A Three-Decade Analysis of Ischemic Stroke in India: Mortality, Morbidity, and Risk Factors Using the Global Burden of Diseases Study from 1990 to 2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Definition and Metrics
2.2. Computation of Disease Burden Metrics
2.3. Risk Factor Attribution
2.4. Statistical Analysis
3. Results
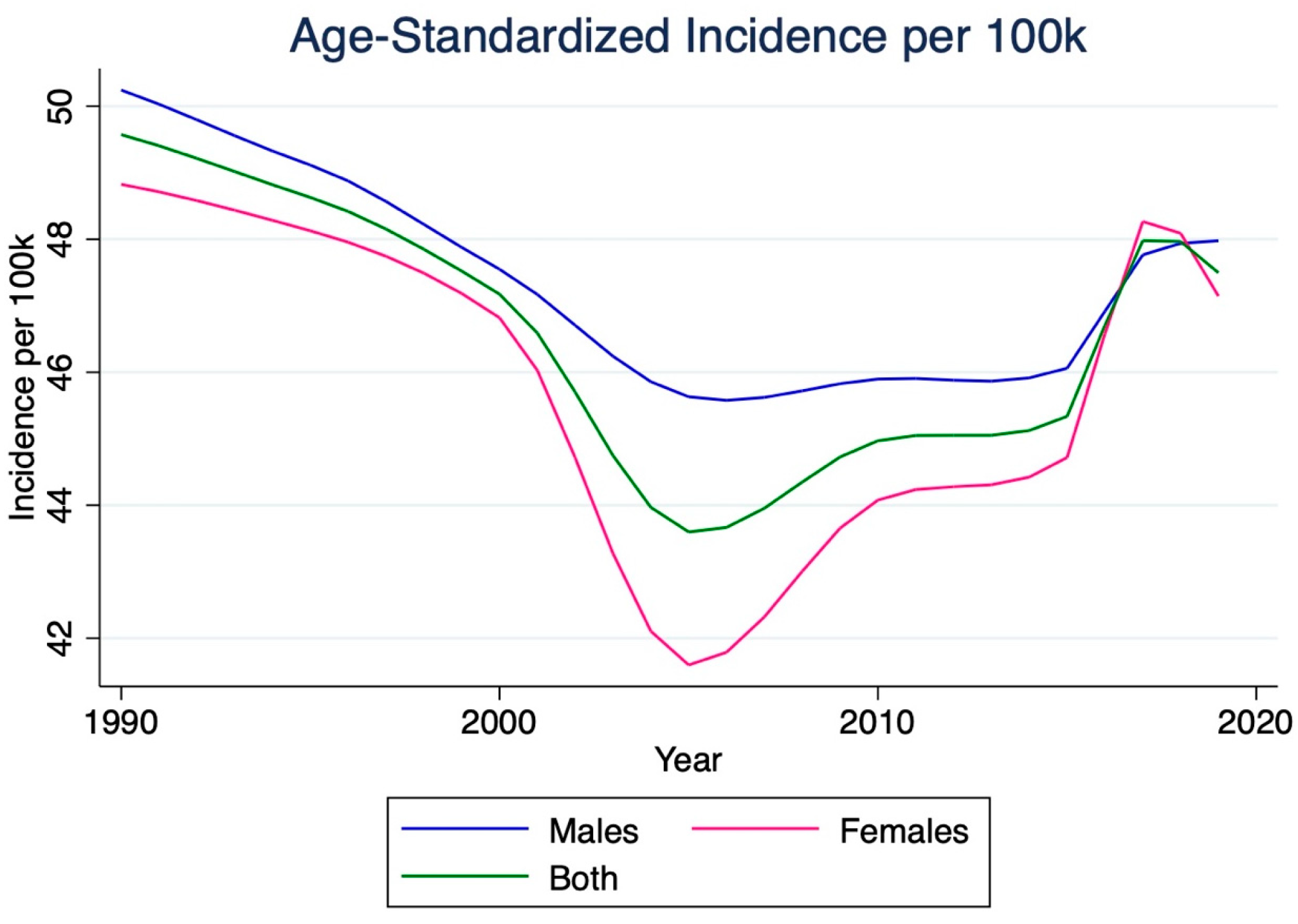
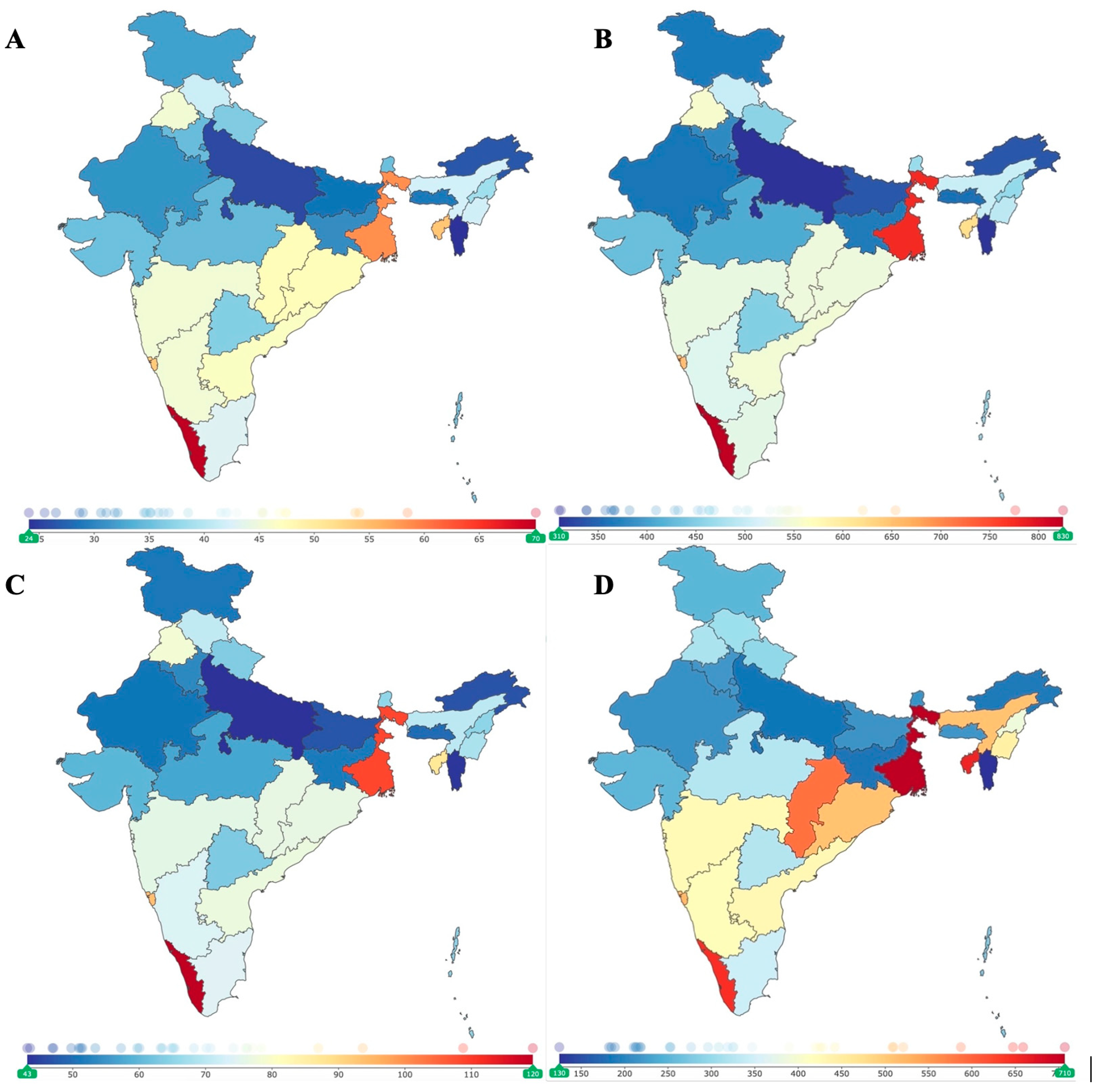
3.1. Incidence
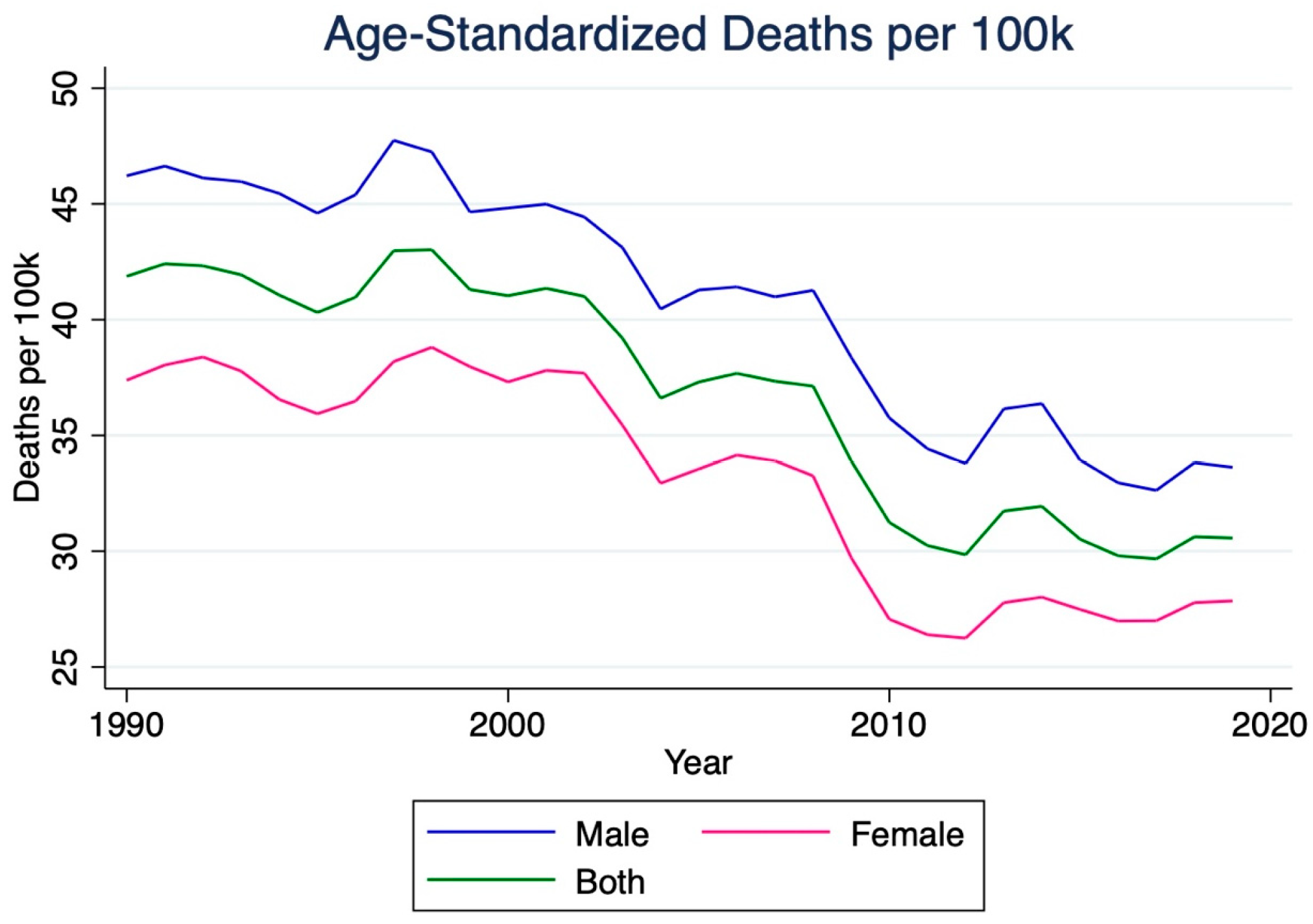
3.2. Mortality
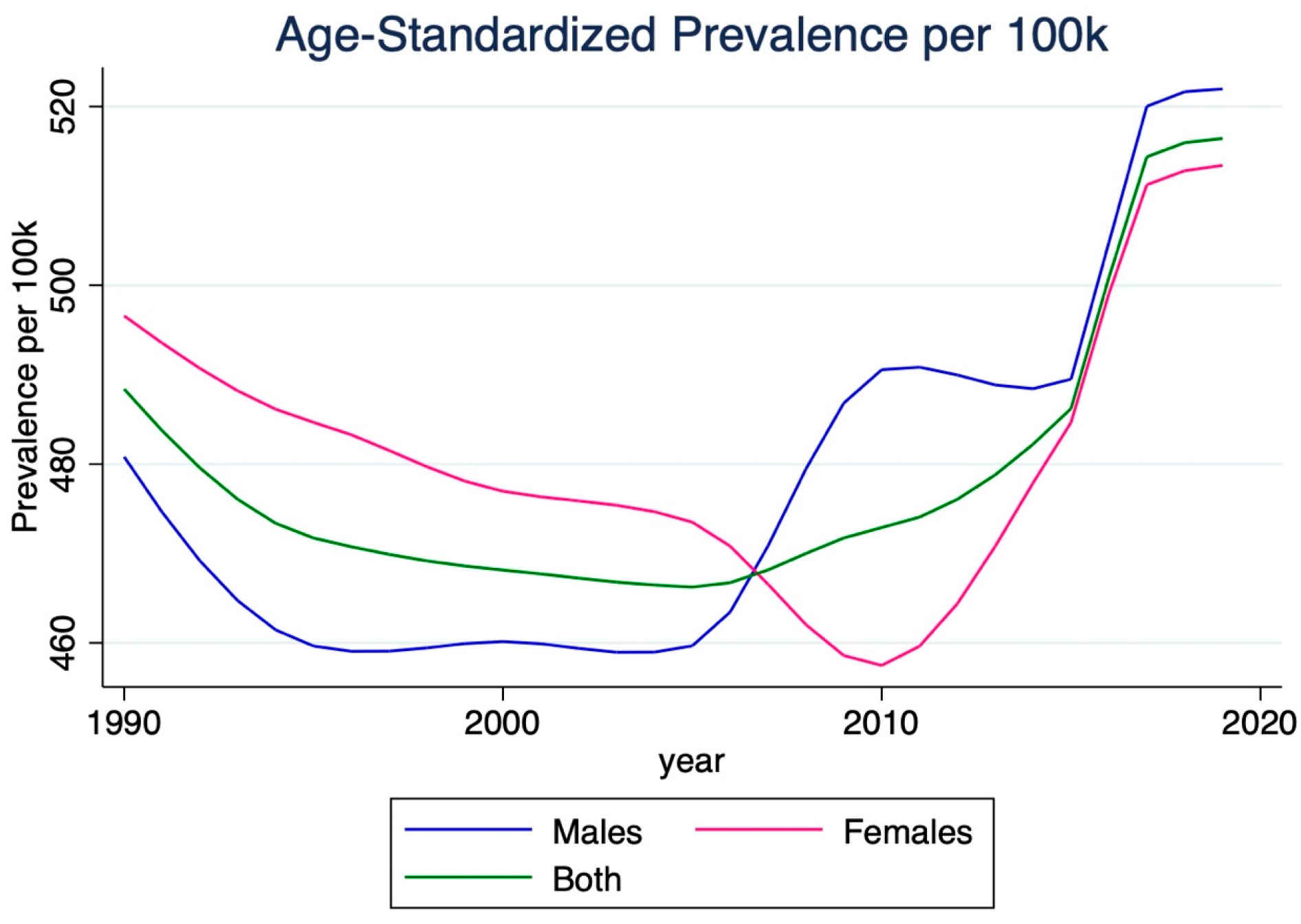
3.3. Prevalence
3.4. Disability-Adjusted Life Years (DALYs)
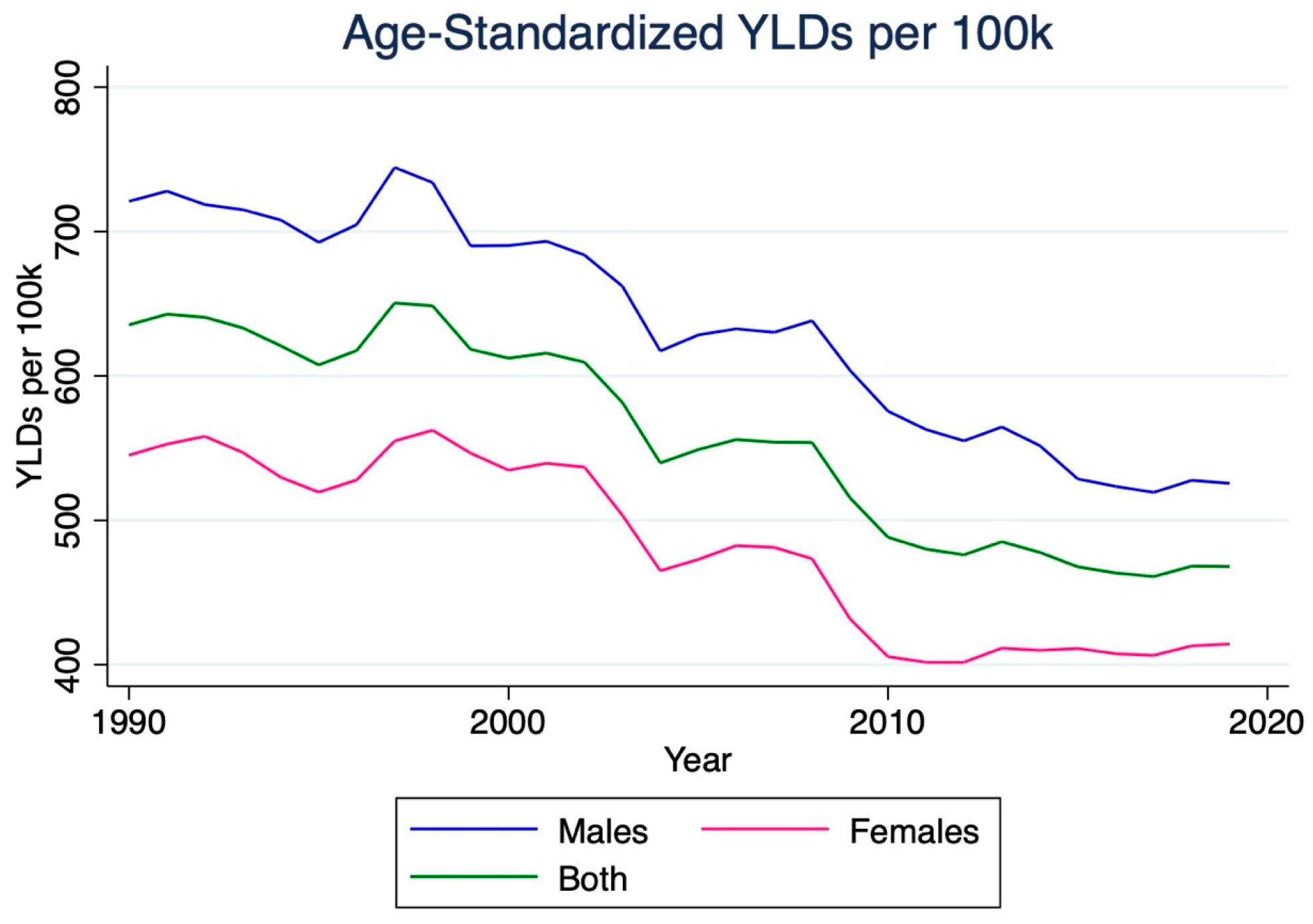
3.5. Years Lived with Disability (YLDs)
3.6. Years of Life Lost (YLLs)
3.7. Risk Factors
| Male | Female | Total | |
|---|---|---|---|
| All Risk Factors | 512.8 (658.3 to 396.8) | 418.1 (503 to 336.1) | 463.8 (547.1 to 389.9) |
| Ambient particulate matter pollution | 142.8 (193.9 to 99.3) | 103.7 (134.3 to 75.5) | 122.6 (154.3 to 92.8) |
| Household air pollution from solid fuels | 74.6 (115.3 to 41.3) | 74.7 (106.7 to 49.8) | 74.7 (105.4 to 49.2) |
| High temperature | 13.4 (26.1 to 1) | 10.7 (19.2 to 0.6) | 12 (21.8 to 0.8) |
| Low temperature | 11.3 (25.9 to −2.1) | 8.4 (19 to −1.9) | 9.8 (21 to −1.9) |
| Lead exposure | 50.2 (74.5 to 31) | 36 (51.8 to 22.1) | 42.8 (60.6 to 27.4) |
| Tobacco Smoking | |||
| Smoking | 95.5 (126.1 to 71.5) | 16.9 (22.5 to 12.1) | 55 (70.5 to 42.5) |
| Secondhand smoke | 14.4 (21.1 to 8.9) | 17.1 (23.4 to 11.7) | 15.8 (21.1 to 10.7) |
| Dietary Risks | |||
| Diet high in red meat | 5 (9.4 to 1.6) | 3.8 (6.9 to 1.3) | 4.4 (7.8 to 1.5) |
| Diet high in sodium | 37.3 (101.5 to 3.5) | 20.7 (68.3 to 1.2) | 28.7 (81.1 to 2.3) |
| Diet low in fruits | 44.3 (80.1 to 13.2) | 36.7 (62.5 to 12.4) | 40.4 (70.5 to 13) |
| Diet low in vegetables | 17 (32.4 to 2.6) | 14.8 (28.3 to 2.6) | 15.8 (30 to 2.6) |
| Diet low in whole grains | 26.4 (43.5 to 6.8) | 20.1 (31.9 to 4.6) | 23.2 (35.9 to 5.7) |
