Longitudinal Skeletal and Dental Changes in Untreated Children with Angle Class I and III Malocclusions: A Retrospective Cephalometric Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Cephalometric Measurements
2.3. Sample Size Calculation
2.4. Statistics
3. Results
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Class I; (SD) | Class III; (SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T3 | T0 | T1 | T2 | T3 | ||
| SNA | Female | 81.91 (3.19) | 81.82 (3.41) | 81.52 (3.95) | 81.86 (2.64) | 81.69 (2.88) | 81.03 (2.36) | 81.39 (3.96) | 81.92 (2.5) |
| Male | 77.83 (4.24) | 78.97 (4.59) | 81.03 (2.48) | 80.99 (2.71) | 82.9 (4.43) | 81.33 (4.63) | 81.63 (5.07) | 82.23 (5.26) | |
| Total | 79.87 (4.22) | 80.39 (4.21) | 81.28 (3.24) | 81.42 (2.65) | 82.25 (3.64) | 81.17 (3.5) | 81.5 (4.4) | 82.06 (3.91) | |
| SNB | Female | 75.1 (3.74) | 76.93 (3.05) | 77.05 (3.65) | 78.19 (3.31) | 77.44 (3.32) | 78.53 (3.22) | 79.61 (3.35) | 81.27 (3.28) |
| Male | 73.76 (3.44) | 75.36 (3.82) | 77.32 (2.39) | 78.09 (2.44) | 78.3 (3.55) | 78.58 (3.16) | 80.34 (3.57) | 81.51 (3.28) | |
| Total | 74.43 (3.58) | 76.15 (3.47) | 77.19 (3.02) | 78.14 (2.84) | 77.83 (3.38) | 78.55 (3.12) | 79.95 (3.4) | 81.38 (3.21) | |
| ANB | Female | 5.98 (2.21) | 4.88 (1.76) | 4.47 (2.64) | 3.67 (1.99) | 4.25 (1.8) | 2.5 (1.81) | 1.77 (3.17) | 0.64 (2.22) |
| Male | 4.07 (2.06) | 3.61 (1.97) | 3.71 (1.42) | 2.9 (1.8) | 4.61 (3.33) | 2.75 (2.97) | 1.29 (3) | 0.71 (3.33) | |
| Total | 5.02 (2.31) | 4.25 (1.94) | 4.09 (2.11) | 3.28 (1.9) | 4.42 (2.56) | 2.61 (2.36) | 1.55 (3.04) | 0.68 (2.72) | |
| Björk’s sum | Female | 395.07 (5.07) | 393.4 (4.49) | 392.83 (4.87) | 390.11 (7.83) | 395.58 (4.54) | 395.97 (4.52) | 395.34 (3.16) | 395.54 (5.57) |
| Male | 379.18 (57.09) | 393.29 (4.52) | 391.58 (3.45) | 388.39 (4.92) | 395.24 (3.6) | 395.18 (3.88) | 394.4 (6.11) | 394.1 (5.69) | |
| Total | 387.12 (40.46) | 393.34 (4.41) | 392.2 (4.18) | 389.25 (6.45) | 395.42 (4.05) | 395.61 (4.17) | 394.91 (4.66) | 394.88 (5.55) | |
| FMA | Female | 27.39 (5.38) | 26.91 (6.28) | 26.13 (4.68) | 22.07 (7.4) | 27.81 (3.63) | 27.33 (5.1) | 26.26 (3.62) | 27.4 (5.58) |
| Male | 28.3 (5.96) | 26 (5.45) | 24.09 (4.5) | 20.39 (4.65) | 28.58 (3.01) | 27.82 (2.94) | 27.4 (4.27) | 27.01 (5.23) | |
| Total | 27.85 (5.57) | 26.45 (5.77) | 25.11 (4.61) | 21.23 (6.1) | 28.17 (3.31) | 27.56 (4.17) | 26.78 (3.88) | 27.22 (5.31) | |
| Gonial angle | Female | 126.86 (8.25) | 124.98 (8.78) | 124.08 (5.46) | 121.25 (10.1) | 127.42 (6.83) | 129.27 (6.67) | 128.04 (6.1) | 128.4 (6.97) |
| Male | 127.57 (8.29) | 126.2 (7.23) | 122.97 (5.96) | 120.14 (6.02) | 130.01 (5.45) | 129.09 (5.02) | 130.64 (6.41) | 129.26 (6.57) | |
| Total | 127.21 (8.09) | 125.59 (7.89) | 123.53 (5.62) | 120.69 (8.15) | 128.61 (6.25) | 129.19 (5.85) | 129.23 (6.24) | 128.8 (6.65) | |
| APDI | Female | 77.13 (3.75) | 78.13 (3.49) | 79.76 (6.35) | 81.32 (5.44) | 79.83 (4.37) | 83.54 (5.7) | 84.2 (5.16) | 84.64 (5.07) |
| Male | 78.01 (5.54) | 78.16 (3.88) | 78.6 (2.55) | 80.43 (3.23) | 81.15 (6.91) | 84.98 (5.19) | 85.68 (5.36) | 86.48 (6.49) | |
| Total | 77.57 (4.65) | 78.15 (3.61) | 79.18 (4.77) | 80.87 (4.4) | 80.44 (5.58) | 84.2 (5.4) | 84.88 (5.19) | 85.48 (5.71) | |
| ODI | Female | 78.24 (6.26) | 78.86 (5.48) | 78.02 (5.56) | 77.49 (7.36) | 73.08 (5.54) | 69.2 (4.97) | 69.73 (5.75) | 67.83 (5.72) |
