joint: A systematic review and meta-analysis regarding the effects on pain and jaw mobility. Clin. Oral Investig. 2022, 26, 3429–3446. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, X.; Yang, X.; Yang, C.; Chen, M.; Haddad, M.S.; Chen, Z. Temporomandibular joint disc repositioning using bone anchors: An immediate post surgical evaluation by Magnetic Resonance Imaging. BMC Musculoskelet. Disord. 2010, 11, 262. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]

| PICO Question | Search Terms | |
|---|---|---|
| P | Patients diagnosed with temporomandibular joint disorders, specifically articular disc displacement (with or without reduction, with or without limited mouth opening) | (“Temporomandibular Joint Disorders”[Mesh] OR “Temporomandibular Disorders”[tiab] OR TMD [tiab]) AND (“Temporomandibular Joint Disc Displacement”[Mesh] OR “disc displacement”[tiab] OR “disk displacement”[tiab] OR “anterior disc displacement”[tiab] OR “internal derangement”[tiab]) |
| I | Arthroscopic disc repositioning and anchor fixation techniques (Suturing, pin, or screw) | (“Open Surgical Procedures”[Mesh] OR “open surgery”[tiab] OR “open reduction”[tiab] OR “open joint surgery”[tiab] OR “Arthroscopy”[Mesh] OR arthroscopy[tiab]) |
| C | Pre-surgical baseline values (VAS, MIO, Joint sounds) compared with post-surgical outcomes (before–after comparison) | |
| O | Pain score by VAS (score 1–10) Maximal interincisal opening (MIO) (mm) Joint sounds (clicking, popping, or crepitation) (Present/Absent) | (“Complications”[Mesh] OR “postoperative complications”[Mesh] OR complication[tiab] OR complications[tiab] OR “adverse event”[tiab] OR “adverse events”[tiab] OR “adverse effects”[tiab] OR “surgical outcome”[tiab] OR outcome[tiab] OR outcomes[tiab] OR sequelae[tiab] OR morbidity[tiab] OR “treatment failure”[tiab]) |
| S | Clinical studies (prospective or retrospective cohort study, case series and randomized controlled trials) | |
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Language | English | Non-English |
| Study design | Full-text peer-reviewed clinical studies (RCTs, cohort studies, case series) | Reviews, meta-analyses, abstracts, posters, protocols, books |
| Population | Patients diagnosed with TMJ disc displacement (with or without reduction) | Animal, cadaveric |
| Type of operation | Arthroscopic disc repositioning with anchor fixation (suture/pin/screw), or Disc discopexy technique | Other surgical procedures |
| Surgical site | Temporomandibular joint | Other areas |
| Outcomes | Reported at least one clinical outcome (Pain score by VAS, MIO, joint sounds) | Studies without relevant clinical outcomes |
| Timeframe | Studies published up through 1 September 2025 | Studies published after the cut-off date |
| First Author, Year | Study Design | Patients/ TMJ (n) | Gender (M, F) | Age Range (y), Mean (SD) | Diagnosis | Arthroscopic Discopexy Technique | Resorbable Suture Material | Location or Material of Anchorage | Additional Surgical Procedure and Postoperative Management |
|---|---|---|---|---|---|---|---|---|---|