| Alcohol use | 16.3 (30.7 to 3.4) | −0.7 (0.8 to −2.1) | 7.5 (14.6 to 1) |
| Physiological Factors | |||
| High fasting plasma glucose | 184 (342 to 91.7) | 132.2 (249.2 to 65.9) | 157.2 (293.2 to 81.4) |
| High LDL cholesterol | 98.9 (179.8 to 51.4) | 91.5 (165.4 to 48.7) | 95.2 (167.8 to 50.6) |
| High systolic blood pressure | 284.3 (386 to 203.7) | 246.3 (319.9 to 181.8) | 265 (336.8 to 202.5) |
| High body mass index | 62.4 (105.7 to 31.2) | 64.6 (99.1 to 35.8) | 63.6 (98.2 to 35.3) |
| Kidney dysfunction | 57.7 (80.4 to 40.1) | 48.2 (65.4 to 32.6) | 52.9 (70.3 to 38.2) |
| Cluster of Risk Factors | |||
| Air pollution | 217.4 (282 to 164.2) | 178.4 (217.2 to 139.9) | 197.3 (235.3 to 162.2) |
| Non-optimal temperature | 24.5 (42.5 to 9.3) | 18.9 (31.3 to 7) | 21.6 (35.9 to 8.6) |
| Tobacco | 107.3 (140.3 to 80.1) | 33.4 (43.2 to 24.9) | 69.2 (86.6 to 54.1) |
| Dietary risks | 131.9 (203.2 to 74.3) | 99.6 (148.4 to 59.9) | 115.2 (170.7 to 68.8) |
| Behavioral risks | 233.4 (319.1 to 166.3) | 142.5 (194 to 96.2) | 186.5 (249 to 135.4) |
| Metabolic risks | 413.2 (538.8 to 307.8) | 347.1 (429.8 to 267.6) | 379.2 (459.2 to 304.9) |
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| GBD | Global Burden of Disease |
| DALYs | Disability-Adjusted Life Years |
| YLDs (YLD) | Years Lived with Disability |
| YLLs (YLL) | Years of Life Lost |
| UI | Uncertainty Interval |
| CI | Confidence Interval |
| WHO | World Health Organization |
| CODEm | Cause of Death Ensemble Model |
| DisMod-MR 2.1 | Disease Modeling–Meta Regression, version 2.1 |
| BMI | Body Mass Index |
| LDL | Low-Density Lipoprotein |
| PAF(s) | Population Attributable Fraction(s) |
| IRB | Institutional Review Board |
| NPCDCS | National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke |
| WHO ICCC | World Health Organization Innovative Care for Chronic Conditions |
| CHWs | Community Health Workers |
| PCPs | Primary Care Physicians |