| Male | 78.43 (10.29) | 77.11 (4.89) | 75.86 (4.47) | 75.83 (4.25) | 74.8 (5.83) | 72.03 (5.8) | 69.36 (5.18) | 68.91 (5.88) | |
| Total | 78.34 (8.33) | 77.98 (5.16) | 76.94 (5.06) | 76.66 (5.94) | 73.87 (5.62) | 70.49 (5.44) | 69.56 (5.38) | 68.33 (5.69) | |
| Combination factor | Female | 154.71 (8.21) | 156.99 (6.55) | 157.78 (6.92) | 158.81 (7.94) | 152.92 (6.06) | 152.74 (7.03) | 153.92 (6.16) | 152.48 (6.45) |
| Male | 156.45 (12.93) | 155.27 (6.09) | 154.46 (4.11) | 156.26 (4.84) | 155.95 (2.95) | 157 (6.51) | 155.04 (5.11) | 155.38 (6.42) | |
| Total | 155.58 (10.62) | 156.13 (6.25) | 156.12 (5.82) | 157.54 (6.56) | 154.3 (5.03) | 154.69 (7) | 154.44 (5.61) | 153.81 (6.46) | |
| FH to AB | Female | 75.33 (4.41) | 76.18 (4.03) | 77.8 (4.78) | 80.05 (6.88) | 79.47 (3.92) | 83.51 (5.59) | 84.1 (5.06) | 84.7 (5.52) |
| Male | 75.64 (5.42) | 77.53 (4.69) | 79.32 (3.95) | 82.1 (3.69) | 78.89 (6.41) | 82.56 (4.71) | 84.51 (4.69) | 85.28 (5.92) | |
| Total | 75.49 (4.83) | 76.85 (4.33) | 78.56 (4.36) | 81.07 (5.5) | 79.2 (5.1) | 83.07 (5.12) | 84.29 (4.79) | 84.97 (5.59) | |
| A-B mandibular plane | Female | 77.28 (4.34) | 76.91 (4.93) | 76.07 (5.94) | 77.06 (7.16) | 72.72 (4.75) | 69.16 (3.79) | 69.63 (4.65) | 67.89 (4.77) |
| Male | 76.06 (6.45) | 76.48 (3.65) | 76.59 (3.55) | 77.51 (3.74) | 72.53 (6.39) | 69.61 (4.62) | 68.15 (5.41) | 67.71 (5.88) | |
| Total | 76.67 (5.41) | 76.69 (4.25) | 76.33 (4.79) | 77.28 (5.59) | 72.63 (5.43) | 69.37 (4.1) | 68.95 (4.96) | 67.81 (5.19) | |
| U1 to FH | Female | 99.69 (6.49) | 107.53 (8.01) | 108.36 (7.76) | 109.02 (7.83) | 100.2 (8.51) | 104.8 (7.04) | 112.11 (6.01) | 110.08 (6.7) |
| Male | 98.85 (9.63) | 105.29 (8.78) | 110.44 (6.81) | 110.24 (5.56) | 99.75 (5.96) | 103.91 (5.87) | 110.45 (6.2) | 112.16 (6.42) | |
| Total | 99.27 (8.04) | 106.41 (8.3) | 109.4 (7.22) | 109.63 (6.67) | 99.99 (7.29) | 104.39 (6.41) | 111.35 (6.03) | 111.04 (6.51) | |
| U1 to SN | Female | 92.01 (7.47) | 101.04 (7.37) | 101.67 (8.74) | 100.98 (8.42) | 92.44 (8.72) | 96.15 (7.03) | 103.12 (6.74) | 101.94 (7.52) |
| Male | 91.26 (9.67) | 98.02 (9.41) | 102.95 (5.7) | 102.24 (5.55) | 92.78 (6.44) | 96.55 (5.38) | 103.43 (6.55) | 105.14 (6.48) | |
| Total | 91.64 (8.46) | 99.53 (8.41) | 102.31 (7.25) | 101.61 (7.01) | 92.6 (7.6) | 96.33 (6.2) | 103.26 (6.51) | 103.41 (7.1) | |
| U1 to UOP | Female | 65.31 (6.32) | 58.95 (5.47) | 57.29 (4.23) | 60.46 (4.67) | 67.19 (7) | 62.17 (4.38) | 57.34 (4.7) | 59.61 (5.35) |
| Male | 64.48 (9) | 61.99 (6.61) | 56.5 (3.48) | 60.38 (4.11) | 66.59 (4.35) | 65.81 (4.84) | 58.27 (3.57) | 57.68 (5.71) | |
| Total | 64.89 (7.62) | 60.47 (6.13) | 56.89 (3.81) | 60.42 (4.3) | 66.91 (5.82) | 63.84 (4.86) | 57.77 (4.16) | 58.73 (5.48) | |
| IMPA | Female | 92.65 (5.73) | 95.59 (5.77) | 95.87 (4.15) | 95.72 (5.91) | 84.61 (5.98) | 85.68 (5.83) | 87.28 (3.32) | 84.2 (4.44) |
| Male | 89.78 (7.57) | 93.67 (5.46) | 95.68 (4.74) | 97.65 (5.33) | 85.83 (5.65) | 85.13 (7.86) | 87.14 (6.4) | 87.52 (7.78) | |
| Total | 91.22 (6.73) | 94.63 (5.58) | 95.78 (4.36) | 96.68 (5.59) | 85.17 (5.74) | 85.43 (6.68) | 87.22 (4.86) | 85.72 (6.28) | |
| L1 to LOP | Female | 75.37 (4.77) | 69.39 (4.46) | 68.21 (5.5) | 67.88 (6.17) | 80.51 (4.73) | 79.55 (3.49) | 74.01 (3.84) | 75.91 (4.66) |
| Male | 76.71 (5.52) | 71.47 (6.98) | 68.51 (5.3) | 65.3 (5) | 79.95 (7) | 78.25 (6.21) | 73.4 (7.35) | 73.87 (8.42) | |