| Goizueta- Adame et al., 2014 [28] | CS | 27/34 | M1, F26 | 17–45, 31.2 ±NM | ADDwR (n = 3) ADDwoR (n = 27) ADDwoR with bone surface change (n = 4) | An arthroscopic disc repositioning using resorbable pin | Not used | Resorbable pin at the lateral surface of the convexity of the condyle (Two pins 33 joints, single pin 1 joints (because small perforation was found)) (SmartNail®; PLA) | 1. Capsulotomy-myotomy 2. Disc reduction 3. Infiltration with sodium hyaluronate Post-operative management: 1. Medication (lornoxicam, ±muscle relaxant) 2. Functional rehabilitation 3. Soft diet 4. Mouth opening and lateral excursion were not forced for 3 months 5. Occlusal splint |
| Liu et al., 2019 [29] | RS | 532/ 749 | M147, F385 | 13–63, 21.23 ±3.53 | Rotational ADD Anterolateral (n = 408) Anteromedial (n = 341) | Modified Yang’s discopexy: double horizontal mattress–like suturing | No (Polyester) | Tragus cartilage (Suture knot) | 1. The anterior attachment release 2. Disc reduction Post-operative management: 1. Medication (Antibiotics and NSAID) 2. Soft diet for 3 days 3. Mouth opening exercise start after operation 1 week 4. A functional appliance (in transient postoperative malocclusion) |
| Abdelrehem et al., 2021 [30] | PS | 104/ 130 | M22, F82 | 16–57, 27.47 ±9.65 | ADDwR (n = 23) ADDwoR (n = 107) | Yang’s discopexy: double horizontal mattress–like suturing (Yang et al., 2012 [31]) | No | The anterior wall of the external auditory canal (Suture knot) | 1. The anterior attachment release 2. Disc reduction Post-operative management: NM |
| Zhang et al., 2023 [17] | RS | 24/27 | M2, F22 | NM, 24.38 ±8.04 | Relapsed ADD | The redo arthroscopic disc repositioning and suturing (Single suture discopexy technique at bilaminar zone and posterior band of the disc) | NM | External auditory canal cartilage (Suture knot) | 1. The anterior attachment release 2. Disc reduction Post-operative management: 1. Medication (Antibiotics and NSAID for three days) 2. Mouth opening exercise was started after operation 1 week (vertical and lateral step by step for 3–6 months) 3. Stabilizing soft splint for 6 months 4. Orthodontic treatment (if needed) |
| Lee et al., 2025 [15] | CS | 31/31 | M2, F29 | 16–45, 26.35 ±7.26 | ADDwoR (Wilkes Classification III-IV) | Posterior double-pass suture technique | No (2/0-Ti-Cron™ polyester) | Subcutaneous tissue (Suture knot) | 1. The anterior attachment release 2. Disc reduction Post-operative management: 1. Anterior disc repositioning splint 2. Mouth opening training (for 2–3 months after operation 2 days) |
| Goizueta- Adame et al., 2012 [32] | CS | 16/21 | M1, F15 | 17–49, 32 ±8.00 | ADDwR (n = 1) ADDwoR (n = 12) ADDwoR + OA (n = 3) | Posterior double-pass suture technique | Yes (2/0-PDS) | Subcutaneous tissue (Suture knot) | 1. Removed adhesion 2. Capsulotomy with anterior myotomy 3. Disc reduction Post-operative management: 1. Medication (Piroxicam, Omeprazole, and Metamizol) 2. Functional rehabilitation 3. Soft diet for at least two months |
| McCain et al., 2015 [16] | PS | 32/42 (s:20 /29) | M4, F28 (s: M2, F18) | Success group: NM, 27.36 ±12.5 | Wilkes Classification II-V | Single suture discopexy technique | Yes (0-PDS) | Lateral capsule and Subcutaneous tissue (Suture knot) | 1. The anterior attachment release and lavage 2. Complete pterygoid myotomy 3. Retrodiscal contracture or scarification 4. Disc reduction Post-operative management: NM |