| TOAST | Trial of ORG 10172 in Acute Stroke Treatment |
References
- Mehndiratta, M.M.; Singhal, A.B.; Chaturvedi, S.; Sivakumar, M.R.; Moonis, M. Meeting the challenges of stroke in India. Neurology 2013, 80, 2246–2247. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, M.O.; Thrift, A.G.; Mahal, A.; Ishida, M.; Martins, S.; Johnson, W.D.; Pandian, J.; Abd-Allah, F.; Yaria, J.; Phan, H.T.; et al. Primary stroke prevention worldwide: Translating evidence into action. Lancet Public Health 2022, 7, e74–e85. [Google Scholar] [CrossRef] [PubMed]
- GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2133–2161. [Google Scholar] [CrossRef]
- Malik, C.; Khanna, S.; Jain, Y.; Jain, R. Geriatric population in India: Demography, vulnerabilities, and healthcare challenges. J. Fam. Med. Prim. Care 2021, 10, 72–76. [Google Scholar] [CrossRef]
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Ma, Q.; Li, R.; Wang, L.; Yin, P.; Wang, Y.; Yan, C.; Ren, Y.; Qian, Z.; Vaughn, M.G.; McMillin, S.E.; et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2021, 6, e897–e906. [Google Scholar] [CrossRef] [PubMed]
- Danaei, G.; Finucane, M.M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.-H.; Stevens, G.A.; et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.O.; Pandian, J.; Lindsay, P.; Grupper, M.F.; Rautalin, I. World Stroke Organization: Global Stroke Fact Sheet 2025. Int. J. Stroke 2025, 20, 132–144. [Google Scholar] [CrossRef]
- Koton, S.; Sang, Y.; Schneider, A.L.C.; Rosamond, W.D.; Gottesman, R.F.; Coresh, J. Trends in Stroke Incidence Rates in Older US Adults: An Update From the Atherosclerosis Risk in Communities (ARIC) Cohort Study. JAMA Neurol. 2020, 77, 109–113. [Google Scholar] [CrossRef]
- Lackland, D.T.; Roccella, E.J.; Deutsch, A.F.; Fornage, M.; George, M.G.; Howard, G.; Kissela, B.M.; Kittner, S.J.; Lichtman, J.H.; Lisabeth, L.D.; et al. Factors influencing the decline in stroke mortality: A statement from the American Heart Association/American Stroke Association. Stroke 2014, 45, 315–353. [Google Scholar] [CrossRef]