| Total | 76.04 (5.09) | 70.43 (5.83) | 68.36 (5.28) | 66.59 (5.65) | 80.25 (5.75) | 78.96 (4.85) | 73.73 (5.59) | 74.98 (6.57) | |
| Interincisal angle | Female | 140.27 (6.34) | 129.97 (8.21) | 129.63 (8.45) | 133.2 (8.15) | 147.37 (8.84) | 142.2 (8) | 134.34 (7.18) | 138.31 (5.33) |
| Male | 143.07 (10.85) | 135.08 (10.29) | 129.79 (7.69) | 131.72 (8.19) | 146.15 (9.27) | 143.14 (7.31) | 135.03 (5.93) | 133.31 (8.76) | |
| Total | 141.67 (8.81) | 132.52 (9.47) | 129.71 (7.9) | 132.46 (8.03) | 146.81 (8.86) | 142.63 (7.54) | 134.66 (6.5) | 136.02 (7.4) | |
| Cant of the occlusal plane | Female | 15.14 (2.94) | 12.78 (5.13) | 12.47 (4.01) | 8.29 (3.98) | 12.82 (2.99) | 12.81 (4.56) | 9.15 (4.32) | 9.01 (4.27) |
| Male | 15.8 (3.8) | 11.98 (4.08) | 10.87 (4.03) | 6.61 (2.81) | 13.91 (3.68) | 10.74 (4.46) | 9.74 (4.19) | 9.32 (3.82) | |
| Total | 15.47 (3.34) | 12.38 (4.55) | 11.67 (4.02) | 7.45 (3.47) | 13.32 (3.3) | 11.86 (4.54) | 9.42 (4.18) | 9.15 (3.99) | |
| U1 to NA | Female | 10.1 (7.87) | 19.22 (6.6) | 20.15 (6.72) | 19.12 (7.21) | 10.75 (7.71) | 15.13 (5.59) | 21.73 (4.48) | 20.03 (5.69) |
| Male | 13.48 (11.91) | 19.02 (8.19) | 21.92 (5.4) | 21.25 (4.74) | 9.88 (8.07) | 15.22 (6.71) | 21.8 (6.63) | 22.85 (6.92) | |
| Total | 11.79 (10.02) | 19.12 (7.27) | 21.03 (6.03) | 20.18 (6.07) | 10.35 (7.72) | 15.17 (5.99) | 21.76 (5.44) | 21.32 (6.31) | |
| L1 to NB | Female | 23.65 (3.38) | 25.92 (4.96) | 26.06 (4.31) | 24.01 (4.21) | 17.62 (4.76) | 20.18 (4.22) | 21.41 (4.07) | 19.45 (3.45) |
| Male | 19.39 (8.09) | 22.29 (7.22) | 23.75 (6.22) | 24.13 (5.56) | 19.37 (5.65) | 18.9 (6.58) | 21.38 (5.84) | 22.14 (6.88) | |
| Total | 21.52 (6.44) | 24.11 (6.33) | 24.9 (5.37) | 24.07 (4.82) | 18.42 (5.14) | 19.59 (5.34) | 21.4 (4.84) | 20.69 (5.35) | |
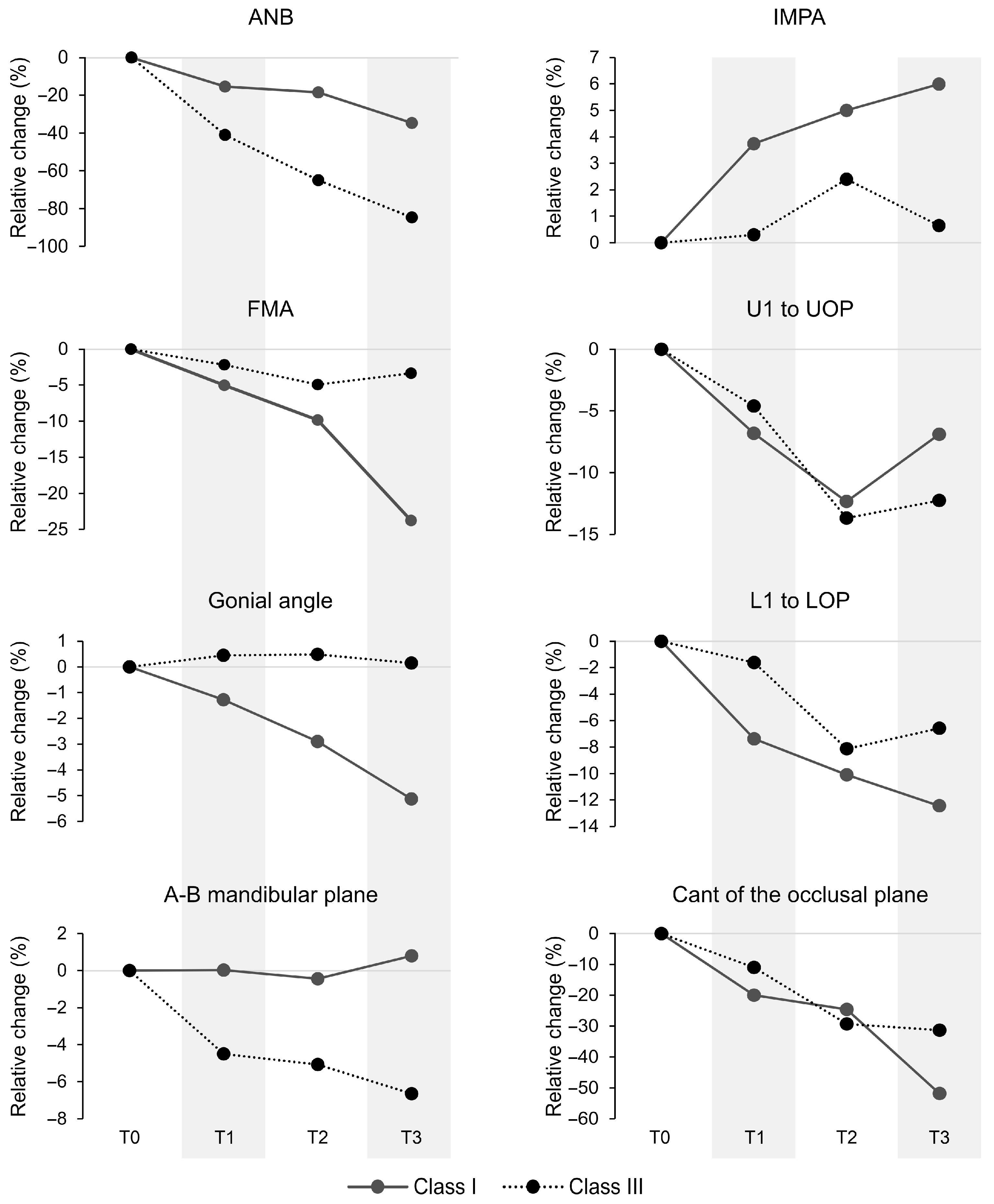
| The ANB angle in Class I malocclusion was 35% lower at T3 than at T0 (p = 0.002; Figure 2). In Class III, it was significantly lower at T1, T2, and T3 compared to T0 (−41%, −65%, and −85%, respectively; p < 0.01). The FMA angle in Class I malocclusion was significantly lower at T3 than at T0–T2 (p < 0.001), with a 24% reduction from T0 (Figure 2). No significant changes were found in Class III. Similarly, the gonial angle in Class I malocclusion was significantly lower at T3 than at T0 and T1 (p < 0.01), with a 5% reduction from T0 (Figure 2). No significant changes were observed for Class III. The A–B mandibular angle in Class I malocclusion showed no significant changes across time points. In contrast, Class III malocclusion showed significant reductions at T1 (−4.5%), T2 (−5.1%), and T3 (−6.6%) compared to T0 (p < 0.05; Figure 2). The U1 to UOP angle in Class I malocclusion was significantly higher at T0 than at T1–T3 (p < 0.05), with reductions of 6.8% at T1, 12.3% at T2, and 6.8% at T3 (Figure 2). In Class III, the angle at T0 was significantly higher than at T2 and T3 (p < 0.001), with reductions of 13.6% and 12.2%, respectively. The L1 to LOP angle in Class I was significantly higher at T0 than at T1–T3 (p < 0.001; reductions of 7.4%, 10.1%, and 12.4%, respectively; Figure 2), and T1 was higher than T3 (p = 0.014). In Class III, angles at T0 and T1 were significantly higher than at T2 and T3 (p < 0.001), with reductions of 8.1% and 6.5% from T0. The IMPA angle in Class I increased significantly at T2 and T3 compared to T0 (by ~5% and 6%, respectively; p < 0.05; Figure 2), with no significant changes in Class III. The cant of the occlusal plane angle in Class I was significantly higher at T0 than at T1 (−20%), T2 (−24.6%), and T3 (−51.8%) (p < 0.001; Figure 2), with T3 also significantly higher than T1 and T2 (p < 0.001). In Class III, T0 was significantly higher than T2 (−29.3%) and T3 (−31.3%) (p < 0.001), and T1 was higher than T3 (p = 0.023). |
