In-Hospital Mortality Among 40,253 Older Adults with Hip Fracture: Survival Outcomes and Multivariate Analysis in a Chilean Cohort
Abstract
1. Introduction
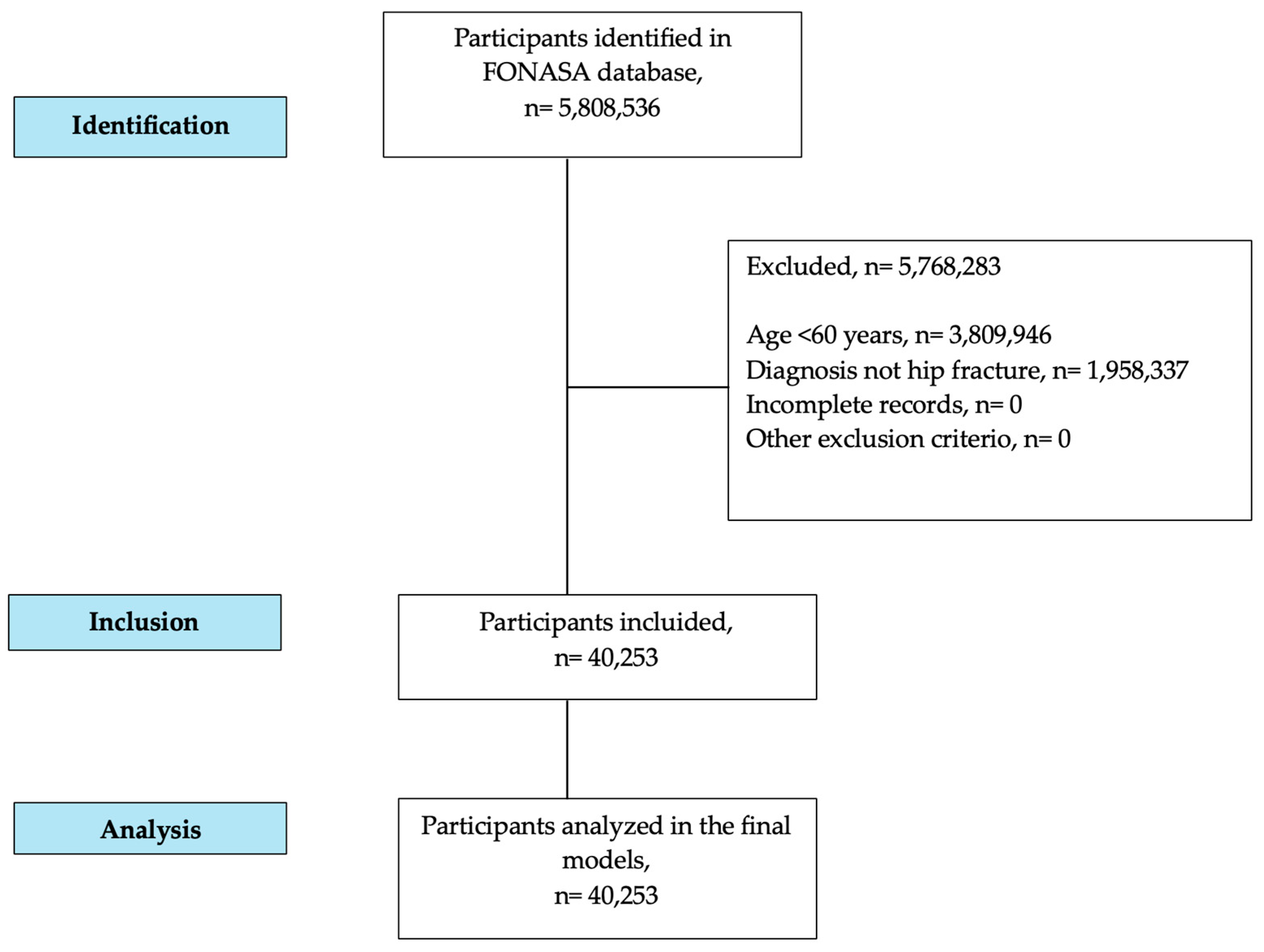
2. Materials and Methods
2.1. Data Collection
2.2. Variables
2.2.1. Dependent Variable
2.2.2. Independent Variables
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DRG | Diagnosis-Related Group |
| FONASA | National Health Fund (Fondo Nacional de Salud, Chile) |
| ICD-10 | International Classification of Diseases |
References
- Viganò, M.; Pennestrì, F.; Listorti, E.; Banfi, G. Proximal hip fractures in 71,920 elderly patients: Incidence, epidemiology, mortality and costs from a retrospective observational study. BMC Public Health 2023, 23, 1963. [Google Scholar] [CrossRef]
- Xu, Q.; Ou, X.; Li, J. The risk of falls among the aging population: A systematic review and meta-analysis. Front. Public Health 2022, 10, 902599. [Google Scholar] [CrossRef]
- Wu, A.-M.; Bisignano, C.; James, S.L.; Abady, G.G.; Abedi, A.; Abu-Gharbieh, E.; Alhassan, R.K.; Alipour, V.; Arabloo, J.; Asaad, M.; et al. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021, 2, e580–e592. [Google Scholar] [CrossRef]
- Williamson, S.; Landeiro, F.; McConnell, T.; Fulford-Smith, L.; Javaid, M.K.; Judge, A.; Leal, J. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos. Int. 2017, 28, 2791–2800. [Google Scholar] [CrossRef] [PubMed]
- Barceló, M.; Torres, O.H.; Mascaró, J.; Casademont, J. Hip fracture and mortality: Study of specific causes of death and risk factors. Arch. Osteoporos. 2021, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Johnell, O.; Kanis, J. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Limpawattana, P.; Manjavong, M.; Chindaprasirt, J.; Wareechai, P. National 5-year data analysis of health outcomes in hospitalized geriatric patients with hip fracture. Injury 2025, 56, 112513. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-Y.; Tsai, C.-F.; Hsu, Y.-H.; Yang, H.-Y. Exploring mortality risk factors and specific causes of death within 30 days after hip fracture hospitalization. Sci. Rep. 2024, 14, 27544. [Google Scholar] [CrossRef]
- Zhang, H.; Ma, L.; Yu, X. Risk factors of postoperative complications and in-hospital mortality after hip fracture among patients older than 80 years old: A retrospective study. BMC Surg. 2025, 25, 122. [Google Scholar] [CrossRef]
- Vitiello, R.; Pesare, E.; Capece, G.; Di Gialleonardo, E.; De Matthaeis, A.; Franceschi, F.; Maccauro, G.; Covino, M. Surgical timing and clinical factor predicting in-hospital mortality in older adults with hip fractures: A neuronal network analysis. J. Orthop. Traumatol. 2025, 26, 30. [Google Scholar] [CrossRef]