- Ruan, Z.; Qi, J.; Yin, P.; Qian, Z.; Liu, J.; Liu, Y.; Yang, Y.; Li, H.; Zhang, S.; Howard, S.W.; et al. Prolonged Life Expectancy for Those Dying of Stroke by Achieving the Daily PM2.5 Targets. Glob. Chall. 2020, 4, 2000048. [Google Scholar] [CrossRef]
- Li, J.-X.; Zhong, Q.-Q.; Yuan, S.-X.; Zhu, F. Trends in deaths and disability-adjusted life-years of stroke attributable to low physical activity worldwide, 1990–2019. BMC Public Health 2023, 23, 2242. [Google Scholar] [CrossRef]
- Kim, A.S.; Cahill, E.; Cheng, N.T. Global Stroke Belt: Geographic Variation in Stroke Burden Worldwide. Stroke 2015, 46, 3564–3570. [Google Scholar] [CrossRef]
- Pandey, B.; Reba, M.; Joshi, P.K.; Seto, K.C. Urbanization and food consumption in India. Sci. Rep. 2020, 10, 17241. [Google Scholar] [CrossRef] [PubMed]
- Bhan, N.; Karan, A.; Srivastava, S.; Selvaraj, S.; Subramanian, S.V.; Millett, C. Have Socioeconomic Inequalities in Tobacco Use in India Increased Over Time? Trends From the National Sample Surveys (2000–2012). Nicotine Tob. Res. 2016, 18, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Asaria, M.; Mazumdar, S.; Chowdhury, S.; Mazumdar, P.; Mukhopadhyay, A.; Gupta, I. Socioeconomic inequality in life expectancy in India. BMJ Glob. Health 2019, 4, e001445. [Google Scholar] [CrossRef]
- Gupta, I.; Mondal, S. Urban health in India: Who is responsible? Int. J. Health Plan. Manag. 2015, 30, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, X.; Sang, H.; Niu, X.; Liu, T.; Liu, W.; Li, J. Urban-rural differences in risk factors for ischemic stroke in northern China. Medicine 2019, 98, e15782. [Google Scholar] [CrossRef]
- Sridharan, S.E.; Unnikrishnan, J.; Sukumaran, S.; Sylaja, P.; Nayak, S.D.; Sarma, P.S.; Radhakrishnan, K. Incidence, Types, Risk Factors, and Outcome of Stroke in a Developing Country: The Trivandrum Stroke Registry. Stroke 2009, 40, 1212–1218. [Google Scholar] [CrossRef]