References
- Sörensen, C.; Lemberger, M.; Larsson, P.; Pegelow, M. Comparing Oral Health-Related Quality of Life, Oral Function and Orofacial Aesthetics among a Group of Adolescents with and without Malocclusions. Acta Odontol. Scand. 2022, 80, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Blanch, K.; Antoun, J.; Smith, L.; Jack, H.; Fowler, P.; Page, L.F. Considering Malocclusion as a Disability. Australas. Orthod. J. 2019, 35, 27–34. [Google Scholar] [CrossRef]
- Zawawi, K.H.; Alsulaimani, F.F.; Al-Dharrab, A.A.; Afify, A.R.; Al-Zahrani, M.S.; Baeshen, H.A. Morphological Features of Class I, II and III Malocclusions of Saudi Adolescents. Saudi J. Biol. Sci. 2021, 28, 3534–3539. [Google Scholar] [CrossRef]
- Zere, E.; Chaudhari, P.K.; Saran, J.; Dhingra, K.; Tiwari, N. Developing Class III Malocclusions: Challenges and Solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global Distribution of Malocclusion Traits: A Systematic Review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef]
- Almotairy, N.; Almutairi, F. A Nation-Wide Prevalence of Malocclusion Traits in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2022, 12, 1–11. [Google Scholar] [CrossRef]
- Zhou, X.; Chen, S.; Zhou, C.; Jin, Z.; He, H.; Bai, Y.; Li, W.; Wang, J.; Hu, M.; Cao, Y.; et al. Expert Consensus on Early Orthodontic Treatment of Class III Malocclusion. Int. J. Oral Sci. 2025, 17, 20. [Google Scholar] [CrossRef]
- Pérez-Varela, J.C.; Campoy, M.D.; López-Vila, M.; Camañes-Gonzalvo, S.; García-Sanz, V.; Paredes-Gallardo, V. Management of Skeletal Class III Discrepancies Using Temporary Anchorage Devices. Clinical Cases Review and Biomechanical Considerations. Semin. Orthod. 2024, 30, 572–590. [Google Scholar] [CrossRef]
- Reyes, B.C.; Baccetti, T.; McNamara, J.A. An Estimate of Craniofacial Growth in Class III Malocclusion. Angle Orthod. 2006, 76, 577–584. [Google Scholar] [CrossRef]
- Wolfe, S.M.; Araujo, E.; Behrents, R.G.; Buschang, P.H. Craniofacial Growth of Class III Subjects Six to Sixteen Years of Age. Angle Orthod. 2011, 81, 211–216. [Google Scholar] [CrossRef]
- Tollaro, I.; Baccetti, T.; Bassarelli, V.; Franchi, L. Class III Malocclusion in the Deciduous Dentition: A Morphological and Correlation Study. Eur. J. Orthod. 1994, 16, 401–408. [Google Scholar] [CrossRef]
- Battagel, J.M. The Aetiological Factors in Class III Malocclusion. Eur. J. Orthod. 1993, 15, 347–370. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.P.; Kinoshita, Z.; Kawamoto, T. Craniofacial Pattern of Class III Deciduous Dentition. Angle Orthod. 1992, 62, 139–144. [Google Scholar] [CrossRef]
- Guyer, E.C.; Ellis, E.E.; McNamara, J.A.; Behrents, R.G. Components of Class III Malocclusion in Juveniles and Adolescents. Angle Orthod. 1986, 56, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Farias, V.C.; Tesch, R.D.S.; Denardin, O.V.P.; Ursi, W. Early Cephalometric Characteristics in Class III Malocclusion. Dent. Press J. Orthod. 2012, 17, 49–54. [Google Scholar] [CrossRef][Green Version]