- Folbert, E.C.; Hegeman, J.H.; Gierveld, R.; van Netten, J.J.; van der Velde, D.; Duis, H.J.T.; Slaets, J.P. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch. Orthop. Trauma. Surg. 2017, 137, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Nunes, B.K.G.; de Lima, B.R.; Guimarães, L.C.d.C.; Guimarães, R.A.; Rosso, C.F.W.; Felipe, L.d.A.; Pagotto, V. Survival analysis of hospitalized elderly people with fractures in Brazil over one year. Geriatrics 2020, 5, 10. [Google Scholar] [CrossRef]
- Di Giovanni, P.; Di Martino, G.; Zecca, I.; Porfilio, I.; Romano, F.; Staniscia, T. Predictors of prolonged hospitalization and in-hospital mortality after hip fracture: A retrospective study on discharge registry. Ann. Ig. 2022, 34, 467–477. [Google Scholar] [CrossRef]
- Sheehan, K.J.; Sobolev, B.; Guy, P.; Kuramoto, L.; Morin, S.N.; Sutherland, J.M.; Beaupre, L.; Griesdale, D.; Dunbar, M.; Bohm, E.; et al. In-hospital mortality after hip fracture by treatment setting. Can. Med. Assoc. J. 2016, 188, 1219–1225. [Google Scholar] [CrossRef]
- Hu, F.; Jiang, C.; Shen, J.; Tang, P.; Wang, Y. Preoperative predictors for mortality following hip fracture surgery: A systematic review and meta-analysis. Injury 2012, 43, 676–685. [Google Scholar] [CrossRef]
- Pincus, D.; Ravi, B.; Wasserstein, D.; Huang, A.; Paterson, J.M.; Nathens, A.B.; Kreder, H.J.; Jenkinson, R.J.; Wodchis, W.P. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA 2017, 318, 1994–2003. [Google Scholar] [CrossRef]
- Warren, M.; Bretherton, C.; Parker, M. Delay to surgery beyond 12 hours is associated with increased hip fracture mortality. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2973–2980. [Google Scholar] [CrossRef]
- Castillón, P.; Nuñez, J.H.; Mori-Gamarra, F.; Ojeda-Thies, C.; Sáez-López, P.; Salvador, J.; Anglés, F.; González-Montalvo, J.I.; Rnfc, P.I.T. Hip fractures in Spain: Are we on the right track? Statistically significant differences in hip fracture management between Autonomous Communities in Spain. Arch. Osteoporos. 2021, 16, 40. [Google Scholar] [CrossRef] [PubMed]
- Ercin, E.; Bilgili, M.G.; Sari, C.; Basaran, S.H.; Tanriverdi, B.; Edipoglu, E.; Celen, K.M.; Cetingok, H.; Kural, C. Risk factors for mortality in geriatric hip fractures: A compressional study of different surgical procedures in 785 consecutive patients. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Haryanto, J.; Suarilah, I.; Saragih, I.D.; Indarwati, R.; Zulkarnain, H.; Qona’ah, A. Global prevalence of mortality and poor functional outcomes among older adults with hip fracture: A meta-analysis of cohort studies. Fizjoterapia Pol. 2025, 25, 345–356. [Google Scholar] [CrossRef]
- Asociación Argentina de Ortopedia y Traumatología (AAOT). Comité de Morbi-Mortalidad. 2021. Available online: https://aaot.org.ar/certificacion/comite-de-morbi-mortalidad/ (accessed on 30 August 2025).