- Yan, L.L.; Li, C.; Chen, J.; Miranda, J.J.; Luo, R.; Bettger, J.; Zhu, Y.; Feigin, V.; O’DOnnell, M.; Zhao, D.; et al. Prevention, management, and rehabilitation of stroke in low- and middle-income countries. eNeurologicalSci 2016, 2, 21–30. [Google Scholar] [CrossRef]
- Yoon, C.W.; Bushnell, C.D. Stroke in Women: A Review Focused on Epidemiology, Risk Factors, and Outcomes. J. Stroke 2023, 25, 2–15. [Google Scholar] [CrossRef]
- Olson, M.M.; Alhelou, N.; Kavattur, P.S.; Rountree, L.; Winkler, I.T. The persistent power of stigma: A critical review of policy initiatives to break the menstrual silence and advance menstrual literacy. PLOS Glob. Public Health 2022, 2, e0000070. [Google Scholar] [CrossRef]
- Shahid, R.; Shoker, M.; Chu, L.M.; Frehlick, R.; Ward, H.; Pahwa, P. Impact of low health literacy on patients’ health outcomes: A multicenter cohort study. BMC Health Serv. Res. 2022, 22, 1148. [Google Scholar] [CrossRef]
- Idris, I.B.; Hamis, A.A.; Bukhori, A.B.M.; Hoong, D.C.C.; Yusop, H.; Shaharuddin, M.A.-A.; Fauzi, N.A.F.A.; Kandayah, T. Women’s autonomy in healthcare decision making: A systematic review. BMC Women’s Health 2023, 23, 643. [Google Scholar] [CrossRef]
- Mondal, D.; Karmakar, S.; Banerjee, A. Women’s autonomy and utilization of maternal healthcare in India: Evidence from a recent national survey. PLoS ONE 2020, 15, e0243553. [Google Scholar] [CrossRef]
- Dhamija, R.K.; Aggarwal, A.; Saluja, A.; Parihar, J.; Garg, D. Emerging Trends in Stroke Epidemiology in Indian Women Over the Last Decade. Neurol. India 2022, 70, 315. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Gaowgzeh, R.A.M.; Al Saif, A.; Chevidikunnan, M.F.; Soman, A.; Mazi, A.; BinMulayh, E.; Sahu, K.S.; Anjamparuthikal, H. Effect of Community Education Program on Stroke Symptoms and Treatment on School and College Students from South India: A Longitudinal Observational Study. Healthcare 2021, 9, 1637. [Google Scholar] [CrossRef]