| Martín- Granizo et al., 2016 [33] | CS | 26/34 | NM | 22–65, 41.5 ±NM | ADDwoR (Wilkes Classification III) | An arthroscopic disc repositioning using resorbable pin | Not used | Resorbable pin (SmartNail®; PLA) (Two pins 13 joints, single pin 21 joints) | 1. The anterior attachment release and lavage 2. Partial pterygoid myotomy 3. Disc reduction Post-operative management: 1. Medication (NSAID) 2. Soft diet for at least one month 3. Active physiotherapy during first month (3 sections per day) 4. Splint therapy |
| Martínez- Gimeno et al., 2021 [34] | RS | 19/21 | M1, F18 | 22–58, 36.84 ±11.16 | ADDwR (n = 16) ADDwoR (n = 5) | Single suture discopexy with single-port arthroscope | No (3/0-nylon) | Tragus cartilage (in Antero-posterior direction) | 1. Removed intraarticular adhesion (if necessary) 2. No Capsulotomy or anterior myotomy 3. Disc reduction Post-operative management: 1. Medication (Metamizole and Diclofenac) 2. Soft diet and limited mouth opening for one week after operation, then normal diet and mouth opening exercise |
| First Author, Year | MIO (mm) (Mean ± SD) | VAS (0–10) (Mean ± SD) | Joint Sounds (n) Present (P)-Absent (A) Case (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-surgery | Post-surgery | n | Pre-surgery | Post-surgery | n | Pre-surgery | Post-surgery | n | |
| Follow-up post-surgery 6-month model (Short-term) | |||||||||
| Goizueta-Adame et al., 2014 [28] ▲▲▲▲ | 34.3 ± 5.2 n = 34(NM) | 38.4 ± 5.5 n = 29(NM) | - | 7.08 ± 1.65 n = 32(NM) | 0.66 ± 0.92 n = 29(NM) | - | P: 12 (35.3%) A: 22 (64.7%) | P: NM A: NM | 34 (patients) |
| Martín-Granizo et al., 2016 [33] *** | 32.04 ± 7.54 | 38.14 ± 4.61 | 26 (patients) | 6.58 ± 2.45 | 1.58 ± 1.75 | 26 (patients) | NM | NM | NM |
| Liu et al., 2019 [29] | 26.65 ± 7.87 | 32.68 ± 6.37 | 532 (patients) | 2.06 ± 2.13 | 0.96 ± 1.56 | 532 (patients) | NM | NM | NM |
| Abdelrehem et al., 2021 [30] ▲▲▲▲ | 17.08 ± 2.90 | 35.61 ± 2.22 | 104 (patients) | 7.05 ± 1.12 | 0.18 ± 0.38 | 130 (joints) | P: 73 (70.2%) A: 31 (29.8%) | P: 1 (1.00%) A: 103 (99.00%) | 104 (patients) |
| Zhang et al., 2023 [17] ** | 25.07 ± 9.73 | 37.37 ± 6.67 | 24 (patients) | 4.11 ± 0.85 | 0.93 ± 0.87 | 24 (patients) | NM | NM | NM |
| Lee et al., 2025 [15] | 23.13 ± 3.54 | 39.35 ± 2.50 | 31 (patients) | 4.77 ± 0.96 | 1.16 ± 0.79 | 31 (patients) | NM | NM | NM |
| Follow-up post-surgery 12-month model (Mid-term) | |||||||||
| Goizueta-Adame et al., 2012 [32] | 31.13 ± 4.63 | 39.88 ± 2.61 | 16 (patients) | 7.08 ± 1.65 n = 32(NM) | 1.00 ± 0.96 | 16 (patients) | NM | NM | NM |
| Goizueta-Adame et al., 2014 [28] ▲▲▲▲ | 34.3 ± 5.2 n = 34(NM) | 43.2 ± 6.1 n = 29(NM) | - | 7.08 ± 1.65 n = 32(NM) | 0.84 ± 1.54 n = 29(NM) | - | P: 12 (35.3%) A: 22 (64.7%) | P: NM A: NM | 34 (patients) |
| McCain et al., 2015 [16] *, ▲▲▲ | 30 ± 8 | 37.9 ± 3.8 | 20 (patients) | 4.19 ± 1.44 | 7.15 ± 1.87 | 20 (patients) | P: 11 (61%) A: 9 (49%) | P: 6 (46%) A: 14 (54%) | 20 (patients) |
| Martín-Granizo et al., 2016 [33] ***, ▲ | 32.04 ± 7.54 | 39.57 ± 4.54 | 26 (patients) | 6.58 ± 2.45 | 1.79 ± 1.88 | 26 (patients) | P: 17 (65%) A: 8 (35%) | P: 7 (29%) A: 18 (71%) | 25 (patients) |
| Liu et al.,2019 [29] | 26.65 ± 7.87 | 34.02 ± 6.12 | 532 (patients) | 2.06 ± 2.13 | 0.79 ± 1.24 | 532 (patients) | NM | NM | NM |
| Abdelrehem et al., 2021 [30] ▲▲▲▲ | 17.08 ± 2.90 | 37.20 ± 1.63 | 104 (patients) | 7.05 ± 1.12 | 0.17 ± 0.76 | 130 (joints) | P: 73 (70.2%) A: 31 (29.8%) | P: 4 (3.80%) A: 100 (96.20%) | 104 (patients) |