- Zegan, G.; Dascălu, C.; Mavru, R.B.; Anistoroaei, D. Cephalometric Features of Class III Malocclusion. Rev. Med. Chir. Soc. Med. Nat. Iasi 2015, 119, 1153–1160. [Google Scholar][Green Version]
- Chen, F.; Terada, K.; Wu, L.; Saito, I. Longitudinal Evaluation of the Intermaxillary Relationship in Class III Malocclusions. Angle Orthod. 2006, 76, 955–961. [Google Scholar] [CrossRef]
- Elhakeem, A.; Hughes, R.A.; Tilling, K.; Cousminer, D.L.; Jackowski, S.A.; Cole, T.J.; Kwong, A.S.F.; Li, Z.; Grant, S.F.A.; Baxter-Jones, A.D.G.; et al. Using Linear and Natural Cubic Splines, SITAR, and Latent Trajectory Models to Characterise Nonlinear Longitudinal Growth Trajectories in Cohort Studies. BMC Med. Res. Methodol. 2022, 22, 68. [Google Scholar] [CrossRef]
- Boedeker, P. Nonlinear Mixed-Effects Growth Models: A Tutorial Using “saemix” in R. Methodology 2021, 17, 250–270. [Google Scholar] [CrossRef]
- Thelwell, M.; Bullas, A.; Kühnapfel, A.; Hart, J.; Ahnert, P.; Wheat, J.; Loeffler, M.; Scholz, M.; Choppin, S. Modelling of Human Torso Shape Variation Inferred by Geometric Morphometrics. PLoS ONE 2022, 17, e0265255. [Google Scholar] [CrossRef]
- Tai, K.; Park, J.; Ohmura, S.; Okadakage-Hayashi, S. Timing of Class III Treatment with Unfavorable Growth Pattern. J. Clin. Pediatr. Dent. 2014, 38, 370–379. [Google Scholar] [CrossRef]
- da Silva, D.B.H.; Gonzaga, A.S. Importance of Orthodontic Intervention of the Class III Malocclusion in Mixed Dentition. Dental Press J. Orthod. 2020, 25, 57–65. [Google Scholar] [CrossRef]
- Owens, D.; Watkinson, S.; Harrison, J.E.; Turner, S.; Worthington, H. V Orthodontic Treatment for Prominent Lower Front Teeth (Class III Malocclusion) in Children. Cochrane Database Syst. Rev. 2024, 2024, CD003451. [Google Scholar] [CrossRef]
- Mahto, R.K.; Kafle, D.; Giri, A.; Luintel, S.; Karki, A. Evaluation of Fully Automated Cephalometric Measurements Obtained from Web-Based Artificial Intelligence Driven Platform. BMC Oral Health 2022, 22, 132. [Google Scholar] [CrossRef]
- Chung, C.-H.; Mongiovi, V.D. Craniofacial Growth in Untreated Skeletal Class I Subjects with Low, Average, and High MP-SN Angles: A Longitudinal Study. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 670–678. [Google Scholar] [CrossRef]
- Zionic Alexander, A.E.; McNamara, J.A.; Franchi, L.; Baccetti, T. Semilongitudinal Cephalometric Study of Craniofacial Growth in Untreated Class III Malocclusion. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 700.e1–700.e14. [Google Scholar] [CrossRef]
- Baccetti, T.; Reyes, B.C.; McNamara, J.A. Gender Differences in Class III Malocclusion. Angle Orthod. 2005, 75, 510–520. [Google Scholar] [CrossRef]
- Santana, L.G.; Flores-Mir, C.; Iglesias-Linares, A.; Pithon, M.M.; Marques, L.S. Influence of Heritability on Occlusal Traits: A Systematic Review of Studies in Twins. Prog. Orthod. 2020, 21, 29. [Google Scholar] [CrossRef] [PubMed]
- Lux, C.J.; Burden, D.; Conradt, C.; Komposch, G. Age-Related Changes in Sagittal Relationship between the Maxilla and Mandible. Eur. J. Orthod. 2005, 27, 568–578. [Google Scholar] [CrossRef]
- Bishara, S.E.; Fahl, J.A.; Peterson, L.C. Longitudinal Changes in the ANB Angle and Wits Appraisal: Clinical Implications. Am. J. Orthod. 1983, 84, 133–139. [Google Scholar] [CrossRef]
- Mohsen, A.M.; Ye, J.; Al-Nasri, A.; Chu, C.; Zhang, W.-B.; Wang, L. Three-Dimensional Evaluation of the Mandibular Condyle in Adults with Various Skeletal Patterns. Korean J. Orthod. 2023, 53, 67–76. [Google Scholar] [CrossRef]