- Chlebeck, J.D.; Birch, C.E.; Blankstein, M.; Kristiansen, T.; Bartlett, C.S.; Schottel, P.C. Nonoperative geriatric hip fracture treatment is associated with increased mortality: A matched cohort study. J. Orthop. Trauma 2019, 33, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Li, Z.; Cao, J.; Jiao, J.; Wang, Y.; Liu, G.; Liu, Y.; Li, F.; Song, B.; Jin, J.; et al. The association between major complications of immobility during hospitalization and quality of life among bedridden patients: A 3 month prospective multi-center study. PLoS ONE 2018, 13, e0205729. [Google Scholar] [CrossRef]
- Loggers, S.A.; Van Lieshout, E.M.; Joosse, P.; Verhofstad, M.H.; Willems, H.C. Prognosis of nonoperative treatment in elderly patients with a hip fracture: A systematic review and meta-analysis. Injury 2020, 51, 2407–2413. [Google Scholar] [CrossRef]
- Guiloff, R.; Valderrama, C.; Edwards, D.; Contreras, M.; Vaisman, A. Epidemiología y mortalidad en pacientes con fractura de cadera: Impacto de la latencia quirúrgica en una cohorte de pacientes de un hospital público en Chile. Rev. Med. Chile 2023, 151, 1456–1463. [Google Scholar] [CrossRef]
- Andaloro, S.; Cacciatore, S.; Risoli, A.; Comodo, R.M.; Brancaccio, V.; Calvani, R.; Giusti, S.; Schlögl, M.; D’angelo, E.; Tosato, M.; et al. Hip Fracture as a Systemic Disease in Older Adults: A Narrative Review on Multisystem Implications and Management. Med. Sci. 2025, 13, 89. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Fakler, J.K.; Pieroh, P.; Höch, A.; Roth, A.; Kleber, C.; Löffler, M.; Heyde, C.E.; Zeynalova, S. Predictors of long-term mortality in older patients with hip fractures managed by hemiarthroplasty: A 10-year study based on a population registry in Saxony, Germany. Patient Saf. Surg. 2024, 18, 15. [Google Scholar] [CrossRef]
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and mortality of hip fractures in the United States. JAMA 2009, 302, 1573–1579. [Google Scholar] [CrossRef]
- Endo, Y.; Aharonoff, G.B.; Zuckerman, J.D.; Egol, K.A.; Koval, K.J. Gender differences in patients with hip fracture: A greater risk of morbidity and mortality in men. J. Orthop. Trauma. 2005, 19, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Bekeris, J.; Wilson, L.A.; Bekere, D.; Liu, J.; Poeran, J.; Zubizarreta, N.; Fiasconaro, M.; Memtsoudis, S.G. Trends in comorbidities and complications among patients undergoing hip fracture repair. Anesth. Analg. 2021, 132, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Gadgaard, N.; Varnum, C.; Nelissen, R.; Vandenbroucke-Grauls, C.; Sørensen, H.; Pedersen, A. Comorbidity and risk of infection among patients with hip fracture: A Danish population-based cohort study. Osteoporos. Int. 2023, 34, 1739–1749. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.-T.; Moon, J.-K.; Kim, Y.-H. Do we really need a surgery for hip fractures in elderly patients? Mortality rate and influencing factors. Arthroplasty 2019, 1, 7. [Google Scholar] [CrossRef] [PubMed]
- Coffield, E.; Thirunavukkarasu, S.; Ho, E.; Munnangi, S.; Angus, L.G. Disparities in length of stay for hip fracture treatment between patients treated in safety-net and non-safety-net hospitals. BMC Health Serv. Res. 2020, 20, 100. [Google Scholar] [CrossRef]