- Pati, M.K.; Swaroop, N.; Kar, A.; Aggarwal, P.; Jayanna, K.; Van Damme, W. A narrative review of gaps in the provision of integrated care for noncommunicable diseases in India. Public Health Rev. 2020, 41, 8. [Google Scholar] [CrossRef]
- Venugopal, V.; Richa, R.; Singh, D.; Gautam, A.; Jahnavi, G. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke: A Scoping Review in the Context of Hypertension Prevention and Control in India. Indian J. Public Health 2023, 67, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- Lindley, R.I. Providing Stroke Expertise across India. J. Neurosci. Rural. Pract. 2021, 12, 226–227. [Google Scholar] [CrossRef] [PubMed]
- Pandian, J.D.; Sudhan, P. Stroke Epidemiology and Stroke Care Services in India. J. Stroke 2013, 15, 128. [Google Scholar] [CrossRef]
- Kamalakannan, S.; Gudlavalleti, A.S.V.; Gudlavalleti, V.S.M.; Goenka, S.; Kuper, H. Incidence & prevalence of stroke in India: A sys-tematic review. Indian J. Med. Res. 2017, 146, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Pandian, J.D.; Gall, S.L.; Kate, M.P.; Silva, G.S.; Akinyemi, R.O.; Ovbiagele, B.I.; Lavados, P.M.; Gandhi, D.B.C.; Thrift, A.G. Prevention of stroke: A global perspective. Lancet 2018, 392, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Renjith, V.; Soman, B.; Shanmughasundaram, S.; Arun, K.; Jeemon, P.; Antony, R.; Gopal, B.; Sylaja, P.N. Stroke awareness among community health workers from rural health blocks of Thiruvananthapuram, India. J. Neurosci. Rural. Pract. 2023, 14, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Kate, M.; Samuel, C.; Kamra, D.; Kaliyaperumal, A.; Nandi, J.; Khatter, H.; Sharma, M.; Pandian, J. Rural Stroke Surveillance and Establishment of Acute Stroke Care Pathway Using Frontline Health Workers in Rural Northwest India: The Ludhiana Experience. Neuroepidemiology 2021, 55, 297–305. [Google Scholar] [CrossRef]