| Martínez-Gimeno et al., 2021 [34] **, ▲▲ | 36.21 ± 8.09 | 39.58 ± 4.35 | 19 (patients) | 5.53 ± 1.93 | 1.00 ± 1.67 | 19 (patients) | P: 14 (73%) A: 5 (27%) | P: 0 (0%) A: 19 (100%) | 19 (patients) |
| Zhang et al., 2023 [17] ** | 25.07 ± 9.73 | 39.43 ± 7.23 | 24 (patients) | 4.11 ± 0.85 | 0.70 ± 0.67 | 24 (patients) | NM | NM | NM |
| Follow-up post-surgery 24-month model (Long-term) | |||||||||
| Goizueta-Adame et al., 2014 [28] ▲▲▲▲ | 34.3 ± 5.2 n = 34(NM) | 43.9 ± 4.8 n = 12(NM) | - | 7.08 ± 1.65 n = 32(NM) | 0.48 ± 0.76 n = 12(NM) | - | P: 12 (35.3%) A: 22 (64.7%) | P: NM A: NM | 34 (patients) |
| Liu et al., 2019 [29] | 26.65 ± 7.87 | 34.73 ± 6.28 | 532 (patients) | 2.06 ± 2.13 | 0.73 ± 1.43 | 532 (patients) | NM | NM | NM |
| Abdelrehem et al., 2021 [30] ▲▲▲▲ | 17.08 ± 2.90 | 38.18 ± 1.21 | 104 (patients) | 7.05 ± 1.12 | 0.20 ± 0.78 | 130 (joints) | P: 73 (70.2%) A: 31 (29.8%) | P: 0 (0%) A: 104 (100%) | 104 (patients) |
| Zhang et al., 2023 [17] ** | 25.07 ± 9.73 | 38.44 ± 7.08 | 24 (patients) | 4.11 ± 0.85 | 0.63 ± 0.79 | 24 (patients) | NM | NM | NM |
| First Author, Year | Arthroscopic Discopexy Technique | Anchorage | Included Model or Excluded Result |
|---|---|---|---|
| Israel, H. A., 1989 [35] | Single suture discopexy technique (at posterior lateral corner of the disc-condyle) | Lateral capsule and Subcutaneous tissue (non-resorbable suture). Disc position maintained by retrodiscal scarring after stitch removal (1–2 weeks) | Reported new surgical technique |
| Tarro et al., 1989 [36] | Lateral capsule and Subcutaneous tissue (Resorbable surgical knot) (holding the disc in a posterior lateral position) | Different follow-up time points (post-operation, 3–12 months) | |
| McCain et al., 1992 [37] | Reported new surgical technique | ||
| Zhang et al., 2011 [38] | Different follow-up time points (post-operation = 10.3 months) | ||
| McCain et al., 2015 [16] | Included in 12-month model | ||
| McNamara et al., 1996 [39] | Cartilaginous part of the external auditory canal (endaural plication) using a non-resorbable suture; the surgical stitch was removed 2 weeks after the operation | Different follow-up time points (post-operation 3 months and 3 years) | |
| Martínez-Gimeno et al., 2021 [34] | Single suture discopexy at the posterolateral disc-condyle corner using a single-port arthroscope (irrigation, visualization, and laser in one working cannula) | Tragal cartilage (anteroposterior direction); non-resorbable surgical knot; stitch removed 2 weeks postoperatively | Included in 12-month model |
| Rosenbrg and Goss, 2020 [40] | Single suture discopexy technique (at bilaminar zone or retrodiscal zone) | External auditory canal cartilage (non-resorbable suture) (endaural approach); stitch removed 2 weeks postoperatively | Reported new surgical technique |
| Zhang et al., 2023 [17] | The redo arthroscopic disc repositioning and suturing (Single suture discopexy technique at bilaminar zone and posterior band of the disc) | External auditory canal cartilage (Suture knot) | Included in 6-month, 12-month, and 24-month model |
| Ward et al., 2025 [18] | Double-suture arthroscopic discopexy (modified from the single-suture discopexy technique) | Posterolateral aspect of the articular disc anchored to the TMJ fibrous capsule, and the posteromedial aspect anchored to the tragal cartilage (resorbable surgical knot) | Different follow-up time points (post-operation = 9 months) |