- Rajbhoj, A.A.; Stroo, M.; Begnoni, G.; Willems, G.; de Llano-Pérula, M.C. Skeletal and Soft-Tissue Changes in Humans with Untreated Normal Occlusion throughout Lifetime: A Systematic Review. Odontology 2023, 111, 263–309. [Google Scholar] [CrossRef]
- Boccalari, E.; Rossi, O.; Baldini, B.; Tripicchio, C.; Serafin, M.; Caprioglio, A. The Maxillomandibular Sagittal Assessment: The ABwise Appraisal and Its Correlation with ANB Angle. J. Clin. Med. 2025, 14, 1379. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, P.M.; Little, R.M. Dentofacial Maturation of Untreated Normals. Am. J. Orthod. 1985, 88, 146–156. [Google Scholar] [CrossRef]
- Sanborn, R.T. Differences Between the Facial Skeletal Patterns Of Class III Malocclusion and Normal Occlusion. Angle Orthod. 1955, 25, 208–222. [Google Scholar]
- Baccetti, T.; Franchi, L.; McNamara, J.A. Growth in the Untreated Class III Subject. Semin. Orthod. 2007, 13, 130–142. [Google Scholar] [CrossRef]
- Andria, L.M.; Leite, L.P.; Dunlap, A.M.; Cooper, E.C.; King, L.B. Mandibular First Molar Relation to Variable Lower Face Skeletal Components. Angle Orthod. 2007, 77, 21–28. [Google Scholar] [CrossRef]
- Chang, H.-P.; Kinoshita, Z.; Kawamoto, T. A Study of the Growth Changes in Facial Configuration. Eur. J. Orthod. 1993, 15, 493–501. [Google Scholar] [CrossRef]
- Ardani, I.G.A.W.; Wicaksono, A.; Hamid, T. The Occlusal Plane Inclination Analysis for Determining Skeletal Class III Malocclusion Diagnosis. Clin. Cosmet. Investig. Dent. 2020, 12, 163–171. [Google Scholar] [CrossRef]
- Mathapun, J.; Charoemratrote, C. Is Incisor Compensation Related to Skeletal Discrepancies in Skeletal Class III? A Retrospective Cephalometric Study. Diagnostics 2024, 14, 1021. [Google Scholar] [CrossRef]
- Liu, L.; Liu, Y.; Guo, K.; Ma, H.; Yang, F. Soft and Hard Tissue Changes after Compensatory Treatment in Skeletal Class III Malocclusion. PLoS ONE 2025, 20, e0322551. [Google Scholar] [CrossRef]
- Kale, B.; Buyukcavus, M.H. Effects of Maxillary Protraction with Skeletal Anchorage and Petit-Type Facemask in High-Angle Class III Patients: A Retrospective Study. J. Clin. Diagn. Res. 2020, 14, 24. [Google Scholar] [CrossRef]
- Ray, P.; Sahoo, P.K.; Sahoo, S.S.; Dash, J.K.; Das, S.K.; Baliarsingh, R.R. Early Orthodontic Intervention in Cleft Lip–Palate and Noncleft Children with Developing Class III Malocclusion: A Clinical Study. Int. J. Clin. Pediatr. Dent. 2023, 16, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Patcas, R.; Wiedemeier, D.B.; Markic, G.; Beit, P.; Keller, H. Evidence of Secular Trend in Mandibular Pubertal Growth. Eur. J. Orthod. 2017, 39, 680–685. [Google Scholar] [CrossRef]

| No. | Cephalometric Variable | Definition |
|---|---|---|
| 1 | SNA | Angle between Sella-Nasion-A point. |
| 2 | SNB | Angle between Sella-Nasion-B point. |
| 3 | ANB | The difference between SNA and SNB. |
| 4 | FMA | Angle between Frankfort horizontal plane (FH) and the lower border of the mandible. |
| 5 | Gonial angle (Ar-Go-Me) | Angle formed by the posterior border of the ramus and the lower border of the mandible. |
| 6 | A-B mandibular angle | Angle between points A and B relative to the lower border of the mandible. |
| 7 | Björk’s sum | Sum of saddle (Ar-S-N), articulare (S-Ar-Go), and gonial (Ar-Go-Me) angles. |