- GBD 2021 Stroke Risk Factor Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 973–1003. [Google Scholar] [CrossRef]
- Krishnamurthi, R.; George, A.; Merkin, A.; Bhattacharjee, R.; Feigin, V.L. Can we stop the stroke tsunami? Mitigating the barriers, amplifying the facilitators. J. R. Soc. N. Z. 2022, 52, 109–128. [Google Scholar] [CrossRef]


| 2019 | Percent Change, 1990–2019 | 2019 | Percent Change, 1990–2019 | |
|---|---|---|---|---|
| Incidence (95% UI), thousands | Age-standardized Incidence per 100k (95% UI) | |||
| Male | 264.1 (222.1 to 311.9) | 107.5 | 48 (40.6 to 56.4) | −4.4 |
| Female | 271.6 (229.4 to 320.7) | 131.1 | 47.1 (39.8 to 55.3) | −3.5 |
| Total | 535.7 (453.2 to 631.8) | 118.8 | 47.5 (40.2 to 55.7) | −4.2 |
| Deaths (95% UI), thousands | Age-standardized mortality per 100k (95% UI) | |||
| Male | 141 (107.5 to 180.3) | 123.0 | 33.6 (26.3 to 42.5) | −27.3 |
| Female | 130.2 (100.7 to 160.4) | 183.5 | 27.8 (21.6 to 34) | −25.7 |
| Total | 271.2 (227.8 to 320.7) | 148.5 | 30.6 (25.7 to 35.8) | −27.0 |
| Prevalence (95% UI), thousands | Age-standardized Prevalence per 100k (95% UI) | |||
| Male | 3215.1 (2745.7 to 3677.6) | 125.4 | 522 (448.8 to 599) | 8.6 |
| Female | 3250.6 (2790.2 to 3702.2) | 135.6 | 513.4 (444.6 to 584) | 3.4 |
| Total | 6465.7 (5541 to 7378) | 130.4 | 516.4 (443.5 to 590) | 5.7 |
| DALYs (95% UI), thousands | Age-standardized DALYs per 100k (95% UI) | |||
| Male | 3009.1 (2320.9 to 3853.5) | 102.8 | 594.6 (466.9 to 753.6) | −24.1 |
| Female | 2680.2 (2154.8 to 3217.5) | 145.7 | 492.5 (395.3 to 587) | −20.6 |
| Total | 5689.3 (4821.1 to 6649.5) | 121.0 | 541.4 (461.6 to 633.2) | −23.1 |
| YLDs (95% UI), thousands | Age-standardized YLDs per 100k (95% UI) | |||
| Male | 416.8 (288.9 to 542.2) | 130.4 | 69 (48.1 to 89.5) | 9.7 |
| Female | 490.3 (345.2 to 632.1) | 140.0 | 78.2 (55.6 to 100.7) | 4.1 |
| Total | 907 (640.3 to 1172.9) | 135.5 | 73.4 (51.5 to 94.9) | 6.7 |