| Goizueta-Adame et al., 2012 [32] | Posterior double-pass suture technique, with the needle penetrating the disc from lateral to medial in the posterior zone | Subcutaneous tissue (Resorbable surgical knot) | Included in 12-month model |
| Lee et al., 2025 [15] | Subcutaneous tissue (non-resorbable surgical knot) | Included in 6-month model | |
| Del Santo et al., 2023 [41] | Tragus cartilage (resorbable surgical knot) | Reported new surgical technique | |
| Zhang et al., 2010 [42] | An arthroscopic double horizontal mattress–like suturing technique performed through 3 punctures (triangulation technique) for pure ADD (Yang’s technique) | The anterior wall of the external auditory canal (non-resorbable surgical knot) | Different follow-up time points (post-operation 1–7 days) |
| Wang et al., 2011 [43] | Different follow-up time points (post-operation, 49 days) | ||
| Yang et al., 2012 [31] | Reported new surgical technique | ||
| Abdelrehem et al., 2021 [30] | Included in 6-month, 12-month, and 24-month model | ||
| Jerez et al., 2022 [44] | Modified Yang technique (Yang et al., 2012 [31]): five punctures; the suture passes from the posterior border of the bilaminar zone and the posterior band of the disc to the medial retrodiscal tissue in the upper joint space | The anterior wall of the external auditory canal (resorbable or non-resorbable surgical knot) | Reported new surgical technique |
| de Barros and Ono, 2025 [45] | Modified Yang technique (Yang et al., 2012 [31]): arthroscopic access to both upper and lower compartments | The retrotragal cartilage | Reported new surgical technique |
| Liu et al., 2019 [29] | Modified Yang’s discopexy: double horizontal mattress–like suturing (6 punctures) for pure ADD/rotational DD; complex technique | Tragus cartilage (Suture knot) | Included in 6-month, 12-month, and 24-month model |
| Dong et al., 2025 [46] | Modified Yang’s technique: double horizontal mattress–like suturing (5 punctures) for pure ADD modified from Yang et al. (2012) [31] and Liu et al. (2019) [29] | External auditory canal cartilage (non-resorbable surgical knot) | Different follow-up time points (post-operation, 1 and 3 months) |
| Goizueta-Adame et al., 2014 [28] | An arthroscopic disc repositioning using resorbable pin | Resorbable pin at the lateral surface of the convexity of the condyle (SmartNail®; PLA) | Included in 6-month, 12-month, and 24-month model |
| Martín-Granizo et al., 2016 [33] | Resorbable pin at postero-lateral corner of the disc (SmartNail®; PLA) | Included in 6-month and 12-month model | |
| Martín-Granizo et al., 2022 [47] | Reported new surgical technique | ||
| Millón-Cruz et al., 2020 [48] | Same subject group with Martín-Granizo et al., 2016 [33] | ||
| González-García et al., 2008 [49] | Unclear surgical technique | Unclassified disc discopexy technique | |
| Ângelo et al., 2023 [50] | Unclear surgical technique | Different follow-up time point (post-operation = 523.7 days) | |
| McCain et al., 1992 [37] | - | - | Reports not retrieved |
| McCain and Menis, 1996 [51] | - | - | Reports not retrieved |
| McCain and Hossameldin, 2011 [52] | - | - | Reports not retrieved |
| Tang et al., 2024 [19] | - | - | Systematic review and meta-analysis of Open Discopexy with suture Anchors |