| 8 | Antero-posterior Dysplasia Indicator (APDI) | Sum of facial angle (FH to NPog) ± A-B plane angle (AB to NPog) ± palatal plane angle (ANS-PNS to FH). |
| 9 | Overbite Depth Indicator (ODI) | The arithmetic sum of the A-B mandibular angle and the palatal plane to the Frankfort horizontal plane angle. |
| 10 | Combination factor | The sum of APDI and ODI. |
| 11 | FH to AB | The angle between Frankfort’s horizontal plane and the AB line. |
| 12 | U1 to FH | The angle between the upper incisor long axis (U1) and the Frankfort horizontal plane. |
| 13 | U1 to SN | The angle between the upper incisor long axis and the S-N line. |
| 14 | U1 to NA | The angle between the upper incisor long axis and the N-A point line. |
| 15 | U1 to UOP | Angle between the upper incisor long axis and the occlusal plane. |
| 16 | L1 to NB | The angle between the lower incisor long axis (L1) and the N-B point line. |
| 17 | L1 to LOP | The angle between the lower incisor long axis and the occlusal plane. |
| 18 | IMPA | The angle formed between the lower incisor long axis and the lower border of the mandible. |
| 19 | Cant of the occlusal plane | Angle of occlusal plane relative to Frankfort horizontal plane. |
| 20 | Interincisal angle | Angle between the upper and lower incisor long axes. |
| Group | n | T0 | T1 | T2 | T3 | |
|---|---|---|---|---|---|---|
| (SD) | (SD) | (SD) | (SD) | |||
| Class I | Female | 12 | 4.23 (0.14) | 7.3 (0.6) | 10.13 (0.28) | 13.15 (0.27) |
| Male | 12 | 4.19 (0.13) | 6.97 (0.49) | 10.05 (0.07) | 13.05 (0.09) | |
| Total | 24 | 4.21 (0.13) | 7.13 (0.56) | 10.09 (0.2) | 13.1 (0.21) | |
| Class III | Female | 12 | 4.8 (0.77) | 7.45 (0.54) | 10.34 (0.47) | 13.2 (0.74) |
| Male | 12 | 4.65 (0.47) | 7.12 (0.3) | 10.3 (0.45) | 13.12 (0.3) | |
| Total | 24 | 4.73 (0.64) | 7.3 (0.47) | 10.32 (0.45) | 13.16 (0.56) | |
| p-value * | Female | 0.02 | 0.49 | 0.18 | 0.82 | |
| Male | 0.004 | 0.4 | 0.07 | 0.46 | ||
| Total | 0.001 | 0.27 | 0.03 | 0.61 | ||
| Variable | T0 | T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|---|---|
| MD | 95% CI | MD | 95% CI | MD | 95% CI | MD | 95% CI | |
| SNA | 2.38 | [0.087, 4.667] | 0.77 | [−2.101, 3.645] | 0.22 | [−2.646, 3.088] | 0.64 | [−2.044, 3.317] |
| SNB | 3.4 | [0.608, 6.191] | 2.41 | [−0.24, 5.051] | 2.76 | [0.184, 5.337] | 3.25 | [0.817, 5.675] |
| ANB | −0.61 | [−3.629, 2.418] | −1.63 | [−4.313, 1.047] | −2.54 | [−4.94, −0.139] | −2.61 | [−5.523, 0.305] |
| Björk’s sum | 8.3 | [−8.451, 25.048] | 2.27 | [−0.765, 5.297] | 2.71 | [−0.418, 5.832] | 5.63 | [1.762, 9.506] |
| FMA | 0.32 | [−2.919, 3.556] | 1.1 | [−2.333, 4.539] | 1.67 | [−1.341, 4.682] | 6 | [2.262, 9.732] |
| Gonial angle | 1.39 | [−3.155, 5.939] | 3.6 | [−0.815, 8.007] | 5.7 | [1.824, 9.582] | 8.1 | [3.425, 12.783] |
| APDI | 2.86 | [−0.558, 6.284] | 6.05 | [2.916, 9.19] | 5.7 | [2.3, 9.103] | 4.61 | [1.219, 8.003] |
| ODI | −4.47 | [−8.982, 0.046] | −7.49 | [−11.017, −3.961] | −7.39 | [−10.861, −3.91] | −8.34 | [−12.135, −4.54] |
| Combination factor | −1.27 | [−6.456, 3.913] | −1.44 | [−5.65, 2.778] | −1.68 | [−5.417, 2.05] | −3.73 | [−7.864, 0.412] |
| FH to AB | 3.72 | [0.325, 7.107] | 6.22 | [2.985, 9.454] | 5.73 | [2.606, 8.86] | 3.89 | [0.272, 7.514] |
| A-B mandibular plane | −4.03 | [−7.643, −0.423] | −7.32 | [−10.271, −4.373] | −7.38 | [−10.703, −4.048] | −9.47 | [−13.061, −5.885] |
| U1 to FH | 0.73 | [−4.064, 5.514] | −2.02 | [−6.68, 2.643] | 1.95 | [−2.277, 6.173] | 1.41 | [−2.779, 5.599] |