| YLLs (95% UI), thousands | Age-standardized YLLs per 100k (95% UI) | |||
| Male | 2592.3 (1906.7 to 3412.8) | 98.9 | 525.6 (395.9 to 679.8) | −27.1 |
| Female | 2189.9 (1688 to 2710.5) | 147.0 | 414.3 (320.2 to 509.7) | −24.0 |
| Total | 4782.3 (3945.5 to 5743.7) | 118.4 | 467.9 (391.6 to 559.2) | −26.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goyal, A.D.; Gajjar, A.A.; Muhammad, N.; Wu, A.Q.; Polavarapu, H.; Tang, O.; Salem, M.M.; Paliwoda, E.D.; Gupta, N.; Doad, J.; et al. A Three-Decade Analysis of Ischemic Stroke in India: Mortality, Morbidity, and Risk Factors Using the Global Burden of Diseases Study from 1990 to 2019. J. Clin. Med. 2025, 14, 7807. https://doi.org/10.3390/jcm14217807
Goyal AD, Gajjar AA, Muhammad N, Wu AQ, Polavarapu H, Tang O, Salem MM, Paliwoda ED, Gupta N, Doad J, et al. A Three-Decade Analysis of Ischemic Stroke in India: Mortality, Morbidity, and Risk Factors Using the Global Burden of Diseases Study from 1990 to 2019. Journal of Clinical Medicine. 2025; 14(21):7807. https://doi.org/10.3390/jcm14217807
Chicago/Turabian StyleGoyal, Aditya D., Avi A. Gajjar, Najib Muhammad, Albert Q. Wu, Hanish Polavarapu, Oliver Tang, Mohamed M. Salem, Ethan D. Paliwoda, Nithin Gupta, Jagroop Doad, and et al. 2025. "A Three-Decade Analysis of Ischemic Stroke in India: Mortality, Morbidity, and Risk Factors Using the Global Burden of Diseases Study from 1990 to 2019" Journal of Clinical Medicine 14, no. 21: 7807. https://doi.org/10.3390/jcm14217807
APA StyleGoyal, A. D., Gajjar, A. A., Muhammad, N., Wu, A. Q., Polavarapu, H., Tang, O., Salem, M. M., Paliwoda, E. D., Gupta, N., Doad, J., Jankowitz, B. T., Srinivasan, V. M., & Burkhardt, J.-K. (2025). A Three-Decade Analysis of Ischemic Stroke in India: Mortality, Morbidity, and Risk Factors Using the Global Burden of Diseases Study from 1990 to 2019. Journal of Clinical Medicine, 14(21), 7807. https://doi.org/10.3390/jcm14217807