| First Author, Year | NHLBI Quality Assessment Tool for Before-After (Pre-Post) Study with No Control Group | Quality (Overall Judgement) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | ||
| Liu et al., 2019 [29] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | NA | Good (10) |
| Abdelrehem et al., 2021 [30] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | NA | Good (10) |
| Zhang et al., 2023 [17] | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | Yes | Yes | NA | Good (9) |
| McCain et al., 2015 [16] | Yes | Yes | No | No | NR | Yes | Yes | No | NR | No | No | NA | Poor (4) |
| Martínez-Gimeno et al., 2021 [34] | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | Yes | Yes | NA | Good (9) |
| First Author, Year | NHLBI Quality Assessment Tool for Case Series Studies | Quality (Overall Judgement) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | ||
| Goizueta-Adame et al., 2012 [32] | Yes | Yes | NR | Yes | Yes | Yes | Yes | Yes | Yes | Good (8) |
| Goizueta-Adame et al., 2014 [28] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Good (8) |
| Lee et al., 2025 [15] | Yes | Yes | NR | Yes | Yes | Yes | Yes | Yes | Yes | Good (8) |
| Martín-Granizo et al., 2016 [33] | Yes | Yes | NR | Yes | Yes | Yes | Yes | Yes | Yes | Good (8) |
| Certainty Domain | Justification | Downgrade/Upgrade | Estimation |
|---|---|---|---|
| Start | Observational studies (cohort and case series) | - | Low (⊕⊕◯◯) |
| Downgrade estimation | |||
| Risk of Bias | Uncontrolled confounding, lack of blinding | Downgraded 1 level | very low (⊕◯◯◯) |
| Inconsistency | Although heterogeneity was high, the direction of effect was consistent across studies | No downgrade | very low (⊕◯◯◯) |
| Indirectness | Population, intervention, comparator, and outcomes directly addressed the review question | No downgrade | very low (⊕◯◯◯) |
| Imprecision | 95% CI do not cross the line of no effect; however, intervals were wide in several analyses | No downgrade | very low (⊕◯◯◯) |
| Publication bias | Not assessed | No downgrade | very low (⊕◯◯◯) |
| Overall (after downgrades): Very low (⊕◯◯◯) | |||
| Upgrade estimation | |||
| Large Effect | Large effect size | Upgraded 1 level | low (⊕⊕◯◯) |
| Dose–response | Not observed | No upgrade | low (⊕⊕◯◯) |
| Residual confounding toward the null | Not observed | No upgrade | low (⊕⊕◯◯) |
| Final certainty rating: Low (⊕⊕◯◯) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nogami, S.; Jewrasumnuay, P.; Yamauchi, K. Arthroscopic Discopexy Techniques for Articular Disc Displacement: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 8046. https://doi.org/10.3390/jcm14228046
Nogami S, Jewrasumnuay P, Yamauchi K. Arthroscopic Discopexy Techniques for Articular Disc Displacement: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(22):8046. https://doi.org/10.3390/jcm14228046
Chicago/Turabian StyleNogami, Shinnosuke, Phasathorn Jewrasumnuay, and Kensuke Yamauchi. 2025. "Arthroscopic Discopexy Techniques for Articular Disc Displacement: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 22: 8046. https://doi.org/10.3390/jcm14228046
APA StyleNogami, S., Jewrasumnuay, P., & Yamauchi, K. (2025). Arthroscopic Discopexy Techniques for Articular Disc Displacement: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(22), 8046. https://doi.org/10.3390/jcm14228046