| U1 to SN | 0.96 | [−4.016, 5.94] | −3.19 | [−7.838, 1.451] | 0.95 | [−3.424, 5.33] | 1.8 | [−2.635, 6.236] |
| U1 to UOP | 2.02 | [−2.284, 6.327] | 3.37 | [−0.319, 7.05] | 0.88 | [−2.083, 3.834] | −1.69 | [−5.057, 1.674] |
| IMPA | −6.04 | [−10.067, −2.023] | −9.2 | [−13.163, −5.244] | −8.56 | [−11.709, −5.412] | −10.97 | [−14.85, −7.082] |
| L1 to LOP | 4.21 | [0.598, 7.825] | 8.52 | [4.954, 12.095] | 5.37 | [1.749, 8.989] | 8.39 | [4.447, 12.331] |
| Interincisal angle | 5.14 | [−0.296, 10.576] | 10.1 | [4.838, 15.369] | 4.94 | [0.393, 9.493] | 3.56 | [−1.254, 8.372] |
| Cant of the occlusal plane | −2.15 | [−4.806, 0.513] | −0.52 | [−3.621, 2.584] | −2.25 | [−5.145, 0.647] | 1.7 | [−1.074, 4.478] |
| U1 to NA | −1.44 | [−6.94, 4.068] | −3.95 | [−8.186, 0.283] | 0.73 | [−3.023, 4.478] | 1.14 | [−2.842, 5.119] |
| L1 to NB | −3.1 | [−6.904, 0.708] | −4.52 | [−8.342, −0.692] | −3.51 | [−6.911, −0.105] | −3.38 | [−6.776, 0.006] |
| Variable | Significant Interaction | Within-Group Differences | Between-Group Differences | |
|---|---|---|---|---|
| Class I | Class III | |||
| SNA | Class × sex × time | ↑ at T2 & T3 in males (~4%) | N.D. | N.D. |
| ANB | Class × time | ↓ at T3 (~35%) | ↓ at T1–T3 (~41% to ~85%) | Class I T0 > Class III T1–T3 Class I T1 & T2 > Class III T2 & T3 Class I T3 > Class III T3 |
| FMA | Class × time | ↓ at T3 (~24%) | N.D. | Class I T3 < Class III T0–T3 |
| Gonial angle | Class × time | ↓ at T3 (~5%) | N.D. | Class I T3 < Class III T0–T3 |
| A-B mandibular angle | Class × time | N.D. | ↓ at T1–T3 (−4.5% to −6.6%) | Class I T0–T2 > Class III T1–T3 Class I T3 > Class III T0–T3 |
| U1 to UOP | Class × time | ↓ at T1–T3 (~7% to ~12%) | ↓ at T2, T3 (~12% to ~14%) | Class I T0 > Class III T2, T3 Class I T1–T3 < Class III T0 Class I T2 < Class III T1 |
| L1 to LOP | Class × time | ↓ at T1–T3 (~7% to ~12%) | ↓ at T2, T3 (~7% to ~8%) | Class I T1 < Class III T1, T2 Class I T2 & T3 < Class III T0–T3 |
| IMPA | Class × time | ↑ at T2, T3 (~5–6%) | N.D. | Class I T0 > Class III T0, T1 & T3 Class I T1–T3 > Class III at T0–T3 |
| Cant of the occlusal plane | Class × time | ↓ at T1–T3 (20% to ~52%) | ↓ at T2, T3 (~29%, ~31%) | Class I T0 > Class III T1–T3 Class I T3 < Class III at T0 & T1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljabr, J.A.S.; Almotairy, N. Longitudinal Skeletal and Dental Changes in Untreated Children with Angle Class I and III Malocclusions: A Retrospective Cephalometric Cohort Study. J. Clin. Med. 2025, 14, 8037. https://doi.org/10.3390/jcm14228037
Aljabr JAS, Almotairy N. Longitudinal Skeletal and Dental Changes in Untreated Children with Angle Class I and III Malocclusions: A Retrospective Cephalometric Cohort Study. Journal of Clinical Medicine. 2025; 14(22):8037. https://doi.org/10.3390/jcm14228037
Chicago/Turabian StyleAljabr, Joud A. S., and Nabeel Almotairy. 2025. "Longitudinal Skeletal and Dental Changes in Untreated Children with Angle Class I and III Malocclusions: A Retrospective Cephalometric Cohort Study" Journal of Clinical Medicine 14, no. 22: 8037. https://doi.org/10.3390/jcm14228037
APA StyleAljabr, J. A. S., & Almotairy, N. (2025). Longitudinal Skeletal and Dental Changes in Untreated Children with Angle Class I and III Malocclusions: A Retrospective Cephalometric Cohort Study. Journal of Clinical Medicine, 14(22), 8037. https://doi.org/10.3390/jcm14228037