| Variable | n = 40,253 |
|---|---|
| Age (years) [mean (DS)] | 81.94 (9.08) |
| Age Group | |
| 60–69 [n (%)] | 4502 (11.18%) |
| 70–79 [n (%)] | 10,124 (25.15%) |
| 80–89 [n (%)] | 16,825 (41.80%) |
| ≥90 [n (%)] | 8802 (21.87%) |
| Sex | |
| Women [n (%)] | 30,908 (76.78%) |
| Men [n (%)] | 9345 (23.22%) |
| Hospital outcome | |
| Survived [n (%)] | 38,840 (96.49%) |
| Deceased [n (%)] | 1413 (3.51%) |
| Surgical treatment | |
| Yes [n (%)] | 35,440 (88.04%) |
| No [n (%)] | 4813 (11.96%) |
| Comorbidities | 6.59 (4.24) |
| <3 [n (%)] | 4215 (10.47%) |
| ≥3 [n (%)] | 36,038 (89.53%) |
| Severity level-DRG | |
| Mild [n (%)] | 15,985 (39.71%) |
| Moderate [n (%)] | 16,150 (40,12%) |
| Severe [n (%)] | 8038 (19.97%) |
| Unclassified [n (%)] | 80 (0.20%) |
| Length of hospital stay (days) [mean (DS)] | 12.73 (13.94) |
| Relative weight (Unitless) [mean (DS)] | 0.54 (0.01) |
| Variable | HR (Unadjusted) | p | HR (Adjusted) | p |
|---|---|---|---|---|
| Age (per year) | 1.07 (1.06–1.07) | <0.001 | 1.05 (1.04–1.05) | <0.001 |
| Sex (male) | 1.17 (1.04–1.31) | 0.009 | 1.12 (1.03–1.27) | <0.001 |
| Surgical treatment (no) | 10.91 (9.81–12.12) | <0.001 | 9.56 (8.38–10.90) | <0.001 |
| Comorbidities (≥3) | 3.27 (2.33–4.77) | <0.001 | 2.73 (1.98–3.99) | <0.001 |
| Severity level-DRG (per level) | 4.66 (4.21–5.15) | <0.001 | 3.87 (3.42–4.37) | <0.001 |
| Relative weight (per unit) | 0.85 (0.78–0.92) | 0.091 | 1.15 (1.09–1.22) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzmán-Muñoz, E.; Concha-Cisternas, Y.; Vásquez-Muñoz, M.; Yañez-Sepúlveda, R.; Núñez-Espinosa, C.; Bittelman Saporte, S.; Nemtala Urquiza, F.; Morales Araneda, R. In-Hospital Mortality Among 40,253 Older Adults with Hip Fracture: Survival Outcomes and Multivariate Analysis in a Chilean Cohort. J. Clin. Med. 2025, 14, 7717. https://doi.org/10.3390/jcm14217717
Guzmán-Muñoz E, Concha-Cisternas Y, Vásquez-Muñoz M, Yañez-Sepúlveda R, Núñez-Espinosa C, Bittelman Saporte S, Nemtala Urquiza F, Morales Araneda R. In-Hospital Mortality Among 40,253 Older Adults with Hip Fracture: Survival Outcomes and Multivariate Analysis in a Chilean Cohort. Journal of Clinical Medicine. 2025; 14(21):7717. https://doi.org/10.3390/jcm14217717
Chicago/Turabian StyleGuzmán-Muñoz, Eduardo, Yeny Concha-Cisternas, Manuel Vásquez-Muñoz, Rodrigo Yañez-Sepúlveda, Cristian Núñez-Espinosa, Sacha Bittelman Saporte, Fernando Nemtala Urquiza, and Rodrigo Morales Araneda. 2025. "In-Hospital Mortality Among 40,253 Older Adults with Hip Fracture: Survival Outcomes and Multivariate Analysis in a Chilean Cohort" Journal of Clinical Medicine 14, no. 21: 7717. https://doi.org/10.3390/jcm14217717
APA StyleGuzmán-Muñoz, E., Concha-Cisternas, Y., Vásquez-Muñoz, M., Yañez-Sepúlveda, R., Núñez-Espinosa, C., Bittelman Saporte, S., Nemtala Urquiza, F., & Morales Araneda, R. (2025). In-Hospital Mortality Among 40,253 Older Adults with Hip Fracture: Survival Outcomes and Multivariate Analysis in a Chilean Cohort. Journal of Clinical Medicine, 14(21), 7717. https://doi.org/10.3390/jcm14217717









